Abstract
The objective of this systematic review was to evaluate current evidence for the efficacy of Ginkgo biloba extract EGb 761® in dementia. Seven of 15 randomized, placebocontrolled trials in patients with dementia identified by database searches met all our selection criteria and were included in the meta-analysis. In these trials, patients were treated with 120 mg or 240 mg per day of the defined extract EGb 761 or placebo. Efficacy was assessed using validated tests and rating scales for the cognitive domain, the functional domain (activities of daily living), and global assessment. Tolerability was evaluated by risk differences based on incidences of adverse events and premature discontinuation rates. Of 2,684 outpatients randomized to receive treatment for 22–26 weeks, 2,625 represented the full analysis sets (1,396 for EGb 761 and 1,229 for placebo). Standardized mean differences for change in cognition (−0.52; 95% confidence interval [CI] −0.98, −0.05; P=0.03), activities of daily living (−0.44; 95% CI −0.68, −0.19; P<0.001), and global rating (−0.52; 95% CI −0.92, −0.12; P=0.01) significantly favored EGb 761 compared with placebo. Statistically significant superiority of EGb 761 over placebo was confirmed by responder analyses as well as for patients suffering from dementia with neuropsychiatric symptoms. Treatment-associated risks in terms of relative risks of adverse events and premature withdrawal rates did not differ noticeably between the two treatment groups. In conclusion, meta-analyses confirmed the efficacy and good tolerability of Ginkgo biloba extract EGb 761 in patients with dementia.
Keywords: Alzheimer’s disease, vascular dementia, mixed dementia, efficacy, safety
Introduction
The most frequent pathologies underlying dementia in the elderly are Alzheimer’s disease (AD) pathology (ie, plaques and tangles) and cerebrovascular disease. Pure AD and pure vascular dementia (VaD) exist, yet a mix of the two pathologies is found most frequently in neuropathology studies.1,2 While treatments targeting plaque and tangle pathology have largely failed so far, cholinesterase inhibitors, memantine, and quantified ginkgo leaf extract have been found to be effective in the symptomatic treatment of dementia and are recommended by current guidelines.3
Ginkgo biloba extract EGb 761® interferes with pathogenic mechanisms involved in both AD and VaD. It restores impaired mitochondrial function, thereby improving neuronal energy supply,4 improves compromised hippocampal neurogenesis and neuroplasticity,5 inhibits the aggregation and toxicity of Aβ protein,6 decreases blood viscosity, and enhances microperfusion.7 In a recent study, EGb 761 specifically increased dopamine levels in the rat prefrontal cortex, which is involved in working memory and executive control.8
The clinical efficacy of defined quantified Ginkgo biloba extract EGb 761 in the treatment of dementia has been assessed by a series of randomized, placebo-controlled, double-blind clinical trials. Findings from most of these studies have been jointly evaluated by meta-analyses,9–12 but data from two further clinical trials13,14 have become available after publication of the latest review.12 Therefore, in this study up-to-date meta-analyses were performed including data from these two trials.
The composition of a plant extract, in particular the quantities and proportions of pharmacodynamically active molecules, is determined by the quality of the raw material, the extraction solvent(s), and the extraction process. Therefore, it is evident that each Ginkgo biloba extract is an active substance on its own and that the efficacy and safety of each individual extract is to be demonstrated in separate studies. Hence, for a systematic review and meta-analysis to yield reasonable and interpretable results, it is mandatory that only studies using one defined extract are included. EGb 761 is a dry extract from Ginkgo biloba leaves (35–67:1), extraction solvent:acetone 60% (weight/weight). The extract is adjusted to 22.0%–27.0% ginkgo flavonoids, calculated as ginkgo flavone glycosides, 5.0%–7.0% terpene lactones consisting of 2.8%–3.4% ginkgolides A, B, and C, and 2.6%–3.2% bilobalide, and contains less than 5 ppm ginkgolic acids. (EGb 761® is a registered trademark of Dr Willmar Schwabe GmbH & Co. KG, Karlsruhe, Germany.)
Methods
Data sources
To identify potentially eligible studies, we used a sensitive search strategy involving the largest databases of research publications in the field: PubMed, including and excluding MedLine (to December 2012), EMBASE (from January 2006 to December 2011), and PASCAL (to December 2011). The following search terms were used (with * characterizing a wildcard, and the items AND and OR being used as Boolean functions): (ginkg* OR gingk*) AND clinical trial[pt] for PubMed including MedLine, ((ginkg* OR gingk*) NOT medline[sb]) AND (clinical* OR trial OR randomized) for PubMed excluding MedLine, (GINKGO OR GINGKO) AND (HUMAN/CT OR HOMME/CTFR) for PASCAL and (ginkgo or gingko) AND CT=(CLINICAL TRIAL; CLINICAL STUDY; DOUBLE BLIND PROCEDURE) AND py>2005 for EMBASE. The search was repeated in December 2013; no new trials were identified. Further, the reference sections of systematic reviews were screened for primary publications.
Selection of clinical trials
Trials were eligible for inclusion if they were placebocontrolled, randomized, double-blind clinical trials of at least 20 weeks in duration, assessing the effects of an oral dosage form of EGb 761 in patients with a diagnosis of AD, VaD, or mixed dementia (ie, with features of both AD and cerebrovascular disease), if the diagnosis was established in accordance with internationally accepted diagnostic criteria (Diagnostic and Statistical Manual of Mental Disorders, Third Revised or Fourth Edition (DSM-III-R, DSM-IV),15,16 International Classification of Diseases Tenth Revision (ICD-10),17 National Institute of Neurological and Communicative Disorders and Stroke, Alzheimer’s Disease and Related Disorders Association (NINCDS-ADRDA),18 or the National Institute for Neurological Disorders and Stroke and Association Internationale pour la Recherche et l’Enseignement en Neurosciences (NINDS-AIREN),19 and if outcome measures were defined for at least two of the three typical domains of assessment in dementia, ie, cognition, activities of daily living (ADL), and clinical global judgment. Trials including mostly patients with other diagnoses, such as aging-associated memory impairment or mild cognitive impairment, and trials using EGb 761 as add-on treatment to cholinesterase inhibitors, were excluded.
Data extraction and critical appraisal of clinical trials
Trial and publication quality were assessed in terms of randomization and allocation concealment, blinding of patients and investigators, sample size estimation, handling and reporting of trial discontinuations, application of the intent-to-treat principle, and relevant data inconsistencies. All included trials adequately met these quality criteria, with Jadad scores ranging from 3 (two trials) to 5 (five trials). All clinical outcomes were assessed in the intention-to-treat/full-analysis sets. All relevant demographic and efficacy-related data were extracted from the published papers and entered into the software used for analysis. One paper was not published in English, but a complete translation was available to the authors.14
Statistical analysis
Effects on rating scales were expressed as standardized mean differences (SMDs, in the event of different outcomes in aggregated trials) or mean differences (same outcome in every clinical trial), as appropriate for the comparison, with 95% confidence intervals (CIs). Since considerable heterogeneity between the trials was expected, a random effects model was used to calculate the combined effect estimate using the inverse variance method. If different dose levels were used in different treatment arms, the treatment group with the higher dosage was chosen for the meta-analysis. Sensitivity analyses were performed for daily dose (120 mg or 240 mg EGb 761 per day) and for clinical trials including patients with neuropsychiatric symptoms (NPS). For binary (safety) data, effect measures were presented as risk ratios (RRs) with corresponding 95% CIs. Fixed effects meta-analyses of binary safety data were performed using the inverse variance method. Since clinical and methodological diversity always occur in meta-analyses, statistical heterogeneity is inevitable.20 To quantify inconsistency, the I2 statistic was calculated. According to the Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0, the importance of the observed value of I2 depends on the magnitude and direction of effects.21 An I2 of at least 50% together with different directions of effects (ie, some trials favoring active treatment and others favoring placebo with an absolute SMD of at least 0.3) was taken as an indicator of substantial heterogeneity. Heterogeneity was classified as moderate if I2 was at least 50% and directions of treatment effects did not differ. In the case of moderate or substantial heterogeneity, the effect was examined by removing single trials from the analysis.
