Abstract
Background and purpose —
The incidence of forearm shaft fractures in children has increased and operative treatment has increased compared with nonoperative treatment in recent years. We analyzed the long-term results of nonoperative treatment.
Patients and methods —
We performed a population-based age- and sex-matched case-control study in Vaasa Central Hospital, concerning fractures treated in the period 1995–1999. There were 47 nonoperatively treated both-bone forearm shaft fractures, and the patients all participated in the study. 1 healthy control per case was randomly selected and evaluated for comparison. We analyzed clinical and radiographic outcomes of all fractures at a mean of 11 (9–14) years after the trauma.
Results —
The main outcome, pronosupination of the forearm, was not decreased in the long term. Grip strength was also equally as good as in the controls. Wrist mobility was similar in flexion (85°) and extension (83°) compared to the contralateral side. The patients were satisfied with the outcome, and pain-free. Radiographally, 4 cases had radio-carpal joint degeneration and 4 had a local bone deformity.
Interpretation —
The long-term outcome of nonoperatively treated both-bone forearm shaft fractures in children was excellent.
Forearm shaft fractures constitute about 6% of all children’s fractures (Landin. 1997) and their incidence is increasing (Sinikumpu et al. 2012b). Closed reduction has traditionally been considered a satisfactory treatment in most cases of forearm shaft fracture (Price 2010). There is little consensus concerning the amount of deformity as an indication for surgery (Annan and Moran 2006, Zlotolow 2012). However, the use of surgery has increased by 60% in recent years (Cheng et al. 1999, Helenius et al. 2009). The increasing interest in operative treatment has been justified by a 2-fold greater rate of immediate complications after nonoperative treatment than after operative treatment (Sinikumpu et al. 2012a). The main complications include redisplacement, refracture, delayed union, compartment syndrome, deep infection, neurovascular injury, residual deformation, and loss of mobility (Flynn et al. 2010, Sinikumpu et al. 2012a). In the long term, loss of rotation is the most important complication (Franklin et al. 2012).
In this case-control study, we investigated late-stage morbidity in cases of both-bone forearm shaft fractures in children after nonoperative treatment. We hypothesized that there would be late morbidity after nonoperative treatment that could justify the recent increased trend towards operative treatment.
Patients and methods
Population-based material catchment
All children (< 16 years of age) with a both-bone forearm fracture in 1995–1999 in a defined geographic area served by Vaasa Central Hospital were initially selected for the study from the computerized hospital database. There are no other trauma centers in the area. 220 patients of 253 were still living in the district, and their original radiographs were reviewed by an experienced radiologist. 49 cases were confirmed to have sustained a two-bone shaft fracture. The shaft was defined as the long tubular bone between the proximal and distal metaphyses (Slongo et al. 2007). All but 2 cases had been treated with closed reduction and casting, without any internal fixation. These 47 cases participated in the study. 4 cases of the 220 had had no fracture at all, and 167 cases were excluded for other reasons (single-bone fracture, distal/proximal fractures beyond metadiaphyseal junctions, fracture luxation, or pathological fracture). For each of the 47 patients who participated, 1 age- and sex-matched control case was included. Control cases were randomly selected from the population living in the study area, via the Finnish Population Register Center. On average, 3 potential control cases per study case were invited to take part in the study, in order to achieve the required number of control cases (47). An age difference of half a year was allowed between the fracture cases and the control cases at the time of the follow-up visit.
Patient characteristics
Half of the children were boys. The mean age at the time of injury was 8.5 (3–16) years. It was 8.6 years in boys and 8.2 in girls. 37 of the fractures had occurred on the non-dominant side. No bilateral fractures were seen. At admission, 1 open fracture (Gustilo-Anderson grade I) was noted. No compartment syndrome was seen. In the radiographs, half of the fractures (25) showed angular deformity of over 15°, 9 showed angular deformity of 0–15°, and 13 showed no angular deformity originally. The mean ages of the children were similar in these 3 groups. Over 2 mm of displacement was seen in 15 patients. 32 patients showed < 2 mm of displacement originally. 2 fractures were segmental. All the patients included were treated nonoperatively, according to the inclusion criterion. 26 were treated at the operating theater (OT) and 21 were treated at the emergency room or during an outpatient visit. In 5 cases, closed re-reduction was carried out during short-term follow-up. Their mean age was 7.2 (3–13) years. No cases were surgically fixed during short-term follow-up. The mean immobilization time was 24 (14–36) days. On average, there were 2.3 (0–6) follow-up visits after the injury.
