Abstract
Introduction: With the amendment of the medical licensure act (Approbationsordnung) in 2012, a four-week clerkship in primary care (FHV) became mandatory. We investigated the expectations with which students begin the FHV, which criteria are relevant in selecting the location for the FHV, and the experiences the students had during the FHV.
Method: In a cross-sectional study, all third-year students at both medical schools in Saxony-Anhalt were surveyed in 2013 about their expectations and experiences regarding the FHV. This is the last cohort for which the FHV is optional. Questions were asked about 29 items addressing six topics (personal information, selection of FHV location, selection of FHV medical practice, expectations, experiences, and specialty selection).
Results: Out of a student body of 446, responses were received from N=424 (response rate 95.1%; of which 61.8% female). Of these students, 71 (16.7%) had completed the FHV and 70 (16.5%) were planning to; another 267 students (63%) had not (yet) planned to participate in an FHV. Where a student’s parents lived, personal recommendations of a particular medical practice and the attractiveness of the region were the most important criteria for selecting the clerkship site. After completing the FHV, the learning objectives reflected themselves in the experiences of the students in a similar order and significance as in the expectations of students who planned or had not (as of yet) planned to complete the FHV. A relevant influence of the FHV confirming the choice to specialize in general practice or outpatient care was not indicated by those who had completed the FHV.
Conclusion: After location and practice, the FHV is selected according to personal criteria and in connection with prioritized learning objectives. From the students’ perspective, the most frequently named learning objectives are also identified as acquired experience after completing the FHV. However, the FHV does not have a reinforcing effect on the selection of general practice as a specialty.
Keywords: general practice, lerkship, primary care, expectation, experiences
Zusammenfassung
Einleitung: Mit Novellierung der Approbationsordnung für Ärzte 2012 wurde eine vier wöchige Famulatur in der hausärztlichen Versorgung (FHV) obligatorisch. Wir untersuchten daher mit welchen Erwartungen Studierende die FHV beginnen, nach welchen Kriterien FHV-Plätze ausgesucht und welche Erfahrungen in der FHV gemacht werden.
Methode: In einer Querschnittserhebung wurden alle Medizinstudierenden des dritten Studienjahres der beiden medizinischen Fakultäten in Sachsen-Anhalt in 2013 zu Erwartungen und Erfahrungen bezüglich FHV befragt. Dieses war der letzte Jahrgang, in dem die FHV fakultativ absolviert werden konnte. Erfragt wurden 29 Items zu 6 Themenkomplexen (Person, FHV-Ortsauswahl, FHV-Praxisauswahl, Erwartungen, Erfahrungen, Fachgebietswahl).
Ergebnisse: Von 446 Studierenden antworteten N=424 (Rücklauf 95,1%; davon weiblich 61,8%). Hiervon hatten 71 (16,7%) die FHV absolviert und 70 (16,5%) planten diese, weitere 267 (63%) hatten (noch) keine FHV geplant. Wohnort der Eltern, persönliche Empfehlung der Famulaturpraxis und Attraktivität der Region waren die wichtigsten Auswahlkriterien für den Famulaturort. Nach der FHV spiegelten sich in den Erfahrungen der Studierenden die Lernziele in ähnlicher Reihenfolge und Gewichtung wie in der Erwartungen der Studierenden mit geplanter FHV oder (noch) ohne geplante FHV. Ein relevanter Einfluss der FHV auf die Bestärkung einer Fachgebietswahl für Allgemeinmedizin oder die ambulante Versorgung wurde von den Absolventen der FHV nicht angegeben.
Zusammenfassung: Die FHV wird nach Ort und Praxis nach persönlichen Kriterien ausgewählt und mit priorisierten Lernzielen verbunden. Die häufigsten Lernziele werden nach FHV auch als gemachte „Erfahrung“ aus Sicht der Studierenden angegeben. Die FHV wirkt jedoch nicht bestärkend auf die Fachgebietswahl für Allgemeinmedizin.