For each single trial, the response rates in the cognition and global judgment domains were compared between EGb 761 and placebo groups using odds ratios and 95% CIs. The combined odds ratios were calculated using the Mantel-Haenszel method in random effects meta-analyses and presented with 95% CIs.
The safety of EGb 761 was assessed by comparing rates of patients with at least one adverse event, patients with at least one serious adverse event, and rates of dropouts due to adverse events between the treatment groups. The meta-analyses were performed using Review Manager version 5 (The Cochrane Collaboration, Oxford, UK). In all analyses, statistical significance was assumed at P<0.05.
Results
Clinical trial characteristics
Fifteen randomized, placebo-controlled clinical trials assessing the effects of oral dosage forms of EGb 761 in patients with dementia were retrieved. Eight trials were excluded from the meta-analysis because they did not meet the selection criteria (Table 1).22–29
Table 1.
Placebo-controlled clinical trials assessing the effects of EGb 761® in patients with dementia
| Clinical trials included in the meta-analysis | |
| Trial | Diagnostic criteria/main inclusion criteria |
| Herrschaft et al13 | NINCDS/ADRDA probable Alzheimer’s disease or NINDS/AIREN probable vascular dementia or mixed form; age ≥50 years, TE4D ≤35, SKT 9–23 (MMSE 14–25a), NPI total score ≥5 |
| Ihl et al36 | NINCDS/ADRDA probable Alzheimer’s disease or NINDS/AIREN probable vascular dementia or mixed form; age ≥50 years, TE4D ≤35, SKT 9–23 (MMSE 14–25a), NPI total score ≥5 |
| Kanowski et al33,34 | DSM III-R, Alzheimer’s disease or vascular dementia; age ≥55 years, MMSE 13–25, SKT 6–18 |
| Le Bars et al30,31 | DSM III-R and ICD-10, Alzheimer’s disease or vascular dementia; age ≥45 years, MMSE 9–26, GDS 3–6 |
| Napryeyenko et al35 | NINCDS/ADRDA probable Alzheimer’s disease or NINDS/AIREN probable vascular dementia or mixed form; age ≥50 years, TE4D ≤35, SKT 9–23 (MMSE 14–25a), NPI total score ≥5 |
| Nikolova et al14 | NINCDS/ADRDA probable Alzheimer’s disease or NINDS/AIREN probable vascular dementia or mixed form; age ≥50 years, TE4D ≤35, SKT 9–23 (MMSE 14–25a), NPI total score ≥5 |
| Schneider et al32 | NINCDS/ADRDA probable Alzheimer’s disease; Hachinki Ischemia Score ≤4, age ≥60 years, MMSE 10–24 |
| Clinical trials excluded from meta-analysis | |
| Trial | Reasons for exclusion from meta-analysis |
| Hofferberth25 | Clinical diagnosis without application of formal diagnostic criteria |
| Mancini et al24 | Clinical diagnosis without application of formal diagnostic criteria |
| Maurer et al26 | Treatment period less than 20 weeks |
| Mazza et al28 | Treatment was not EGb 761 |
| McCarney et al29 | Clinical diagnosis of dementia without application of formal diagnostic criteria; ongoing treatment with cholinesterase inhibitors in a substantial proportion of patients; statistical analysis inadequate for factorial study design with different intensity of follow-up |
| Rai et al23 | Only cognitive assessment, no second clinical outcome |
| Van Dongen et al27 | Inclusion diagnosis was aging-associated memory impairment in most patients |
| Weitbrecht and Jansen22 | Clinical diagnosis without application of formal diagnostic criteria |
Note:
Range of MMSE scores corresponding to SKT 9–23.43
Abbreviations: DSM-III-R, Diagnostic and Statistical Manual of Mental Disorders, Third Edition Revised; GDS, Global Deterioration Scale; ICD-10, International Classification of Diseases, Tenth Edition; MMSE, Mini-Mental State Examination; NINCDS/ADRDA, National Institute of Neurological and Communicative Disorders and Stroke/Alzheimer’s Disease and Related Disorders Association; NINDS/AIREN, National Institute of Neurological Disorders and Stroke/Association Internationale pour la Recherche et l’Enseignement en Neurosciences; NPI, Neuropsychiatric Inventory; TE4D, Test for the Early Detection of Dementia with Differentiation from Depression; SKT, Short Cognitive Performance Test (Syndrom-Kurztest).
The remaining seven trials fulfilled all selection criteria outlined above and were found to be methodologically adequate. They were therefore included in the meta-analysis. All patients enrolled in these trials were diagnosed with dementia, specified as AD, VaD (or its special form, multi-infarct dementia), or mixed dementia (with features of AD and cerebrovascular disease), according to widely accepted diagnostic criteria. Only patients with mild or moderate dementia were included in the studies (operationally defined, eg, by severity criteria of the DSM-III-R or cognitive scores).
Seven clinical trials with 2,684 randomized patients (1,423 for EGb 761 and 1,261 for placebo) will be described. In two trials, a daily dose of 120 mg EGb 761 was administered in one treatment arm.30–32 In six trials, a daily dose of 240 mg was administered.13,14,32–36 In six clinical trials, patients with NPS were accepted for inclusion.13,14,30,31,33–36 In four of these trials, only patients with clinically significant NPS were eligible for inclusion;13,14,35,36 in the remaining two trials, patients with or without NPS were accepted.30,33 In fact, more than 90% of patients enrolled in the two latter trials presented NPS.37 Patients meeting diagnostic criteria for a concomitant psychiatric disorder were excluded from all trials.
Characteristics of the included trials are presented in Table 2. Trial quality was appropriate, with Jadad scores of 314,32 and 5.13,30,33,35,36 In total, 2,625 randomized patients (1,396 for EGb 761 and 1,229 for placebo) could be evaluated with respect to efficacy of EGb 761 compared with placebo. Within each trial, the rates of female patients were similar across the treatment groups and varied between 50% and 86%. The mean age was between 63 and 79 years. With respect to anthropometric data, eg, height, weight, and body mass index, no relevant differences were observed between the treatment groups in the selected clinical trials. Within each trial, mean baseline values of cognitive scores, ADL scores, and global assessment (if available) were comparable between active treatment and placebo groups (Table 3).
Table 2.
