Abstract
The central hypothesis of functional tissue engineering is that an engineered construct can serve as a viable replacement tissue in vivo by replicating the structure and function of native tissue. In the case of articular cartilage, this requires the reproduction of the bulk mechanical and surface lubrication properties of native hyaline cartilage. Cartilage tissue engineering has primarily focused on achieving the bulk mechanical properties of native cartilage such as the compressive aggregate modulus and tensile strength. A scaffold-free self-assembling process has been developed that produces engineered cartilage with compressive properties approaching native tissue levels. Thus, the next step in this process is to begin addressing the friction coefficient and wear properties of these engineered constructs. The superficial zone protein (SZP), also known as lubricin or PRG4, is a boundary mode lubricant that is synthesized by surface zone (SZ) articular chondrocytes. Under conditions of high loading and low sliding speeds, SZP reduces friction and wear at the articular surface. The objective of this investigation was to determine whether increasing the proportion of SZ chondrocytes in cartilage constructs, in the absence of external stimuli such as growth factors and mechanical loading, would enhance the secretion of SZP and improve their frictional properties. In this study, cartilage constructs were engineered through a self-assembling process with varying ratios of SZ and middle zone (MZ) chondrocytes (SZ:MZ): 0:100, 25:75, 50:50, 75:25, and 100:0. Constructs containing different ratios of SZ and MZ chondrocytes did not significantly differ in the glycosaminoglycan composition or compressive aggregate modulus. In contrast, tensile properties and collagen content were enhanced in nearly all constructs containing greater amounts of SZ chondrocytes. Increasing the proportion of SZ chondrocytes had the hypothesized effect of improving the synthesis and secretion of SZP. However, increasing the SZ chondrocyte fraction did not significantly reduce the friction coefficient. These results demonstrate that additional factors, such as SZP-binding macromolecules, surface roughness, and adhesion, need to be examined to modulate the lubrication properties of engineered cartilage.
Introduction
The goal of cartilage tissue engineering is to provide an improved treatment for articular cartilage degeneration observed in osteoarthritis. Current clinical strategies for treating damaged cartilage, including microfracture surgery,1–3 autologous chondrocyte implantation,4 and osteochondral grafting,2,4–6 have achieved modest success. However, in general, these approaches have been unable to completely regenerate and restore hyaline cartilage. By generating viable tissue replacements that mimic the structure and function of native tissue, tissue engineering will overcome the limitations of current clinical strategies for treating small focal defects in articular cartilage. One of the main challenges of tissue engineering has been to create tissue substitutes with mechanical properties on par with native tissue to function under in vivo loading. Using a scaffold-free self-assembling process, articular cartilage constructs have been engineered with compressive properties approaching those of native tissue.7,8 However, to maintain the bulk mechanical integrity of the tissue, engineered cartilage must also include surface lubrication and a low friction coefficient; the other defining features of articular cartilage.
Articular cartilage is an anisotropic tissue consisting of three structurally distinct zones, each having unique biochemical and biomechanical properties.9,10 The surface zone (SZ), which comprises 10–20% of the total cartilage thickness, contains low proteoglycan content and flattened discoid cells referred to as SZ articular chondrocytes.11 These cells are embedded in an organized type II collagen matrix aligned parallel to the articular surface that resists shear and tensile forces.11,12 The middle zone (MZ) comprises 40–60% of the total cartilage thickness and consists of larger, spherical MZ chondrocytes surrounded by a randomly oriented type II collagen matrix. Of the three zones, MZ cells produce the greatest amount of proteoglycans, which contribute to the tissue's compressive integrity.11,12 The deep zone comprises the remaining 30% of the tissue thickness, with the chondrocytes in this region arranged in a columnar manner. The type II collagen matrix is aligned perpendicular to the articular surface and extends into a calcified matrix, anchoring the tissue to the subchondral bone.12
The superficial zone protein (SZP) is a characteristic glycoprotein of the SZ and is localized at the articular surface.13 It is produced by synoviocytes and superficial zone chondrocytes14 but virtually not produced by middle or deep zone chondrocytes.13 SZP plays an important role in the boundary lubrication of synovial joints by reducing friction and wear at the articular surface, thereby maintaining the mechanical integrity of the cartilage.15–20 Also known as lubricin (227 kDa) or PRG4 (460 kDa), SZP (345 kDa) is a product of the prg4 gene.15,21 This boundary lubricant is localized and expressed in other tissues as well, including tendons,22 ligaments,23 and in the pericardium,15 where it has also been proposed to act as a boundary lubricant. The boundary mode friction coefficient of cartilage either sliding against cartilage or glass in the presence of SZP has been reported to be ∼0.02 to 0.04.24–27 In bovine femoral condyles, SZP synthesis was found to correlate with mechanical loading.26
In previous studies, self-assembled constructs have been generated from primary chondrocytes isolated from the SZ and MZ of bovine articular cartilage.8,28 Due to the differences in thickness between the two zones, these self-assembled constructs possessed a smaller abundance of SZ chondrocytes in comparison to MZ cells.29 Thus, the primary objective of this study was to determine whether improving the production of SZP by increasing the number of SZ chondrocytes would enhance the frictional properties of self-assembled articular cartilage. The seeding density was unaltered since a previous study demonstrated that the biochemical and biomechanical properties of constructs vary according to seeding density.30 This additional variable would confound the analysis of the primary objective, and thus, the seeding density was kept constant. The SZ to MZ cell ratios (0:100, 25:75, 50:50, 75:25, and 100:0) were generated and self-assembled, using the 25:75 group as the control for a typical self-assembled articular cartilage construct. Since altering the phenotypic composition of self-assembled cartilage may affect its bulk mechanical properties, the secondary objective was to examine the effects of varying the ratio of SZ and MZ chondrocytes on the mechanical and biochemical properties of self-assembled cartilage. The results of this investigation suggest that additional factors may need to be considered when attempting to modulate the frictional properties of engineered cartilage.
