Abstract
Background:
Inhalation anesthetics have many advantages for outpatient general anesthesia, such as minimal postoperative side-effects and rapid and full recovery. The aim of this randomized study was to compare the postoperative recovery time of sevoflurane and desflurane and to observe the effects of anesthesia on mental, psychomotor and cognitive functions and pain in outpatients undergoing arthroscopic surgery.
Patients and Methods:
This study included 40 American Society of Anesthesiologists I-II patients who were divided into two groups via sealed envelopes. For maintenance of anesthesia, a mixture of 66% N2O and 33% O2 and 4–7% desflurane was used in Group D, and a mixture of 66% N2O and 33% O2 and 1–2.5% sevoflurane was used in Group S. The modified Aldrete score (MAS) was evaluated postoperatively at time points determined previously. An MAS of 8 or higher was considered to indicate alertness. Mental and psychomotor functions of the patients were evaluated using the short cognitive examination (SCE), and postoperative pain levels were evaluated using the visual analogue scale (VAS).
Results:
There was no difference between the groups in terms of demographic data (P > 0.05). The mean time to reach MAS 8, eye-opening, and orientation were higher in Group S as compared to Group D (P < 0.01). The mean MAS initially and at 5 and 10 min was higher in Group D as compared to Group S (P < 0.001). The mean SCE at 5 and 15 min was higher in Group D as compared to Group S (P < 0.01). There was no significant difference between the groups in terms of VAS scores (P > 0.05).
Conclusion:
It has been determined that desflurane provided better quality and more rapid recovery than sevoflurane, and the return of cognitive functions in the early postoperative period was faster. In conclusion, both agents can apparently be used safely in outpatient anesthetic procedures.
Keywords: Desflurane, outpatient anesthesia, pain, psychomotor functions, recovery, sevoflurane
INTRODUCTION
The numbers of day surgeries performed have increased rapidly due to technological advances for modern anesthesiologists.[1] The use of rapid and short-acting intravenous (IV) anesthetics, inhalation anesthetics, analgesics and muscle relaxants in anesthesia, in addition to new minimally invasive surgery options, have made outpatient general anesthesia possible in many patients with concomitant illness.[1] General anesthesia is fairly commonly used for outpatient surgery. It is often preferred because of the favorable properties at the surgical site as well as due to the patients’ desire to be rendered unaware of the procedure.[2]
Inhalation anesthetics are often preferred because they have minimal postoperative side effects and usually allow a quick and complete recovery.[3] Easier control of the depth of intraoperative anesthesia and rapid recovery with inhalation anesthetics provide a significant advantage.[4] The ideal inhalation anesthetic must have certain properties: Chemical purity, good stability, resistance to metabolism by the body, no organ-specific toxic effects, low blood/gas solubility which will enable rapid induction and elimination, low flammability (in air, oxygen or nitrous oxide), no long-term adverse effects on employees, be fragrant and nonirritating, minimal effects on vital functions, good analgesic effects, short-acting effects on the central nervous system, and reasonably priced.[5] Halothane was the first halogenated agent, which gave rise to the development of isoflurane, desflurane, and sevoflurane, all of which have drawbacks and are not considered the “ideal” volatile anesthetic.
In this study, we aimed to compare the postoperative recovery time and the effects of sevoflurane and desflurane on mental, psychomotor and cognitive functions and pain in patients undergoing outpatient arthroscopic surgery.
PATIENTS AND METHODS
This study included 40 patients (20 females, 20 males) between the ages of 22 and 63 and of the American Society of Anesthesiologists (ASA) I-II classification, who had been admitted to the Haseki Training and Research Hospital Clinic of Orthopedics and Traumatology to undergo outpatient arthroscopy. For this prospective, randomized, double-blinded study, local ethics committee approval and informed consent were obtained. Exclusion criteria were as follows: Patients with significant coronary, pulmonary, renal, or hepatic disease; medical history of neurological disease; chronic alcoholism or drug use; diabetes; medical or family history of malignant hyperthermia; allergy to any medications to be used; morbidly obese patients; those who had undergone general anesthesia in the last 7 days; and patients who were illiterate. Patients with ASA II classification who used regular medications and had normal arterial blood pressure were included in the study.