Assessment of outcome and statistical methods
Outcome was determined at outpatient visits in 2009–2012, at a mean of 11 (9–14) years after the trauma. Controls were investigated in a similar manner to the fracture cases, except for radiographic examination. The patients and controls were evaluated by the same investigators. Rotation was taken to be the main outcome feature of the study (Franklin et al. 2012). Normally, supination range of motion is around 90° and pronation 80° in a population corresponding to the age of the cases in the study cohort (Soucie et al. 2011). A decrease of ≥ 30° in supination or pronation was classified as an unsatisfactory result (Flynn et al. 2010). Forearm rotation was compared with that in the control case. Ranges of motion (ROMs) were estimated using a goniometer. In the examination, the subjects were sitting, adducting arms to the trunk and elbows in 90o of flexion. The forearms were in a neutral position with the thumbs upwards. Wrist motions were compared with those on the contralateral side, following the established practice of using the uninjured extremity as a control (Daruwalla 1979, Goldfarb et al. 2005, Kang et al. 2011). ROM in the wrist and grip strength were measured and analyzed as continuous variables. Strength was measured by using a hydraulic Jamar gauge. The highest of 3 attempts was recorded. The fracture cases were asked about satisfaction, tolerance of physical activity and work, need for analgesics, and cold sensitivity.
Late-stage radiographs were taken in anteroposterior and lateral projections. Signs of radio-carpal joint degeneration (osteophytes, cysts at the joint level, or decreased joint space) were recorded. Furthermore, alignment, other residual bone deformity, heterotrophic ossification, and cross-union between the radius and ulna were assessed. Radial bowing of < 5° or > 15° in the anteroposterior radiographs was considered to represent malalignment (Sage 1959). The bow was determined by measuring the highest visible angular curve of the shafts. Rotational movement of the forearm is dependent on the shape of the radius, the distal part of which swings about the ulna, allowing rotation of the wrist and hand (Firl and Wunsch 2004). The styloid of the radius and the biceps tuberosity are normally orientated about 180° away from each other (Mehlman and Wall 2006). We aimed to recognize visually whether there was substantial rotational malformation (> 30°).
This was a population-based study. All of the nonoperatively treated children in the hospital district in the given time period were requested to attend a follow-up visit. Post hoc power analysis was performed in order to ensure that the study population was large enough and thus fit for the purpose. The calculation was based on the normal range of rotation (mean 170° with a standard deviation of 30°) in the forearm. More than 30° of a decrease in pronation or supination was considered to be clinically significant (Flynn et al. 2010). Type-I error was set at 0.05 (p-value). The final sample size of 47 would achieve 100% power. Statistically significant differences in long-term outcomes between the fracture cases and the control cases were assessed by using the paired t-test for continuous variables, McNemar’s test for dichotomous variables, and the signed-rank test for ordinal variables. Statistical analyses were carried out using IBM SPSS software version 20. The threshold of statistical significance was set at p < 0.05.
Ethics
The Ethics Committee of Vaasa Central Hospital evaluated and approved the study plan in advance (§2008-05-26). The study was performed according to the Helsinki Declaration of 1983. Informed consent was obtained from every case and every control before inclusion.
Results
Range of pronosupination
Range of pronosupination was similar in cases and controls. Loss of pronosupination of > 30˚ did not occur (Table 1).
Table 1.
