Abstract
Background: Learning on the ward as a practice-oriented preparation for the future workplace plays a crucial role in the medical education of future physicians. However, students’ ward internship is partially problematic due to condensed workflows on the ward and the high workload of supervising physicians. For the first time in a German-speaking setting, students’ expectations and concerns about their internship on the ward are examined in a qualitative analysis regarding their internal medicine rotation within clinical medical education.
Methods: Of a total of 168 medical students in their 6th semester at the Medical Faculty of Heidelberg, 28 students (m=8, f=20, Ø 23.6 years) took part in focus group interviews 3 to 5 days prior to their internship on the internal medicine ward within their clinical internal medicine rotation. Students were divided into four different focus groups. The protocols were transcribed and a content analysis was conducted based on grounded theory.
Results: We gathered a total of 489 relevant individual statements. The students hope for a successful integration within the ward team, reliable and supportive supervisors and supervision in small groups. They expect to face the most common diseases, to train the most important medical skills, to assume full responsibility for their own patients and to acquire their own medical identity. The students fear an insufficient time frame to achieve their aims. They are also concerned they will have too little contact with patients and inadequate supervision.
Conclusion: For the development and standardization of effective student internships, the greatest relevance should be attributed to guidance and supervision by professionally trained and well-prepared medical teachers, entailing a significant increase in staff and costs. A structural framework is required in order to transfer the responsibility for the treatment of patients to the students at an early stage in medical education and in a longitudinal manner. The data suggest that the development and establishment of guidelines for medical teachers associated with clearly defined learning objectives for the students’ internships are urgently needed. Based on our findings, we provide first recommendations and suggest possible solutions.
Keywords: Workplace learning, undergraduate medical education, clinical training, focus groups, grounded theory
Zusammenfassung
Hintergrund: Innerhalb der medizinischen Ausbildung angehender Ärzte kommt dem Lernen am späteren Arbeitsplatz als praxisrelevante Vorbereitung auf die spätere ärztliche Tätigkeit eine entscheidende Rolle zu. Doch studentische Stationseinsätze sind aufgrund verdichteter Arbeitsabläufe auf Station und Arbeitsbelastung der betreuenden Stationsärzte problembehaftet. Erstmals werden hier im deutschsprachigen Raum die studentischen Erwartungen und Befürchtungen im Hinblick auf die Stationseinsätze im klinischen Studienabschnitt für den Fachbereich der Inneren Medizin untersucht.
Methodik: 28 Medizinstudierende des 6. Semesters der Medizinischen Fakultät Heidelberg (m=8; w=20; Ø 23,6 Jahre) nahmen 3-5 Tage vor ihrem Stationseinsatz in der Inneren Medizin verteilt auf vier Fokusgruppen an jeweils einer Fokusgruppenanalyse teil. Die Protokolle wurden transkribiert und inhaltsanalytisch auf der Grundlage der Grounded Theory ausgewertet.
Ergebnisse: Es wurden insgesamt 489 relevante Einzelaussagen erfasst: Die Studierenden wünschen sich eine gelungene Integration auf Station, verlässliche und unterstützende ärztliche Betreuer und eine Betreuung in kleinen Gruppen; sie erwarten sich die häufigsten Krankheitsbilder kennenzulernen, die wichtigsten ärztlichen Fertigkeiten zu trainieren, Verantwortung für eigene Patienten zu übernehmen und eine eigene ärztliche Identität zu entwickeln. Die Studierenden befürchten einen zu knappen zeitlichen Rahmen, zu wenig Patientenkontakt und eine mangelhafte ärztliche Betreuung.
Schlussfolgerung: Bei der Entwicklung und Standardisierung effektiver studentischer Stationseinsätze sollte der ärztlichen Betreuung und Supervision durch professionell geschulte und gut vorbereitete ärztliche Dozenten höchste Relevanz zukommen, was einen erheblichen Mehraufwand an personellen und finanziellen Ressourcen bedeutet. Es bedarf strukturell gelungener Rahmenbedingungen, die es ermöglichen, den Studierenden frühzeitig und longitudinal Verantwortung für die Behandlung von Patienten übertragen zu können. Die Daten legen nahe, dass die Entwicklung und Etablierung von Handlungsrichtlinien für Dozierende verbunden mit klar definierten Lernzielen für den studentischen Einsatz auf Station dringend notwendig sind. Auf der Basis unserer Ergebnisse liefern wir hierzu erste Empfehlungen und Lösungsansätze.
Project sponsorship
This work was supported by the Ministry of Science, Research and the Arts of Baden-Württemberg (project number: D 100011720; AZ32-402.17(05)/34)
Introduction
Learning on the job within medical education is of crucial importance for future physicians. During clinical ward internships, students work under conditions that are as close as possible to their future workplace [28]. Prior to their final year medical education (German: “Praktisches Jahr”), medical students have already rotated between different medical departments during their clinical training, and have thus experienced clinical practice and contact with real patients. In the course of the internship, students are integrated into the ward teams of the university hospitals and academic teaching hospitals, with the aim of fostering professionalism and competence in patient management [14]. Based on principles of learning theory, these internships combine theoretical knowledge and practical competencies acquired in the clinical context [8], [12].
Therefore, clinical internships are of the greatest relevance for the quality of medical education. Furthermore, bedside teaching can prevent later medical errors and guarantee patient safety, as emphasized in the current literature [1], which attributes even greater importance to the adequate training of future physicians. However, students’ training on the ward is still beset with numerous problems. The national and international development of health care systems has led to condensed workflows, more complex organizational structures and shorter stays of patients on the ward, leading to higher workloads for the supervising physicians. For clinicians, the difficulty of reconciling student supervision with routine work on the ward has been further exacerbated by the current situation of the health care systems [24]. These unfavorable training conditions inevitably lead to deficits in the supervision of students and ultimately prevent the students from receiving an appropriate introduction to the crucial clinical skills [30], [31], [37].
