Abstract
Background and purpose —
Even small design modifications of uncemented hip stems may alter the postoperative 3-D migration pattern. The Furlong Active is an uncemented femoral stem which, in terms of design, is based on its precursor—the well-proven Furlong HAC—but has undergone several design changes. The collar has been removed on the Active stem along with the lateral fin; it is shorter and has more rounded edges in the proximal part. We compared the migration patterns of the uncemented Furlong HAC stem and the modified Furlong Active stem in a randomized, controlled trial over 5 years using radiostereometry (RSA).
Patients and methods —
50 patients with primary osteoarthritis were randomized to receive either the HAC stem or the Active stem. The patients underwent repeated RSA examinations (postoperatively, at 3 months, and after 1, 2, and 5 years) and conventional radiography, and they also filled out hip-specific questionnaires.
Results —
During the first 3 months, the collarless Active stem subsided to a greater extent than the collar-fitted HAC stem (0.99 mm vs. 0.31 mm, p = 0.05). There were, however, no other differences in movement measured by RSA or in clinical outcome between the 2 stems. After 3 months, both stem types had stabilized and almost no further migration was seen.
Interpretation —
The Active stem showed no signs of unfavorable migration. Our results suggest that the osseointegration is not compromised by the new design features.
Since the introduction of the Charnley cemented hip stem, it has been emphasized that immediate stability is of great importance for achievement of long-term stem survival (Loudon and Charnley 1980). Nowadays, it is well documented that different design features influence the migration pattern of the stem. Highly polished, collarless cemented stems like the Exeter continuously subside within the cement mantle without compromising the long-term survival of the stem (Stefansdottir et al. 2004, Nieuwenhuijse et al. 2012). Uncemented stems depend on osseointegration to stabilize, and the common perception is that postoperative migration should not be tolerated (Kirk et al. 2007, Demey et al. 2011, Gortchacow et al. 2012). According to several RSA investigations, however, many modern uncemented stems show a small degree of initial migration before osseointegration occurs (Strom et al. 2006a,b, 2007, Campbell et al. 2011).
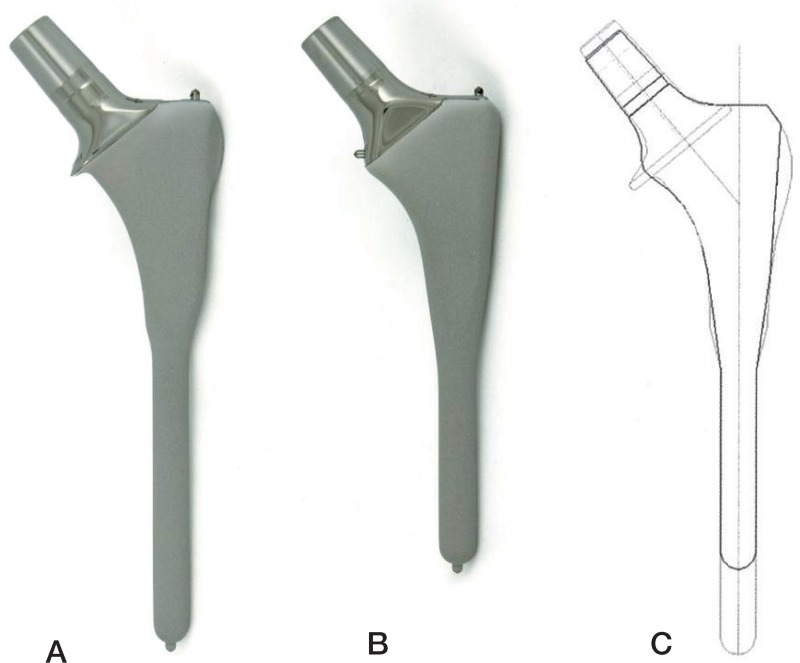
Over the last decade, long-term follow-up has shown good results for the contemporary uncemented stems (McNally et al. 2000, Skinner et al. 2003, Eskelinen et al. 2006, Sharma and Brooks 2006, Gabbar et al. 2008, Rajaratnam et al. 2008, Hailer et al. 2010, Vidalain 2011), including a 99% survival rate for the Furlong HAC stem (JRI Ltd., London, UK) at 13–15 years (Shetty et al. 2005). The design of the Furlong HAC stem has not changed since its introduction in the mid-eighties, but demands for a more modern, shorter and less bulky femoral stem have led to the introduction of a modified version of the Furlong HAC stem with the aim of making it easier to implant: the Furlong Active stem (JRI Ltd, London, UK). From here on, the stems will be referred to as the HAC and the Active. The lateral fin, which was originally designed to improve rotational stability, has been removed. The rationale for this change is the risk of fracturing the trochanter major when using the lateral fin cutter (“breadknife”) in order to make room for the fin. The Active stem has more rounded edges both medially and laterally in the proximal part (Figure 1). Proximally, the Active stem is slightly double-tapered whereas the HAC stem is parallel-sided in the coronal plane. In the AP view, the central section of the stem has more or less remained the same in the form of a cone to provide transfer of body weight under hoop stress. The transition zone from the cone-shaped proximal section to the distal cylindrical section is less distinct in the Active stem, and the distal cylindrical section is shorter. Similarly to the HAC stem, it is made from forged titanium alloy and is vacuum plasma-sprayed with a 200-µm-thick layer of Supravit (150-µm hydroxyapatite ceramic on 50-µm titanium substrate), which provides a high-density coating without metal-to-bone contact.
