Abstract
Background and purpose —
Due to the known drawbacks of metal implants, new biomaterials for internal fracture fixation are attracting increasing interest, among them poly(lactic-co-glucolic) acids (PLGAs) and the recently developed silk-tenoin derived materials (STDMs). In accordance with the new philosophy of bio-derived biomaterials (BIODERIBIOs), I describe a novel innovative technology for use in fracture fixation.
Patients and methods —
Screws (2 mm dia.) were manufactured from cylindrical bars of polyglucose-lignol composite (POGLICO) in the form of birch toothpicks from the hospital canteen, dip-coated with alendronate (1 mg/mL, n = 6) or saline (n = 6), and inserted in the proximal tibias of rats for 4 weeks. Fixation was evaluated by mechanical pullout testing. POGLICO nails were inserted in the contralateral tibia for microCT and histology.
Results —
All POGLICO implants remained fixed in the bone (p < 0.001) with a mean pullout force of 37 (SD 5.5) N. MicroCT showed that the control nails were surrounded by a thin layer of new bone, while all bisphosphonate-treated implants were surrounded by a thick layer of cancellous bone. Bisphosphonates more than doubled the bone density around the nails (p = 0.004).
Interpretation —
POGLICO is biocompatible, remains in situ, and appears to provide a higher resistance to pullout forces than bulk silk protein. The material is light, strong, and bio-derived. BIODERIBIO-POGLICO can be sterilized by autoclaving, and has a porous surface that can serve for slow release of drugs applied by simple dip-coating, as demonstrated by the effect of the alendronate treatment. As the raw material for the screws is readily available from the toothpick industry, I believe that the possibilities for commercial development of the material for fracture fixation are promising.
In order to eliminate the problems associated with metal implants, such as temperature sensitivity (Perrone et al. 2014), the development of non-metal, resorbable implant materials has gained increasing interest. Such materials include polylactic-co-glucolic acids, which are, however, associated with problems of local inflammation due to degradation products (Bostman and Pihlajamaki 2000). For this reason, a new biomaterial—bulk silk-tenoin—has recently been tested for biocompatibility and reported in a high-impact journal (Perrone et al. 2014). This material is claimed to be superior to poly(lactic-co-glucolic) acids in many ways, including biocompatibility, its ability to undergo machining and autoclaving, and its usefulness for elution of drugs (Perrone et al. 2014). In view of these recent advances in the research on bio-derived biomaterials (BIODERIBIO), I have tested another material, namely birch, in much the same way as the silk-derived implants were tested. I found that birch may be equally useful and has advantages over silk from its well-documented use in other fields of construction, its easy availability, and the manufacturing know-how gained through the toothpick industry.
Local bisphosphonate treatment has been shown to improve implant fixation in clinical randomized trials of knee prostheses, external fixation pins, and dental implants (Hilding and Aspenberg 2007, Abtahi 2012, Toksvig-Larsen and Aspenberg 2013). I therefore determined whether birch could also act as a carrier of a bisphosphonate.
Material and methods
Overview
12 rats received one polyglucose-lignol composite (POGLICO; i.e. birch) implant in each proximal tibia (PT). The implants in the left proximal tibia (LPT) were spiral-helix-shaped (SHS), and those in the right tibia (RPT) were semi-conical (SCS). Half of the implants were biofunctionalized (BF) with alendronate (POGLICO-ALN+). The remainder were untreated (POGLICO-UNTR). Thus, we had 4 groups, namely POGLICO-SHS-ALN+, POGLICO-SHS-UNTR, POGLICO-SCS-ALN+, and POGLICO-SCS-UNTR. The POGLICO-SHS tibias were used for biomechanical traction resistance construct evaluation (BTRCE). POGLICO-SCS implants were used for microCT (CT) and histology (HIST). So, in short, 6 POGLICO-SHS-ALN+ and 6 POGLICO-SHS-UNTR from the LPT underwent BTRCE, and 6 POGLICO-SCS-ALN+ and 6 POGLICO-SCS-UNTR from the RPT were used for CT and HIST.