In a qualitative focus group study, Schrauth et al. [33] showed that during their internship, final year students in Germany had barely any responsibility for diagnosis, treatment planning and treatment of patients, and were weighed down by routine work. The students primarily attributed these unsatisfactory learning conditions and the lack of training success to the time constraints of the supervising physicians. A particularly dramatic finding was that, according to the students, the training on the ward led to uncertainty and fear regarding their future independent work as physicians. Moreover, they were afraid that once they had become fully qualified physicians, they might commit errors in the treatment of patients due to the lack of practical learning experience [33].
International studies consistently show that the quality of the medical internship varies hugely, because internship rotations are carried out at different hospital sites, with different supervisors and with variations in terms of the mix of patients. Bedside teaching is far less structured and standardized than theoretical learning during the preclinical training, where all students complete the same program, study the same material, read the same books and take the same final examinations [38], [40]. International studies also confirm that students on the ward spend too much time on activities that have little educational value [5], [10], [30], [37], [40]. Therefore, on the whole, clinical rotations can be described as opaque and unpredictable, and students appear to learn rather through ‘trial and error’ than through an appropriate and well-grounded educational concept [12].
To the best of our knowledge, no investigation in the German-speaking countries has explored students’ expectations and fears regarding their training on the ward prior to final year medical education. Therefore, we conducted a qualitative focus group analysis with students in their 6th semester. The study took place during clinical undergraduate lessons shortly before the internal medicine rotation. The main objective was to gain an understanding of whether the expectations and concerns of students in the clinical part of medical education correspond to those of the final year medical students evaluated in the study by Schrauth et al. [33]. If this is indeed the case, on the basis of our results and the findings of Schrauth et al. [33], we can provide concrete and pragmatic guidelines for the arrangement of students’ internships on the ward.
Methods
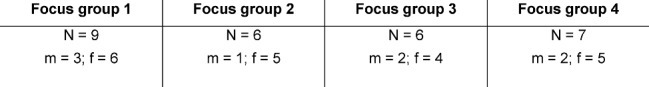
The focus group analysis of students’ expectations and concerns regarding their training on the ward was based on a sample of N=28 medical students (m=8, f=20, mean age 23.6 years) in their 6th semester (third year) from a total of 168 sixth-semester medical students (N=168, m=59, f=109, mean age 23.2 years). In the summer semester of 2007, the students had to complete their rotation in the subject of Internal Medicine as part of HeiCuMed (Heidelberger Curriculum Medicinale; [36]). The internship took place over a 10-week period, with all students assigned to 14 different wards at the Medical Hospital at the University of Heidelberg and to the Academic Teaching Hospitals of the University of Heidelberg for 5 weeks each. The focus group analysis took place 3-5 days prior to the students’ ward internship. By an announcement during lectures the students were approached and recruited to participate in the study on a voluntary basis. All participants received a medical textbook as compensation. From the student sample (N=28), a total of four focus groups (N=4) were formed. The number of focus groups conducted resulted from a content saturation in the discussions, i.e. for the generation of new content aspects a new discussion group was formed each time until there were no more new notable results of the discussions [9], [26]. The groups were composed as shown in Table 1 (Tab. 1).
Table 1. Participants of focus group analysis (N=28) for every focus group from 1 to 4 (m=male; f=female).
Accompanying internal medicine curriculum
Besides their training on the ward, the students attended lectures, interactive small group seminars on various internal medicine disciplines and lessons in problem-based learning [11], skills-lab training [21], [22] as well as communication training with standardized patients [34]. During their internal medicine clinical training, the students had to achieve a total of 50 credit points on the ward within a credit scoring system: For instance, one point was given for the correctly executed technique of intravenous cannulation. Each week, every student had to admit a patient onto the ward, taking the patient’s history and conducting a physical examination. They were then required to present the patient to an external medical supervisor using a patient documentation form based on the “SOAP” concept by Dahmer et al. [6]. Additionally, students were required to write a patient report. At the end of the semester, students completed a multiple-choice exam and an objective structured clinical examination/OSCE for the assessment of clinical skills [19].
Focus group interviews
The aim of the focus group interviews was to shed light on the personal perception, judgment and experience of students with regard to the upcoming clinical internship in internal medicine with as wide a range as possible [13], [25]. The moderated discussion took an average of 70 minutes across all focus groups. Each focus group discussion was based on the following ‘question route’:
Question 1: What are your expectations / wishes about your training on the ward?
Question 2: What fears do you have about your training on the ward?
The discussions were recorded and subsequently transcribed.
Evaluation of the transcripts
The discussions were transcribed verbatim and analyzed using qualitative content analysis with the aid of the software MaxQDA (2007 version, VERBI GmbH, Berlin). The content analysis approach was based on grounded theory. First, we conducted an open coding of the discussions to search for recurring topics, and in a second step we derived the relevant categories [4]. The allocation to the respective topics and categories was conducted by a first coder and subsequently validated by an expert. Since the focus of this study is to establish a theory out of practice, a purely inductive category development in accordance with grounded theory was chosen as the procedure for content analysis with the aim of developing aspects of evaluation directly from the transcripts [4], [9], [26]. Compared to the method of Mayring [15], in which inductive and deductive categories are derived with the aim of achieving a systematic, comprehensible analysis of transcripts, the current method has the advantage that the transcripts can be evaluated freely without being tied to a priori defined, theoretically founded aspects of evaluation in the sense of methodological safeguarding.