Figure 1.
A. Furlong HAC. B. Furlong Active, both with tantalum markers. C. Superimposition of outlines (right image).
It is important that the postoperative 3-D migratory pattern is well established before a prosthesis of new or modified design is implanted on a larger scale, thereby reducing the risk of potential future complications for patients (Karrholm et al. 1997). The most accurate radiographic method used to identify early warning signs of prosthesis migration and to predict long-term results with a specific prosthesis is radiostereometry (RSA) (Valstar et al. 2005).
The main goal of our study was to compare the 3-D migration patterns of the Active stem and the well-proven HAC stem using RSA. We wanted to determine if the design changes would have any impact on the migration behavior, influence the osseointegration, and thereby affect the long-term result.
Patients and methods
Study group
50 patients with primary osteoarthritis who were scheduled for total hip arthroplasty (THA) at Skåne University Hospital were recruited for the study. The mean age of the patients was 63 years and their mean BMI was 27 (Table 1). The exclusion criteria were Charnley category C patients and patients with a femoral anatomy which from plain radiographs was considered to be unsuitable for a HAC or Active hip stem. The study was started in April 2007, was completed in April 2013, and it was approved by the Ethics Committee of Lund University, Sweden. Informed written consent was obtained from all patients. The study was carried out according to the Helsinki Declaration of 1975, as revised in 2000.
Table 1.
Patient characteristics
| Variables | HAC | Active | Total |
|---|---|---|---|
| No. of patients | 25 | 25 | 50 |
| Age, years (range) | 63 (49–75) | 62 (50–77) | 63 (49–77) |
| Gender (M; F) | 18; 7 | 9; 16 | 27; 23 |
| BMI (SD) | 26 (3.4) | 29 (5.0) | 27 (4.4) |
The patients were randomized using closed envelopes, which were opened intraoperatively. 2 patients, both in the Active group, were excluded from the study. 1 had poor marker distribution, resulting in a condition number that was too high for the RSA analysis, and the other patient fell 3 weeks postoperatively and sustained a periprosthetic fracture. 2 patients, both in the HAC group, completed the 2-year follow-up but died of cancer before the 5-year follow-up. For these patients, only the results at 0, 3, 12, and 24 months were included in the study. 1 patient in the Active group had poor radiographic quality as a result of obesity at the 5-year follow-up. For this patient, only the results at 0, 3, 12, and 24 months were included in the study. 45 patients (25 men and 20 women) completed the study, which lasted for 5 years.
Surgery
The enrollment of patients and surgery were done by 2 experienced hip surgeons (GF and MS). A posterolateral approach was used. 8–10 well-scattered tantalum bone markers with a diameter of 0.8 mm were implanted in the trochanter major and minor during surgery. The prostheses were pre-marked by the manufacturer with tantalum markers at the tip, shoulder, and medial collar of the stem (Figure 1). The femoral head was used as the fourth marker.
Radiostereometry
All RSA examinations were performed according to the guidelines for standardization of radiostereometry (Valstar et al. 2005). The patients underwent RSA examinations and conventional radiographic examinations on the first postoperative day, before weight bearing, and then at 3, 12, 24, and 60 months with a time tolerance of ± 5% for each examination. For calculation of the precision value, all patients had 1 double examination during the follow-up period (Table 2).
Table 2.