Introduction
Ensuring access to primary care by encouraging young doctors is increasingly being perceived as a governmental responsibility within the context of providing services to the public. This responsibility is also being passed by the legislature to the universities in the form of pertinent recommendations [1]. Evidence speaks for influencing the choice of medical specialty through making changes in medical education; the structure and method of teaching medicine (including the time point, duration and intensity of contact with primary care) are important for the later selection of a specialty in ambulant medical care [2]. With the revision of the licensing regulations (Ärztliche Approbationsordnung) of July 24, 2012, medical students in the clinical study phase now must demonstrate the completion of a four-week clerkship in a primary care medical practice (FHV) when registering for the second part of the state medical exam after June 10, 2015. This clerkship can take place in the medical practices of general practitioners, internists without a specialty, or pediatricians.
According to the expectations of the health administration, this required clerkship is supposed to encourage young physicians at the beginning of their careers and strengthen the field of general practice. Besides the influence of a particular university medical program, there are already a series of other well-analyzed predicators for the later choice of specialty. Along with sociodemographic (sex, etc.) and work-related (working conditions, etc.) factors [2], these include professional demands [3], [4], [5], individual plans for the future, geographic origin, family ties [6], [7], children [3], [6], option to work part-time, mentoring programs [8], type of medical practice [5] and compatibility between having a family and practicing medicine [5], [6], [9].
A possible influence among or interaction between the FHV and specialty choice has not yet been extensively analyzed in Germany. It is questionable if any reasons for rejecting a specialty in primary care could be positively influenced by the FHV: the perception of low professional recognition [5], presumption of lower income [4], assumption of greater administrative burdens [3], [5], the fear of compensation demands from the state-run health insurance funds [5], and a supposed lower level of professional self-determination [3].
For these reasons, we investigated the final student cohort for whom the FHV is still optional and who, as a result, could provide baseline data prior to the introduction of the required clerkship. These students were surveyed about their expectations, learning objectives and criteria for selecting a medical practice for the clerkship prior to beginning the FHV and whether or not after FHV completion, the students perceived confirmation of a decision to specialize in general practice or outpatient care.
Method
A cross-sectional study using a standardized questionnaire was conducted of all medical students attending required courses in the third year of study at the universities in Halle and Magdeburg in July 2013. Twenty-nine items were asked addressing six areas (person, clerkship, experiences & expectations, attained / expected learning objectives, criteria for FHV location, influence of the clerkship on specialty choice). The questions used single-choice and multiple-choice responses, as well as a bipolar Likert rating scale (1=fully agree to 6=fully disagree). The expected learning objectives describe skills which the medical students wished to acquire from a planned or a not (yet) completed FHV, or which were expected of an FHV by students even if they had not yet at the time made plans to participate in the clerkship. The attained learning objectives covered the students’ subjectively acquired skills after completing the FHV. The statements of students who gave unclear information about their clerkship status (n=16) were disregarded. Students with an uncompleted FHV (planned or unplanned/not yet planned) were described separately. The statistical calculations using SPSS.22 were carried out descriptively for mean values, standard deviations and odds ratios with 95% confidence interval. Differences in mean values were tested by means of the t-test and significance levels of the odds ratios using logistic regression.
Results
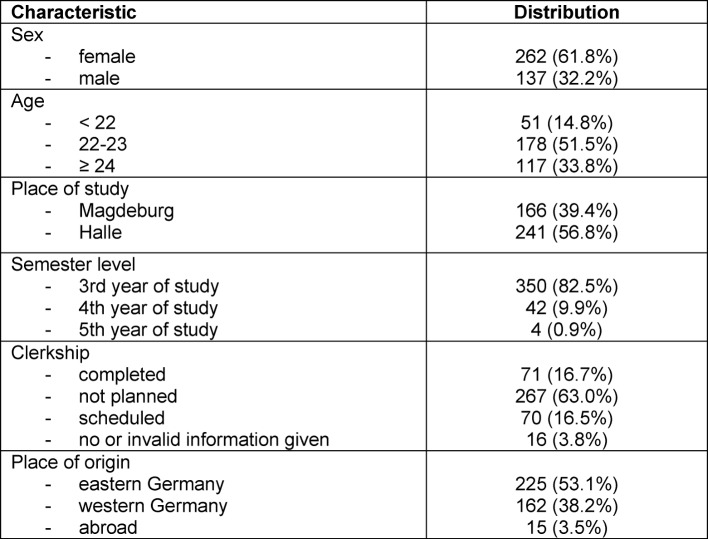
The analysis encompassed 424 questionnaires from a total of 446 students (response rate 95.1%). Due to very similar sociodemographic make-up and responses, the cohorts from Halle and Magdeburg were combined into one sample. Sex and age distribution correspond to the expected values for the third year of university study in Germany, even in regard to the 11% of “older students” as a consequence of career changes or an extended duration of study due to examination delays. The relatively low overall percentage of students who have completed or already planned the FHV totaling around 30% of all respondents is conspicuous here (see Table 1 (Tab. 1)).