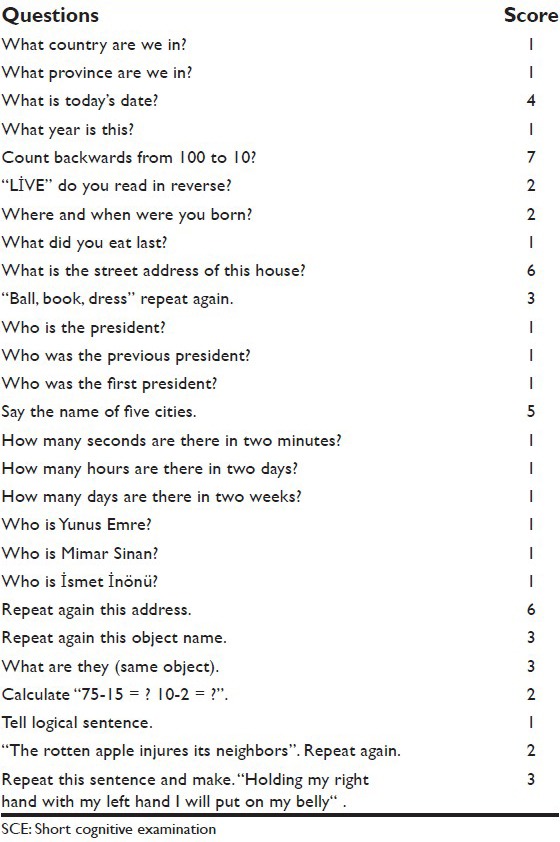
On the day of surgery, a preoperative short cognitive examination (SCE) [Table 1] was applied to the patients in the operating room, and the control values were calculated. For the patients who did not receive premedication, a PETAS KMA 260R monitor was used after vascular access was obtained with a 22 G cannula and an infusion of 0.9% NaCl was started. Anesthesia was induced with thiopental (5 mg/kg) and vecuronium bromide (0.1 mg/kg) was administered for muscle relaxation and endotracheal intubation. Endotracheal intubation was performed after 2 min of who were 100% O2 mask ventilation.
Table 1.
SCE
Patients were divided into two groups using sealed envelopes. For Group D, anesthesia was maintained with a mixture of 66% N2O and 33% O2 and 4–7% desflurane, while Group S received a mixture of 66% N2O and 33% O2 and 1–2.5% sevoflurane. No opioid medications were used for the patients preoperatively, and 0.03 mg/kg vecuronium bromide was administered when muscle relaxation was required. At the end of surgery, patients were ventilated with 100% O2, and 0.01 mg/kg atropine and 0.04 mg/kg neostigmine were administered to patients exhibiting increased respiratory effort. When spontaneous respiration was adequate, patients were extubated. Following extubation, the modified Aldrete score (MAS) [Table 2] value was recorded as the baseline value.
Table 2.
MAS
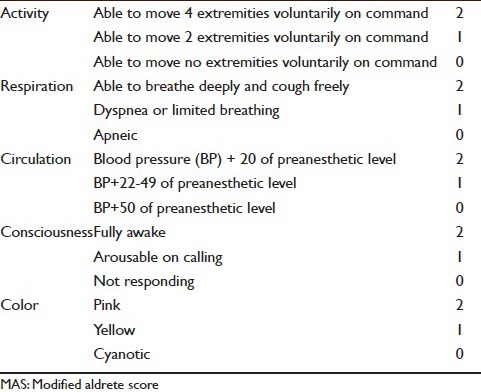
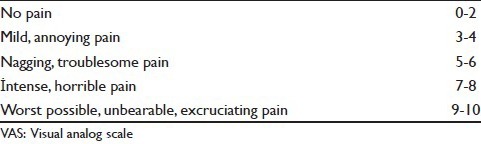
The MAS of patients taken to the recovery room was re-evaluated at 5, 10, 15, 20, 25, 30, 40, 50 and 60 min after the baseline measurement. MAS[6] was used as a unit for evaluation of the activity, respiration, circulation, consciousness, and color of the patients. After recovery from anesthesia, following a painful stimulus, MAS values of 8 and higher were considered to indicate consciousness. The time required to reach an MAS of 8 was recorded. Patients’ eye-opening and orientation time (able to provide their year and location of birth) were recorded. Sixty minutes after recovery, tenoxicam 20 mg IV was administered to all patients. To evaluate the patients’ mental and psychomotor functions, the SCE test[7] was used, which has 29 questions with a total value of 64. A chart was used to assess orientation (1–4 questions), attention (5 and 6 questions), memory (7–10 questions), general information (ll-20 questions), short-term memory (21–22 questions), dyscalculia, dysgraphia, dyslexia, nominal aphasia and disorientation (23–29 questions). The questions included and the scoring for each are shown in Table 1. To assess postoperative pain levels, a visual analogue scale (VAS)[8] was used [Table 3]. The VAS was evaluated at 5, 10, 15, 20, 25, 30, 40, 50 and 60 min postoperatively.