Precision of the RSA measurements a
| Axis | Translation, mm | Rotation, ° |
|---|---|---|
| Transverse (X) | 0.12 | 0.23 |
| Longitudinal (Y) | 0.08 | 0.30 |
| Sagittal (Z) | 0.12 | 0.09 |
a The precision is based on 50 double examinations of the patients in the study. The value given represents the smallest migration that is considered statistically significant and is based on 2 standard deviations of the error obtained. This therefore corresponds to the 95% confidence limit.
An upper limit for the mean error, i.e. the mean difference between the markers in one examination compared to that in another examination, was set at 0.30 mm, with a resulting mean for all examinations of 0.17 mm for the femur and 0.11 mm for the stem. An upper limit for the condition number, which is used for indication of appropriate marker distribution, was set at 120 with a mean for all examinations of 49 for the femur and 32 for the stem. The RSA examinations were performed using a biplanar technique with the patient in the supine position and the calibration cage below the patient. We used UmRSA software for the RSA analysis (version 6.0; RSA Biomedical, Umeå, Sweden) and a type 41 calibration cage (Tilly Medical AB, Lund, Sweden).
We analyzed the segment motion of the stem in relation to the tantalum markers implanted in the femur, and the 3-D movement of the stem could thereby be reconstructed as rotation and translation along the 3 axes in an orthogonal coordinate system. The stem subsidence (Y-translation) and retroversion (Y-rotation) were selected as primary effect variables.
After the first RSA examination was performed, the patients were mobilized with the help of a physiotherapist according to a standardized training program, and they were allowed full weight bearing.
Routine clinical follow-up was performed at 3, 12, 24, and 60 months. Standard radiographic examinations were performed preoperatively, on the first postoperative day, and at 12, 24, and 60 months. The patients had a clinical examination and filled out the self-administered Hip Disability and Osteoarthritis Outcome Score (HOOS) (Nilsdotter et al. 2003) before surgery and at 12, 24, and 60 months.
Statistics
Known data suggest a difference in mean distal migration of 0.25 mm, and posterior rotation of 0.5 degrees may be clinically significant. With 25 patients in each group, with the use of data in the literature and expected standard deviations, and with an α-value of 0.05, the study would have power of more than 90% to detect differences in migration of > 0.1 mm. Thus, 50 patients were included in the study, with 25 in each group. To compare differences between groups at any given time, Student’s t-test was used. All results are given as signed values for migration. Friedman’s test was used to analyze migration over time in each group. For analysis of the outcome questionnaire (HOOS), we used the Mann-Whitney U-test.
We used IBM SPSS statistics software version 21.0 and any p-value < 0.05 was considered significant.
Results
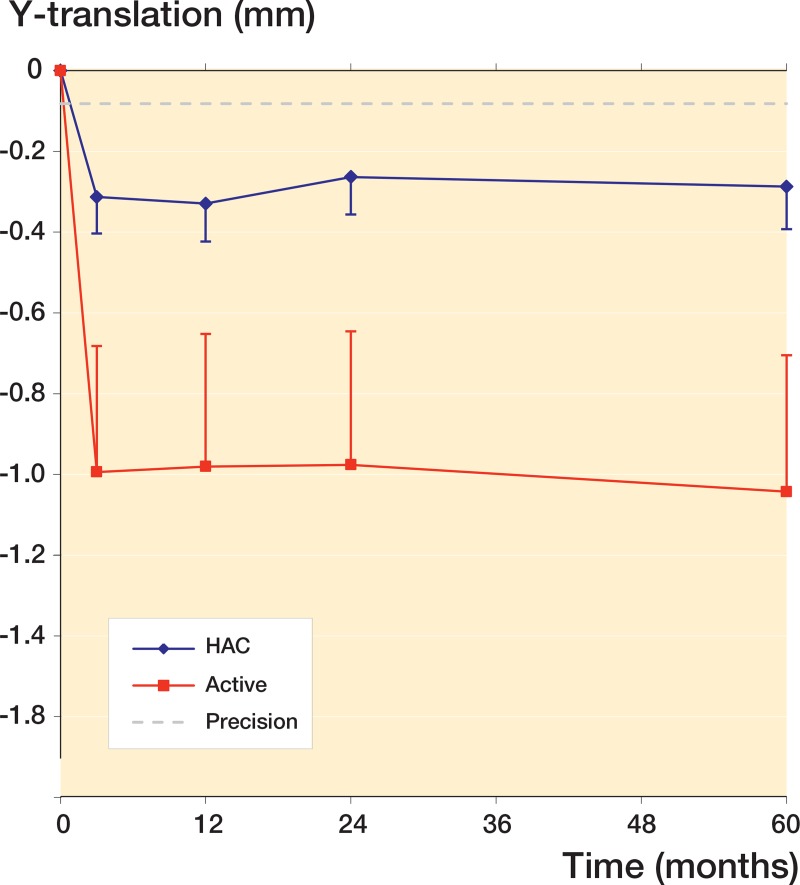
The overall migration measured with RSA for both stem types along the 3 cardinal axes was small (Table 3). The mean subsidence during the first 3 months was 0.31 mm for the Furlong HAC stem and it was 0.99 mm for the Furlong Active stem (p = 0.046, 95% CI: 0.013–1.35) (Figure 2). In the interval between 3 months and 5 years, looking at the subsidence of each stem type separately, no statistically significant migration was seen for either the HAC stem (p = 0.06) or the Active stem (p = 0.5).