Results
Main categories and topics
Within the structured focus group discussions, we detected a total of 489 relevant individual statements. From these individual statements, three main categories were derived:
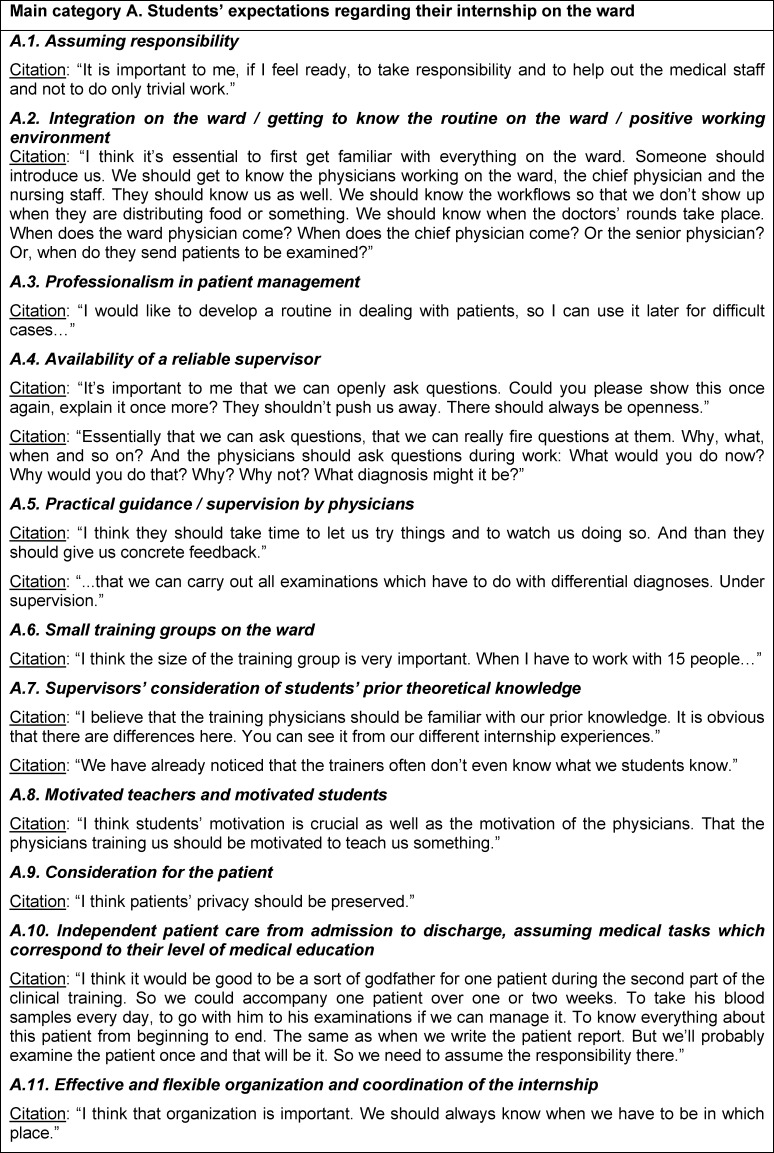
A. Students’ expectations regarding their internship on the ward (see table 2 (Tab. 2))
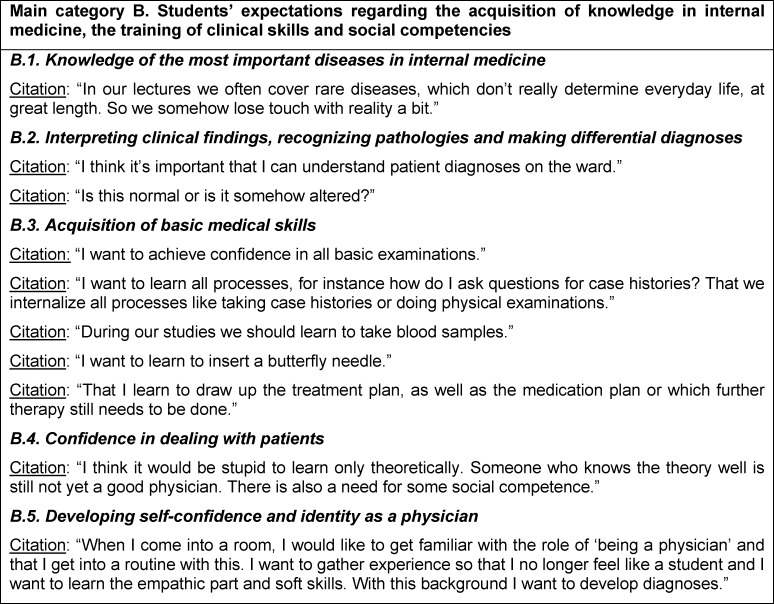
B. Students’ expectations regarding the acquisition of knowledge in internal medicine, the training of clinical skills and social competencies (see table 3 (Tab. 3))
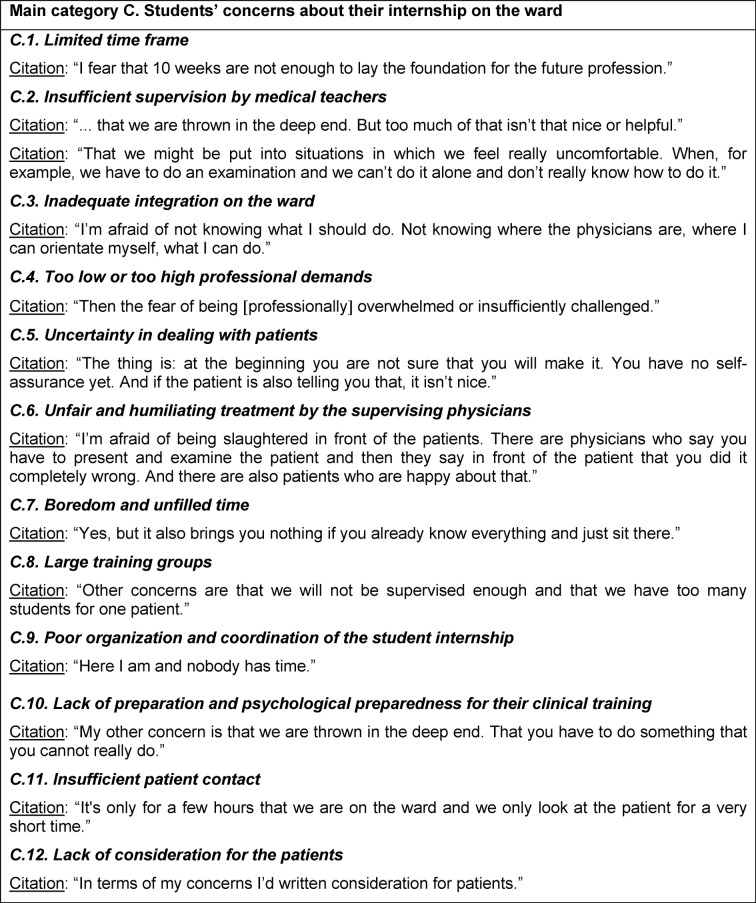
C. Students’ concerns about their internship on the ward (see table 4 (Tab. 4))
Table 2. Examples of students’ citations for the main category A.