Range of motion and grip strength in the upper limbs in fracture cases and controls
| Fractures n = 47 |
Controls
a
n = 47 |
||||||
|---|---|---|---|---|---|---|---|
| mean (SD) | n b (% of all) | mean (SD) | n b (% of all) | Difference | 95% CI | p-value | |
| Diminished rotation c | 0 (0%) | 4 (9%) | –9 | -21 to 0.6 | 0.1 | ||
| Flexion of wrist (°) d | 84.9 (5.1) | 85.1 (5.3) | 0.4 | -0.9 to 0.5 | 0.6 | ||
| Extension of wrist (°) d | 82.9 (10.3) | 82.9 (10.5) | 2.1 | -0.6 to 0.6 | 1.0 | ||
| Grip strength (kg) e | 43.9 (16.0) | 43.9 (14.3) | 1.3 | -2.5 to 2.5 | 1.0 | ||
| Ulnar deviation (°) d | 52.7 (10.0) | 42.9 (9.7) | 9.8 | 6.7 to 13.0 | < 0.001 | ||
Age and sex related matched control case is used in comparison for motion, grip strength and ulnar deviation. The corresponding finding at the contralateral side is used as control for wrist motions in flexion and extension.
Number of cases with poor rotation (< 60° of supination and/or < 50° of pronation) with correlated marginal proportions.
Difference in marginal proportions between age- and gender-matched fracture-control pairs with 95% confidence interval (95% CI) and p-value with McNemar test.
Continuous variables analyzed via means and standard deviations (SD). Difference in means between fracture side and contralateral side with 95% CI and p-value of paired t-test.
Measured with a hydralic Jamar gauge (Asimow Engineering, Santa Monica, CA, USA). Differences in means between age- and gender-matched fracture-control pairs with 95% CI and p-value of paired t-test for grip strength.
Wrist movement
There was no difference in maximal wrist flexion (85˚) between the injured and uninjured sides. No difference was seen in extension (83˚) between the injured and uninjured sides. The findings were similar regarding the right and left sides in both the fracture cases and the control cases. The range of flexion in the wrist was 15% greater (p < 0.001) and extension was 24% greater (p < 0.001) in the cases than in the controls. The findings for both the injured and uninjured forearms were similar in the cases and the controls. In addition, the fracture cases had a greater range of motion (53°) in the wrist from neutral position to maximal ulnar deviation than did the controls (43°) (p < 0.001) (Table 1).
Grip strength
Grip strength was similar in the fracture cases and the controls. It was also similar on the injured and uninjured sides (Table 1).
Other clinical findings
A crackling sound or sensation during rotation of the forearm was found in 8 cases and in 1 control (p = 0.04). 6 of these 8 patients had suffered from a fracture with ≥ 15° of malangulation originally. Tenderness was found in 4 fracture cases but not in any of the control cases (p = 0.1). 1 visible deformity was recognized in a fracture case (p = 1.0). No inequality in the length of the forearms, no weakness in radial artery pulsation, no disturbance in capillary perfusion, and no reduced flexion of the fingers was found in the fracture cases. Radial nerve, median nerve, and ulnar nerve function was normal in all fracture cases and control cases (Table 2).
Table 2.
Subjective symptoms and abnormal findings in patients at follow-up
| Pairs a | Fractures | Controls | 95% CI b | p-value c | |
|---|---|---|---|---|---|
| Subjective symptoms | |||||
| Decreased tolerance of physical activity | 47 | 10 | 3 | -0.3 to 30 | 0.09 |
| Any symptom disturbing work/recreation | 47 | 6 | 4 | -9.9 to 18 | 0.8 |
| Clinical findings | |||||
| Tenderness | 43 | 4 | 0 | -0.6 to 22 | 0.1 |
| Crepitus | 43 | 8 | 1 | 2.6 to 31 | 0.04 |
| Visible deformation of forearm | 45 | 1 | 0 | -5.9 to 12 | 1 |
Number of pairs analyzed with available information.
95% confidence interval (95% CI) of proportional differences bewteen the cases and the controls.
McNemar test.