Table 3.
Stem translation and rotation at 3 months, 1 year, 2 years, and 5 years
| 3 Months |
12 months |
24 months |
60 months |
|||||
|---|---|---|---|---|---|---|---|---|
| Type of motion | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | Mean | 95% CI |
| Stem translation, segment motion, mm | ||||||||
| Y-translation a | ||||||||
| HAC | –0.31 | –0.50 to –0.13 | –0.33 | –0.52 to –0.14 | –0.26 | –0.46 to –0.07 | –0.29 | –0.51 to –0.07 |
| Active | –0,99 | –1.64 to –0.35 | –0.98 | –1.66 to –0.30 | –0.98 | –1.66 to –0.29 | –1.04 | –1.75 to –0.34 |
| X-translation | ||||||||
| HAC | 0.04 | –0.04 to 0.12 | 0.04 | –0.05 to 0.13 | 0.07 | –0.02 to 0.15 | 0.07 | –0.02 to 0.17 |
| Active | –0.10 | –0.38 to 0.17 | –0.09 | –0.37 to 0.20 | –0.08 | –0.35 to 0.18 | –0.08 | –0.38 to 0.21 |
| Z-translation | ||||||||
| HAC | –0.22 | –0.33 to –0.11 | –0.21 | –0.32 to –0.09 | –0.13 | –0.27 to 0.00 | –0.19 | –0.32 to –0.05 |
| Active | –0.22 | –0.49 to 0.05 | –0.15 | –0.42 to 0.11 | –0.18 | –0.46 to 0.10 | –0.22 | –0.51 to 0.07 |
| Stem rotation, segment motion, degrees | ||||||||
| Y-rotation b | ||||||||
| HAC | 0.80 | 0.38 to 1.22 | 0.80 | 0.37 to 1.23 | 0.92 | 0.53 to 1.32 | 0.86 | 0.41 to 1.30 |
| Active | 1.18 | 0.44 to 1.93 | 1.28 | 0.47 to 2.09 | 1.26 | 0.46 to 2.05 | 1.32 | 0.48 to 2.16 |
| X-rotation | ||||||||
| HAC | –0.07 | –0.20 to 0.07 | –0.08 | –0.25 to 0.09 | –0.25 | –0.41 to –0.10 | –0.15 | –0.37 to 0.07 |
| Active | 0.02 | –0.17 to 0.21 | –0.22 | –0.39 to –0.04 | –0.23 | –0.42 to–0.04 | –0.22 | –0.37 to –0.07 |
| Z-rotation | ||||||||
| HAC | –0.19 | –0.32 to –0.06 | –0.22 | –0.34 to –0.09 | –0.22 | –0.34 to –0.10 | –0.25 | –0.40 to –0.09 |
| Active | –0.28 | –0.59 to 0.03 | –0.29 | –0.63 to 0.05 | –0.30 | –0.64 to 0.03 | –0.32 | –0.68 to 0.04 |
a proximal (+), distal (–)
b retroversion (+)
Figure 2.
Graph showing the mean stem subsidence for the HAC and Active stems, with SEM bars. The p-values for the difference in mean subsidence were 0.05 at 3 months, 0.07 at 1 year, 0.05 at 2 years, and 0.04 at 5 years.