Table 3. Examples of students’ citations for the main category B.
Table 4. Examples of students’ citations for the main category C.
Within the three main categories, a total of 28 sub-topics were identified, which are defined in the following sections:
Main category A: Students’ expectations regarding their internship on the ward
A.1. Assuming responsibility
Definition: Besides introduction and supervision by physicians, students wish to be allowed to assume responsibility on the ward. This would enable them to perceive themselves as part of the ward team, to expect learning success, and to feel that their self-efficacy is enhanced.
A.2. Integration on the ward / getting to know the routine on the ward / positive working environment
Definition: The students wish for an appropriate integration on the ward (introduction to the team at the beginning of their internship, participation in the ward rounds, supporting the physicians). Through this, they hope to become familiar with the daily work on the ward and to establish a good working relationship with the medical and nursing staff.
A.3. Professionalism in patient management
Definition: The students wish to attain professionalism in patient management and to be optimally prepared for their future medical work.
A.4. Availability of a reliable supervisor
Definition: The students wish to have a supervising physician who acts as a reliable, accessible and supportive partner and accompanies them continuously over the entire period of their internship.
A.5. Practical guidance / supervision by physicians
Definition: The students wish to be guided and supervised by physicians in terms of learning all relevant clinical skills (e.g., blood sampling, physical examination).
A.6. Small training groups on the ward
Definition: The students would like to work in small training groups with two to three participants. They hope that this would allow them to spend sufficient time with the supervisors. Moreover, supervisions would be intensive and each trainee would have the opportunity to apply the newly learned skills extensively.
A.7. Supervisors’ consideration of students’ prior theoretical knowledge
Definition: To avoid unnecessary repetitions or excessive demands in terms of expert knowledge, the students want the supervisors to take their prior theoretical knowledge into account.
A.8. Motivated teachers and motivated students
Definition: The students wish for motivated medical teachers who are happy to share their knowledge with the students. They also want the students to be highly motivated for their training.
A.9. Consideration for the patient
Definition: The students hope that bedside training will only take place with the patients’ express consent. Severely ill patients should be treated with special consideration. The dignity and privacy of the patients should always be respected.
A.10. Independent patient care from admission to discharge, assuming medical tasks which correspond to their level of medical education
Definition: The students would like to assume responsibility for a patient from admission to discharge in accordance with their level of medical education (introduction to the team at the beginning, participation in ward rounds, assisting the physicians). Through this, they hope to become familiar with all necessary clinical procedures and to professionalize their diagnostic, therapeutic and clinical skills.
A.11. Effective and flexible organization and coordination of the internship
Definition: The students wish for a successful organization, coordination and flexible arrangement of their training on the ward. To avoid unnecessary loss of time, they should only be on the ward when they are needed. The medical advisor should be generally informed about the students’ time schedule.
Main category B: Students’ expectations regarding the acquisition of knowledge in internal medicine, the training of clinical skills and social competencies
B.1. Knowledge of the most important diseases in internal medicine
Definition: The students wish to be become familiar with the most important and current pathologies in internal medicine in order, in a next step, to be able to deal with more complex and rare disorders.
B.2.Interpreting clinical findings, recognizing pathologies and making differential diagnoses
Definition: During their internship, the students expect to learn to interpret symptoms, to diagnose and classify diseases and pathologies and to establish working hypotheses.
B.3. Acquisition of basic medical skills
Definition: The students expect to learn and train all elementary and basic medical skills during their internship in a structured and schematic way: patient presentation, history-taking, clinical skills (e.g. intravenous cannulation, taking blood samples), physical examination (e.g. auscultation of heart and lung), diagnostic procedures as well as treatments, medication schedules, lab orders and discharge letters.
B.4. Confidence in dealing with patients
Definition: The students expect to achieve confidence in dealing even with difficult patients by gaining concrete and practical experiences during their internship.
B.5. Developing self-confidence and identity as a physician
Definition: Through their training on the ward, the students expect to achieve self-confidence and professionalism with respect to all medical activities and to gradually find their own identity as physicians.
Main category C: Students’ concerns about their internship on the ward
C.1. Limited time frame
Definition: The students fear that the time on the ward might be too tight to sufficiently incorporate all of the foundations of the later medical profession.
C.2. Insufficient supervision by medical teachers
Definition: The students are afraid that they might be supervised too infrequently by their medical teachers, and therefore be left to their own devices if problems arise during their internships.
C.3. Inadequate integration on the ward
Definition: The students worry that deficiencies might arise in terms of their integration into the ward team and into the daily routine on the ward.
