Abstract
CCAAT-enhancer binding protein β (C/EBPβ) is a transcription factor that has a critical role in mammary gland development and breast cancer progression. Loss of C/EBPβ increases metastatic dissemination of mouse mammary tumor cells. However, the mechanism by which C/EBPβ expression affects metastasis formation remains unknown. This study aims at determining the relationship between C/EBPβ and survival of breast cancer patients, and elucidating C/EBPβ's link with metastasis formation. C/EBPβ expression was evaluated in 137 cases of human breast cancer, and the correlation with overall survival was estimated by Kaplan–Meier analysis. Additionally, the mouse 4T1 tumor model was used for in vivo studies. Decreased C/EBPβ expression was found to be associated with shorter overall survival of breast cancer patients. In the murine 4T1 model, loss of C/EBPβ affects tumor growth, morphology and promotes metastatic spread to the lungs. Immunohistochemical analyses showed that C/EBPβ inhibition leads to increased major histocompatibility complex II (MHCII) expression, followed by the accumulation of CD45-, CD3- and CD4-positive (CD4+) lymphocytes in the tumors. Inflammation involvement in C/EBPβ-mediated metastasis formation was confirmed by DNA microarray and by experiments on CD4+ cell-deprived nude mice. Additionally, anti-CD3 and anti-CD4 treatments of C/EBPβ-silenced tumor-bearing mice resulted in reverting the C/EBPβ effect on tumor growth and metastasis. Altogether, C/EBPβ is a predictor of overall survival in breast cancer patients, and affects tumor growth, morphology and lung metastasis formation in murine 4T1 model. The mechanism of metastasis formation involves immunologic response depending on C/EBPβ-mediated activation of MHCII and accumulation of CD4+ lymphocytes in the tumor.
Introduction
Breast cancer is the most common malignancy among women and is a significant health problem in the world. Metastatic spread of cancer cells to organs such as the lungs and the liver is the major cause of death in breast cancer, and in many other cancer types. Currently, there is a lack of therapies targeting metastatic process, and also of diagnostic markers predicting the metastatic capacity of a certain tumor.
Existing tools for diagnosis and treatment of cancer rely on the evaluation of prognostic factors such as tumor size, histopathologic type, patient's age, presence of metastasis and expression of specific proteins (receptors for estrogen, progesterone, human epidermal growth factor receptor 2 (HER2)/neu, K-ras, B-raf, and so on). With the current stage of imaging and histopathologic examination, the multifactorial nature of the diagnosis makes the correct evaluation of the disease stage difficult and expensive. Therefore, finding new markers of disease progression and mechanisms related to disease development is pivotal for successful progress in the breast cancer field. In particular, it would be useful to identify early markers of invasion that can predict metastatic spread of cancer cells, and thereby prognosis.
Recently, we found that loss of the transcription factor CCAAT-enhancer binding protein β (C/EBPβ), which has an essential role in mammary epithelium differentiation,1, 2, 3 promotes epithelial–mesenchymal transition and invasion in breast cancer.4 Mechanistic studies revealed that C/EBPβ protects against epithelial–mesenchymal transition by acting as a transcriptional activator of epithelial junction proteins including E-cadherin and the coxsackie and adenovirus receptor. However, it is unknown whether loss of C/EBPβ expression is a prognostic factor in breast cancer. So far, it has only been shown that C/EBPβ is involved in progression of glioblastoma and lymphoma.5, 6 C/EBPβ is produced, through alternative initiation of translation, in three isoforms: the two transcriptional activators liver-activating protein 1 and 2, and liver inhibitory protein, which is believed to inhibit C/EBPβ-mediated gene activation.3 An excess of the C/EBPβ inhibitory isoform liver inhibitory protein is implicated in breast cancer progression.7, 8, 9
In this study, we performed immunohistochemical analysis to determine whether C/EBPβ can be used as a prognostic marker in human breast cancer. Indeed, we found that C/EBPβ is a factor related to survival of breast cancer patients. In addition, we used the 4T1 breast cancer mouse model and microarray analysis to determine mechanisms by which loss of C/EBPβ promotes formation of lung metastasis. We found a novel mechanism linking directly loss of C/EBPβ to major histocompatibility complex II (MHCII) activation and indirectly to the accumulation of CD4-positive (CD4+) lymphocytes. In support of this, lack of CD4+ T cells in short hairpin (sh) C/EBPβ tumor-bearing mice attenuated the effect of C/EBPβ on metastasis formation and tumor growth.