Characteristics of included clinical trial populations
| Clinical trial | Duration (weeks) | Diagnostic groups (number in full analysis set) | Treatment groups | na | Dropouts (%) | Age, years, mean (SD) | Sex, % female | Body weight, kg, mean (SD) | Prior intake of antidementia drugs (n) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||
| AD | VaD | Mixed | |||||||||
| Kanowski et al33,34 | 24 | 158 | 47 | – | EGb 240 mg | 109 | 16 (14.7) | 72 (10) | 68 | 69 (13) | Nonec |
| Placebo | 107 | 16 (15.0) | 72 (10) | 71 | 67 (13) | Nonec | |||||
| Le Bars et al30,31 | 52b | 236 | 73 | – | EGb 120 mg | 161 | 39 (24.2) | 69 (10) | 51 | 69 (14) | Nonec |
| Placebo | 166 | 44 (26.5) | 69 (10) | 56 | 70 (13) | Nonec | |||||
| Schneider et al32 | 26 | 513 | – | – | EGb 240 mg | 170 | 30 (18) | 78 (7) | 56 | 68 (14) | NDd |
| EGb 120 mg | 169 | 34 (20) | 79 (7) | 50 | 6 (15) | NDd | |||||
| Placebo | 174 | 39 (22) | 78 (7) | 52 | 70 (13) | NDd | |||||
| Nikolova et al14 | 22 | 178 | 80 | 139 | EGb 240 mg | 203 | 13 (6) | 69 (8) | 57 | 72 (13) | 4 |
| Placebo | 205 | 17 (8) | 69 (8) | 60 | 72 (14) | 3 | |||||
| Napryeyenko et al35 | 22 | 53 | 181 | 161 | EGb 240 mg | 200 | 4 (2) | 65 (8) | 86 | 74 (12) | 2 |
| Placebo | 200 | 5 (3) | 63 (8) | 82 | 73 (11) | 0 | |||||
| Ihl et al36 | 24 | 121 | 71 | 212 | EGb 240 mg | 206 | 16 (8) | 65 (10) | 69 | 74 (14) | 0 |
| Placebo | 204 | 12 (6) | 65 (9) | 66 | 74 (14) | 0 | |||||
| Herrschaft et al13 | 24 | 208 | 42 | 152 | EGb 240 mg | 205 | 7 (3) | 65 (9) | 70 | 76 (13) | 1 |
| Placebo | 205 | 5 (2) | 65 (9) | 69 | 73 (13) | 4 | |||||
Notes: –There were no patients with these diagnoses.
AD with cerebrovascular disease.
n includes all patients randomized;
data for week 26 analyzed and presented;
there were no approved antidementia drugs when these trials were conducted;
not determinable (ND).
Many patients had participated in double-blind, controlled clinical trials of antidementia drugs before. How many patients received an effective antidementia drug, placebo, or an ineffective investigational drug within these trials is not known.
Abbreviations: EGb, EGb 761®; AD, Alzheimer’s disease; VaD, vascular dementia; SD, standard deviation.
Table 3.
Baseline scores
| Clinical trial | Treatment groups | na | Cognition scale | ADL scale | Global assessment | Depression scale | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Kanowski et al33,34 | EGb 240 mg | 106 | SKT | 10.5 (3.2) | NAB | 21.5 (3.8) | CGI (item 1) | 4.8 (0.8) | MADRS | 15.7 (7.2) |
| Placebo | 99 | 11.2 (3.3) | 21.1 (3.7) | 4.7 (0.8) | 16.2 (7.2) | |||||
| Le Bars et al30,31 | EGb 120 mg | 155 | ADAS-cog | 20.0 (16.0) | GERRI | 2.1 (0.6) | CGI (item 1) | 3.5 (1.0) | HAMD | 5.1 (4.5) |
| Placebo | 154 | 20.5 (14.7) | 2.1 (0.6) | 3.4 (0.8) | 4.7 (4.2) | |||||
| Schneider et al32 | EGb 240 mg | 170 | ADAS-cog | 24.8 (12.7) | GERRI | 2.4 (0.5) | ADCS-CGIC | – | HAMD | 3.3 (3.1) |
| EGb 120 mg | 169 | 24.7 (12.7) | 2.4 (0.6) | – | 3.6 (3.2) | |||||
| Placebo | 174 | 25.0 (11.1) | 2.4 (0.6) | – | 3.4 (3.2) | |||||
| Nikolova et al14 | EGb 240 mg | 196 | SKT | 14.9 (4.3) | GBS-ADL | 2.3 (3.4) | GBS- total score | 26.0 (13.1) | HAMD | 9.5 (4.1) |
| Placebo | 201 | 15.4 (4.2) | 2.6 (3.6) | 26.7 (12.7) | 9.0 (3.8) | |||||
| Napryeyenko et al35 | EGb 240 mg | 198 | SKT | 15.6 (3.9) | GBS-ADL | 4.8 (3.9) | GBS- total score | 35.3 (9.1) | HAMD | 11.5 (4.3) |
| Placebo | 197 | 15.4 (3.7) | 4.9 (4.1) | 34.3 (8.7) | 11.8 (4.4) | |||||
| Ihl et al36 | EGb 240 mg | 202 | SKT | 16.7 (3.9) | ADL-IS | 1.9 (0.6) | ADCS-CGIC | – | HAMD | 9.1 (3.4) |
| Placebo | 202 | 17.2 (3.7) | 2.0 (0.5) | – | 9.8 (3.5) | |||||
| Herrschaft et al13 | EGb 240 mg | 200 | SKT | 15.1 (4.1) | ADL-IS | 1.7 (0.6) | ADCS-CGIC | – | HAMD | 9.3 (4.4) |
| Placebo | 202 | 15.3 (4.2) | 1.8 (0.6) | – | 9.4 (4.5) | |||||
Notes:
n includes all patients valid for evaluation of efficacy (full analysis set). Data are presented as the mean (standard deviation).
Abbreviations: ADAS-cog, cognitive subscale of the Alzheimer’s Disease Assessment Scale; ADL, activities of daily living; EGb, EGb 761®; CGI, Clinical Global Impression; CGIC, Clinical Global Impression of Change; ADCS-CGIC, Alzheimer’s Disease Cooperative Study Clinical Global Impression of Change; NAB, Nuremberg Gerontopsychological Observation Scale; GERRI, Geriatric Evaluation by Relatives Rating Instrument; GBS, Gottfries-Bråne-Steen scale; GBS-ADL, Gottfries-Bråne-Steen Activities of Daily Living Scale; ADL-IS, Alzheimer’s Disease Activities of Daily Living International Scale; HAMD, Hamilton Depression Rating Scale; MADRS, Montgomery-Åsberg Depression Rating Scale; SKT, Short Cognitive Performance Test (Syndrom-Kurztest).
Continuous outcome variables (changes from baseline)
Clinical outcomes at study end, ie, at 22–26 weeks, considering the whole patient group and subgroups, are described here. The results are presented within three domains of assessment. Negative changes in outcome variables indicate improvement. Negative (standardized) mean differences indicate a greater improvement in EGb 761 as compared with placebo.