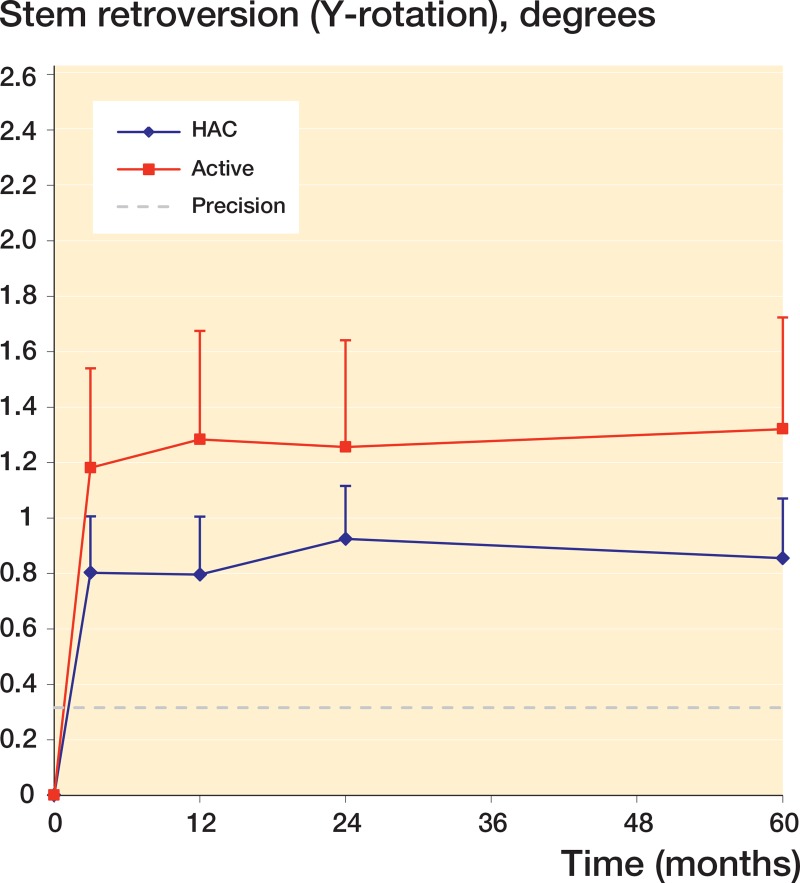
The stems had an initial retroversion during the first 3 months with a mean of 0.80 degrees for the HAC stem and 1.18 degrees for the Active stem (p = 0.4, 95% CI: –1.22 to 0.46) (Figure 3).
Figure 3.
Graph showing stem retroversion (°) for both stems, with SEM bars. The difference in retroversion between the 2 stems was not significantly different at any time point (p = 0.4 at 3 months, p = 0.3 at 1 year, p = 0.5 at 2 years, and p = 0.3 at 5 years).
In the interval between 3 months and 5 years, looking at the retroversion of each stem type separately, no statistically significant retroversion was seen for either the HAC stem (p = 0.1) or the Active stem (p = 0.1).
1 extreme outlier regarding subsidence was noticed in the Active group: the subsidence was 6.5 mm during the first 3 months. Thereafter, no further subsidence was seen. The BMI of this patient was 41. If we excluded this patient from the material, the difference between the groups regarding subsidence would no longer be statistically significant at 3 months (p > 0.05). 2 patients were found to have a more pronounced retroversion over the first 3 months, one in each group. The retroversion for these patients was 4.2° (HAC) and 5.1° (Active), but between 3 months and 5 years, no further retroversion was seen for either of these stems. No stems were considered to be loose from a clinical or standard radiographic standpoint during the follow-up period.
The HOOS values were similar in both groups preoperatively and at 12, 24, and 60 months of follow-up, with no statistically significant difference between the groups. As expected, when comparing preoperative and postoperative scores, HOOS values improved significantly for both stems.
Discussion
We found only minor differences in the 3-D migration patterns of the Active stem and the HAC stem, and the migration of both stems was confined to the first 3 postoperative months. The Active stem subsided to a greater extent than the HAC stem during the first 3 months, but thereafter no further subsidence was seen, suggesting that the osseointegration was not compromised by the early subsidence. The pattern of subsidence seen for the Active stem was similar to the pattern of subsidence observed in RSA studies with other uncemented collarless prostheses with excellent long-term results, for example the Cone stem (Strom et al. 2006b), the CLS stem (Strom et al. 2007), and the Corail stem (Campbell et al. 2011, Faisal et al. 2011).