Results
C/EBPβ predicts overall survival in breast cancer patients
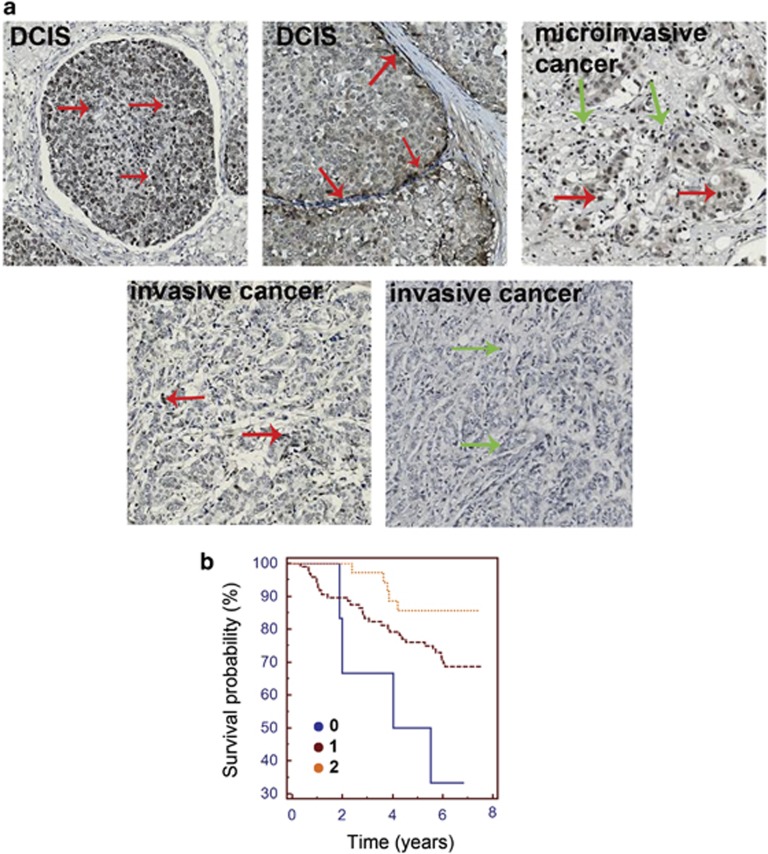
A descriptive analysis of tissue microarray showed strong nuclear positive staining for C/EBPβ in normal breast tissue and in ductal cancer in situ (Figure 1a, upper left and middle panel). However, C/EBPβ expression in ductal cancer in situ was lower compared with the expression in normal breast tissue, and in many nodules it was mostly present in their basal layer. These nodules were surrounded by desmoplastic stroma infiltrated with lymphocytes. Thus, C/EBPβ staining intensity was lower in case of inflammation combined with desmoplastic reaction in the tumor stroma. This phenomenon was strongly visible particularly in areas of microinvasive cancer (Figure 1a, upper right panel). Decreased C/EBPβ expression was observed in areas of invasive cancer, especially low in areas with strong lymphocytic infiltration (Figure 1a, lower panels), which indicates that C/EBPβ might have a role in progression of breast cancer and appearance of inflammation.
Figure 1.
C/EBPβ expression in breast cancer. (a) Different areas within breast cancer tissue: upper left—ductal cancer in situ (DCIS); upper middle—basal layer of DCIS; upper right panel—microinvasive cancer; and lower panels—invasive cancer. Red arrows indicate cancer cells; green arrows indicate lymphocytes. (b) Kaplan–Meier plot of overall survival of breast cancer patients stratified according to 0–2 scale based on C/EBPβ expression.
The descriptive analysis of patients is presented in Table 1. Univariate and multivariate analyses were used to assess the effect of C/EBPβ expression on overall survival (OS) of patients, adjusted for established prognostic factors (Table 2). All parameters were assessed in univariate models using Cox proportional hazards models and factors significant at P<0.05 were included in the final multivariate analysis. In univariate analysis, independent predictors of OS were C/EBPβ expression (hazard ratio (HR) 0.392; 95% confidence interval (CI): 0.201–0.764; P=0.006), relapse-free survival (RFS) (HR 0.554; 95% CI: 0.49–0.625; P=0.001), age (HR 1.067; 95% CI: 1.038–1.096; P=0.001), menopausal status (HR 1.002; 95% CI: 1–1.003; P=0.013), tumor size (HR 1.018; 95% CI: 1.009–1.028; P=0.001), lymph node status (HR 1.961; 95% CI: 1.295–2.969; P=0.001), HER2 status (HR 1.64; 95% CI: 1.223–2.198; P=0.001), estrogen receptor status (HR 0.39; 95% CI: 0.19–0.802; P=0.01), luminal A subtype (HR 0.319; 95% CI: 0.165–0.617; P=0.001) and luminal B subtype (HR 3.802; 95% CI: 1.342–10.77; P=0.012). For the multivariate analyses, all potentially significant biochemical variables (P<0.05) in the univariate analyses were included. In multivariate analysis, independent predictors of OS were C/EBPβ expression (P=0.046) and age (P=0.01).