Cognition
All included trials (n=7) evaluated cognition, five13,14,33,35,36 using the SKT Short Cognitive Performance Test (Syndrom-Kurztest)38,39 and two30,32 using the cognitive subscale of the Alzheimer’s Disease Assessment Scale (ADAS-cog).40 The SKT was preferred in the European trials. It does not use word lists or other language-bound test material, and is therefore particularly feasible for use in different countries and cultures without the need to create numerous different versions for different cultures and languages. The validity of the SKT across cultures and languages has been demonstrated.41,42 The high correlation between SKT and ADAS-cog scores suggests that both tests largely measure the same abilities.43
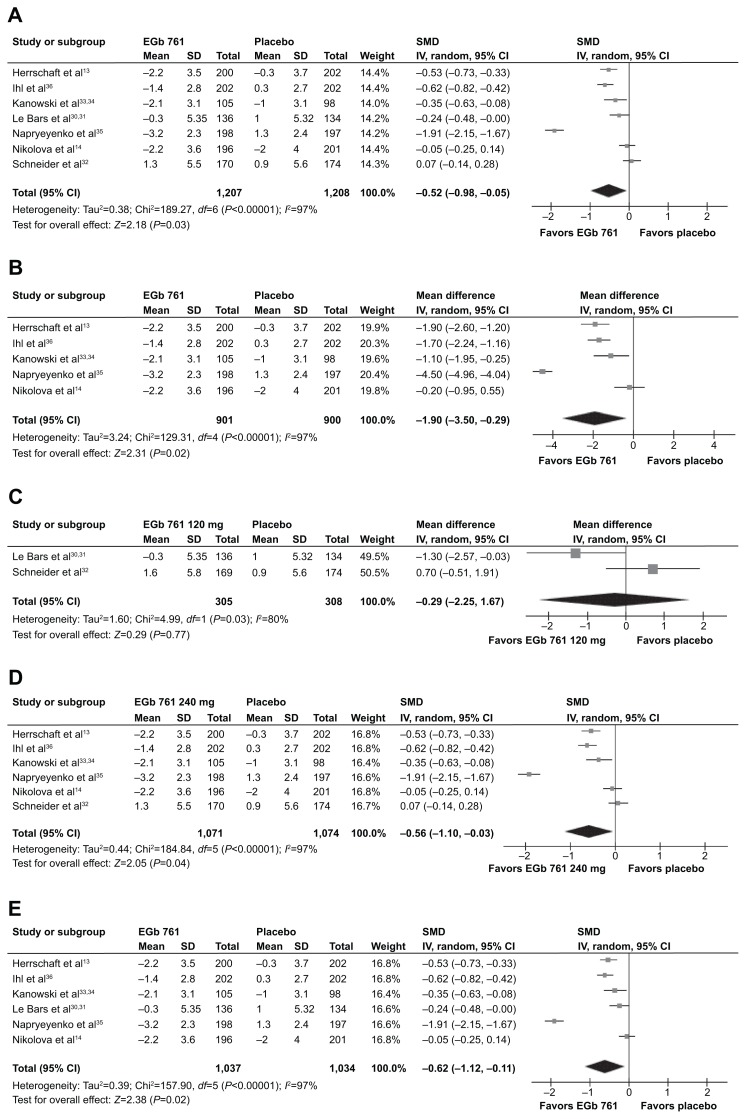
Five of seven trials significantly favored EGb 761 over placebo. Meta-analysis showed a significant difference in favor of EGb 761 (SMD −0.52; 95% CI −0.98, −0.05; P=0.03, n=7). Heterogeneity was classified as moderate (I2=97%, no trial favored placebo; Figure 1A). I2 could be reduced to 85% by removing the trial with the best results for EGb 761 compared with placebo.35 The statistical significance of the overall treatment effect was not affected by removing this trial (SMD −0.29; 95% CI −0.51, −0.06; P=0.01). Since most trials used the SKT as the cognitive outcome, and the SKT correlates well with ADL,42 a separate meta-analysis of effects on the SKT total score was calculated (Figure 1B).
Figure 1.
Change in scores for cognition (SKT, ADAS-cog).
Notes: (A) All trials, (B) trials using the SKT, (C) daily dose of EGb 761 120 mg, (D) daily dose of EGb 761 240 mg, and (E) studies in patients with NPS.
Abbreviations: ADAS-cog, cognitive subscale of the Alzheimer’s Disease Assessment Scale; EGb, EGb 761®; SKT, Short Cognitive Performance Test (Syndrom-Kurztest); NPS, neuropsychiatric symptoms; CI, confidence interval; SD, standard deviation; SMD, standardized mean difference; IV, inverse variance method.
The effects of EGb 761 on cognition were dose-dependent (Figure 1C and D). At the higher daily dose (240 mg), EGb 761 showed a significantly better overall effect on cognition than placebo (Figure 1D). In patients with NPS, improvement in cognition was significantly greater in patients treated with EGb 761 than in those receiving placebo (Figure 1E).
Activities of daily living
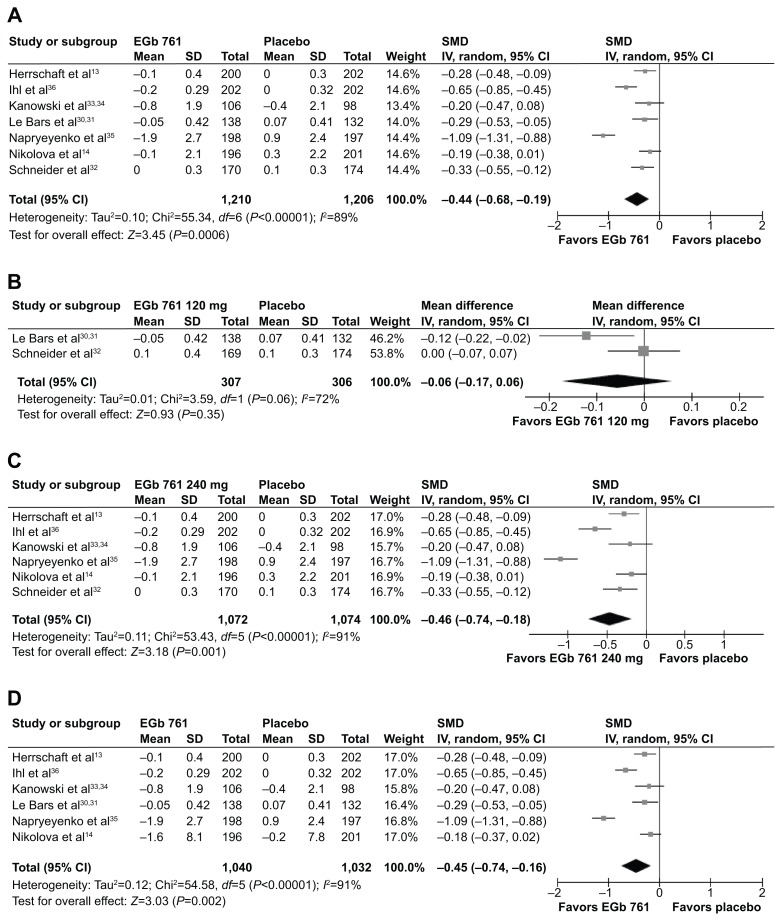
ADL were evaluated in all included trials. Two trials30,32 used the Geriatric Evaluation by Relative’s Rating Instrument (GERRI),44 two trials14,35 used the Activities of Daily Living Subscale of the Gottfries-Bråne-Steen Scale (GBS-ADL),45 and two trials13,36 employed the Alzheimer’s Disease Activities of Daily Living International Scale (ADL-IS).46 In one trial33,34 the Nuremberg Gerontopsychological Observation Scale (NAB, Nürnberger Alters-Beobachtungsskala)47 was used. Meta-analysis resulted in a statistically significant difference in favour of EGb 761 (SMD −0.44; 95% CI −0.68, −0.19; P<0.001, n=7). There was moderate heterogeneity (I2=89%, no different direction of effects, Figure 2A). I2 could be reduced to 62% by removing the trial with the best results for EGb 761 compared with placebo.35 The statistical significance of the overall treatment effect was not affected by removing this trial (SMD −0.33; 95% CI −0.47, −0.18; P<0.001).
Figure 2.
Change in scores for activities of daily living (NAB, GERRI, GBS-ADL, ADL-IS).
Notes: (A) All trials, (B) daily dose of EGb 761 120 mg, (C) daily dose of EGb 761 240 mg, and (D) studies in patients with NPS.
Abbreviations: EGb, EGb 761®; NAB, Nuremberg Gerontopsychological Observation Scale; GERRI, Geriatric Evaluation by Relatives Rating Instrument; GBS-ADL, Gottfries-Bråne-Steen Activities of Daily Living Scale; ADL-IS, Alzheimer’s Disease Activities of Daily Living International Scale; CI, confidence interval; SD, standard deviation; SMD, standardized mean difference; IV, inverse variance method.
The effects on ADL were dose-dependent (Figure 2B and C). At the higher daily dose (240 mg), ADL improved significantly more on active treatment than on placebo (Figure 2C). In trials enrolling patients with NPS, ADL improved significantly more in those treated with EGb 761 than in the placebo groups (Figure 2D).