Materials and Methods
Chondrocyte isolation
As described previously, bovine chondrocytes were isolated14,31 and self-assembled.8,28 Briefly, articular cartilage was harvested from 1- to 3-month-old bovine stifle joints obtained from a local abattoir. The SZ of femoral condyle articular cartilage (∼100 μm thick) was harvested using a dermatome. MZ articular cartilage was harvested from the subsequent layer (∼1 mm thick) using a scalpel blade. Cartilage slices were finely minced into ∼1 mm pieces and digested in Digestion Media (DM) consisting of 0.2% Collagenase P (Roche) in a chemically defined medium (Medium-A) consisting of Dulbecco's modified Eagle's medium (DMEM), containing 4.5 mg/mL glucose and GlutaMAX (Gibco), and supplemented with 100 nM dexamethasone (Sigma), 1% penicillin/streptomycin (Invitrogen), 0.5% Fungizone (Invitrogen), 50 μg/mL ascorbate-2-phosphate, 40 μg/mL l-proline, and 100 μg/mL sodium pyruvate. The DM also contained 3% fetal bovine serum (FBS; Gibco). The SZ cartilage was digested for 2 h. The MZ cartilage was incubated in the DM for 6 h. The released chondrocytes were filtered through a cell strainer (70 μm; BD Falcon), washed in Medium-A containing 10% FBS, and the cell number determined using a hemocytometer. Cells were then frozen in DMEM containing 10% dimethyl sulfoxide (Sigma) and 20% FBS at −80°C. Thawed SZ and MZ chondrocytes were again counted, assessed for viability (>70%) using the trypan blue exclusion test, and then mixed into five SZ:MZ ratios (0:100, 25:75, 50:50, 75:25, and 100:0) before seeding in 5-mm-diameter, nonadherent cylindrical wells made of 2% agarose.
Self-assembly of engineered cartilage constructs
Nonadherent agarose wells were prepared by placing sterile stainless steel molds consisting of 5-mm-diameter×10-mm-long cylindrical prongs into a 48-well plate containing 1 mL/well of molten 2% agarose (Fisher Scientific) in phosphate-buffered saline (PBS).8,28 After the agarose solidified at room temperature, the mold was removed and the agarose was perfused with Medium-A supplemented with 1% ITS+ Premix (BD Biosciences) (culture medium). Into each well, 4 million live cells were seeded in 100 μL of serum-free culture media, followed by an additional 400 μL of media 4 h later. Full media changes were then performed daily for the entire culture duration (4 weeks). All engineered tissues were cultured at 37°C in a moist atmosphere containing 5% carbon dioxide. On the fifth day of culture, constructs were unconfined and transferred to nonadherent tissue culture plates coated with a thin layer of agarose. Following 4 weeks of culture, constructs were processed for gross morphology, histology, quantitative biochemistry, and mechanical testing.
Gross morphology, histology, and immunohistochemistry
Construct dimensions were measured using ImageJ (National Institutes of Health). For histology, constructs were fixed in Bouin's solution (Sigma) for 24 h, followed by paraffin embedding and sectioning (4 μm thick). Samples were stained with Toluidine blue to examine glycosaminoglycan (GAG) content. For immunohistochemistry (IHC), slides were deparaffinized using xylene and rehydrated with graded ethanol, quenched of peroxidase activity with hydrogen peroxide, and blocked with 1% bovine serum albumin (BSA). SZP immunostaining was performed according to standard methods26,32 using the monoclonal antibody S6.79 (1:1000 dilution) as the primary antibody. To expose collagen epitopes, samples were pretreated with Proteinase K (Sigma). Collagen type I and II immunostaining utilized mouse monoclonal antibodies (Pierce) at 1:200 dilution. The signal detection for all immunostaining was performed using a mouse IgG secondary antibody with an avidin-biotin-peroxidase kit (Vector Laboratories) following the manufacturer's directions. As a comparison, 5 mm diameter explants were obtained from bovine femoral condyles, cut to a thickness of ∼400 μm (SZ), and processed for histology and IHC.26
Friction testing
The friction coefficients of the constructs were determined using a pin-on-disk tribometer operated in the boundary lubrication regime in reciprocating sliding mode, as described previously.26,27 Briefly, a 5 mm punch was taken from the center of each construct, affixed to acrylic pins by ethyl cyanoacrylate, and then brought into contact with a polished glass disk while fully immersed in PBS. Before the initiation of each friction test, the sample was allowed to equilibrate unconfined under the applied load (0.1 MPa) for 2 min to minimize any fluid effects during testing. The test duration of each friction experiment was fixed at 5 min at a sliding speed of 0.5 mm/s.26 Data were collected (Daqview; IOtech) and processed using a standard software package (Microsoft). As a comparison, native SZ and MZ cartilages (∼400 μm thick) were also measured.
SZP detection and quantification
SZP accumulation in the media was determined by sodium dodecyl sulfate–polyacrylamide gel electrophoresis and immunoblotting. After electrophoresis, the separated proteins were transferred to a PVDF membrane. The membrane was blocked with 5% nonfat dry milk in tris-buffered saline with tween (TBST; 25 mM Tris HCl, 125 mM NaCl, and 0.1% Tween 20) for 2 h and incubated overnight at 4°C with the monoclonal antibody S6.79 at a 1:5000 dilution. The membrane was then incubated with goat anti-rabbit IgG conjugated with horseradish peroxidase (Bio-Rad) at a 1:3000 dilution for 1 h, followed by a 1-min incubation with the SuperSignal West Pico Chemiluminescent Substrate (Thermo Fisher Scientific), and imaged with film.
SZP accumulation in the media was quantified by enzyme-linked immunosorbent assay (ELISA)32,33 using SZP purified from the bovine synovial fluid as a standard. Each well of 96-well MaxiSorp plates (Nalge Nunc International) was coated with 1 μg/mL peanut lectin (EY Laboratories) in a 50 mM sodium carbonate buffer (pH 9.5). The wells were then blocked with 1% BSA in the same buffer. Aliquots of culture medium from days 8 to 14, the monoclonal antibody S6.79 (1:5000 dilution), and horseradish peroxidase-conjugated goat anti-mouse IgG (1:3000) were sequentially incubated for 1 h each in the wells. Finally, the SuperSignal ELISA Femto Maximum Sensitivity Substrate (Thermo Fisher Scientific) was applied, and the chemiluminescence of each well was measured. Wells were washed with PBS containing 0.05% Tween 20 (Sigma) between all steps. SZP levels were calculated using a SZP standard purified by affinity chromatography on a peanut lectin column; SZP was verified by immunoblot analysis and quantified using a Micro BCA Protein Assay Kit (Pierce).33
Biochemical composition analysis
Constructs and native tissue were frozen overnight and lyophilized for 48 h, after which the dry weights were obtained. They were then digested in 125 μg/mL papain (Sigma) in phosphate buffer (pH 6.5) containing 2 mM N-acetyl-l-cysteine (Sigma) and 2 mM EDTA for 18 h at 60°C. The GAG content was quantified through a 1,9-dimethylmethylene blue binding assay using a commercially available kit according to the manufacturer's directions (Blyscan GAG Assay; Biocolor). Total collagen was quantified after hydrolyzing samples with 2 N NaOH for 20 min at 120°C using a chloramine-T hydroxyproline assay with trans-4-hydroxyl-l-proline (Sigma) as a standard, assuming a 12.5% hydroxyproline content in collagen.34
Compressive and tensile testing
The compressive aggregate modulus was determined using a creep indentation apparatus.35 A 3 mm diameter punch was taken from the center of each construct, attached to a flat stainless steel surface with a thin layer of cyanoacrylate glue, and allowed to equilibrate for 20 min in PBS. The sample was then placed into the creep indentation apparatus, which automatically loaded and unloaded the specimen while recording the tissue's creep and recovery behavior. A tare load of 0.2 g, followed by a test load of 0.7 g (2.0 g for native tissue), was applied to all samples with a 1-mm-diameter, flat-ended, porous rigid tip. All loads were applied until equilibrium was reached. To calculate the specimen's aggregate modulus, a semianalytical, seminumeric, linear biphasic model was used.36
Tensile mechanical properties were determined using the Test Resources 840L.37 Briefly, 3 mm punches were used to trim construct samples and generate a dog-bone shape, which were glued to paper tabs to establish a gauge length of 1.45 mm. Samples were loaded at a constant rate of 1% strain per second. The Young's modulus and ultimate tensile strength (UTS) were quantified from stress–strain curves generated from the load–displacement results.