In layman’s terms, 12 rats received screws made of birch in the left tibia and nails made of birch in the right tibia. Half of these implants were impregnated with a bisphosphonate. The screws were used for pullout testing and the nails were used for radiography and histology.
Implant production
Toothpicks made of birch were obtained from the canteen of Linköping University Hospital. The diameter was 2.0 mm. Screws were made by cutting out a thread under the dissecting microscope, with 1 turn per mm length, the threaded part being 3 mm long (Figure 1). Nails were made by cutting off the pointed ends of the toothpicks (3 mm long). The implants were placed in 70% ethanol for 24 h and then air-dried. Because the implants were handmade with some unavoidable variation, they were matched in pairs, and one from each pair was randomly chosen for alendronate treatment (by tossing a coin). Screws and nails for alendronate and saline treatment were then packed separately in ordinary bags for autoclaving. After autoclaving, they were air-dried in the bags. Immediately before surgery, each implant was vortexed in alendronate solution (1 mg/mL in saline) for 1 min, kept in the solution until use, and then gently wiped dry and inserted. Controls were treated similarly, but with saline alone.
Figure 1.
A POGLICO-SHS implant (birch screw).
Rats and surgery
12 male Sprague-Dawley rats (mean weight 414 (SD 11) g) were included in the study. The surgery was performed under aseptic conditions as previously described (Agholme 2014). A 6- to 7-mm longitudinal incision was made along the medial aspect of the rat’s left tibia and the periosteum was deflected proximally to the physis. A hole, 2.5 mm in diameter, was drilled with a hand-held drill through one of the cortices, approximately 3 mm distal to the physis. The screw was inserted and the skin was sutured. The nail was then inserted in the contralateral leg by a similar procedure.
An assistant randomized the rats to receive either aledronate-treated implant or control implant (both legs received implants with the same treatment). Randomization was done by use of a randomization list, obtained from www.random.org. The surgeon was unaware of implant treatment.
The study was approved by the regional ethics committee for animal experiments, and institutional guidelines for care and treatment of laboratory animals were followed. I apologize for the predominance of the male gender and will do a follow-up study in female rats.
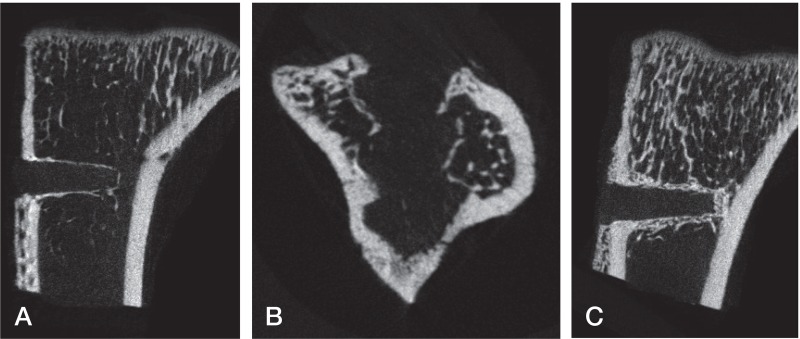
Mechanical analysis and microCT (Figure 2)
Figure 2.
MicroCT results. A. POGLICO-SHS-UNTR tibia (birch nail, no bisphosphonate). B. POGLICO-SCS-UNTR tibia (birch screw, no bisphosphonate). Note the screw-shaped layer of new bone indicating the implant surface. C. POGLICO-SHS-ALN+ tibia (birch nail, bisphosphonate-treated). Note the increased thickness of the surrounding bone.