Clinical global impression
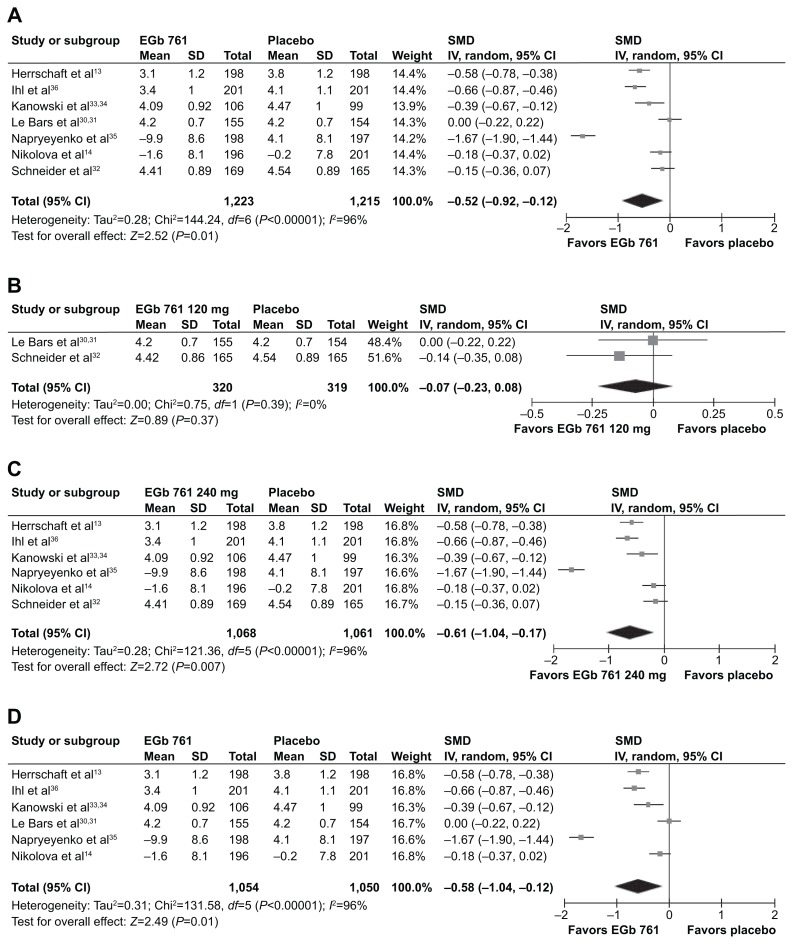
Clinical global impression was rated in all selected trials. Traditional Clinical Global Impression of Change (CGIC)48 was administered in two studies,30,33 the Alzheimer’s Disease Cooperative Study Clinical Global Impression of Change (ADCS-CGIC)49 in three trials,13,32,36 and the Gottfries-Bråne-Steen Scale,45 an overall geriatric assessment scale (GBS total score), in two trials.14,35 The difference between treatment groups was statistically significant in favor of EGb 761 in the meta-analysis (SMD −0.52; 95% CI −0.92, −0.12; P=0.01, n=7; Figure 3A). Heterogeneity was classified as moderate (I2=96%, no different direction of treatment effects). I2 could be reduced to 81% by removing the trial with the largest drug–placebo differences in favor of EGb 761.35 The statistical significance of the overall treatment effects was not affected by removing this trial (SMD −0.33; 95% CI −0.55, −0.11; P=0.003).
Figure 3.
Clinical global impression of change from baseline (CGIC, ADCS-CGIC, GBS).
Notes: (A) All trials, (B) daily dose of EGb 761 120 mg, (C) daily dose of EGb 761 240 mg, and (D) studies in patients with NPS.
Abbreviations: EGb, EGb 761®; CI, confidence interval; SD, standard deviation; NPS, neuropsychiatric symptoms; SMD, standardized mean difference; IV, inverse variance method; GBS, Gottfries-Bråne-Steen scale; CGIC, Clinical Global Impression of Change; ADCS-CGIC, Alzheimer’s Disease Cooperative Study Clinical Global Impression of Change.
Effects on global ratings were dose-dependent (Figure 3B and C). At daily doses of 240 mg, global ratings significantly favored EGb 761 over placebo (Figure 3C). Global change was rated significantly more favorably for patients treated with EGb 761 than for patients receiving placebo in the group suffering from NPS (Figure 3D).
Responder analyses
Response criteria were defined prospectively. They were chosen due to considerations of obvious clinical relevance and published expert consensus. For cognition, an improvement of at least 4 points on the ADAS-cog is generally regarded as clinically relevant.50 According to regression analyses performed by Ihl et al,43 a 3-point change in the SKT corresponds to a 3.9-point change on the ADAS-cog, and thus matches most closely what is considered to be a clinically relevant change on the ADAS-cog. For global assessment, any improvement in a clinician’s global assessment (CGIC, ADCS-CGIC) after 24 weeks is generally considered as clinically relevant in a naturally progressing disease like dementia.3
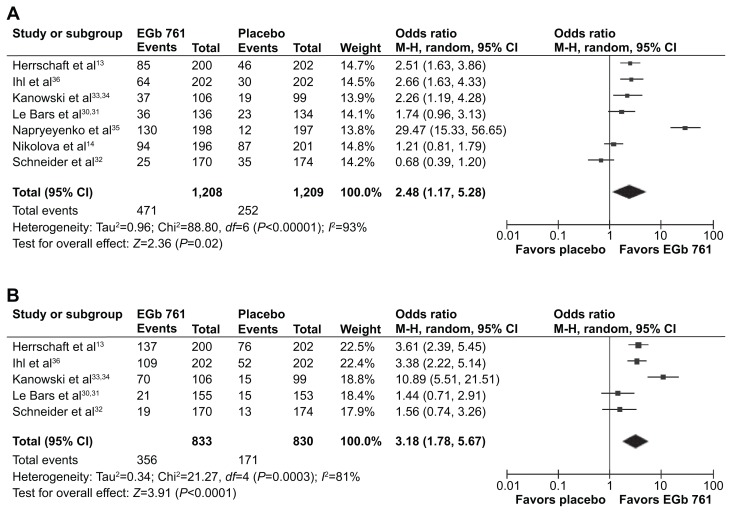
Cognition
The odds ratios were significantly higher than 1, ie, in favor of EGb 761, in four of the seven trials. The meta-analysis demonstrated significant superiority of EGb 761, with an overall odds ratio of 2.48 (95% CI 1.17, 5.28; P=0.02; Figure 4A). Heterogeneity (I2=93%) was mainly attributable to the trial reported by Napryeyenko et al.35 Excluding this trial from the analysis resulted in an I2 of 75%, and the superiority of EGb 761 over placebo remained statistically significant (odds ratio 1.67; 95% CI 1.11, 2.53; P=0.01).
Figure 4.
Clinically relevant response.
Notes: (A) Odds ratios for improvement in cognition (at least 3 points in the SKT or at least 4 points on the ADAS-cog). (B) Odds ratios for improvement in CGIC and ADCS-CGIC.
Abbreviations: EGb, EGb 761®; CGIC, Clinical Global Impression of Change; ADAS-cog, cognitive subscale of the Alzheimer’s Disease Assessment Scale; ADCS-CGIC, Alzheimer’s Disease Cooperative Study Clinical Global Impression of Change; CI, confidence interval; M-H, Mantel-Haenszel test; SKT, Short Cognitive Performance Test (Syndrom-Kurztest).
Clinical global impression
Traditional CGIC, ADCS-CGIC, and GBS total scores were used to evaluate global change from baseline as described above. Meta-analysis of treatment response combines data from clinical trials using traditional CGIC and ADCS-CGIC.
In three trials,13,33,34,36 the odds ratios for improvement were significantly higher than 1. The combined odds ratio was statistically significant in favor of EGb 761 (odds ratio 3.18, 95% CI 1.78, 5.67; P<0.0001; Figure 4B). Heterogeneity (I2=81%) was mainly caused by one trial.33,34 Excluding this trial resulted in an I2 of 63%, and the superiority of EGb 761 compared with placebo remained statistically significant.