Statistics
Biochemical and biomechanical testing of self-assembled cartilage and native tissue consisted of a sample size of n=6 and n=9, respectively. A sample size of n=8 was used for SZP ELISA and n=2 for histology and IHC. To determine if construct composition was a significant factor, a one-way analysis of variance (ANOVA) followed by Tukey's post hoc test was performed. Groups not connected by the same letter are significantly different. A Student's t-test was performed on surface and MZ native articular cartilage, with a p-value of <0.05 considered significant.
Results
Gross morphology, histology, and IHC
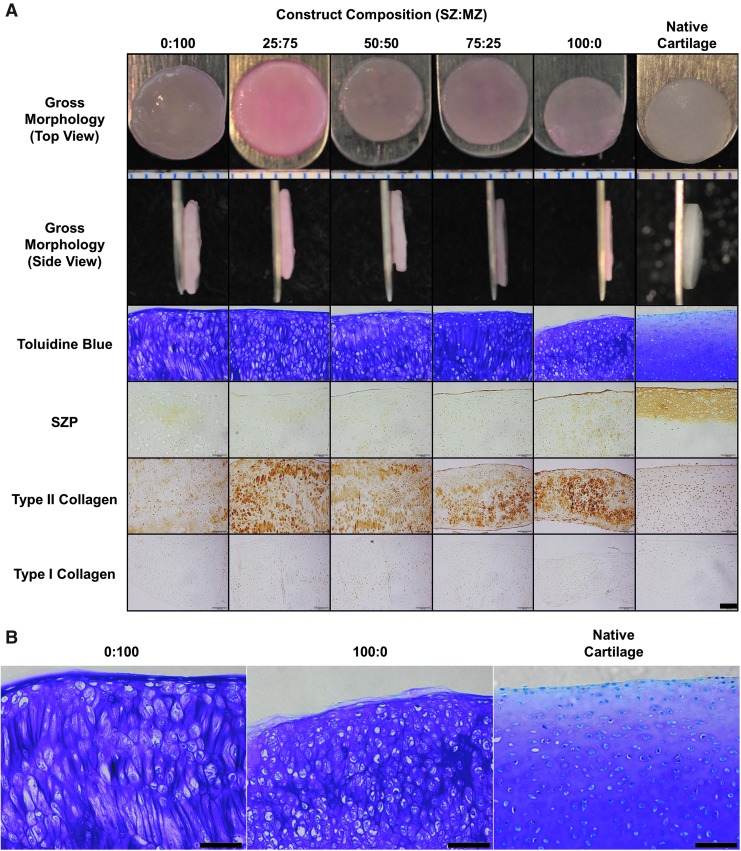
All constructs appeared flat and thin (Fig. 1A). Toluidine blue staining revealed the presence of sulfated GAG in all constructs. Metachromasia was more intense in the engineered constructs compared to the SZ and MZ in the native cartilage control. There were no apparent differences between the construct groups. The SZP was minimally detected in 0:100 (SZ:MZ) constructs and increased in constructs consisting of increasing numbers of SZ chondrocytes. While nonspecific or artifactual staining cannot be completely ruled out, the edge staining of SZP is likely due to comparable edge staining in native tissues. Compared to the SZ native cartilage control, there was less SZP immunolocalization throughout the engineered constructs. IHC revealed the presence of type II collagen in all constructs, with a slight decrease in staining intensity for MZ constructs (0:100). Type I collagen was not detected in either the constructs or native cartilage control. The wet weight, hydration, diameter, and thickness of constructs all increased along with the MZ chondrocyte content (Table 1). Regarding cell morphology, SZ chondrocytes did not retain the flattened discoid-shaped morphology as in native tissue. There were no significant differences between SZ and MZ chondrocytes, except that MZ chondrocytes appeared larger than SZ chondrocytes, as expected (Fig. 1B).
FIG. 1.
Gross morphology, histology, and immunohistochemistry (IHC) of constructs and native articular cartilage. (A) The gross morphology from a top (row 1) and side view (row 2) of constructs after t=4 weeks of culture and native bovine articular cartilage is shown (ruler segments=1 mm). Histology sections were stained with toluidine blue to detect sulfated glycosaminoglycans (GAGs) (row 3). IHC was performed on sections for superficial zone protein (SZP) (row 4), type II collagen (row 5), and type I collagen (row 6) (scale bar: 100 μm). (B) Images of middle zone (MZ) constructs (0:100), surface zone (SZ) constructs (100:0), and native cartilage were enlarged to display chondrocyte morphologies (scale bar: 100 μm).
Table 1.
Physical Properties of Constructs After 4 Weeks of Culture
| Construct composition (SZ:MZ) | Wet weight (mg) | Hydration (%) | Diameter (mm) | Thickness (mm) |
|---|---|---|---|---|
| 0:100 | 32.6±1.4a | 87±2a | 6.2±0.1a | 0.92±0.05a |
| 25:75 | 24.0±3.1b | 85±2a,b | 6.1±0.1b | 0.72±0.06b |
| 50:50 | 17.8±2.4c | 84±2b,c | 5.4±0.1c | 0.66±0.10b |
| 75:25 | 16.9±1.6c | 84±3c | 5.7±0.1c | 0.51±0.06c |
| 100:0 | 9.7±0.5d | 81±3c | 5.3±0.1d | 0.37±0.06d |
The diameter, thickness, wet weight, and hydration of constructs were measured. Construct size and hydration increased with increasing proportion of MZ chondrocytes. Values are presented as mean±SD.