C.4. Too low or too high professional demands
Definition: The students fear that they might be professionally under- or over-burdened during their internship due to their prior knowledge not being adequately taken into account.
C.5. Uncertainty in dealing with patients
Definition: The students are afraid that their personal insecurity might lead to learning deficits and shortcomings in dealing with patients.
C.6. Unfair and humiliating treatment by the supervising physicians
Definition: The students are concerned that physicians might treat them unfairly because of their insecurity and lack of competence or humiliate them in the presence of the patients.
C.7. Boredom and unfilled time
Definition: The students are concerned that boredom and periods without clearly defined and useful tasks might arise during their internship.
C.8. Large training groups
Definition: The students worry that the training groups on the ward may be too large, leading to a disregard for individual care and supervision.
C.9. Poor organization and coordination of the student internship
Definition: The students fear poor organization and coordination of their ward internship, leading to an inadequate integration into the ward team and insufficient supervision.
C.10. Lack of preparation and psychological preparedness for their clinical training
Definition: The students are worried that they might be psychologically unprepared for the demands of their clinical training, and might therefore be overburdened.
C.11. Insufficient patient contact
Definition: The students fear that their direct contact with the patients might be insufficient.
C.12. Lack of consideration for the patients
Definition: The students fear that during their internship, there might be a lack of regard for the dignity, privacy and wellbeing of the patients.
Discussion
The results presented in our study clearly show that during their internal medicine rotation, students primarily wish to be integrated into the ward team and to be trained by motivated and reliable medical supervisors who accompany them continuously throughout their whole internship. The students’ prior medical knowledge should be taken into consideration by the supervisors. The supervisors should support the students and deal with their uncertainties. In the course of this, the students would like to be trained in small groups. Furthermore, they wish to learn about the most common diseases, to gather practical clinical experience and to train all of the most important and basic clinical skills. Last but not least, students wish to assume real responsibility for patients and clinical procedures, allowing them to gradually develop their own identity as future physicians.
The students are concerned that the time frame for their internship will be too narrow, that they will have too little patient contact and insufficient medical supervision. They are worried about not being adequately integrated into the ward team, about a possibly inflexible organization of their internship, and about being professionally over- or under-burdened, and are afraid of generally feeling unprepared for their whole clinical training.
The presented findings are broadly in line with those of Schrauth et al. [33], who assessed final year students. The timing of the internship and the level of training (the number of semesters completed) therefore appear to have little influence on the students' expectations and concerns about their internship even though, in the daily hospital routine, the differing level of medical education requires a differing degree of supervision by the medical teachers, and a differing extent of patient care is to be realized.
Students from both study populations wish in particular for reliable and continuous medical supervision and a positive relationship with their medical supervisor. The research literature in the field of clinical training on the ward shows that coaching, feedback and supervision increases students’ satisfaction [30], and that the frequency and quality of supervision by medical teachers has a decisive influence on the students' learning success and indirectly on the frequency of students’ contact with patients [40]. It has already been shown that the prerequisites for high-quality medical guidance and supervision are usually not given due to the condensed workflows on the ward and the heavy workload of the supervising physicians. There is little time available and the internship in general proceeds with little structure or standardization [30], [31], [37]. The students are more likely to receive their feedback from junior physicians than from clinically experienced specialists [29], [37], [40].
Based on these results, we suggest the following recommendations for the arrangement of students’ internships on the ward in the field of internal medicine and other conservative areas:
Planning and coordinating the introduction and integration of the students on the ward (e.g. personal introduction of all employees of the ward team at a fixed appointment, regular team meetings with the opportunity for feedback)
Informing and training the medical supervisors about the significance of the quality of students’ supervision for their learning success
Developing learning objectives which take into account the students’ prior knowledge. These objectives will serve as guidelines for the medical supervisors and should cover all relevant diseases as well as the training in all major clinical skills
Transferring responsibility to the students for treatment of patients in accordance with their current level of studies
Forming small training groups
Introducing a clearly structured time frame for the continuous medical supervision of the students with the aim of reducing the workload of the supervising physicians through successful coordination and sufficient staff.
For the development and standardization of effective student internships in medical education, the greatest relevance should be attributed to medical guidance, supervision and feedback, meaning a significant increase in staff and costs. Based on the recommendations listed above, it can be concluded that the following general conditions should be in place: There is a need for a reasonable and well-structured time period for providing supervision. Physicians’ awareness of the importance and quality of their supervision should be improved through professional training. The elaboration of guidelines on the basis of solid didactical concepts coupled with clearly defined learning objectives should be given greater focus. In this respect, it is necessary to appropriately integrate the learning objectives for the acquisition and training of clinical skills.
Beyond learning objectives, students should be strengthened and supported in terms of their self-efficacy and self-confidence, which can be achieved through a consideration of social learning theory and psychological learning principles, for instance “learning through role models” and observation or facilitation of the students’ expectation of self-efficacy [3], [24], [35]. Furthermore, the introduction of open communication about errors and guidance on dealing with difficult patients is essential. This would be an important contribution to the currently called for improvement of patient safety and to the development of a workplace culture which encourages young physicians to report on problems of patient care [1]. To this aim, it would be extremely desirable for medical supervisors to receive social skills training.
A further area for student internships that should be promoted is the development of longitudinal care of patients by the students. To achieve this, a structural framework needs to be created to transfer responsibility to the students, and students’ time should not be fully engaged with activities of little didactic value. In this way, the students are able to learn continuously at their future workplace, which, as mentioned at the outset, is of decisive importance in medical education. If responsibility were transferred early on and with adequate supervision, a step which can be associated with personal experiences of success, students’ anxiety concerning on-ward work would be substantially reduced and the students would be optimally prepared for their future work as physicians. Didactic approaches like clinical education wards for final year students can provide directional impetus in this regard [23], [27], [32], [39].