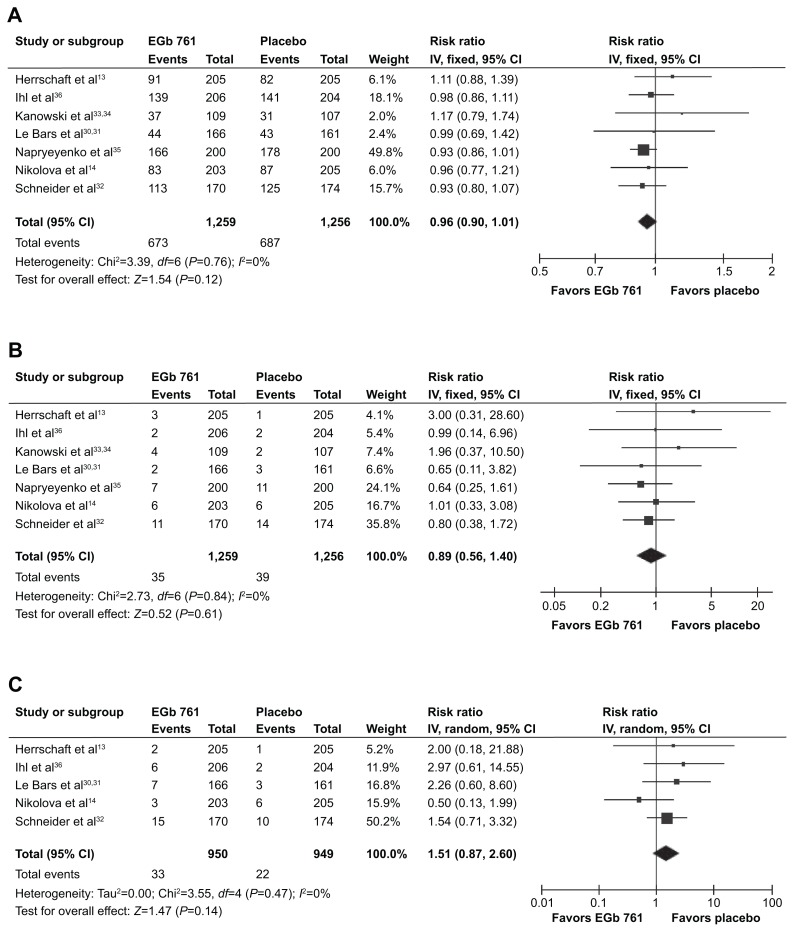
Adverse events
The proportions of patients who reported at least one adverse event were slightly higher with EGb 761 than with placebo in two studies.13,33,34 Nearly equal proportions in both treatment groups were observed in five trials.14,30–32,35,36 Overall, there is no suggestion of an increased risk for adverse events under active treatment (RR 0.96, 95% CI 0.90, 1.01; Figure 5A). The numbers of patients with serious adverse events were comparable across treatment groups in all included trials (RR 0.89, 95% CI 0.56, 1.40; Figure 5B).13,14,30–36 The adverse events reported most frequently were headache (EGb 761 11% and placebo 14%), dizziness (5% and 9%, respectively), hypertension (4% and 4%, respectively), tinnitus (3% and 4%, respectively), angina pectoris (3% and 4%, respectively), and respiratory tract infections (3% and 3%, respectively).
Figure 5.
Safety analyses.
Notes: (A) Patients reporting at least one adverse event, (B) patients reporting at least one serious adverse event, and (C) patients who terminated the study prematurely due to an adverse event.
Abbreviations: CI, confidence interval; IV, inverse variance method; EGb, EGb 761®.
In two trials, study termination due to an adverse event was documented for only one patient (Kanowski et al33 placebo group; Napryeyenko et al35 EGb 761 group). These trials were therefore excluded from the overall evaluation. In four of the five remaining trials,13,30–32,36 the incidence of premature termination due to an adverse event was slightly higher in the EGb 761 group, whereas in one trial14 it was higher in the placebo group. Overall, the RR was slightly increased in patients taking EGb 761 (1.51, 95% CI 0.87, 2.60; Figure 5C). Adverse events that led to early termination in more than one case in either treatment group were typical symptoms of dementia, such as agitation (EGb 761, three patients; placebo, one patient), anxiety (two and one, respectively), and insomnia (two and none, respectively), or unspecific symptoms that may have a variety of underlying causes, such as constipation (EGb 761, two patients; placebo, one patient), nausea (two and none, respectively), headache (one and three), and dizziness (none and three).
Discussion
This meta-analysis included all large, randomized, placebocontrolled, double-blind clinical trials of the defined, quantified Ginkgo biloba extract EGb 761 in patients prospectively diagnosed with dementia (AD, VaD, or dementia with mixed AD/vascular pathology) in accordance with internationally accepted criteria, treated for at least 20 weeks, and assessing efficacy in at least two of the three traditionally specified domains, ie, cognition, ADL, and global rating. Meta-analyses demonstrate a statistically significant advantage of treatment with EGb 761 compared with placebo in improving cognition, ADL, and global rating of change from baseline. Including trials published recently, the results of the present meta-analyses add to and strengthen the findings from recent meta-analyses performed by others.9–12 With this up-to-date meta-analysis of seven randomized, placebo-controlled, double-blind trials comprising 2,625 patients and showing significant superiority over placebo in all three main domains of assessment, there is level Ia evidence of the efficacy of Ginkgo biloba extract EGb 761 in the treatment of dementia.51
A limitation of our meta-analysis is the heterogeneity of the clinical trials that enrolled varying proportions of patients with AD, VaD, and mixed pathology. We included from all studies the datasets on which the intention-to-treat analyses were based, rather than subsets from patients with different etiologies. However, no systematic increase or decrease in effect sizes was observed with higher or lower proportions of patients with vascular pathology. To draw firm conclusions with regard to efficacy in the subgroups with AD, VaD, or mixed dementia, further meta-analyses using datasets from these subgroups will be necessary, which is beyond the intention of this review. The heterogeneity of effect sizes was accounted for by using a random effects model. Treatment effects were nevertheless statistically significant.
The results of these meta-analyses indicate that a 240 mg dose of EGb 761 is required daily to achieve clinically significant effects. They further support the notion that NPS are important effect modifiers, as suggested earlier by Ihl et al.52 While the one study that strictly excluded patients with clinically significant NPS showed hardly any treatment effects,32 significant effects across the three outcomes of interest were found in most studies in which nearly all patients had NPS at baseline,13,14,30,31,33–36 and the effects were most pronounced in studies that only included patients with clinically significant NPS.13,35,36
EGb 761 was well tolerated in all evaluated trials, with rates of adverse events, serious adverse events, and premature adverse event-related withdrawals not being conspicuously different between the active treatment groups and placebo. The most frequent adverse events that affected more than 2% of patients did not point toward any specific risk of treatment with EGb 761. The few types of adverse events that led to discontinuation of treatment in more than one patient in either treatment group were predominantly symptoms typical for dementia; the numbers were too low to indicate differences between treatment groups beyond chance.
Conclusion
Overall, this meta-analysis demonstrates the clinical efficacy, safety, and tolerability of Ginkgo biloba extract EGb 761 at daily doses of 240 mg in the treatment of patients with dementia.
Acknowledgment
Stefan Wellek, PhD, Professor Emeritus of Biostatistics, University of Heidelberg, and Head of the Department of Biostatistics, Mannheim Central Institute of Mental Health, conducted independent meta-analyses of the data on continuous variables presented in this review. He received the summary statistics for the individual clinical trials from the authors, and verified step by step all results for continuous variables contained in the forest plots and tables.
Footnotes
Disclosure
This independent statistical analysis was funded by Dr Willmar Schwabe GmbH & Co. KG. The systematic search of the pertinent literature and extraction of the studies eligible for meta-analysis was the sole responsibility of the authors. SG has received a speaker honorarium from Dr Willmar Schwabe GmbH & Co. KG, and SS is an employee of Dr Willmar Schwabe GmbH & Co. KG, receiving a fixed salary.