Within a column, groups not sharing an identical alphabet are significantly different from one another (p<0.05). For each metric, each group was significantly differnt from all others.
MZ, middle zone; SZ, surface zone.
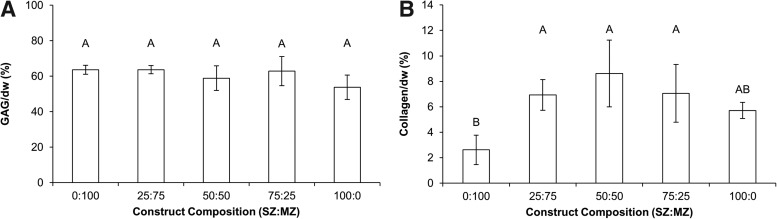
Biochemical content
The percentage of GAG per dry weight of the 0:100, 25:75, 50:50, 75:25, and 100:0 (SZ:MZ) constructs was 64%±3%, 64%±2%, 59%±7%, 63%±8%, and 54%±7%, respectively (Fig. 2A). There were no significant differences in GAG content on a dry weight basis among the experimental construct groups. Collagen per dry weight for the 0:100, 25:75, 50:50, 75:25, and 100:0 (SZ:MZ) constructs was 2.6%±1.2%, 6.9%±1.2%, 8.6%±2.6%, 7.1%±2.3%, and 5.7%±0.6%, respectively (Fig. 2B). MZ constructs (0:100) contained significantly less collagen than constructs containing a combination of SZ and MZ cells (25:75, 50:50, and 75:25). There were no significant differences between SZ constructs (100:0) and the remaining groups. In the native tissue controls, MZ cartilage had significantly more GAG and collagen than SZ cartilage. Compared to the engineered constructs, native tissue contained fewer GAGs but more collagen per dry weight. GAG per dry weight for native MZ and SZ was 36%±3% and 29%±4%, respectively. Collagen per dry weight for native MZ and SZ was 47%±13% and 32%±3%, respectively.
FIG. 2.
Biochemical properties of constructs after 4 weeks of culture. GAG (A) and collagen content (B) of each construct was assayed using the dimethylmethylene blue and hydroxyproline assays, respectively. All values are normalized by construct dry weight (dw). There were no significant differences in GAG between groups. Collagen content was significantly lower in the 100% MZ constructs compared to all other groups, with the exception of 100% SZ constructs. Values are presented as mean±SD.
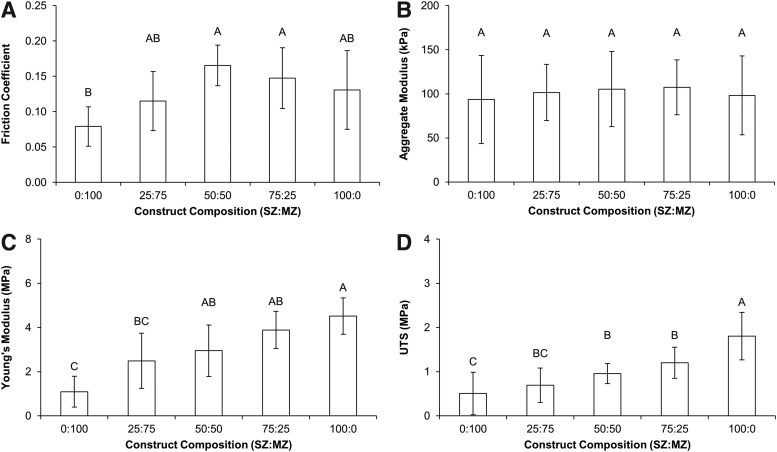
Mechanical properties
Changing the relative amounts of SZ and MZ chondrocytes in the engineered cartilage did not significantly affect the compressive mechanical properties of the constructs. The aggregate moduli of the 0:100, 25:75, 50:50, 75:25, and 100:0 (SZ:MZ) constructs were 94±50, 102±32, 105±43, 107±31, and 98±45 kPa, respectively (Fig. 3B). On the other hand, increasing the SZ chondrocyte content of constructs enhanced the tensile properties as measured by the Young's modulus (Fig. 3C) and UTS (Fig. 3D). The Young's moduli and UTS of the 0:100, 25:75, 50:50, 75:25, and 100:0 (SZ:MZ) constructs were 1.1±0.7, 2.5±1.2, 2.9±1.2, 3.9±0.8, and 4.5±0.8 MPa and 0.5±0.5, 0.7±0.4, 1.0±0.2, 1.2±0.4, and 1.8±0.5 MPa, respectively. For native cartilage, the MZ was found to be stiffer in compression and tension compared with the SZ. MZ cartilage had an aggregate modulus of 457±124 kPa, Young's modulus of 59±19 MPa, and UTS of 25±8 MPa, whereas SZ cartilage had an aggregate modulus of 211±106 kPa, Young's modulus of 21±9 MPa, and UTS of 10±4 MPa.
FIG. 3.
Biomechanical properties of constructs after 4 weeks of culture. The boundary mode friction coefficient (A), aggregate modulus (B), Young's modulus (C), and ultimate tensile strength (D) of the constructs were measured. The friction coefficient of engineered constructs was significantly lowest in the 100% MZ constructs. There were no significant differences in frictional properties between the other construct groups. The friction coefficient of 100% MZ constructs approached the value of native MZ articular cartilage. There were no statistically significant differences between constructs in the compressive mechanical properties measured. However, tensile properties were enhanced in constructs composed of greater proportions of SZ chondrocytes. Values are presented as mean±SD.