Preparation courses for the student internships or clinical training programs held in parallel to the ward internship might complement the regular internship [20]. Potential difficulties in this respect can be targeted in advance, thus saving resources. The introduction of ‘shadowing’ projects, in which medical students at earlier stages of their training shadow more experienced medical students when they are performing their usual clerkship duties, as described by Alford and Currie [2], would be useful. Moreover peer-assisted learning programs with student tutors [18] who accompany students during their internships might represent a specific and economical implementation of the guidelines presented above. Furthermore, interventions by specially trained external medical staff have been shown to be promising [7], enabling supervising physicians to be relieved of parts of their daily clinical duties. In this context, the wish expressed by many students to be appropriately integrated into the ward team could be accomplished here if medical staff and nursing staff participate together at an introductory meeting with the students.
In methodological terms, there are several limitations to this study: In terms of the selection of students who took part in the focus group interviews, it should be mentioned that predominantly females participated, possibly leading to a selection bias due to the voluntary nature of participation. Nevertheless, the higher proportion of female participants in the focus groups (71%) realistically reflects the gender distribution in the medical degree course in the summer semester of 2007, with 57% females http://www.uni-heidelberg.de/imperia/md/content/studium/download/studierendenstatistik/ss07.pdf, last cited 2014-04-14. Moreover, as the allocation to the focus groups was oriented to the principle of convenience sampling, the focus groups were practical and efficient to implement. According to Morse and Merkens [16],[17], the attributes of helpful “informants” are defined as follows: The participants possess the knowledge which the researchers need, the ability to reflect, time for the research, and willingness to participate. These criteria would not have been met if participation had been mandatory.
The focus group interviews were conducted according to the concept of theoretical saturation [4], [9], [26], meaning that focus groups were conducted until no new findings could be expected through further interviews. This implies that regardless of the quantity, all contributions – including those of the male participants – were sufficiently recorded. However, in the context of qualitative studies, the proper and desirable intention is to depict excerpts of subjective and therefore limited perception. Another limiting aspect is the delay with which the focus group analysis was published, as different responses in the interviews might have arisen at the current time point. However, with regard to the general conditions of internships for students and faculty today, little has changed in the interim.
The findings presented here and the derived guidelines regarding the relevance of quality and continuity of supervision by medical teachers, the significance of defined learning objectives on the ward, the importance of early transfer of responsibility to the students, and the benefit of appropriate integration of the students into the ward teams, can all make a significant contribution to developing student ward internships which have the best possible learning outcome and provide medical students with the optimum preparation for their future work. At the same time, clearly defined learning objectives, fixed and limited time frames for supervision in conjunction with a successful organization of all necessary general conditions for the students’ clinical training can prevent the supervising medical staff from being overloaded. It has already been pointed out that in order to achieve this, it is also reasonable to use external medical staff – for example with a “Venia Legendi” – as together with the aforementioned accompanying peer teaching projects, this can provide a realistic solution for the additional staff needs brought about by the implementation of guidelines for internships. Further research efforts should focus on the differential acceptance and effectiveness of different teaching formats for student training on the ward.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Ahmed M, Arora S, Carley S, Sevdalis N, Neale G. Junior doctors' reflections on patient safety. J Postgrad Med. 2012;88(1037):125–129. doi: 10.1136/postgradmedj-2011-130301. Available from: http://dx.doi.org/10.1136/postgradmedj-2011-130301. [DOI] [PubMed] [Google Scholar]
- 2.Alford CL, Currie DM. Introducing first-year medical students to clinical practice by having them "shadow" third-year clerks. Teach Learn Med. 2004;16(3):260–263. doi: 10.1207/s15328015tlm1603_7. Available from: http://dx.doi.org/10.1207/s15328015tlm1603_7. [DOI] [PubMed] [Google Scholar]
- 3.Bandura A. Self-efficacy: The exercise of control. New York: Freeman; 1997. [Google Scholar]
- 4.Corbin J, Strauss A. Grounded Theory Research: Procedures, Canons, and Evaluative Criteria. Qualit Sociol. 1990;13(1):3–21. doi: 10.1007/BF00988593. Available from: http://dx.doi.org/10.1007/BF00988593. [DOI] [Google Scholar]