Table 1. Sociodemographic characteristics (sex, age, place of study, and level of study) of the responding medical students (n=424). Percentages not totaling 100% indicate missing values.
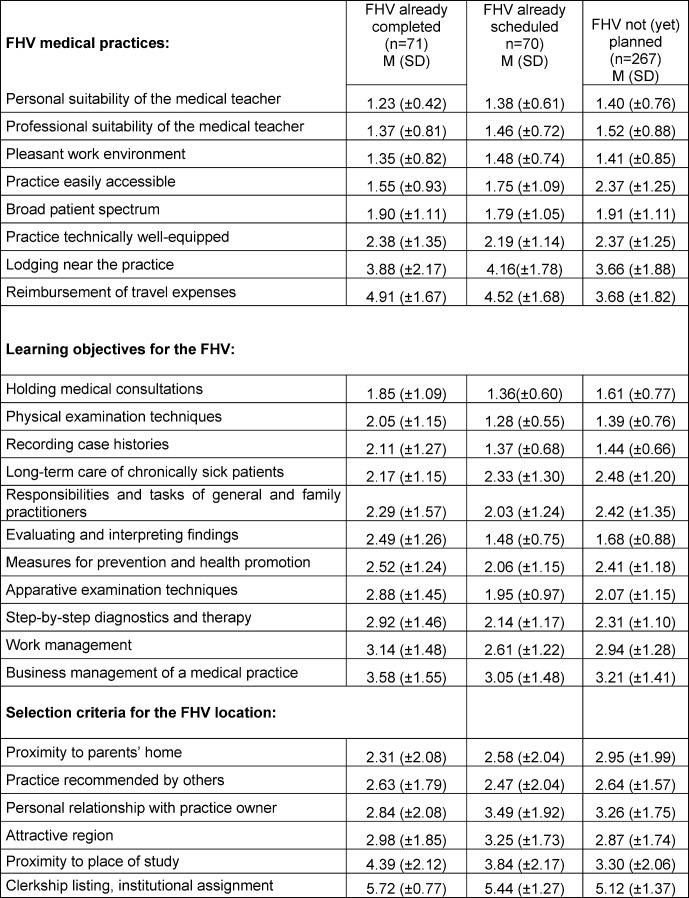
The personal and professional suitability of the medical teacher, work atmosphere in the teaching practice, broad patient spectrum, and easy accessibility of the practice belong to both the most important expectations and experiences of the students. Overnight accommodations near the place of the clerkship and reimbursement of travel expenses were less important for students who had completed the FHV and were less frequently expected by the two groups of students who were planning or had not (yet) made plans to participate in the FHV.
Acquisition of skills in conducting medical consultations, physical examination techniques, recording case history, and long-term care of chronically sick patients frequently occurred during the FHV. These expectations were given a similar order of importance by students who had not (yet) completed the FHV. In contrast, becoming acquainted with organizing work and managing a medical practice from a business standpoint occurred less frequently and were also less often expected. It is noticeable that in both groups of students still without the FHV, the expected learning objectives are predominantly weighted more heavily than the educational experience indicated by the students who have completed the FHV. Particularly conspicuous is the difference between the expectations and experiences for the objective of evaluating and interpreting findings, which was clearly more frequently expected (M 1.63; SD 0.85) than it was experienced as a learning objective in practice (M 2.49; SD 1.26).