Subjective symptoms
10 patients and 3 controls suffered from reduced physical activity as a result of symptoms in the fractured forearm (p = 0.09). Unspecific forearm symptoms that disturbed work/recreation were reported by 6 fracture cases and 4 control cases (p = 0.8). Cold sensitivity, sensory functions, need for analgesics, and dissatisfaction were similar between the fracture cases and the control cases (Table 2).
Radiographic outcome
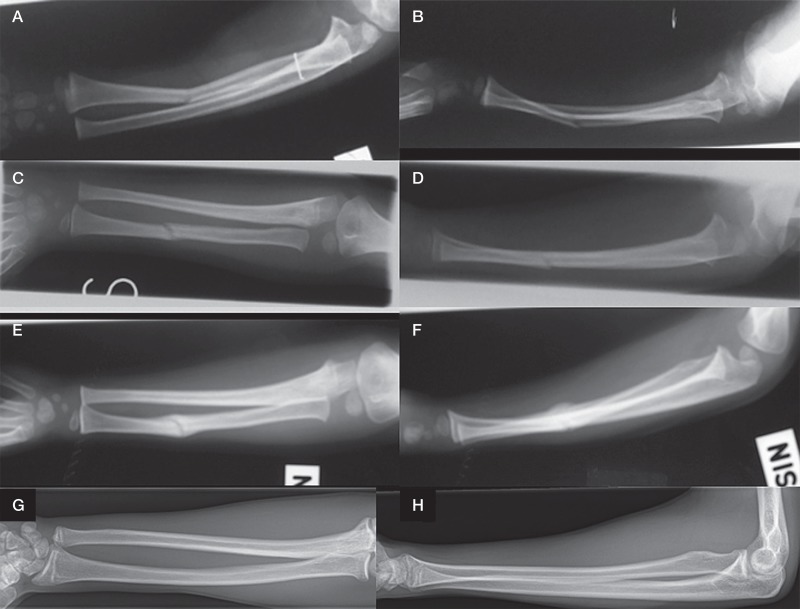
4 patients had osteophytes, cysts at the joint level, or reduced joint space in the radio-carpal area. 3 of these 4 had had a fracture with ≥ 15° angular deformity initially. No abnormality (< 5° or ≥ 15°) in radial shaft bowing was noted as a sign of residual angular malformation (Figure 1). 4 patients showed residual deformity (local bone thickening) of the radius or ulna in radiographs. No rotational disturbance (> 30°) was recognized. There was no radio-ulnar cross-union or heterotrophic ossification visible in the follow-up films.
Figure 1.
An illustrative series of radiographs taken from a case who participated in the study. A 4-year-old boy suffered from a left-side both-bone forearm shaft fracture in the middle third. A. and B. There was a greenstick fracture in the radius and plastic bowing in the ulnar shaft. C. and D. 3 weeks after closed reduction and cast immobilization, the forearm presented good alignment in 2 directions. Slight malalignment remained in the bowed ulna. E. and F. 6 weeks after the injury, free mobilization was allowed. However, worsening alignment with both posterior and radial angular curvatures in the radius was seen (panel F). G. and H. Long-term radiographs 11 years after the injury show good alignment without any other bone complication. The remaining lateral bowing of the radius does not exceed 15° and is consistent with anatomic variation (panel G).
Effect of age
Age of the patients (children < 9 and ≥ 9 years of age at the time of trauma) did not affect clinical and radiographic outcome. Crepitus was no more common in the cases than in the controls, as the age groups were analyzed separately.
Discussion
We found excellent 11-year outcome of nonoperatively treated both-bone forearm shaft fractures in children. These results were achieved with a short casting time (mean 24 (14–36) days) with a low risk of re-reduction. Our findings do not support the recent increasing trend towards surgery. We found no restriction in pronosupination, as reported previously (Hogstrom et al. 1976, Daruwalla 1979). Furthermore, it has even been suspected that poor results of forearm shaft fractures in children may be under-reported (Kay et al. 1986).