- 5.Daelmans HE, Hoogenboom RJ, Donker AJ, Scherpbier AJ, Stehouwer CD, van der Vleuten CP. Effectiveness of clinical rotations as a learning environment for achieving competences. Med Teach. 2004;26(4):305–312. doi: 10.1080/01421590410001683195. Available from: http://dx.doi.org/10.1080/01421590410001683195. [DOI] [PubMed] [Google Scholar]
- 6.Dahmer J. Anamnese und Befund – Die ärztliche Untersuchung als Grundlage klinischer Diagnostik. Stuttgart: Thieme; 1998. [Google Scholar]
- 7.Eden M, Köhl-Hackert N, Krautter M, Jünger J, Nikendei C. An innovative model for the structured on-ward supervision of final year students. Med Tech. 2010;32(2):181. doi: 10.3109/01421591003656867. [DOI] [PubMed] [Google Scholar]
- 8.Evans DE, Wood DF, Roberts CM. The effect of an extended hospital induction on perceived confidence and assessed clinical skills of newly qualified pre-registration house officers. Med Educ. 2004;38(9):998–1001. doi: 10.1111/j.1365-2929.2004.01908.x. Available from: http://dx.doi.org/10.1111/j.1365-2929.2004.01908.x. [DOI] [PubMed] [Google Scholar]
- 9.Glaser BG, Strauss AL. The Discovery of Grounded Theory: strategies for qualitative research. New York: Aldine Pub; 1967. [Google Scholar]
- 10.Howley LD, Wilson WG. Direct Observation of Students during Clerkship Rotations: A Multiyear Descriptive Study. Acad Med. 2004;79(3):276–280. doi: 10.1097/00001888-200403000-00017. Available from: http://dx.doi.org/10.1097/00001888-200403000-00017. [DOI] [PubMed] [Google Scholar]
- 11.Huwendiek S, Skelin S, Nikendei C, Bosse HM, Kischfink M. PBL in der medizinischen Ausbildung: Erfahrungen an der Medizinischen Fakultät Heidelberg. In: Zumbach J, Weber A, Olsowski G, editors. Problembasiertes Lernen: Konzepte, Werkzeuge und Fallbeispiele aus dem deutschsprachigen Raum. Bern: HEP; 2007. pp. 147–159. [Google Scholar]
- 12.Jolly BC, Macdonald MM. Education for practice: the role of practical experience in undergraduate and general clinical training. Med Educ. 1989;23(2):189–195. doi: 10.1111/j.1365-2923.1989.tb00885.x. Available from: http://dx.doi.org/10.1111/j.1365-2923.1989.tb00885.x. [DOI] [PubMed] [Google Scholar]
- 13.Krueger R, Casey M. Focus Groups: A Practical Guide for Applied Research. Thousand Oaks, CA: Sage Publications; 2000. [Google Scholar]
- 14.Lempp H, Seabrook M, Cochrane M, Rees J. The transition from medical student to doctor: perceptions of final year students and preregistration house officers related to expected learning outcomes. Int J Clin Pract. 2005;59(3):324–329. doi: 10.1111/j.1742-1241.2005.00438.x. Available from: http://dx.doi.org/10.1111/j.1742-1241.2005.00438.x. [DOI] [PubMed] [Google Scholar]
- 15.Mayring P. Qualitative Inhaltsanalyse. Forum Qual Sozialforsch. 2000;1(2) Available from: http://qualitative-research.net/fqs/fqs-d/2-00inhalt-d.htm. [Google Scholar]
- 16.Merkens H. Stichproben bei qualitativen Studien. In: Friebertshäuser B, Prengel A, editors. Handbuch Qualitative Forschungsmethoden in der Erziehungswissenschaft. Weinheim, München: Juventa; 1997. pp. 97–106. [Google Scholar]
- 17.Morse JM. Designing qualitative research. In: Denzin NK, Lincoln YS, editors. Handbook of qualitative inquiry. Thousand Oaks, CA: Sage; 1994. pp. 220–235. [Google Scholar]
- 18.Nikendei C, Andreesen S, Hoffmann K, Junger J. Cross-year peer tutoring on internal medicine wards: effects on self-assessed clinical competencies--a group control design study. Med Teach. 2009;31(2):e32–e35. doi: 10.1080/01421590802464452. Available from: http://dx.doi.org/10.1080/01421590802464452. [DOI] [PubMed] [Google Scholar]
- 19.Nikendei C, Jünger J. OSCE – praktische Tipps zur Implementierung einer klinisch-praktischen Prüfung. GMS Z Med Ausbild. 2006;23(3):Doc47. Available from: http://www.egms.de/static/de/journals/zma/2006-23/zma000266.shtml. [Google Scholar]
- 20.Nikendei C, Mennin S, Weyrich P, Kraus B, Zipfel S, Schrauth M, Jünger J. Effects of a supplementary final year curriculum on students' clinical reasoning skills as assessed by key-feature examination. Med Teach. 2009;31(9):e438–442. doi: 10.1080/01421590902845873. Available from: http://dx.doi.org/10.1080/01421590902845873. [DOI] [PubMed] [Google Scholar]
- 21.Nikendei C, Schilling T, Nawroth P, Hensel M, Ho AD, Schwenger V, Zeier M, Herzog W, Schellberg D, Katus HA, Dengler T, Stremmel W, Müller M, Jünger J. Integrated skills laboratory concept for undergraduate training in internal medicine. Dtsch Med Wochenschr. 2005;130(18):1133–1138. doi: 10.1055/s-2005-866799. Available from: http://dx.doi.org/10.1055/s-2005-866799. [DOI] [PubMed] [Google Scholar]
- 22.Nikendei C, Zeuch A, Dieckmann P, Roth C, Schäfer S, Völkl M, Schellberg D, Herzog W, Jünger J. Role-playing for a more realistic technical skills training. Med Teach. 2005;27(2):122–126. doi: 10.1080/01421590400019484. Available from: http://dx.doi.org/10.1080/01421590400019484. [DOI] [PubMed] [Google Scholar]
- 23.Ponzer S, Hylin U, Kusoffsky A, Lauffs M, Lonka K, Mattiasson AC, Nordstrom G. Interprofessional training in the context of clinical practice: goals and students' perceptions on clinical education wards. Med Educ. 2004;38(7):727–736. doi: 10.1111/j.1365-2929.2004.01848.x. Available from: http://dx.doi.org/10.1111/j.1365-2929.2004.01848.x. [DOI] [PubMed] [Google Scholar]