In respect to the criteria for choosing an FHV practice and location, the proximity to parents and the positive recommendations of others regarding a particular medical practice were of greatest importance to students, both those who had completed the FHV and those who still had yet to do so. The proximity to the university, formal listings of clerkships, or placement by university institutions had no great importance for any of the three groups (see Table 2 (Tab. 2)).
Table 2. Expectations and experiences regarding the learning objectives and criteria for selection and location of the FHV of third-year medical students (n=408) grouped according to completed FHV, scheduled FHV and not (yet) planned FHV. Mean value (M) with standard deviation (SD) on a Likert scale of 1=fully agree to 6=fully disagree.
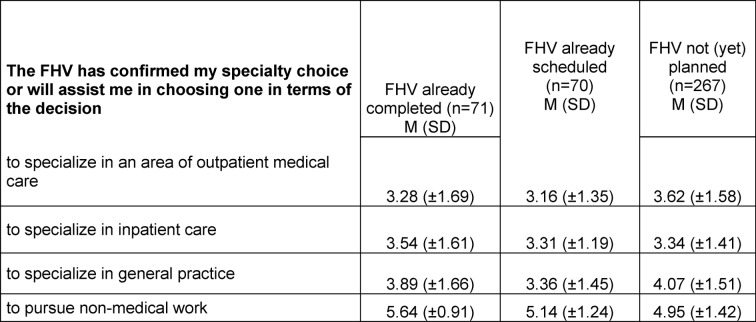
Regarding the importance of the FHV for the later choice of specialty, only moderate agreement was seen across the board, without significant differences arising between students who had completed the FHV and those (still) without a planned FHV. Overall, taking part in the FHV did not reinforce the surveyed students who had completed the FHV in their decision to specialize in general practice (M 3.89; SD 1.66) or in another field of outpatient care (M 3.28; SD 1.69). Likewise and to the same degree, students who planned or (still) had yet to plan the FHV did not expect that they would find confirmation in the FHV regarding a decision to specialize in general practice or another field of ambulant care (see Table 3 (Tab. 3)).
Table 3. Expectations and experiences regarding the influence of the FHV on the selection of a specialty (n=408) by third-year medical students grouped according to completed FHV, scheduled FHV, and not (yet) planned FHV. Mean value (M) with standard deviation (SD) on a Likert scale of 1=fully agree to 6=fully disagree.
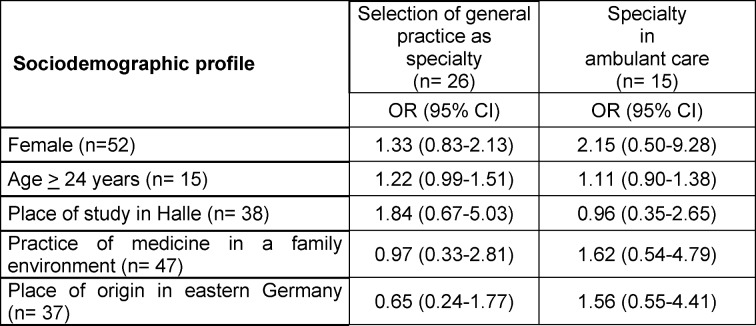
Considering the possible predictors for the future choice of a specialty (in general practice or another area of outpatient medical care) among students with an already completed FHV (n=71), only tendencies can be seen depending upon the independent variables of age, sex and place of study, etc. However, none of these tendencies attained the level of statistical significance due to the small sample size and wide variance. Individual tendencies are presented in the following despite having no statistical significance, since in prior studies investigating the effects of general practice curricula on choice of specialty, these tendencies have played an important role. Female FHV graduates demonstrate a 33% higher chance of selecting a specialty in general practice and a 115% higher chance of taking up work in another area of ambulant care than men. In addition, students above the age of 23 show a 22% higher chance of choosing a specialty in general practice than younger students. Studying at the medical school in Halle increases the chance of selecting general practice as a specialty by 84%; however, not for other areas in ambulant health care (see Table 4 (Tab. 4)).