References
- 1.Kling MA, Trojanowski JQ, Wolk DA, Lee VMY, Arnold SE. Vascular disease and dementias: paradigm shifts to drive research in new directions. Alzheimers Dement. 2013;9(1):76–92. doi: 10.1016/j.jalz.2012.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schneider JA, Arvanitakis Z, Bang W, Bennett DA. Mixed brain pathologies account for most dementia cases in community-dwelling older persons. Neurology. 2007;69(24):2197–2204. doi: 10.1212/01.wnl.0000271090.28148.24. [DOI] [PubMed] [Google Scholar]
- 3.Ihl R, Frölich L, Winblad B, Schneider L, Burns A, Möller HJ WFSBP Task Force on Treatment Guidelines for Alzheimer’s Disease and other Dementias. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of Alzheimer’s disease and other dementias. World J Biol Psychiatry. 2011;12(1):2–32. doi: 10.3109/15622975.2010.538083. [DOI] [PubMed] [Google Scholar]
- 4.Abdel-Kader R, Hauptmann S, Keil U, et al. Stabilization of mitochondrial function by Ginkgo biloba extract (EGb 761®) Pharmacol Res. 2007;56(6):493–502. doi: 10.1016/j.phrs.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 5.Tchantchou F, Xu Y, Wu Y, Christen Y, Luo Y. EGb 761® enhances adult hippocampal neurogenesis and phosphorylation of CREB in transgenic mouse model of Alzheimer’s disease. FASEB J. 2007;21(10):2400–2408. doi: 10.1096/fj.06-7649com. [DOI] [PubMed] [Google Scholar]
- 6.Wu Y, Wu Z, Butko P, et al. Amyloid-β-induced pathological behaviors are suppressed by Ginkgo biloba extract EGb 761® and ginkgolides in transgenic Caenorhabditis elegans. J Neurosci. 2006;26(50):13102–13113. doi: 10.1523/JNEUROSCI.3448-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Költringer P, Langsteger W, Ober O. Dose-dependent hemorheological effects and microcirulatory modifications following intravenous administration of Ginkgo biloba special extract EGb 761. Clin Hemorheol. 1995;15(4):649–656. [Google Scholar]
- 8.Yoshitake T, Yoshitake S, Kehr J. The Ginkgo biloba extract EGb 761® and its main constituent flavonoids and ginkgolides increase extracellular dopamine levels in the rat prefrontal cortex. Br J Pharmacol. 2010;159(3):659–668. doi: 10.1111/j.1476-5381.2009.00580.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang BS, Wang H, Song YY, et al. Effectiveness of standardized Ginkgo biloba extract on cognitive symptoms of dementia with a six-month treatment: a bivariate random effect meta-analysis. Pharmacopsychiatry. 2010;43(3):86–91. doi: 10.1055/s-0029-1242817. [DOI] [PubMed] [Google Scholar]
- 10.Weinmann S, Roll S, Schwarzbach C, Vauth C, Willich SN. Effects of Ginkgo biloba in dementia: systematic review and meta-analysis. BMC Geriatr. 2010;10:14. doi: 10.1186/1471-2318-10-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Janssen IM, Sturtz S, Skipka G, Zentner A, Garrido MV, Busse R. Ginkgo biloba in Alzheimer’s disease: a systematic review. Wien Med Wochenschr. 2010;160(21–22):539–546. doi: 10.1007/s10354-010-0844-8. [DOI] [PubMed] [Google Scholar]
- 12.Yang Z, Li WJ, Huang T, Chen JM, Zhang X. Meta-analysis of Ginkgo biloba extract for the treatment of Alzheimer’s disease. Neural Regen Res. 2011;6(15):1125–1129. [Google Scholar]
- 13.Herrschaft H, Nacu A, Likhachev S, Sholomov I, Hoerr R, Schlaefke S. Ginkgo biloba extract EGb 761® in dementia with neuropsychiatric features: a randomised, placebo-controlled trial to confirm the efficacy and safety of a daily dose of 240 mg. J Psychiatr Res. 2012;46(6):716–723. doi: 10.1016/j.jpsychires.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 14.Nikolova G, Yancheva S, Raychev I, Hoerr R for the PLAGIN Study Group. Ginkgo biloba extract in dementia: a 22-week randomised, placebo-controlled, double-blind trial. Bulgarian Neurology. 2013;14(3):139–143. [Google Scholar]
- 15.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Third Edition, Revised. Washington, DC, USA: American Psychiatric Association; 1987. [Google Scholar]
- 16.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition. Washington, DC, USA: American Psychiatric Association; 1994. [Google Scholar]
- 17.World Health Organization. International Statistical Classification of Diseases and Related Health Problems Tenth Revision. Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- 18.McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34(7):939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- 19.Roman GC, Tatemichi TK, Erkinjuntti T, et al. Vascular dementia: diagnostic criteria for research studies. Report of the NINDS-AIREN International Workshop. Neurology. 1993;43(2):250–260. doi: 10.1212/wnl.43.2.250. [DOI] [PubMed] [Google Scholar]
- 20.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration; 2011. [Accessed July 8, 2014]. Version 5.1.0. Available from: http://handbook.cochrane.org/ [Google Scholar]
- 22.Weitbrecht WU, Jansen W. Placebo-kontrollierte Doppelblindstudie zur Wirksamkeit von Ginkgo-biloba-Extrakt bei geriatrischen Patienten mit primär degenerativer Demenz. [Ginkgo-biloba extract in the treatment of primary degenerative dementia. Placebo-controlled, double-blind and comparative study]. Fortschr Med. 1986;104(9):199–202. German. [PubMed] [Google Scholar]
- 23.Rai GS, Shovlin C, Wesnes KA. A double-blind, placebo controlled study of Ginkgo biloba extract (‘tanakan’) in elderly outpatients with mild to moderate memory impairment. Curr Med Res Opin. 1991;12(6):350–355. doi: 10.1185/03007999109111504. [DOI] [PubMed] [Google Scholar]
- 24.Mancini M, Agozzino B, Bompani E. [Clinical and therapeutic effects of Ginkgo-biloba extract EGb compared to placebo in the treatment of patients affected by senile psychoorganic dementia on an arteriosclerotic basis]. Gazz Med Ital. 1993;152:69–80. Italian. [Google Scholar]
- 25.Hofferberth B. The efficacy of EGb 761 in patients with senile dementia of the Alzheimer type. A double-blind, placebo-controlled study on different levels of investigation. Hum Psychopharmacol. 1994;9(3):215–222. [Google Scholar]
- 26.Maurer K, Ihl R, Dierks T, Frolich L. Clinical efficacy of Ginkgo biloba spezial extract EGb 761 in dementia of the Alzheimer type. J Psychiatr Res. 1997;31(6):645–655. doi: 10.1016/s0022-3956(97)00022-8. [DOI] [PubMed] [Google Scholar]
- 27.van Dongen M, van Rossum E, Kessels A, Sielhorst H, Knipschild P. Ginkgo for elderly people with dementia and age-associated memory impairment: a randomized clinical trial. J Clin Epidemiol. 2003;56(4):367–376. doi: 10.1016/s0895-4356(03)00003-9. [DOI] [PubMed] [Google Scholar]