With the RSA technique, we could accurately determine the rotational patterns of the stems. The lateral fin on the HAC stem is thought to provide rotational stability. In spite of the fact that the fin was removed on the Active stem, we found no differences between the HAC stem and the Active stem at any time point during the follow-up regarding retroversion, and the pattern of retroversion was similar to that for other uncemented stems (Strom et al. 2006b, 2007, Campbell et al. 2011).
There is a substantial variability in the initial stem subsidence between patients, which was evident not only in our study, but also in other contemporary collarless stems studied (Strom et al. 2006a,b, 2007, Simpson et al. 2010, Campbell et al 2011, Schewelov et al. 2012). There has been much speculation about the cause of this variability, for example, the quality of initial stem fixation and bone quality. Caution should be exercised in predicting long-term results exclusively based on the magnitude of initial subsidence if it is followed by early stabilization (Campbell et al. 2011). We believe that a minor degree of early migration within the first few months, during the “settling in” period, is not a sign of inferior osseointegration for a contemporary, collarless, uncemented stem. Regarding subsidence, we recorded 1 extreme outlier, belonging to the Active group. This was an obese patient with subsidence of 6.5 mm during the first 3 months. One could speculate that the amount of press fit during implantation was insufficient and/or that the force of axial compression had led to the additional stem subsidence for this specific patient. This stem also stabilized after 3 months, and after that no further subsidence was seen up to 5 years.
1 patient in the Active group fell 3 weeks after surgery and had a periprosthetic fracture. It has previously been postulated that tapered collarless prostheses could increase the risk of periprosthetic fractures. This is mainly documented for cemented prostheses (Franklin and Malchau 2007). According to Demey et al. (2011), the axial force required to achieve a fracture is lower for collarless prostheses than for collared prostheses, and one cannot deny the fact that this fracture may be related to the design of the Active stem, being a collarless, tapered stem. According to the Swedish Hip Register (2011), the risk of a periprosthetic fracture is increased for uncemented prostheses in general and possibly collarless prostheses in particular, but the incidence appears to decrease after osseointegration.
Simpson et al. (2010) published a study similar to ours, but with 2-years follow-up, and stated that the subsidence of the HAC stem was approximately one-third of that of the Active stem during the first year. They suggested that the early migration might compromise effective osseointegration and thereby the long-term performance of the stem. In their study, the first follow-up RSA examination was performed at 6 months postoperatively whereas ours was done at 3 months. The results at 12 and 24 months from these 2 studies look very similar, but we were able to determine that the migration occurs already within the first 3 months after surgery, and that no further retroversion or subsidence was apparent in the time interval of 3 months to 5 years. Our study supports the actual results of Simpson et al. (2010), but we do not support their interpretation of these results. The design features of an uncemented prosthesis will influence the pattern of movement before osseointegration is complete.
Complete stability directly after implantation has previously been thought to be important, but as long as the initial migration is small and the stem stabilizes and osseointegrates within reasonable time after surgery, the long-term result is apparently not influenced. Continuous migration, on the other hand, is thought to compromise long-term survival of an uncemented prosthesis, and should therefore not be tolerated. It has been postulated that early migration might affect the functional outcome in terms of risk of dislocation, leg length discrepancy, and pain (Demey et al. 2011), but a minor subsidence does not apparently compromise the functional outcome based on the fact that many contemporary uncemented collarless stems show an initial subsidence and/or retroversion with very good clinical results.
The initial migration pattern of the HAC stem could be compared to the migration pattern of cemented prostheses where the design (i.e the collar, cone, and/or specific geometric shape) provides an immediate stability, known as “shape closed” (Bottner et al. 2005) for cemented prostheses. The movement pattern of the Active stem, however, is more similar to that of the expression “force closed” in cemented prostheses. Here, the prosthesis is designed to migrate into the cement mantle—or in the case of an uncemented prosthesis, to “settle in” under the force of rotation and axial compression—to the position that it will be osseointegrated in. The amount of migration before osseointegration is thought to be influenced by the amount of press fit, stem positioning during surgery, stem size in relation to femur size, the shape of the femur, the presence or absence of osteoporosis, stem geometry and coating, and external factors such as postoperative axial compression and rotation (Bottner et al. 2005, Campbell et al. 2011).
In conclusion, the Active stem behaves like many other contemporary, collarless uncemented prostheses in terms of migration.