The mechanical analysis was performed as previously described, by an investigator blinded to the treatment (Agholme 2014). 4 weeks after surgery, the rats were anesthetized and killed. The tibias were mounted in a materials testing machine with the head of the screw pointing out from a hole (3.5 mm in diameter) in a metal plate. The head of the screw was fixed to the machine by a clamp clasping the protruding part of the implant. The screws were then pulled out from the bone until failure, at a constant speed of 0.1 mm/s. Force at failure and energy were calculated by the software of the machine. The measurements were performed within 20 min after the animals were killed. MicroCT was used to measure bone volume per tissue volume and bone density in a cylindrical volume comprising the implant, with settings as previously described (volume diameter: 2 mm; Agholme 2014).
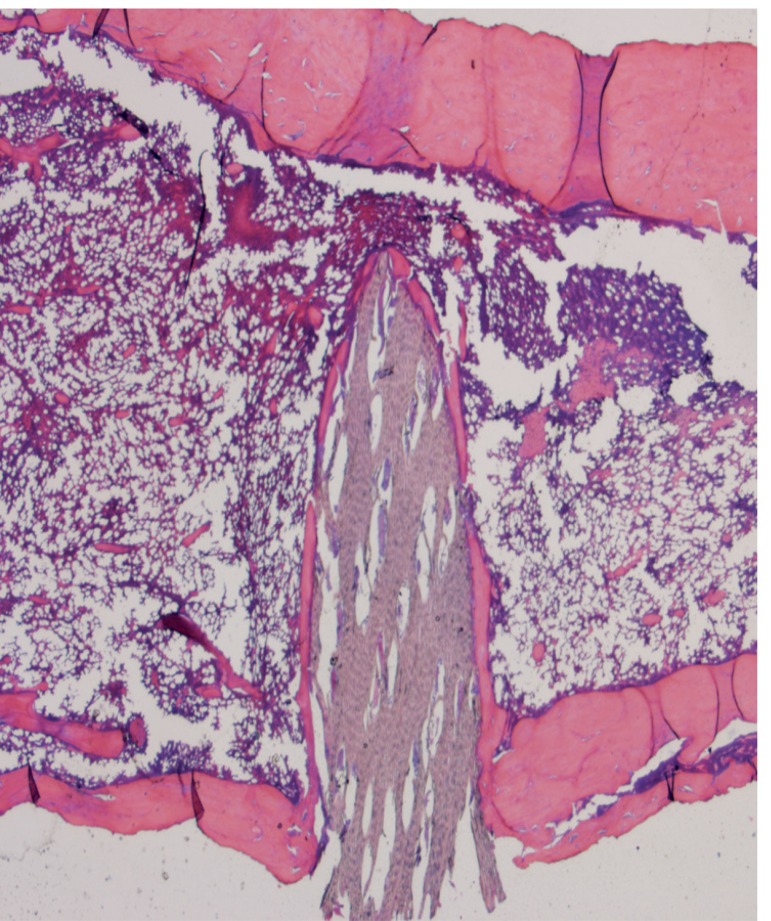
Histology
After evaluation by microCT, the specimens were decalcified, fixed, and sectioned in the sagittal plane, parallel to the axis of the nails. Sections were stained with hematoxylin and eosin.
Statistics
The primary hypothesis was similar to that of a previous study of silk-derived implants (Perrone et al. 2014), namely that the screw implants would remain in the bone. This was tested by sign test.
A secondary hypothesis was that alendronate would increase the bone density (BV/TV) in the vicinity of the nails. This was tested with the Mann-Whitney U-test.