- 24.Prideaux D, Alexander H, Bower A, Dacre J, Haist S, Jolly B, Norcini J, Roberts T, Rothman A, Rowe R, Tallett S. Clinical teaching: maintaining an educational role for doctors in the new health care environment. Med Educ. 2000;34(10):820–826. doi: 10.1046/j.1365-2923.2000.00756.x. Available from: http://dx.doi.org/10.1046/j.1365-2923.2000.00756.x. [DOI] [PubMed] [Google Scholar]
- 25.Przyborski A, Wohlrab-Sahr M. Qualitative Sozialforschung. München: Oldenburg Verlag; 2009. [Google Scholar]
- 26.Rabiee F. Focus-group interview and data analysis. Proc Nutr Soc. 2004;63(4):655–660. doi: 10.1079/PNS2004399. Available from: http://dx.doi.org/10.1079/PNS2004399. [DOI] [PubMed] [Google Scholar]
- 27.Reeves S, Freeth D, McCrorie P, Perry D. 'It teaches you what to expect in future interprofessional learning on a training ward for medical, nursing, occupational therapy and physiotherapy students. Med Educ. 2002;36(4):337–344. doi: 10.1046/j.1365-2923.2002.01169.x. Available from: http://dx.doi.org/10.1046/j.1365-2923.2002.01169.x. [DOI] [PubMed] [Google Scholar]
- 28.Regehr G, Norman GR. Issues in cognitive psychology: implications for professional education. Acad Med. 1996;71(9):988–1001. doi: 10.1097/00001888-199609000-00015. Available from: http://dx.doi.org/10.1097/00001888-199609000-00015. [DOI] [PubMed] [Google Scholar]
- 29.Remmen R, Denekens J, Scherbier AJ, Van der Vleuten CP, Hermann I, Van Puymbroeck H, Bossaert L. Evaluation of skills training during clerkships using student focus groups. Med Teach. 1998;20(5):428–432. [Google Scholar]
- 30.Remmen R, Denekens J, Scherpbier A, Hermann I, van der Vleuten C, Royen PV, et al. An evaluation study of the didactic quality of clerkships. Med Educ. 2000;34(6):460–464. doi: 10.1046/j.1365-2923.2000.00570.x. Available from: http://dx.doi.org/10.1046/j.1365-2923.2000.00570.x. [DOI] [PubMed] [Google Scholar]
- 31.Remmen R, Derese A, Scherpbier A, Denekens J, Hermann I, van der Vleuten C, Van Royen P, Bossaert L. Can medical schools rely on clerkships to train students in basic clinical skills? Med Educ. 1999;33(8):600–605. doi: 10.1046/j.1365-2923.1999.00467.x. Available from: http://dx.doi.org/10.1046/j.1365-2923.1999.00467.x. [DOI] [PubMed] [Google Scholar]
- 32.Scheffer C, Edelhäuser F, Tauschel D, Riechmann M, Tekian A. Can final year medical students significantly contribute to patient care? A pilot study about the perception of patients and clinical staff. Med Teach. 2010;32(7):552–527. doi: 10.3109/01421590903437170. Available from: http://dx.doi.org/10.3109/01421590903437170. [DOI] [PubMed] [Google Scholar]
- 33.Schrauth M, Weyrich P, Kraus B, Jünger J, Zipfel S, Nikendei C. Lernen am späteren Arbeitsplatz: Eine Analyse studentischer Erwartungen und Erfahrungen im Praktischen Jahr". Z Evid Fortbild Qual Gesundheitswesen. 2009;103(3):169–174. doi: 10.1016/j.zefq.2008.05.005. Available from: http://dx.doi.org/10.1016/j.zefq.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 34.Schultz JH, Schönemann J, Lauber H, Nikendei C, Herzog W, Jünger J. Einsatz von Standardisierten Patienten im Kommunikations- und Interaktionstraining für Medizinstudierende (Medi-KIT): Bedarfsanalyse - Training - Perspektiven. Gruppendyn Organisationsber. 2007;38(1):7–23. doi: 10.1007/s11612-007-0002-y. Available from: http://dx.doi.org/10.1007/s11612-007-0002-y. [DOI] [Google Scholar]
- 35.Schwarzer R, Jerusalem M. Das Konzept der Selbstwirksamkeit. In: Jerusalem M, Hopf D, editors. Selbstwirksamkeit und Motivationsprozesse in Bildungsinstitutionen. Weinheim: Beltz; 2002. pp. 28–53. [Google Scholar]
- 36.Steiner T, Jünger J, Schmidt J, Bardenheuer H, Kirschfink M, Kadmon M, Schneider G, Seller H, Sonntag HG. HEICUMED: Heidelberger Curriculum Medicinale – Ein modularer Reformstudiengang zur Umsetzung der neuen Approbationsordnung. Gesundheitswesen (Suppl Med Ausbild) 2003;20(Suppl2):87–91. Available from: https://gesellschaft-medizinische-ausbildung.org/files/ZMA-Archiv/2003/2/Steiner_T,_J%C3%BCnger_J,_Schmidt_J,_Bardenheuer_H,_Kirschfink_M,_Kadmon_M,_Schneider_G,_Seller_H,_Sonntag_HG.pdf. [Google Scholar]
- 37.Van Der Hem-Stokroos HH, Scherpbier AJ, Van Der Vleuten CP, De Vries H, Haarman HJ. How effective is a clerkship as a learning environment? Med Teach. 2001;23(6):599–604. doi: 10.1080/01421590127200. Available from: http://dx.doi.org/10.1080/01421590127200. [DOI] [PubMed] [Google Scholar]
- 38.Van der Vleuten CP, Scherpbier AJ, Dolmans DH, Schuwirth LW, Verwijnen GM, Wolfhagen HA. Clerkship assessment assessed. Med Teach. 2000;22(6):592–600. doi: 10.1080/01421590050175587. Available from: http://dx.doi.org/10.1080/01421590050175587. [DOI] [PubMed] [Google Scholar]
- 39.Wahlstrom O, Sanden I, Hammar M. Multiprofessional education in the medical curriculum. Med Educ. 1997;31(6):425–429. doi: 10.1046/j.1365-2923.1997.00669.x. Available from: http://dx.doi.org/10.1046/j.1365-2923.1997.00669.x. [DOI] [PubMed] [Google Scholar]
- 40.Wimmers PF, Schmidt, HG, Splinter TA. Influence of clerkship experiences on clinical competence. Med Educ. 2006;40(5):450–458. doi: 10.1111/j.1365-2929.2006.02447.x. Available from: http://dx.doi.org/10.1111/j.1365-2929.2006.02447.x. [DOI] [PubMed] [Google Scholar]