Acknowledgments
Recruitment of patients and operations was done by GF and MS. The data were analyzed by EW, GF, and MS. The paper was written by EW and reviewed by GF and MS.
We thank Håkan Leijon of the RSA laboratory in Lund, Skåne University Hospital, for help in computerizing the RSA pictures and data, and Phillipe Wagner, Statistician, RC Syd, Clinical Sciences, Skåne University Hospital for statistical advice.
JRI Ltd. sponsored the RSA examinations in this study, but did not take part in planning, data collection, analysis, interpretation of the results, or in writing of the manuscript. Otherwise, no benefits have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- Bottner F, Su E, Nestor B, Azzis B, Sculco TP, Bostrom M. Radiostereometric analysis: the hip . HSS J. 2005;1(1):94–9. doi: 10.1007/s11420-005-0114-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell D, Mercer G, Nilsson KG, Wells V, Field JR, Callary SA. Early migration characteristics of a hydroxyapatite-coated femoral stem: an RSA study . Int Orthop. 2011;35(4):483–8. doi: 10.1007/s00264-009-0913-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demey G, Fary C, Lustig S, Neyret P, si Selmi T. Does a collar improve the immediate stability of uncemented femoral hip stems in total hip arthroplasty? A bilateral comparative cadaver study . J Arthroplasty. 2011;26(8):1549–55. doi: 10.1016/j.arth.2011.03.030. [DOI] [PubMed] [Google Scholar]
- Eskelinen A, Remes V, Helenius I, Pulkkinen P, Nevalainen J, Paavolainen P. Uncemented total hip arthroplasty for primary osteoarthritis in young patients: a mid-to long-term follow-up study from the Finnish Arthroplasty Register . Acta Orthop. 2006;77(1):57–70. doi: 10.1080/17453670610045704. [DOI] [PubMed] [Google Scholar]
- Faisal M, Thomas G, Young SK. Subsidence of the Corail femoral component in the elderly. A retrospective radiological review . Hip Int. 2011;21(3):325–9. doi: 10.5301/HIP.2011.8409. [DOI] [PubMed] [Google Scholar]
- Franklin J, Malchau H. Risk factors for periprosthetic femoral fracture . Injury. 2007;38(6):655–60. doi: 10.1016/j.injury.2007.02.049. [DOI] [PubMed] [Google Scholar]
- Gabbar OA, Rajan RA, Londhe S, Hyde ID. Ten- to twelve-year follow-up of the furlong hydroxyapatite-coated femoral stem and threaded acetabular cup in patients younger than 65 years . J Arthroplasty. 2008;23(3):413–7. doi: 10.1016/j.arth.2007.01.027. [DOI] [PubMed] [Google Scholar]
- Gortchacow M, Wettstein M, Pioletti DP, Muller-Gerbl M, Terrier A. Simultaneous and multisite measure of micromotion, subsidence and gap to evaluate femoral stem stability . J Biomech. 2012;45(7):1232–8. doi: 10.1016/j.jbiomech.2012.01.040. [DOI] [PubMed] [Google Scholar]
- Hailer NP, Garellick G, Karrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish Hip Arthroplasty Register . Acta Orthop. 2010;81(1):34–41. doi: 10.3109/17453671003685400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karrholm J, Herberts P, Hultmark P, Malchau H, Nivbrant B, Thanner J. Radiostereometry of hip prostheses. Review of methodology and clinical results . Clin Orthop. 1997;344:94–110. [PubMed] [Google Scholar]
- Kirk KL, Potter BK, Lehman RA, Jr., Xenos JS. Effect of distal stem geometry on interface motion in uncemented revision total hip prostheses . Am J Orthop (Belle Mead NJ) 2007;36(10):545–9. [PubMed] [Google Scholar]
- Loudon JR, Charnley J. Subsidence of the femoral prosthesis in total hip replacement in relation to the design of the stem . J Bone Joint Surg (Br) 1980;62(4):450–3. doi: 10.1302/0301-620X.62B4.7430222. [DOI] [PubMed] [Google Scholar]
- McNally SA, Shepperd JA, Mann CV, Walczak JP. The results at nine to twelve years of the use of a hydroxyapatite-coated femoral stem . J Bone Joint Surg (Br) 2000;82(3):378–82. doi: 10.1302/0301-620x.82b3.10114. [DOI] [PubMed] [Google Scholar]