Table 4. Odds ratios (OR) with 95% confidence intervals (95% CI) for medical students following completion of the FHV (n=71) for the chance of selecting general practice or a specialty in ambulant care depending on sociodemographic variables. None of the ORs indicated statistical significance.
Discussion
For students who are planning to complete a clerkship in primary care (FHV), this is connected with realistically prioritized expectations. The experiences gathered by students during the FHV show that these expectations are often met. Despite this, there is no indication that the FHV reinforces or encourages a decision to specialize in general practice or another field in outpatient care.
The expectations and experiences of the students regarding the FHV correspond to a great extent with other studies on the general practice clerkship (Blockpraktikum Allgemeinmedizin / BPAM) [10]. It is positive to see that students demonstrate a realistic prioritization of learning objectives for the FHV. What is surprising is that mean values and the ranking of the individual expectations and experiences are very similar after FHV completion, prior to a planned FHV, and in the absence of a planned FHV. Due to the later scheduling of the BPAM and main lecture in Halle and Magdeburg, the FHV represents the first point of contact with general practice and ambulant care. For this reason, the FHV medical teachers, who seem to fulfill their function during this educational phase despite little standardization, are so much the more important [10], [11].
The one-on-one mentoring of the students at the practice demands that medical teachers take time to prepare (asking about expectations and learning objectives, etc.), to teach (case discussions, instruction on carrying out examinations and evaluating findings, etc.), and to conduct wrap-up activities (giving feedback and reflecting on experiences, etc.). This work is presently done (across the board) without compensation or adequate structural support. So that in future approximately 8,000 clerkships can take place each year in sufficiently trained and committed teaching practices, instruments to encourage and motivate medical teachers are needed to acquire students for this specialty and field of healthcare [2], [12], [10], [13].
The learning objectives expected by students prior to a planned FHV and subjectively experienced after a completed FHV were evaluated with a slight tendency to “higher expectation”, particularly in regard to the four most important learning objectives: medical consultations, recording case history, physical examination techniques, and evaluation of findings. This possibly points out the danger of a certain slowing down effect on the daily routine of a medical practice, for there is not always sufficient time to hold discussions, case conferences with evaluation of findings, or impart complex skills [11]. Still, precisely for the development of complex skills students need a secure environment for active and supervised participation in the contact between doctors and patients [14]. It is possible in this case that through the keeping of a clerkship journal the communication between the student and medical teacher regarding the acquisition of skills could be improved further and learning content imparted in a somewhat more standardized manner [15].
Selecting the “right” point in time for the clerkship also very possibly helps determine the expectations and experiences. A lack of practical skills and clinical experience at the beginning of the clinical study phase could not only lead to an all too uncritical assumption of “knowledge”, but also to unrealistic expectations in the student; for the medical teachers this poses a great challenge. Even though curricular phases dealing with general practice in the third and fourth years of study already positively correlate with the selection of a specialty in general practice, this also involves – in terms of the desired effect of the FHV to acquire new doctors – effectively integrating students’ previous experiences from the FHV into the existing curriculum in order to avoid repetition and correct any misconceptions regarding outlook [16], [17].
Since students usually complete their clerkship where their parents live, lodging and reimbursement of travel expenses play a subordinate role in the choice of the FHV location. Centralized listings of clerkships, such as on the website of the German College of General Practitioners and Family Physicians (Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin) (http://www.degam.de), were still being set up at the time of this study and seldom used by students for assistance in making decisions about FHV location. This could however change in the future with a greater demand for FHV practices.
A positive influence exerted by a completed FHV on the choice of general practice as a specialty could not be derived from our data. This stands in opposition to studies on other educational courses and seminars; certainly the FHV is not a formally “scheduled” curricular course and the coordination offices for general practice at the universities have no formal role in the selection of FHV practices, nor the possibility of intervening in regard to the FHV practices [10], [13], [18].