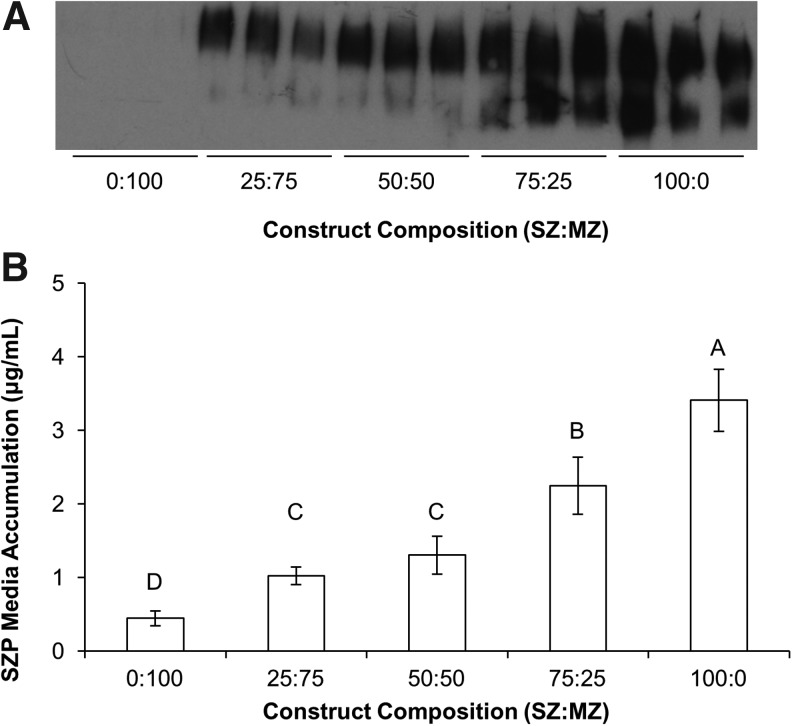
SZP and friction characteristics
The SZP production from the engineered constructs was measured through SZP accumulation in the media cultured over days 8–14 by both qualitative immunoblotting (Fig. 4A) and quantitative ELISA (Fig. 4B). Increasing the proportion of SZ chondrocytes in the constructs had the intended effect of enhancing SZP synthesis. The boundary mode friction coefficient, however, did not concomitantly decrease with increased SZP synthesis (Fig. 3A). The friction coefficient values for the 0:100, 25:75, 50:50, 75:25, and 100:0 (SZ:MZ) constructs were 0.08±0.03, 0.12±0.04, 0.17±0.03, 0.15±0.04, and 0.13±0.06, respectively. The 50:50 and 75:25 constructs exhibited the highest friction coefficient, whereas the 0:100 constructs possessed the lowest frictional properties. The 25:75 and 100:0 constructs had intermediate values of friction that did not significantly differ from the other groups. The friction coefficient of native SZ and MZ cartilage was measured as 0.02±0.01 and 0.06±0.02, respectively.
FIG. 4.
SZP synthesis increases in constructs containing greater proportions of SZ chondrocytes. Immunoblotting (A) and enzyme-linked immunosorbent assay (ELISA) (B) demonstrated that SZP media accumulation in culture from days 8 to 14 was significantly enhanced in constructs composed of greater amounts of SZ chondrocytes. Three separate media samples were randomly chosen from a total of eight and assayed per construct group. Media accumulation results were confirmed and quantified through ELISA (n=8). Values are presented as mean±SD.
Discussion
The objective of this investigation was to improve the frictional properties of engineered cartilage by enhancing the production of the boundary lubricant, SZP. To accomplish this aim, engineered cartilage was generated by varying the proportions of SZ and MZ (SZ:MZ—0:100, 25:75, 50:50, 75:25, 100:0) chondrocytes to determine whether SZP production could be increased by increasing the number of SZP-secreting cells. The 25:75 (SZ:MZ) constructs are representative of a typical self-assembled construct. Modulation of the zonal composition of constructs had no effect on their compressive properties, but construct tensile properties were significantly improved with the addition of SZ chondrocytes. Increasing the fraction of SZ chondrocytes also increased SZP production as measured by media accumulation. However, construct frictional properties did not improve with increasing SZP synthesis. This investigation is the first to explore the effects of SZ chondrocytes on the lubrication and bulk mechanical properties of engineered cartilage produced from a scaffold-free self-assembling process and suggests that modulation of the frictional properties of engineered cartilage may entail other factors in addition to SZP production, such as SZP-binding macromolecules, surface roughness, and adhesion.
Increasing the proportion of SZ chondrocytes in self-assembled constructs did not result in a reduced friction coefficient (Fig. 3A) despite the attendant increase in SZP production (Fig. 4). To gain a clearer picture of the friction and wear characteristics of engineered tissues, additional parameters besides SZP synthesis and the coefficient of friction may be required. In addition to the presence of a protein-based boundary lubricant, surface roughness and adhesion also contribute to friction.38 For example, interleukin-1β, a catabolic cytokine, has been shown to increase the surface roughness of cartilage and reduce friction since roughening decreases the interfacial contact area during sliding.27 However, surface roughening may not be desired as it can promote wear of the tissues.27 Furthermore, adhesive forces at the cartilage surface are reduced in regions of cartilage expressing more SZP.39,40 Although SZP IHC is only a semiquantitative assessment, low levels of SZP staining in the engineered constructs compared to native tissue suggest poor retention of the boundary lubricant. In order for SZP to effectively reduce friction, it must be able to bind to the cartilage surfaces.16,41 These factors need to be examined in future studies to gain a clearer picture of how surface roughness and adhesion are affected by the zonal composition of constructs.
Compared to native articular cartilage, all the self-assembled constructs in this investigation contained more GAG and less collagen per dry weight. The GAG (Fig. 2A) and compressive stiffness (Fig. 3B) results are surprising since native SZ cartilage produces less GAG and has lower compressive properties than native MZ cartilage. Therefore, the compressive properties of constructs consisting of more SZ chondrocytes were expected to decrease. However, the GAG content was not affected by the number of SZ chondrocytes as the compressive properties were maintained at ∼100 kPa, the level generally observed in self-assembled constructs. Furthermore, the overproduction of GAG in the self-assembled tissue did not yield compressive properties on par with native tissue. Both these phenomena are likely due to the under-production of collagen. Collagen has been shown to play a role in improving the compressive properties of articular cartilage by prestressing the matrix.42,43 These findings suggest that a balance of both GAG and collagen is needed to contribute to the mechanical properties of engineered constructs.
The development of a strong type II collagen matrix to support tensile loads has been a long-standing challenge in cartilage tissue engineering.7,8,44,45 Excess GAG and high cellularity may be inhibiting development of the collagen matrix. Chondrocytes in vitro may synthesize excess GAG to recreate the hyperosmotic environment they experience in vivo in native tissue.46 In addition, retention of secreted collagen may also be an issue since engineered cartilage has been shown to retain little collagen. Despite these details, the tensile properties of constructs improved with increasing proportions of SZ chondrocytes (Fig. 3C, D) and without consistent increases in the total collagen content.7,45 We hypothesize that the collagen in constructs with greater proportions of SZ chondrocytes is more organized or has a greater crosslinking, which would explain the increase in tensile stiffness and strength. As one of the limitations of this study, the relationship between the construct tensile stiffness and collagen content cannot be readily explained by the presented data.