Crepitus in the forearm was more common in the fracture group than in the control group. This may reflect changed congruence and incipient osteoarthritis in the radio-carpal joint. However, it is unclear whether this particular finding was relevant, as there was no difference in tenderness, need for analgesics, or tolerance of exercise between cases with and without crepitus.
We found greater wrist motility in the fracture cases than in the controls. It has been pointed out that higher ROM in the injured wrist may reflect a risk factor for fractures rather than being a late-stage consequence of fractures (Nork et al. 1999). Accordingly, we believe that existing bilateral wrist hypermobility in the fracture cases would have remained undetected until bone fracture, because few children with hypermobility have symptoms (Foster and Cabral 2006). In addition, there may be confounding factors—such as sports—that could explain the relationship between hypermobility and increased risk of fracture: child athletes who are physically active in various sports such as soccer show both increased fracture risk and a high prevalence of hypermobility (Konopinski et al. 2012). Repeated progressive stretch training increases ROM in the joints (Konopinski et al. 2012).
The present study had some weaknesses, the limited sample size (n = 47) being the most important. However, according to the results of post hoc power analysis, the study still had excellent power for its purpose. The original clinical evaluation at the time of injury did not follow any consistent pattern; nor was a common strategy of fracture treatment available at the time of the initial trauma. Elastic stable intramedullary nailing (ESIN) was not an established method in the study center in the period 1995–1999, and for this reason a comparative study between nonoperatively and operatively treated fractures would not have been practicable. During the study period (1995–1999) there were just 2 both-bone forearm shaft fractures that were primarily treated operatively. However, the incidence of plate and screw fixation has remained stable: we have previously demonstrated a 5% incidence of plating of both-bone forearm shaft fractures in Finland in 1997–2009 (Sinikumpu et al. 2013b). We also found that the incidence of ESIN increased from 10% to 30% from 1997 to 2009. In our opinion, the main reason for the increase in ESIN is its good immediate outcome and the lack of major short-term complications compared with nonoperative treatment (Kay et al. 1986, Salonen et al. 2012, Sinikumpu et al. 2012a, Colaris et al. 2013). The technique is trendy, and a new method based on biodegradable intramedullary nailing has been described (Sinikumpu et al. 2013a). Despite its popularity, the indications for ESIN are still controversial (Abraham et al. 2011). It has been suggested that indications should include open fractures, failure of closed treatment, fractures with adjacent joint dislocation or severe soft-tissue damage, compartment syndrome, and fractures occurring shortly before skeletal maturity (Goodwin and Kuivila 2002). Forearm shaft fractures that are apparently unstable should be fixed primarily, but it is difficult to determine the stability of forearm shaft fractures by way of plain radiographs (Ploegmakers and Verheyen 2006).
Regarding the strengths of the study, it was population-based with full participation, and as a result there was no selection bias. We believe that our findings are generalizable.
In summary, our findings do not support the recent increasing trend towards surgery in forearm shaft fractures in children. However, it would be of interest to compare ESIN with traditional nonoperative treatment in a randomized clinical trial.
Acknowledgments
J-JS and EA: study design, data collection, data analysis, and preparation of the manuscript; SV: study design, interpretation of primary and follow-up radiographs, and preparation of the manuscript; TP: study design, statistical analysis, and preparation of the manuscript; WS: study design, preparation of the manuscript, and supervision.
The study was supported financially by the Finnish Paediatric Orthopaedic Association, Vaasa Foundation of Physicians, Finska Läkaresällskapet, the Medical Society of Finland, and Oulu University.
The authors declare that they have no competing interests.