Results
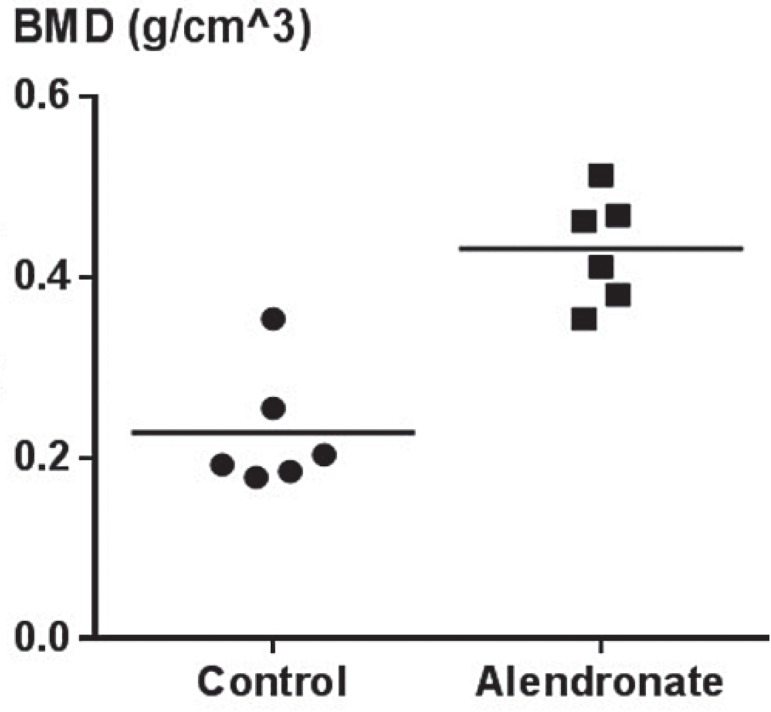
All implants remained in the bone (p < 0.001). The alendronate pretreatment led to a tripling of the bone density around the nails (p = 0.004) (Figures 2 and 3). Mechanical and morphological data are presented in Table. The pullout force was about 36% lower than that of similar-sized metal screws (Wermelin 2008), but 73% higher than that of silk-tenoin screws (Perrone et al. 2014). Histology showed a layer of new bone covering the implant, in some places with no or few visible cells between the bone matrix and the implant (Figure 4).
Figure 3.
Bone density in the vicinity of the implant.
Results from mechanical testing and microCT
| n | Remaining in situ | Peak pullout force, N | Stiffness at pullout, N/mm | Bone density around nail, BV/TV | Bone density around nail, BMD | |
|---|---|---|---|---|---|---|
| Saline | 6 | 6 | 38.3 | 7.3 | 0.084 (0.051) | 0.23 (0.067) |
| Alendronate | 6 | 6 | 35.8 | 4.0 | 0.24 (0.056) | 0.43 (0.060) |
| p-value | 0.001 a | 0.5 | 0.3 | < 0.001 | < 0.001 |
aAs compared to falling out.
Figure 4.
Histology of POGLICO-SHS-UNTR tibia (birch nail, no bisphosphonate). Note the layer of new bone covering the wood.
Discussion
Biomaterial inventions such as bone cement, titanium, and possibly hydroxyapatite coatings lie several decades back in history. Now, the time is ripe for a new wave of biomaterials. Whereas the old materials were all inorganic, we now witness the breakthrough of modern, bio-derived, environmentally friendly organic materials with new properties. Implants made of bio-derived biomaterials (BIODERIBIOs) is a completely new, innovative philosophy.
Fracture surgery has changed dramatically during the past decade, due to simple and somewhat boring practical and engineering improvements, such as angle-stable plates and soft tissue-sparing surgical techniques. Because these improvements were not suitable for publication in high-impact-factor journals, we need to use new, innovative, dynamic philosophies such as BIODERIBIOs. This has the advantage of not requiring the broad knowledge—including clinical experience, engineering, and biology—that slows down scientific progress.
The orthopedic field needs to put more emphasis on philosophies such as robotic surgery, tissue engineering, stem cells, and new innovative breakthrough biomaterials. Another important field of research is to try to find clinical applications for high-technology inventions. There might also be a need for philosophical analysis of orthopedic philosophies.
Bisphosphonates are simple, cheap, well-characterized and safe drugs that improve implant fixation. However, their simplicity and affordability makes research unattractive. I hope to overcome this problem by using Wnt-related drugs (Agholme and Aspenberg 2011). As this signaling pathway is involved in many different processes in the body, including the brain, I expect this to yield more complex, much cited, high-profile research.