Typical self-assembled scaffold-free constructs possess a Young's modulus of around 0.6–1.8 MPa.7,28,45 The 0:100 and 25:75 SZ to MZ ratio constructs, which are indicative of the typical self-assembled construct, have comparable Young's moduli of ∼1.1 and 2.5 MPa, respectively. The compressive stiffness of hydrogels often reaches at the most 50 kPa47–49 compared with 100 kPa for this self-assembled cartilage. These self-assembled constructs have much greater mechanical properties than chondrocytes seeded in hydrogels47–49 and have similar mechanical properties to other scaffold-free tissue-engineered cartilage.50,51 Compared to these other studies, this is a significant result since no serum or growth factors were used in our study to stimulate the mechanical properties of our engineered tissues.
Through the application of exogenous stimuli such as transforming growth factor-β (TGF-β) and hydrostatic pressure, the compressive properties of tissue-engineered cartilage produced from a scaffold-free self-assembling process have approached native tissue levels.7 To avoid any confounding effects from these treatments, the effects of SZ chondrocytes on the bulk and surface mechanical properties of self-assembled cartilage were investigated in the absence of any external stimuli, in serum-free conditions. As a result, the mechanical properties of the constructs in this investigation (Fig. 3) are lower compared to previous reports that employed anabolic stimuli such as hydrostatic pressure, TGF-β, and chondroitinase ABC.7,44,45 We hypothesize that this relative softness lends itself toward a plowing mechanism that contributed to the observed friction values.52 TGF-β enhances SZP secretion in SZ articular chondrocytes14,26,27 and may provide an avenue to concomitantly improve mechanical and frictional properties.
Although the biochemical data show underproduction of collagen, the collagen II IHC displayed a greater staining intensity in the self-assembled tissues compared to native controls (Fig. 1A). The constructs have a greater cellularity and overall contain less extracellular matrix (ECM) than native articular cartilage. This attribute may have resulted in a more concentrated collagen network that lacks the superior organization and strength of the native tissue. In previous publications,28,53 self-assembled tissues were stained with picrosirius red, observed under polarized light, and found to not exhibit the collagen birefringence that is characteristic of the collagen fiber alignment and organization observed in native tissue. Thus, it is likely that the tensile properties of the self-assembled cartilage fall short of native cartilage due to the lack of collagen organization.
Whereas a lack of collagen organization likely does not affect SZP binding,54 the self-assembled tissues may also be deficient in macromolecules critical for SZP binding. Thus, although constructs may have produced sufficient amounts of SZP, the friction coefficient was not reduced due to lack SZP-binding sites. This conjecture is supported by a similar study in hydrogels, where increased production of SZP did not lower their friction coefficient due to poor retention of SZP in the bulk and on the surface of the hydrogel.55 It is unknown which ECM components are most critical for SZP binding to the surface and bulk matrix. Additional studies into cartilage lubrication engineering will need to focus not only on producing cartilage lubricants, such as SZP, but also determining methods to keep them bound to the surface.
Cell morphology is an important determinant of the articular chondrocyte phenotype56,57 and can affect the synthesis of SZP. Induction of cell rounding through 3D culture58 or cytoskeletal modulation31 is not conducive toward SZP synthesis. In this self-assembly system, SZ chondrocytes do not retain their native cell morphology and appear round like MZ chondrocytes (Fig. 1B). The round morphology of the SZ cells may be reducing the synthesis of SZP and SZP-binding macromolecules required for SZP localization.
The SZ has been reported to be stiffer in tension due to an organized collagen matrix that runs parallel to the articular surface.11 In contrast, the results of this investigation show that the MZ is over twice as strong in tension as the SZ in native tissue. These differences may arise from the rates of maturation of the cartilage obtained. Most studies in the literature were performed with adult cartilage. Like the native tissue used in this investigation, the MZ of immature bovine articular cartilage was found to be stiffer in tension than the SZ while the growth plate is still open.59
The increased proportion of SZ chondrocytes in self-assembled articular cartilage had the intended effect of enhancing the production of the boundary lubricant, SZP. However, the enhanced production of SZP was not sufficient to reduce friction. The most probable cause for this is a lack of SZP-binding macromolecules that are present at the articular surface of native cartilage. Compared to the typical self-assembled articular cartilage constructs, increasing the proportion of SZ chondrocytes had no effect on its compressive properties, but did improve the tensile stiffness and strength. However, the biochemical compositions of engineered constructs and native tissues are still quite different and reflect the gap between construct and native tissue mechanical properties that remains to be bridged by tissue engineering. In future experiments, the use of external stimuli, such as mechanical loading and growth factors, must be investigated to improve the synthesis of both SZP and SZP-binding macromolecules to improve the frictional properties of engineered cartilage.
Acknowledgments
The authors thank Thomas M. Schmid, PhD (Department of Biochemistry, Rush Medical College, Chicago, IL) for his generous gift of the monoclonal antibody S6.79. Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number R01 AR061496. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosure Statement
No competing financial interests exist.
References
- 1.Goldberg V.M., and Caplan A.I.Biological resurfacing: an alternative to total joint arthroplasty. Orthopedics 17,819, 1994 [DOI] [PubMed] [Google Scholar]
- 2.Laurencin C.T., Ambrosio A.M., Borden M.D., and Cooper J.A., Jr Tissue engineering: orthopedic applications. Annu Rev Biomed Eng 1,19, 1999 [DOI] [PubMed] [Google Scholar]
- 3.Temenoff J.S., and Mikos A.G.Review: tissue engineering for regeneration of articular cartilage. Biomaterials 21,431, 2000 [DOI] [PubMed] [Google Scholar]