References
- Abraham A, Kumar S, Chaudhry S, Ibrahim T. Surgical interventions for diaphyseal fractures of the radius and ulna in children . Cochrane Database Syst Rev. 2011;11 doi: 10.1002/14651858.CD007907.pub2. CD007907. doi (11): CD007907. [DOI] [PubMed] [Google Scholar]
- Annan I, Moran M. Indications for inetrnal fixation of fractures in children. Curr Orthop. 2006;20:241–55. [Google Scholar]
- Cheng JC, Ng BK, Ying SY, Lam PK. A 10-year study of the changes in the pattern and treatment of 6,493 fractures . J Pediatr Orthop. 1999;19(3):344–50. [PubMed] [Google Scholar]
- Colaris JW, Allema JH, Reijman M, Biter LU, de Vries MR, van de Ven CP, Bloem RM, Verhaar JA. Risk factors for the displacement of fractures of both bones of the forearm in children . Bone Joint J. 2013;95-B(5):689–93. doi: 10.1302/0301-620X.95B5.31214. [DOI] [PubMed] [Google Scholar]
- Daruwalla JS. A study of radioulnar movements following fractures of the forearm in children . Clin Orthop. 1979;139:114–20. [PubMed] [Google Scholar]
- Firl M, Wunsch L. Measurement of bowing of the radius . J Bone Joint Surg Br. 2004;86(7):1047–9. doi: 10.1302/0301-620x.86b7.14294. [DOI] [PubMed] [Google Scholar]
- Flynn JM, Jones KJ, Garner MR, Goebel J. Eleven years experience in the operative management of pediatric forearm fractures . J Pediatr Orthop. 2010;30(4):313–9. doi: 10.1097/BPO.0b013e3181d98f2c. [DOI] [PubMed] [Google Scholar]
- Foster HE, Cabral DA. Is musculoskeletal history and examination so different in paediatrics? . Best Pract Res Clin Rheumatol. 2006;20(2):241–62. doi: 10.1016/j.berh.2005.11.001. [DOI] [PubMed] [Google Scholar]
- Franklin CC, Robinson J, Noonan K, Flynn JM. Evidence-based medicine: Management of pediatric forearm fractures . J Pediatr Orthop. 2012;32(Suppl 2):S131–4. doi: 10.1097/BPO.0b013e318259543b. [DOI] [PubMed] [Google Scholar]
- Goldfarb CA, Ricci WM, Tull F, Ray D, Borrelli J., Jr Functional outcome after fracture of both bones of the forearm . J Bone Joint Surg Br. 2005;87(3):374–9. doi: 10.1302/0301-620x.87b3.15509. [DOI] [PubMed] [Google Scholar]
- Goodwin RC, Kuivila TE. Pediatric elbow and forearm fractures requiring surgical treatment . Hand Clin. 2002;18(1):135–48. doi: 10.1016/s0749-0712(02)00017-3. [DOI] [PubMed] [Google Scholar]
- Helenius I, Lamberg TS, Kaariainen S, Impinen A, Pakarinen MP. Operative treatment of fractures in children is increasing. A population-based study from finland . J Bone Joint Surg Am. 2009;91(11):2612–6. doi: 10.2106/JBJS.H.01519. [DOI] [PubMed] [Google Scholar]
- Hogstrom H, Nilsson BE, Willner S. Correction with growth following diaphyseal forearm fracture . Acta Orthop Scand. 1976;47(3):299–303. doi: 10.3109/17453677608991994. [DOI] [PubMed] [Google Scholar]
- Kang SN, Mangwani J, Ramachandran M, Paterson JM, Barry M. Elastic intramedullary nailing of paediatric fractures of the forearm: A decade of experience in a teaching hospital in the united kingdom . J Bone Joint Surg Br. 2011;93(2):262–5. doi: 10.1302/0301-620X.93B2.24882. [DOI] [PubMed] [Google Scholar]
- Kay S, Smith C, Oppenheim WL. Both-bone midshaft forearm fractures in children . J Pediatr Orthop. 1986;6(3):306–10. doi: 10.1097/01241398-198605000-00009. [DOI] [PubMed] [Google Scholar]
- Konopinski MD, Jones GJ, Johnson MI. The effect of hypermobility on the incidence of injuries in elite-level professional soccer players: A cohort study . Am J Sports Med. 2012;40(4):763–9. doi: 10.1177/0363546511430198. [DOI] [PubMed] [Google Scholar]