I believe that new philosophies in the context of resorbable implants will open up the field for the development of resorbable total joint replacements, something that we have in the pipeline. I am uncertain whether POGLICO is the optimal solution, and we are currently evaluating new advanced kinds of steel that are resorbed by oxidation (so-called RUST technology).
The development of resorbable implants may be a threat to lucrative implant removal, but the risk seems to be small. Because fracture healing time is often difficult to predict, a degradable fracture fixation implant must remain strong for several months. Thus, it will probably take years of frustration before the implant disappears. This opens for an innovative combination: I recommend the use of resorbable implants and surgical removal after the fracture has healed. With this philosophy, we reap the benefits of both principles. This philosophy is called “Sell Two Unnecessary Procedures with Implant Devices” (acronym inappropriate).
When all is said and done, I believe that POGLICO will revolutionize orthopedic surgery. The next step in my research will be to develop plates for fracture fixation. As suggested by a younger member of the research team, these will be produced from ice-cream pins.
Addendum
While writing up the paper, I found that birch has already been seriously evaluated as a bone replacement material. After appropriate heat treatment, birch wood even appears to allow osseointegration and chemical bonding to bone minerals (Rekola 2009). It has not been my intention to cast any doubt on this research.
References
- Abtahi J, Tengvall P, Aspenberg P. A bisphosphonate-coating improves the fixation of metal implants in human bone. A randomized trial of dental implants . Bone. 2012;50(5):1148–51. doi: 10.1016/j.bone.2012.02.001. [DOI] [PubMed] [Google Scholar]
- Agholme F, Aspenberg P. Wnt signaling and orthopedics, an overview . Acta Orthop. 2011;82(2):125–30. doi: 10.3109/17453674.2011.572252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agholme F, Macias B, Hamang M, Lucchesi J, Adrian MD, Kuhstoss S, et al. Efficacy of a sclerostin antibody compared to a low dose of PTH on metaphyseal bone healing . J Orthop Res. 2014;32(3):471–6. doi: 10.1002/jor.22525. [DOI] [PubMed] [Google Scholar]
- Aspenberg P. Black holes in bone - irresistible attractors of foreign materials? . Acta Orthop. 2009;80(1):2–3. doi: 10.1080/17453670902804489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostman OM, Pihlajamaki HK. Adverse tissue reactions to bioabsorbable fixation devices . Clin Orthop Relat Res. 2000;371:216–27. [PubMed] [Google Scholar]
- Hilding M, Aspenberg P. Local peroperative treatment with a bisphosphonate improves the fixation of total knee prostheses - A randomized, double-blind radiostereometric study of 50 patients . Acta Orthop. 2007;78(6):795–9. doi: 10.1080/17453670710014572. [DOI] [PubMed] [Google Scholar]
- Perrone GS, Leisk GG, Lo TJ, Moreau JE, Haas DS, Papenburg BJ, et al. The use of silk-based devices for fracture fixation . Nat Commun. 2014;5:3385. doi: 10.1038/ncomms4385. [DOI] [PubMed] [Google Scholar]
- Rekola J, Aho AJ, Gunn J, Matinlinna J, Hirvonen J, Viitaniemi P, et al. The effect of heat treatment of wood on osteoconductivity . Acta Biomater. 2009;5(5):1596–604. doi: 10.1016/j.actbio.2009.01.018. [DOI] [PubMed] [Google Scholar]
- Toksvig-Larsen S, Aspenberg P. Bisphosphonate-coated external fixation pins appear similar to hydroxyapatite-coated pins in the tibial metaphysis and to uncoated pins in the shaft . Acta Orthop. 2013;84(3):314–8. doi: 10.3109/17453674.2013.797315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wermelin K, Suska F, Tengvall P, Thomsen P, Aspenberg P. Stainless steel screws coated with bisphosphonates gave stronger fixation and more surrounding bone. Histomorphometry in rats . Bone. 2008;42(2):65–71. doi: 10.1016/j.bone.2007.10.013. 3. [DOI] [PubMed] [Google Scholar]