- Nieuwenhuijse MJ, Valstar ER, Kaptein BL, Nelissen RG. The Exeter femoral stem continues to migrate during its first decade after implantation: 10-12 years of follow-up with radiostereometric analysis (RSA) . Acta Orthop. 2012;83(2):129–34. doi: 10.3109/17453674.2012.672093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nilsdotter AK, Lohmander LS, Klassbo M, Roos EM. Hip disability and osteoarthritis outcome score (HOOS)—validity and responsiveness in total hip replacement . BMC Musculoskelet Disord. 2003;4:10. doi: 10.1186/1471-2474-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajaratnam SS, Jack C, Tavakkolizadeh A, George MD, Fletcher RJ, Hankins M, et al. Long-term results of a hydroxyapatite-coated femoral component in total hip replacement: a 15- to 21-year follow-up study . J Bone Joint Surg (Br) 2008;90(1):27–30. doi: 10.1302/0301-620X.90B1.19731. [DOI] [PubMed] [Google Scholar]
- Schewelov T, Ahlborg H, Sanzen L, Besjakov J, Carlsson A. Fixation of the fully hydroxyapatite-coated Corail stem implanted due to femoral neck fracture . Acta Orthop. 2012;83(2):153–8. doi: 10.3109/17453674.2011.641107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma DK, Brooks S. Long-term follow-up (11 years plus) results of JRI (Furlong) total hip arthroplasty in young patients: cause for concern regarding acetabular cup? . Int Orthop. 2006;30(5):375–80. doi: 10.1007/s00264-006-0083-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shetty AA, Slack R, Tindall A, James KD, Rand C. Results of a hydroxyapatite-coated (Furlong) total hip replacement: a 13- to 15-year follow-up . J Bone Joint Surg (Br) 2005;87(8):1050–4. doi: 10.1302/0301-620X.87B8.16011. [DOI] [PubMed] [Google Scholar]
- Simpson DJ, Kendrick BJ, Hughes M, Glyn-Jones S, Gill HS, Rushforth GF, et al. The migration patterns of two versions of the Furlong cementless femoral stem: a randomised, controlled trial using radiostereometric analysis . J Bone Joint Surg (Br) 2010;92(10):1356–62. doi: 10.1302/0301-620X.92B10.24399. [DOI] [PubMed] [Google Scholar]
- Skinner JA, Kroon PO, Todo S, Scott G. A femoral component with proximal HA coating. An analysis of survival and fixation at up to ten years . J Bone Joint Surg (Br) 2003;85(3):366–70. doi: 10.1302/0301-620x.85b3.13054. [DOI] [PubMed] [Google Scholar]
- Stefansdottir A, Franzen H, Johnsson R, Ornstein E, Sundberg M. Movement pattern of the Exeter femoral stem; a radiostereometric analysis of 22 primary hip arthroplasties followed for 5 years . Acta Orthop Scand. 2004;75(4):408–14. doi: 10.1080/00016470410001169-1. [DOI] [PubMed] [Google Scholar]
- Strom H, Huss K, Larsson S. Unrestricted weight bearing and intensive physiotherapy after uncemented total hip arthroplasty . Scand J Surg. 2006a;95(1):55–60. doi: 10.1177/145749690609500111. [DOI] [PubMed] [Google Scholar]
- Strom H, Kolstad K, Mallmin H, Sahlstedt B, Milbrink J. Comparison of the uncemented Cone and the cemented Bimetric hip prosthesis in young patients with osteoarthritis: an RSA, clinical and radiographic study . Acta Orthop. 2006b;77(1):71–8. doi: 10.1080/17453670610045713. [DOI] [PubMed] [Google Scholar]
- Strom H, Nilsson O, Milbrink J, Mallmin H, Larsson S. The effect of early weight bearing on migration pattern of the uncemented CLS stem in total hip arthroplasty . J Arthroplasty. 2007;22(8):1122–9. doi: 10.1016/j.arth.2006.11.015. [DOI] [PubMed] [Google Scholar]
- Valstar ER, Gill R, Ryd L, Flivik G, Borlin N, Karrholm J. Guidelines for standardization of radiostereometry (RSA) of implants . Acta Orthop. 2005;76(4):563–72. doi: 10.1080/17453670510041574. [DOI] [PubMed] [Google Scholar]
- Vidalain JP. Twenty-year results of the cementless Corail stem . Int Orthop. 2011;35(2):189–94. doi: 10.1007/s00264-010-1117-2. [DOI] [PMC free article] [PubMed] [Google Scholar]