- 4.Clair B.L., Johnson A.R., and Howard T.Cartilage repair: current and emerging options in treatment. Foot Ankle Spec 2,179, 2009 [DOI] [PubMed] [Google Scholar]
- 5.Borazjani B.H., Chen A.C., Bae W.C., Patil S., Sah R.L., Firestein G.S., and Bugbee W.D.Effect of impact on chondrocyte viability during insertion of human osteochondral grafts. J Bone Joint Surg Am 88,1934, 2006 [DOI] [PubMed] [Google Scholar]
- 6.Huntley J.S., Bush P.G., McBirnie J.M., Simpson A.H., and Hall A.C.Chondrocyte death associated with human femoral osteochondral harvest as performed for mosaicplasty. J Bone Joint Surg Am 87,351, 2005 [DOI] [PubMed] [Google Scholar]
- 7.Elder B.D., and Athanasiou K.A.Synergistic and additive effects of hydrostatic pressure and growth factors on tissue formation. PLoS One 3,e2341, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hu J.C., and Athanasiou K.A.A self-assembling process in articular cartilage tissue engineering. Tissue Eng 12,969, 2006 [DOI] [PubMed] [Google Scholar]
- 9.Klein T.J., Malda J., Sah R.L., and Hutmacher D.W.Tissue engineering of articular cartilage with biomimetic zones. Tissue Eng Part B Rev 15,143, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schinagl R.M., Gurskis D., Chen A.C., and Sah R.L.Depth-dependent confined compression modulus of full-thickness bovine articular cartilage. J Orthop Res 15,499, 1997 [DOI] [PubMed] [Google Scholar]
- 11.Mow V.C., Ratcliffe A., and Poole A.R.Cartilage and diarthrodial joints as paradigms for hierarchical materials and structures. Biomaterials 13,67, 1992 [DOI] [PubMed] [Google Scholar]
- 12.Becerra J., Andrades J.A., Guerado E., Zamora-Navas P., Lopez-Puertas J.M., and Reddi A.H.Articular cartilage: structure and regeneration. Tissue Eng Part B Rev 16,617, 2010 [DOI] [PubMed] [Google Scholar]
- 13.Schumacher B.L., Block J.A., Schmid T.M., Aydelotte M.B., and Kuettner K.E.A novel proteoglycan synthesized and secreted by chondrocytes of the superficial zone of articular cartilage. Arch Biochem Biophys 311,144, 1994 [DOI] [PubMed] [Google Scholar]
- 14.Niikura T., and Reddi A.H.Differential regulation of lubricin/superficial zone protein by transforming growth factor beta/bone morphogenetic protein superfamily members in articular chondrocytes and synoviocytes. Arthritis Rheum 56,2312, 2007 [DOI] [PubMed] [Google Scholar]
- 15.Ikegawa S., Sano M., Koshizuka Y., and Nakamura Y.Isolation, characterization and mapping of the mouse and human PRG4 (proteoglycan 4) genes. Cytogenet Cell Genet 90,291, 2000 [DOI] [PubMed] [Google Scholar]
- 16.Swann D.A., Slayter H.S., and Silver F.H.The molecular structure of lubricating glycoprotein-I, the boundary lubricant for articular cartilage. J Biol Chem 256,5921, 1981 [PubMed] [Google Scholar]
- 17.Flannery C.R., Hughes C.E., Schumacher B.L., Tudor D., Aydelotte M.B., Kuettner K.E., and Caterson B.Articular cartilage superficial zone protein (SZP) is homologous to megakaryocyte stimulating factor precursor and is a multifunctional proteoglycan with potential growth-promoting, cytoprotective, and lubricating properties in cartilage metabolism. Biochem Biophys Res Commun 254,535, 1999 [DOI] [PubMed] [Google Scholar]
- 18.Jay G.D., Harris D.A., and Cha C.J.Boundary lubrication by lubricin is mediated by O-linked beta(1–3)Gal-GalNAc oligosaccharides. Glycoconj J 18,807, 2001 [DOI] [PubMed] [Google Scholar]
- 19.Rhee D.K., Marcelino J., Baker M.A., Gong Y.Q., Smits P., Lefebvre V., Jay G.D., Stewart M., Wang H.W., Warman M.L., and Carpten J.D.The secreted glycoprotein lubricin protects cartilage surfaces and inhibits synovial cell overgrowth. J Clin Invest 115,622, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jay G.D., Torres J.R., Rhee D.K., Helminen H.J., Hytinnen M.M., Cha C.J., Elsaid K., Kim K.S., Cui Y.J., and Warman M.L.Association between friction and wear in diarthrodial joints lacking lubricin. Arthritis Rheum 56,3662, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McNary S.M., Athanasiou K.A., and Reddi A.H.Engineering lubrication in articular cartilage. Tissue Eng Part B Rev 18,88, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rees S.G., Davies J.R., Tudor D., Flannery C.R., Hughes C.E., Dent C.M., and Caterson B.Immunolocalisation and expression of proteoglycan 4 (cartilage superficial zone proteoglycan) in tendon. Matrix Biol 21,593, 2002 [DOI] [PubMed] [Google Scholar]
- 23.Sun Y., Berger E.J., Zhao C., An K.N., Amadio P.C., and Jay G.Mapping lubricin in canine musculoskeletal tissues. Connect Tissue Res 47,215, 2006 [DOI] [PubMed] [Google Scholar]
- 24.Schmidt T.A., and Sah R.L.Effect of synovial fluid on boundary lubrication of articular cartilage. Osteoarthritis Cartilage 15,35, 2007 [DOI] [PubMed] [Google Scholar]
- 25.Schmidt T.A., Gastelum N.S., Nguyen Q.T., Schumacher B.L., and Sah R.L.Boundary lubrication of articular cartilage: role of synovial fluid constituents. Arthritis Rheum 56,882, 2007 [DOI] [PubMed] [Google Scholar]
- 26.Neu C.P., Khalafi A., Komvopoulos K., Schmid T.M., and Reddi A.H.Mechanotransduction of bovine articular cartilage superficial zone protein by transforming growth factor beta signaling. Arthritis Rheum 56,3706, 2007 [DOI] [PubMed] [Google Scholar]
- 27.DuRaine G., Neu C.P., Chan S.M., Komvopoulos K., June R.K., and Reddi A.H.Regulation of the friction coefficient of articular cartilage by TGF-beta1 and IL-1beta. J Orthop Res 27,249, 2009 [DOI] [PubMed] [Google Scholar]
- 28.Elder B.D., and Athanasiou K.A.Effects of confinement on the mechanical properties of self-assembled articular cartilage constructs in the direction orthogonal to the confinement surface. J Orthop Res 26,238, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jadin K.D., Wong B.L., Bae W.C., Li K.W., Williamson A.K., Schumacher B.L., Price J.H., and Sah R.L.Depth-varying density and organization of chondrocytes in immature and mature bovine articular cartilage assessed by 3d imaging and analysis. J Histochem Cytochem 53,1109, 2005 [DOI] [PubMed] [Google Scholar]
- 30.Revell C.M., Reynolds C.E., and Athanasiou K.A.Effects of initial cell seeding in self assembly of articular cartilage. Ann Biomed Eng 36,1441, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McNary S.M., Athanasiou K.A., and Reddi A.H.Transforming growth factor beta-induced superficial zone protein accumulation in the surface zone of articular cartilage is dependent on the cytoskeleton. Tissue Eng Part A 20,921, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Su J.L., Schumacher B.L., Lindley K.M., Soloveychik V., Burkhart W., Triantafillou J.A., Kuettner K., and Schmid T.Detection of superficial zone protein in human and animal body fluids by cross-species monoclonal antibodies specific to superficial zone protein. Hybridoma 20,149, 2001 [DOI] [PubMed] [Google Scholar]