Assumptions and prejudices on the part of students toward general practice (e.g. heavy paperwork, compensation claims asserted by state-run health insurers, lack of professional prestige) are well-described motivational barriers to choosing general practice as a specialty [16]. This makes it that much more important to gain realistic understandings and insights during the FHV through positive personal and professional role models [19], [20], [21].
The inclination to specialize in general practice is known to decrease over the course of medical study, something that is attributed to competition with other clinical specialties [2]. A reversed increase in motivation could possibly be expected as a result of supervised courses/internships in general medicine and ambulant care that are offered earlier in the curriculum and over the long term, and which are ultimately embedded in the overall medical program. Even in this context, the expectations, prior knowledge and experiences of the students should be systematically integrated in respect to the FHV [15], [18], [22].
In conformance with other studies, our survey revealed a tendency in female and older students to select a specialty in outpatient care, in particular general practice. This could possibly have its roots in the expectations of family-friendly work schedules and employment models [2], [12], [14]. The tendency for place of study to have importance concerning the inclination to specialize in general practice has already been described for Bavarian universities as the factor of institutionalization: the more present and convincing the teaching of a subject in the medical program, the more likely this subject is to be considered when selecting a specialty [23].
Strengths and weaknesses:
Our survey is representative for Saxony-Anhalt, the federal German state with the lowest number of physicians per capita and geographical area. It is not, however, reflective of all Germany, since only 5% of all medical students were surveyed. Especially the different native regions of the students could have caused a bias in the results. Presumably there are changes in attitudes toward the field of general practice among the students who have and who have not completed the FHV (or who will have completed the FHV at a later date) which we were unable to uncover as a consequence of having too small a sample size and the cross-sectional nature of the study. In addition, confusing information given by students about the status of their clerkships made the analysis more difficult due to reduced case numbers. The time point for the study of students finishing their third year of medical study in July 2013 represents another possible source of bias, since these students only had narrow windows of time following the preliminary medical examination (Physikum) to complete an FHV. The extent to which an “(as of yet) unplanned FHV” means that this will not be reconsidered in the future was not separately addressed on our questionnaire. In regard to questions about specialty selection, our survey was directed toward a population whose decisions are often not yet final, presumably still subject to change through future events, and accordingly our questions about this have a more hypothetical character [24].
In the future and at more advanced semester levels, the percentage of completed FHVs will increase and possibly result in changes in the responses to questions about specialty choice. This is to be particularly expected if those students for whom the FHV is required are also surveyed, and who as a larger, more representative sample should then be investigated longitudinally with validated instruments.
Conclusions