- 28.Mazza M, Capuano A, Bria P, Mazza S. Ginkgo biloba and donepezil: a comparison in the treatment of Alzheimer’s dementia in a randomized placebo-controlled double-blind study. Eur J Neurol. 2006;13(9):981–985. doi: 10.1111/j.1468-1331.2006.01409.x. [DOI] [PubMed] [Google Scholar]
- 29.McCarney R, Fisher P, Iliffe S, et al. Ginkgo biloba for mild to moderate dementia in a community setting: a pragmatic randomised, parallel-group, double-blind, placebo-controlled trial. Int J Geriatr Psychiatry. 2008;23(12):1222–1230. doi: 10.1002/gps.2055. [DOI] [PubMed] [Google Scholar]
- 30.Le Bars PL, Katz MM, Berman N, Itil TM, Freedman AM, Schatzberg AF for the North American EGb Study Group. A placebo-controlled, double-blind, randomized trial of an extract of Ginkgo biloba for dementia. JAMA. 1997;278(16):1327–1332. doi: 10.1001/jama.278.16.1327. [DOI] [PubMed] [Google Scholar]
- 31.Le Bars PL, Kieser M, Itil KZ. A 26-week analysis of a double-blind, placebo-controlled trial of the Ginkgo biloba extract EGb 761® in dementia. Dement Geriatr Cogn Disord. 2000;11(4):230–237. doi: 10.1159/000017242. [DOI] [PubMed] [Google Scholar]
- 32.Schneider LS, DeKosky ST, Farlow MR, Tariot PN, Hoerr R, Kieser M. A randomized, double-blind, placebo-controlled trial of two doses of Ginkgo biloba extract in dementia of the Alzheimer’s type. Curr Alzheimer Res. 2005;2(5):542–551. doi: 10.2174/156720505774932287. [DOI] [PubMed] [Google Scholar]
- 33.Kanowski S, Herrmann WM, Stephan K, Wierich W, Hoerr R. Proof of efficacy of the ginkgo biloba special extract EGb 761 in outpatients suffering from mild to moderate primary degenerative dementia of the Alzheimer type or multi-infarct dementia. Pharmacopsychiatry. 1996;29(2):47–56. doi: 10.1055/s-2007-979544. [DOI] [PubMed] [Google Scholar]
- 34.Kanowski S, Hoerr R. Ginkgo biloba extract EGb 761 in dementia: intent-to-treat analyses of a 24-week, multi-center, double-blind, placebo-controlled, randomized trial. Pharmacopsychiatry. 2003;36(6):297–303. doi: 10.1055/s-2003-45117. [DOI] [PubMed] [Google Scholar]
- 35.Napryeyenko O, Borzenko I for the GINDEM-NP Study Group. Ginkgo biloba special extract in dementia with neuropsychiatric features. A randomised, placebo-controlled, double-blind clinical trial. Arzneimittelforschung. 2007;57(1):4–11. doi: 10.1055/s-0031-1296579. [DOI] [PubMed] [Google Scholar]
- 36.Ihl R, Bachinskaya N, Korczyn A, et al. Efficacy and safety of a once-daily formulation of Ginkgo biloba extract EGb 761® in dementia with neuropsychiatric features. A randomized controlled trial. Int J Geriatr Psychiatry. 2011;26(11):1186–1194. doi: 10.1002/gps.2662. [DOI] [PubMed] [Google Scholar]
- 37.Hoerr R. Behavioural and psychological symptoms of dementia (BPSD): effects of EGb 761®. Pharmacopsychiatry. 2003;36( Suppl 1):S56–S61. doi: 10.1055/s-2003-40451. [DOI] [PubMed] [Google Scholar]
- 38.Erzigkeit H. SKT Manual A Short Cognitive Performance Test for Assessing Memory and Attention. Weinheim; Germany: Beltz Test; 1992. [DOI] [PubMed] [Google Scholar]
- 39.Kim YS, Nibbelink DW, Overall JE. Factor structure and scoring of the SKT test battery. J Clin Psychol. 1993;49(1):61–71. doi: 10.1002/1097-4679(199301)49:1<61::aid-jclp2270490109>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 40.Rosen WG, Mohs RC, Davis KL. A new rating scale for Alzheimer’s disease. Am J Psychiatry. 1984;141(11):1356–1364. doi: 10.1176/ajp.141.11.1356. [DOI] [PubMed] [Google Scholar]
- 41.Lehfeld H, Rudinger G, Rietz C, et al. Evidence of the cross-cultural stability of the factor structure of the SKT short test for assessing deficits of memory and attention. Int Psychogeriatr. 1997;9(2):139–153. doi: 10.1017/s1041610297004304. [DOI] [PubMed] [Google Scholar]
- 42.Lehfeld H, Reisberg B, Finkel S, et al. Informant-rated activities-of-daily-living (ADL) assessments: results of a study of 141 items in the USA, Germany, Russia, and Greece from the International ADL Scale Development Project. Alzheimer Dis Assoc Disord. 1997;11( Suppl 4):S39–S44. [PubMed] [Google Scholar]
- 43.Ihl R, Grass-Kapanke B, Jänner M, Weyer G. Neuropsychometric tests in cross sectional and longitudinal studies – a regression analysis of ADAS-cog, SKT and MMSE. Pharmacopsychiatry. 1999;32(6):248–254. doi: 10.1055/s-2007-991102. [DOI] [PubMed] [Google Scholar]
- 44.Schwartz GE. Development and validation of the Geriatric Evaluation by Relatives Rating Instrument (GERRI) Psychol Rep. 1983;53(2):479–488. doi: 10.2466/pr0.1983.53.2.479. [DOI] [PubMed] [Google Scholar]
- 45.Bråne G, Gottfries CG, Winblad B. The Gottfries-Bråne-Steen Scale: validity, reliability and application in anti-dementia drug trials. Dement Geriatr Cogn Disord. 2001;12(1):1–14. doi: 10.1159/000051230. [DOI] [PubMed] [Google Scholar]
- 46.Reisberg B, Finkel S, Overall J, et al. The Alzheimer’s Disease Activities of Daily Living International Scale (ADL–IS) Int Psychogeriatr. 2001;13(2):163–181. doi: 10.1017/s1041610201007566. [DOI] [PubMed] [Google Scholar]
- 47.Oswald WD, Fleischmann UM. Nuremberg Gerontopsychological Inventory (NAI) Göttingen, Germany: Hogrefe; 1995. Third Revised Supplementary Edition. [Google Scholar]
- 48.National Institute of Mental Health. 028 CGI. Clinical Global Impressions. In: Guy W, Bonato RR, editors. ECDEU Assessment Manual for Psychopharmacology. Revised Edition. Rockville, MD, USA: National Institute of Mental Health; 1976. [Google Scholar]
- 49.Schneider LS, Olin JT, Doody RS, et al. Validity and reliability of the Alzheimer’s Disease Cooperative Study-Clinical Global Impression of Change. Alzheimer Dis Assoc Disord. 1997;11( Suppl 2):S22–S32. doi: 10.1097/00002093-199700112-00004. [DOI] [PubMed] [Google Scholar]
- 50.Rogers SL, Farlow MR, Doody RS, Mohs R, Friedhoff LT the Donepezil Study Group. A 24 week, double-blind, placebo-controlled trial of donepezil in patients with Alzheimer’s disease. Neurology. 1998;50(1):136–145. doi: 10.1212/wnl.50.1.136. [DOI] [PubMed] [Google Scholar]
- 51.European Medicines Agency. Guideline on the assessment of clinical safety and efficacy in the preparation of community herbal monographs for well-established and of community herbal monographs/entries to the community list for traditional herbal medicinal products/substances/preparations. London, UK: European Medicines Agency; 2006. [Accessed October 25, 2014]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500003644.pdf. [Google Scholar]
- 52.Ihl R, Tribanek M, Bachinskaya N. Baseline neuropsychiatric symptoms are effect modifiers in Ginkgo biloba extract (EGb 761®) treatment of dementia with neuropsychiatric features. Retrospective data analyses of a randomized controlled trial. J Neurol Sci. 2010;299(1–2):184–187. doi: 10.1016/j.jns.2010.08.033. [DOI] [PubMed] [Google Scholar]