- 33.Neu C.P., Reddi A.H., Komvopoulos K., Schmid T.M., and Di Cesare P.E.Increased friction coefficient and superficial zone protein expression in patients with advanced osteoarthritis. Arthritis Rheum 62,2680, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reddy G.K., and Enwemeka C.S.A simplified method for the analysis of hydroxyproline in biological tissues. Clin Biochem 29,225, 1996 [DOI] [PubMed] [Google Scholar]
- 35.Athanasiou K.A., Agarwal A., and Dzida F.J.Comparative study of the intrinsic mechanical properties of the human acetabular and femoral head cartilage. J Orthop Res 12,340, 1994 [DOI] [PubMed] [Google Scholar]
- 36.Mow V.C., Gibbs M.C., Lai W.M., Zhu W.B., and Athanasiou K.A.Biphasic indentation of articular cartilage—II. A numerical algorithm and an experimental study. J Biomech 22,853, 1989 [DOI] [PubMed] [Google Scholar]
- 37.Murphy M.K., Huey D.J., Reimer A.J., Hu J.C., and Athanasiou K.A.Enhancing post-expansion chondrogenic potential of costochondral cells in self-assembled neocartilage. PLoS One 8,e56983, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chan S.M., Neu C.P., Duraine G., Komvopoulos K., and Reddi A.H.Atomic force microscope investigation of the boundary-lubricant layer in articular cartilage. Osteoarthritis Cartilage 18,956, 2010 [DOI] [PubMed] [Google Scholar]
- 39.Chan S.M., Neu C.P., Komvopoulos K., and Reddi A.H.Dependence of nanoscale friction and adhesion properties of articular cartilage on contact load. J Biomech 44,1340, 2011 [DOI] [PubMed] [Google Scholar]
- 40.Chan S.M., Neu C.P., Komvopoulos K., and Reddi A.H.The role of lubricant entrapment at biological interfaces: reduction of friction and adhesion in articular cartilage. J Biomech 44,2015, 2011 [DOI] [PubMed] [Google Scholar]
- 41.Jones A.R., Gleghorn J.P., Hughes C.E., Fitz L.J., Zollner R., Wainwright S.D., Caterson B., Morris E.A., Bonassar L.J., and Flannery C.R.Binding and localization of recombinant lubricin to articular cartilage surfaces. J Orthop Res 25,283, 2007 [DOI] [PubMed] [Google Scholar]
- 42.Williamson A.K., Chen A.C., and Sah R.L.Compressive properties and function-composition relationships of developing bovine articular cartilage. J Orthop Res 19,1113, 2001 [DOI] [PubMed] [Google Scholar]
- 43.Khalsa P.S., and Eisenberg S.R.Compressive behavior of articular cartilage is not completely explained by proteoglycan osmotic pressure. J Biomech 30,589, 1997 [DOI] [PubMed] [Google Scholar]
- 44.Responte D.J., Arzi B., Natoli R.M., Hu J.C., and Athanasiou K.A.Mechanisms underlying the synergistic enhancement of self-assembled neocartilage treated with chondroitinase-ABC and TGF-beta1. Biomaterials 33,3187, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Natoli R.M., Responte D.J., Lu B.Y., and Athanasiou K.A.Effects of multiple chondroitinase ABC applications on tissue engineered articular cartilage. J Orthop Res 27,949, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Urban J.P., Hall A.C., and Gehl K.A.Regulation of matrix synthesis rates by the ionic and osmotic environment of articular chondrocytes. J Cell Physiol 154,262, 1993 [DOI] [PubMed] [Google Scholar]
- 47.Mauck R.L., Soltz M.A., Wang C.C., Wong D.D., Chao P.H., Valhmu W.B., Hung C.T., and Ateshian G.A.Functional tissue engineering of articular cartilage through dynamic loading of chondrocyte-seeded agarose gels. J Biomech Eng 122,252, 2000 [DOI] [PubMed] [Google Scholar]
- 48.Huang A.H., Yeger-McKeever M., Stein A., and Mauck R.L.Tensile properties of engineered cartilage formed from chondrocyte- and MSC-laden hydrogels. Osteoarthritis Cartilage 16,1074, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Erickson I.E., Huang A.H., Chung C., Li R.T., Burdick J.A., and Mauck R.L.Differential maturation and structure-function relationships in mesenchymal stem cell- and chondrocyte-seeded hydrogels. Tissue Eng Part A 15,1041, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fedewa M.M., Oegema T.R., Jr., Schwartz M.H., MacLeod A., and Lewis J.L.Chondrocytes in culture produce a mechanically functional tissue. J Orthop Res 16,227, 1998 [DOI] [PubMed] [Google Scholar]
- 51.Gemmiti C.V., and Guldberg R.E.Fluid flow increases type II collagen deposition and tensile mechanical properties in bioreactor-grown tissue-engineered cartilage. Tissue Eng 12,469, 2006 [DOI] [PubMed] [Google Scholar]
- 52.Coles J.M., Blum J.J., Jay G.D., Darling E.M., Guilak F., and Zauscher S.In situ friction measurement on murine cartilage by atomic force microscopy. J Biomech 41,541, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Natoli R.M., Revell C.M., and Athanasiou K.A.Chondroitinase ABC treatment results in greater tensile properties of self-assembled tissue-engineered articular cartilage. Tissue Eng Part A 15,3119, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chang D.P., Guilak F., Jay G.D., and Zauscher S.Interaction of lubricin with type II collagen surfaces: adsorption, friction, and normal forces. J Biomech 47,659, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gleghorn J.P., Jones A.R., Flannery C.R., and Bonassar L.J.Boundary mode frictional properties of engineered cartilaginous tissues. Eur Cell Mater 14,20, 2007 [DOI] [PubMed] [Google Scholar]
- 56.Benya P.D., and Shaffer J.D.Dedifferentiated chondrocytes reexpress the differentiated collagen phenotype when cultured in agarose gels. Cell 30,215, 1982 [DOI] [PubMed] [Google Scholar]
- 57.Benya P.D., Brown P.D., and Padilla S.R.Microfilament modification by dihydrocytochalasin B causes retinoic acid-modulated chondrocytes to reexpress the differentiated collagen phenotype without a change in shape. J Cell Biol 106,161, 1988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Klein T.J., Schumacher B.L., Blewis M.E., Schmidt T.A., Voegtline M.S., Thonar E.J., Masuda K., and Sah R.L.Tailoring secretion of proteoglycan 4 (PRG4) in tissue-engineered cartilage. Tissue Eng 12,1429, 2006 [DOI] [PubMed] [Google Scholar]
- 59.Roth V., and Mow V.C.The intrinsic tensile behavior of the matrix of bovine articular cartilage and its variation with age. J Bone Joint Surg Am 62,1102, 1980 [PubMed] [Google Scholar]