To date, the FHV has demonstrated no determinable effects on the later specialty choices made by students. In future, the effects of medical teacher training programs, journals and systematic evaluation during the FHV should also be investigated over the long term, as should the issue regarding fair remuneration for medical teachers and coordination by the universities, especially in regard to the influence on specialty selection.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Deutscher Bundestag. Sachverständigenrat zur Begutachtung der Entwicklung im Gesundheitswesendes. Sondergutachten des Sachverständigenrates 2009. Koordination und Integration – Gesundheitsversorgung in einer Gesellschaft des längeren Lebens. Berlin: Deutscher Bundestag; 2009. Available from: http://dip21.bundestag.de/dip21/btd/16/137/1613770.pdf. [Google Scholar]
- 2.Kruschinski C, Wiese B, Hummers-Pradier E. Einstellungen zur Allgemeinmedizin: eine vergleichende querschnittliche Befragung von Medizinstudierenden des 1. und 5. Studienjahres. GMS Z Med Ausbild. 2012;29(5):Doc71. doi: 10.3205/zma000841. Available from: http://dx.doi.org/10.3205/zma000841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Behmann M, Schmiemann G, Lingner H, Kühne F, Hummers-Pradier E, Schneider N. Job satisfaction among primary care physicians: results of a survey. Dtsch Arztebl Int. 2012;109(11):193–200. doi: 10.3238/arztebl.2012.0193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Buddeberg-Fischer B, Stamm M, Buddeberg C, Klaghofer R. Möglichkeiten zur Attraktivitätssteigerung der Hausarztmedizin aus Sicht junger Ärztinnen und Ärzte. Gesundheitswes. 2008;70:123–128. doi: 10.1055/s-2008-1062721. Available from: http://dx.doi.org/10.1055/s-2008-1062721. [DOI] [PubMed] [Google Scholar]
- 5.Gibis B, Heinz A, Jacob R, Müller CH. Berufserwartungen von Medizinstudierenden: Ergebnisse einer bundesweiten Befragung. Dtsch Arztebl Int. 2012;109(18):327–332. doi: 10.3238/arztebl.2012.0327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roick C, Heider D, Günther OH, Kürstein B, Riedel-Heller SG, König HH. Was ist künftigen Hausärzten bei der Niederlassungsentscheidung wichtig? Ergebnisse einer postalischen Befragung junger Ärzte in Deutschland. Gesundheitswes. 2012;74:12–20. doi: 10.1055/s-0030-1268448. Available from: http://dx.doi.org/10.1055/s-0030-1268448. [DOI] [PubMed] [Google Scholar]
- 7.Stengler K, Heider D, Roick C, Günther OH, Riedel-Heller S, König HH. Weiterbildungsziel und Niederlassungsentscheidung bei zukünftigen Fachärztinnen und Fachärzten in Deutschland, eine genderspezifische Analyse. Bundesgesundheitsbl. 2012;55:121–128. doi: 10.1007/s00103-011-1397-8. Available from: http://dx.doi.org/10.1007/s00103-011-1397-8. [DOI] [PubMed] [Google Scholar]
- 8.Sambunjak D, Straus SE, Marusic A. Mentoring in academic medicine: a systematic review. JAMA. 2006:206(9):1103–1115. doi: 10.1001/jama.296.9.1103. Available from: http://dx.doi.org/10.1001/jama.296.9.1103. [DOI] [PubMed] [Google Scholar]
- 9.Hermann K, Buchholz A, Loh A, Kiolbassa K, Miksch A, Joos S, Götz K. Entwicklung, faktorenanalytische Überprüfung und psychometrische Evaluation eines Fragenbogens zur Gebietswahl von Medizinstudenten. Gesundheitswes. 2012;74:426–434. doi: 10.1055/s-0031-1280845. Available from: http://dx.doi.org/10.1055/s-0031-1280845. [DOI] [PubMed] [Google Scholar]
- 10.Dunker-Schmidt C, Breetholt A, Gesenhues S. Blockpraktikum in der Allgemeinmedizin: 15 Jahre Erfahrung an der Universität Duisburg-Essen. Z Allg Med. 2009;85(4):170–175. [Google Scholar]
- 11.Cruess SR, Cruess RL, Steinert Y. Role modelling-making the most of a powerful teaching strategy. BMJ. 2008;336:718–721. doi: 10.1136/bmj.39503.757847.BE. Available from: http://dx.doi.org/10.1136/bmj.39503.757847.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kruschinski C, Wiese B, Eberhard J, Hummers-Pradier E. Einstellungen von Studierenden zur Allgemeinmedizin: Einflüsse von Geschlecht, Blockpraktikum und Gesamtcurriculum. GMS Z Med Ausbild. 2011;28(1):Doc16. doi: 10.3205/zma000728. Available from: http://dx.doi.org/10.3205/zma000728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schäfer HM, Sennekamp M, Güthlin C, Krentz H, Gerlach F. Kann das Blockpraktikum Allgemeinmedizin zum Beruf des Hausarztes motivieren? Z Allg Med. 2009;86(3):109–112. [Google Scholar]