- Landin LA. Epidemiology of children’s fractures. J Pediatr Orthop B. 1997;6(2):79–83. doi: 10.1097/01202412-199704000-00002. [DOI] [PubMed] [Google Scholar]
- Mehlman CT, Wall EJ. 6th. Lippincott Williams & Wilkins, Philadelphia; 2006. Injuries to the shafts of the radius and ulna. In the book: Beaty & Kasser (Ed.): Rockwood and Wilkins’ Fractures in Children; pp. 399–441. Edition. [Google Scholar]
- Nork SE, Hennrikus WL, Loncarich DP, Gillingham BL, Lapinsky AS. Relationship between ligamentous laxity and the site of upper extremity fractures in children: Extension supracondylar fracture versus distal forearm fracture . J Pediatr Orthop. 1999;8(2):90–2. [PubMed] [Google Scholar]
- Ploegmakers JJ, Verheyen CC. Acceptance of angulation in the non-operative treatment of paediatric forearm fractures . J Pediatr Orthop. 2006;15(6):428–32. doi: 10.1097/01.bpb.0000210594.81393.fe. [DOI] [PubMed] [Google Scholar]
- Price CT. Acceptable alignment of forearm fractures in children: Open reduction indications. J Pediatr Orthop. 2010;30(2):82–4. [Google Scholar]
- Sage FP. Medullary fixation of fractures of the forearm. A study of the medullary canal of the radius and a report of fifty fractures of the radius treated with a prebent triangular nail . J Bone Joint Surg Am. 1959;41-A(8):1489–516. [PubMed] [Google Scholar]
- Salonen A, Salonen H, Pajulo O. A critical analysis of postoperative complications of antebrachium TEN-nailing in 35 children . Scand J Surg. 2012;101(3):216–21. doi: 10.1177/145749691210100313. [DOI] [PubMed] [Google Scholar]
- Sinikumpu JJ, Lautamo A, Pokka T, Serlo W. Complications and radiographic outcome of children’s both-bone diaphyseal forearm fractures after invasive and non-invasive treatment. Injury. 2012a;44(4):431–6. doi: 10.1016/j.injury.2012.08.032. Apr. [DOI] [PubMed] [Google Scholar]
- Sinikumpu JJ, Lautamo A, Pokka T, Serlo W. The increasing incidence of paediatric diaphyseal both-bone forearm fractures and their internal fixation during the last decade . Injury. 2012b;43(3):362–6. doi: 10.1016/j.injury.2011.11.006. [DOI] [PubMed] [Google Scholar]
- Sinikumpu J, Keränen J, Haltia A, Serlo W, Merikanto J. A new mini-invasive technique in treating paediatric diaphyseal forearm fractures by bioabsorbable elastic stable intramedullary nailing: A preliminary technical report . Scand J Surg. 2013a;20 doi: 10.1177/1457496913490459. (Sep): Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Sinikumpu J, Pokka T, Serlo W. The changing pattern of pediatric both-bone forearm shaft fractures among 86,000 children from 1997 to 2009 . European Journal of Pediatric Surgery. 2013b. Feb 26, [DOI] [PubMed]
- Slongo TF, Audige L D VM, on behalf of the AO Pediatric Classification Group Fracture and dislocation classification compendium for children: The AO pediatric comprehensive classification of long bone fractures (PCCF)1 . J Orthop Trauma. 2007;21(10):S135–60. doi: 10.1097/00005131-200711101-00020. Supplement. [DOI] [PubMed] [Google Scholar]
- Soucie JM, Wang C, Forsyth A, Funk S, Denny M, Roach KE, Boone D. Hemophilia Treatment Center Network. Range of motion measurements: Reference values and a database for comparison studies . Haemophilia. 2011;17(3):500–7. doi: 10.1111/j.1365-2516.2010.02399.x. [DOI] [PubMed] [Google Scholar]
- Zlotolow DA. Pediatric forearm fractures: Spotting and managing the bad actors . J Hand Surg. 2012;37(2):363–6. doi: 10.1016/j.jhsa.2011.10.032. [DOI] [PubMed] [Google Scholar]