Table 3.
VAS
Statistical analysis
The SPSS for Windows 10.0 statistical software package was used to analyse the data. For comparisons, Student's t-test, Mann–Whitney U-test, a paired t-test, and Chi-square tests were used. P < 0.05 and <0.01 were considered to indicate statistically significant and highly significant, respectively.
RESULTS
The groups were evaluated in terms of demographic data; no differences were identified [P > 0.05, Table 4]. There was no statistically significant difference between Groups D and S in terms of mean duration of the operation (61.80 ± 15.08, 63.65 ± 13.65, respectively) or the mean duration of anesthesia (78.25 ± 14:37, 79.65 ± 12.45, respectively) [P > 0.05, Table 5].
Table 4.
Sex and ASA score
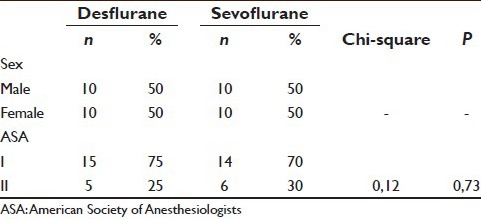
Table 5.
Comparison of the groups in terms of recovery
The mean time to reach MAS of 8, eye opening and orientation in Group S was significantly higher than in Group D (P < 0.01). The mean MAS initially and after 5 and 10 min was significantly higher in Group D as compared to Group S (P < 0.01). No significant difference was observed between the groups in the MAS at other time points [P > 0.05, Table 5].
The mean SCE values of Group D at 5 and 15 min were significantly higher than those of Group S (P < 0.01). No significant difference was observed in the SCE at other time points between the groups [P > 0.05, Table 6].
Table 6.
Comparison of the groups in terms of SCE
In Group D, the mean SCE values at 5, 10, 15, 20, 25, 30, 40 and 50 min were significantly lower than those at baseline (P < 0.01). In Group S, the mean SCE at 5, 10, 15, 20, 25, 30, 40, 50 and 60 min was significantly lower than those at baseline [P < 0.01, Table 7].
Table 7.
Internal comparison of the groups in terms of SCE
There was no significant difference between the groups in terms of VAS score [P > 0.05, Table 8].
Table 8.
Comparison of the groups in terms of VAS
DISCUSSION
Due to the increasing incidence of outpatient surgical applications, full return of complex physiological functions after general anesthesia with a short-duration and reliable recovery has become increasingly important. Due to the low solubility of sevoflurane and desflurane, they have the advantages of easier control of anesthetic depth and more rapid recovery from anesthesia. In our study of physical score ASA I-II patients who underwent outpatient arthroscopic surgery under general anesthesia, we compared the postoperative recovery time for desflurane and sevoflurane and the effects of anesthesia on mental, psychomotor and cognitive functions and pain.
We determined that the mean time to reach MAS 8, eye opening and orientation of the sevoflurane group were significantly higher compared to those in the desflurane group, the mean SCE values at 5 and 15 min were higher in the desflurane group than the sevoflurane group, but there was no statistically significant difference between the groups in terms of VAS values. Nathanson et al.[9] compared the recovery characteristics of sevoflurane and desflurane, and extubation, waking up, and orientation duration was found to be shorter in the desflurane group than the sevoflurane group. In our study, we found similar results.