- 14.Van der Zwet J, Zwietering PJ, Teunissen PW, van der Vleuten CP, Scherpbier AJ. Workplace learning from a social-cultural perspective: creating developmental space during the general practice clerkship. Adv Health Sci Educ. 2011;16:359–373. doi: 10.1007/s10459-010-9268-x. Available from: http://dx.doi.org/10.1007/s10459-010-9268-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kraus B, Jünger J, Schrauth M, Weyrich P, Herzog W, Zipfel S, Nikendei C. Logbücher im klinisch-praktischen Einsatz: Profitieren die Studenten? Eine Bestandaufnahme bei PJ-Studenten der Inneren Medizin. GMS Z Med Ausbild. 2007;24(2):Doc112. Available from: http://www.egms.de/static/de/journals/zma/2007-24/zma000406.shtml. [Google Scholar]
- 16.Senf JH, Campos-Outcalt D, Kutob R. Factors related to the choice of family medicine: a reassessment and literature review. J Am Board Fam Pract. 2003;16(6):502–512. doi: 10.3122/jabfm.16.6.502. Available from: http://dx.doi.org/10.3122/jabfm.16.6.502. [DOI] [PubMed] [Google Scholar]
- 17.Howe A, Ives G. Does community-based experience alter career preference? New evidence from a prospective longitudinal cohort study of undergraduate medical students. Med Educ. 2001;35(4):391–397. doi: 10.1046/j.1365-2923.2001.00866.x. Available from: http://dx.doi.org/10.1046/j.1365-2923.2001.00866.x. [DOI] [PubMed] [Google Scholar]
- 18.Sinclair HK, Ritchie LD, Lee AJ. A future carrer in general practice? A longitudinal study of medical students and preregistration house officers. Eur J Gen Pract. 2006;12(3):120–127. doi: 10.1080/13814780600780833. Available from: http://dx.doi.org/10.1080/13814780600780833. [DOI] [PubMed] [Google Scholar]
- 19.Steinhäuser J, Annan N, Roos M, Szecsenyi J, Joos S. Lösungsansätze gegen den Allgemeinarztmangel auf dem Land - Ergebnisse einer online Befragung unter Ärzten in Weiterbildung. DMW. 2011;136:1715–1719. doi: 10.1055/s-0031-1272576. Available from: http://dx.doi.org/10.1055/s-0031-1272576. [DOI] [PubMed] [Google Scholar]
- 20.Schwarz MD, Basco WT, Grey MR, Elmore JG, Rubenstein A. Rekindling student interest in general careers. Ann Intern Med. 2005;142(8):715–714. doi: 10.7326/0003-4819-142-8-200504190-00040. Available from: http://dx.doi.org/10.7326/0003-4819-142-8-200504190-00040. [DOI] [PubMed] [Google Scholar]
- 21.Miettola J, Mäntyselkä P, Vaskilampi T. Doctor-patient interaction in Finnisch primary health care as perceived by first year medical students. BMC Med Educ. 2005;5:34. doi: 10.1186/1472-6920-5-34. Available from: http://dx.doi.org/10.1186/1472-6920-5-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Trachsel S, Schuafelberger M, Feller S, Küng L, Frey P, Guttormsen Schär S. Evaluation eines neuen Mentoring-Programmes für Medizinstudierende in der hausärztlichen Grundversorgung: Erfahrungen von Studierenden und Lehrärzten. GMS Z Med Ausbild. 2010;27(3):Doc42. doi: 10.3205/zma000679. Available from: http://dx.doi.org/10.3205/zma000679. [DOI] [Google Scholar]
- 23.Schneider A, Karsch-Völk M, Rupp A, Fischer MR, Drexler H, Schelling J, Berberat P. Determinanten für eine hausärztliche Berufswahl unter Studierenden der Medizin: Eine Umfrage an drei bayrischen Medizinischen Fakultäten. GMS Z Med Ausbild. 2013;30(4):Doc45. doi: 10.3205/zma000888. Available from: http://dx.doi.org/10.3205/zma000888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kiolbassa K, Miksch A, Hermann K, Loh A, Szecsenyi J, Joos S, Goetz K. Becoming a general practitioner – Which factors have most impact on career choice of medical students? BMC Fam Pract. 2011;12:25. doi: 10.1186/1471-2296-12-25. Available from: http://dx.doi.org/10.1186/1471-2296-12-25. [DOI] [PMC free article] [PubMed] [Google Scholar]