Dupont et al.[10] found that the time until extubation and eye-opening were significantly shorter in the desflurane group. They used the MAS to assess the recovery and reported that recovery of the desflurane group was significantly rapider than the sevoflurane group. The prolonged effect of residual sevoflurane with hexafluoroisopropanol was considered to account for the slower recovery from sevoflurane. In addition, the degradation of sevoflurane to compound A has been reported to delay waking after sevoflurane anaesthesia.[11] We believe that the slower elimination and recovery of sevoflurane compared with desflurane can be explained by the irreversible binding of the compound A to body proteins. The study by Eger et al.[12] supports this finding. In the meta-analysis of Macario et al.,[13] the time until extubation, fulfill the commands and orientation in patients administered desflurane was l. 0–l. 2 min shorter than in the patients administered sevoflurane.
Song et al.[14] recorded wake-up times and the MAS and compared the effects of propofol, desflurane, and sevoflurane in patients undergoing ambulatory anesthesia. Desflurane was found to have the fastest recovery time. In this study, we recorded the time needed to reach MAS 8, eye-opening, and orientation. The mean MAS initially and after 5 and 10 min was significantly higher in the desflurane group compared to the sevoflurane group (P < 0.0l). There was no significant difference between the groups in terms of MAS values at other time points (P > 0.05). The mean time required to reach MAS 8, eye opening and orientation was significantly longer in the sevoflurane group than the desflurane group (P < 0.0l).
Larsen et al.[15] used the Trieger Dot Test and Digit Substitution Test (DSST) to assess cognitive functions and reported no difference between the groups in terms of postoperative TDT. They also reported that 30 min after the operation, more patients in the desflurane group than in the sevoflurane group successfully passed the DSST. In addition, they reported a difference between the sevoflurane and desflurane groups at 60 min.
Chen et al.[16] reported no difference between the desflurane and sevoflurane groups in terms of mini-mental state examination (MMSE) values; the MMSE values in the first postoperative hour were significantly lower than the baseline values. It was reported that, in both groups, 85% of patients returned to initial values by the 3rd hour and all patients (with the exception of one patient in the sevoflurane group) returned to the initial MMSE values at by 24 h postoperatively. Furthermore, there was no significant difference between the two groups regarding the preoperative and postoperative l, 3, 6 and 24-h MMSE values.
Dupont et al.[10] reported that the time until eye opening, extubation, orientation, being able to say their date of birth and to name three flowers or cars in 100 patients who underwent unilateral ventilation was significantly shorter in the desflurane group compared with the sevoflurane and isoflurane groups (P < 0.01). It has also been reported that while return of cognitive functions (ability to name places, date of birth, and three flowers or cars) was significantly enhanced at 5 min in the desflurane group, there was no difference at 15 min.
Chen et al.[16] used the VAS not only to assess pain but also to assess sedation, fatigue, discomfort and nausea, and detected no difference between the groups in terms of side effects. Nathanson et al.[9] also used the VAS to assess sedation, confusion, coordination, nausea, and pain. They found that the VAS scores and the incidence of postoperative nausea and vomiting were similar in both groups. In our study, we found no significant difference between the groups in terms of VAS scores.
CONCLUSION
The study results indicate that the desflurane provides a shorter-duration, better-quality recovery than sevoflurane; return of cognitive functions was also faster in the early postoperative period. Postoperative pain, blood pressure, heart rate and SpO2 values were affected similarly by both agents. In conclusion, both agents can be used safely for outpatient anesthesia.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Verma R, Alladi R, Jakson I, Johnston I, Kumar C, Page R, et al. Day case and short stay surgery: 2. Anaesthesia. 2011;66:417–34. doi: 10.1111/j.1365-2044.2011.06651.x. [DOI] [PubMed] [Google Scholar]
- 2.Ebert TJ, Muzi M, Lopotka CW. Effects of sevoflurane on hemodynamics and sympathetic neural activity in humans: A comparison to isoflurane. Anesthesiology. 1994;81:A133. [Google Scholar]
- 3.Motsch J, Wandel C, Neff S, Martin E. A comparative study of the use of sevoflurane and propofol in ambulatory surgery. Anaesthesist. 1996;45(Suppl 1):S57–62. [PubMed] [Google Scholar]
- 4.Jones RM. Desflurane and sevoflurane: Inhalation anaesthetics for this decade? Br J Anaesth. 1990;65:527–36. doi: 10.1093/bja/65.4.527. [DOI] [PubMed] [Google Scholar]
- 5.Vlymen JM, White PF. Outpatient anesthesia. In: Miller RD, editor. Anesthesia. 5th ed. Pennsylvania, USA: Churchill Livingstone; 2000. pp. 2213–46. [Google Scholar]
- 6.White PF, Song D. New criteria for fast-tracking after outpatient anesthesia: A comparison with the modified Aldrete's scoring system. Anesth Analg. 1999;88:1069–72. doi: 10.1097/00000539-199905000-00018. [DOI] [PubMed] [Google Scholar]
- 7.Kayatekin MS, Ozturk MO, Savasir I. The reliability and validity studies of a brief cognitive status schedule (KKM) Dusunen Adam: The Journal of Psychiatry and Neurological Sciences. 1986;1:63–6. [Google Scholar]
- 8.Melzack R, Katz J. Pain measurement in persons in pain. In: Wall PD, Melzack R, editors. Textbook of Pain. 3rd ed. London: Churchill Livingstone; 1994. pp. 337–51. [Google Scholar]
- 9.Nathanson MH, Fredman B, Smith I, White PF. Sevoflurane versus desflurane for outpatient anesthesia: A comparison of maintenance and recovery profiles. Anesth Analg. 1995;81:1186–90. doi: 10.1097/00000539-199512000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Dupont J, Tavernier B, Ghosez Y, Durinck L, Thevenot A, Moktadir-Chalons N, et al. Recovery after anaesthesia for pulmonary surgery: Desflurane, sevoflurane and isoflurane. Br J Anaesth. 1999;82:355–9. doi: 10.1093/bja/82.3.355. [DOI] [PubMed] [Google Scholar]
- 11.Muzi M, Ebert TJ, Hope WG, Robinson BJ, Bell LB. Site (s) mediating sympathetic activation with desflurane. Anesthesiology. 1996;85:737–47. doi: 10.1097/00000542-199610000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Eger EI, 2nd, Gong D, Koblin DD, Bowland T, Ionescu P, Laster MJ, et al. The effect of anesthetic duration on kinetic and recovery characteristics of desflurane versus sevoflurane, and on the kinetic characteristics of compound A, in volunteers. Anesth Analg. 1998;86:414–21. doi: 10.1097/00000539-199802000-00037. [DOI] [PubMed] [Google Scholar]
- 13.Macario A, Dexter F, Lubarsky D. Meta-analysis of trials comparing postoperative recovery after anesthesia with sevoflurane or desflurane. Am J Health Syst Pharm. 2005;62:63–8. doi: 10.1093/ajhp/62.1.63. [DOI] [PubMed] [Google Scholar]
- 14.Song D, Joshi GP, White PF. Fast-track eligibility after ambulatory anesthesia: A comparison of desflurane, sevoflurane, and propofol. Anesth Analg. 1998;86:267–73. doi: 10.1097/00000539-199802000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Larsen B, Seitz A, Larsen R. Recovery of cognitive function after remifentanil-propofol anesthesia: A comparison with desflurane and sevoflurane anesthesia. Anesth Analg. 2000;90:168–74. doi: 10.1097/00000539-200001000-00035. [DOI] [PubMed] [Google Scholar]
- 16.Chen X, Zhao M, White PF, Li S, Tang J, Wender RH, et al. The recovery of cognitive function after general anesthesia in elderly patients: A comparison of desflurane and sevoflurane. Anesth Analg. 2001;93:1489–94. doi: 10.1097/00000539-200112000-00029. [DOI] [PubMed] [Google Scholar]