Table 1. Characteristics of breast cancer patients stratified according to 0–2 scale based on C/EBPβ expression.
|
C/EBPβ expression |
0 |
1 |
2 |
| Number of patients | 6 | 96 | 35 |
| Age (years)±s.d. | 70.2±24 | 64.9±13.3 | 64.6±12.3 |
| tumor size (mm)±s.d. | 29.3±12.8 | 26.3±21.3 | 24.1±16.6 |
| ER+ (%) | 6 (100%) | 82 (85) | 31 (89) |
| ER− (%) | 0 (0) | 14 (15) | 4 (11) |
| PR+ (%) | 5 (83) | 65 (68) | 23 (66) |
| PR− (%) | 1 (17) | 31 (32) | 12 (34) |
| HER2+ (%) | 2/6 (33) | 36/94 (38) | 13/33 (39) |
| HER2− (%) | 4/6 (67) | 58/94 (62) | 20/33 (61) |
| Lymph node metastasis+ | 4/6 (67) | 36/86 (42) | 15/31 (48) |
| RFS (years)±s.d. | 3.4±2.3 | 5.3±2.4 | 6.1±1.6 |
| OS (years)±s.d. | 4.5±2.4 | 5.6 ±2.1 | 6.3±1.2 |
| Relapse event (%) | 2/6 (33) | 20/96 (21) | 6/35 (17) |
| Mortality (%) | 4/6 (66) | 30/96 (31) | 5/35 (14) |
| Luminal A (%) | 5/6 (83) | 70/91 (77) | 26/32 (81) |
| Luminal B (%) | 0/6 (0) | 4/92 (4) | 2/34 (6) |
| Basal (triple neg.) (%) | 0/6 (0) | 12/92 (13) | 2/34 (6) |
| Ki67 grade 0 (%) | 0/6 (0) | 7/86 (8) | 0/27 (0) |
| Ki67 grade 1 (%) | 3/6 (50) | 33/86 (38) | 14/27 (52) |
| Ki67 grade 2 (%) | 3/6 (50) | 46/86 (54) | 13/27 (48) |
Abbreviations: C/EBPβ, CCAAT-enhancer binding protein β ER, estrogen receptor; HER2, human epidermal growth factor receptor 2; OS, overall survival; PR, progesterone receptor; RFS, relapse-free survival; s.d., standard deviation.
Table 2. Results of univariate and multivariate analyses.
| Patient characteristics | Univariate analysis HR (95% CI) | P-value | Multivariate analysis (P-value) |
|---|---|---|---|
| C/EBP β | 0. 392 (0.201–0.764) | 0.006 | 0.046 |
| Tumor side | 1.33 (0.706–2.504) | 0.378 | — |
| RFS | 0.554 (0.49–0.625) | 0.001 | — |
| Age (years) | 1.067 (1.038–1.096) | 0.001 | 0.001 |
| Menopausal status | 1.002 (1–1.003) | 0.013 | 0.419 |
| Chemotherapy | 1.447 (0.703–2.979) | 0.316 | — |
| Endocrine therapy | 0.778 (0.402–1.505) | 0.456 | — |
| Tumor size | 1.018 (1.009–1.028) | 0.001 | — |
| Lymph node status | 1.961 (1.295–2.969) | 0.001 | 0.05 |
| HER2 status | 1.64 (1.223–2.198) | 0.001 | 0.422 |
| ER status | 0.39 (0.19–0.802) | 0.01 | 0.097 |
| PR status | 0.419 (0.223–0.786) | 0.07 | — |
| Luminal A | 0.319 (0.165–0.617) | 0.001 | 0.413 |
| Luminal B | 3.802 (1.342–10.77) | 0.012 | 0.175 |
| Basal (triple negative) | 2.039 (0.897–4.632) | 0.089 | — |
Abbreviations: C/EBPβ, CCAAT-enhancer binding protein β CI, confidence interval; ER, estrogen receptor; HER2, human epidermal growth factor receptor 2; HR, hazard ratio; PR, progesterone receptor; RFS, relapse-free survival. Bold and italic numerals mark probability that was considered statistically significant (P<0.05).
Moreover, the results were confirmed by Kaplan–Meier analysis and were also used to assess the effect of C/EBPβ expression on OS. Lack of C/EBPβ expression in patient samples was associated with shorter OS of breast cancer patients (4.5±2.4 years) compared with higher C/EBPβ expression (respectively, in qualitative scale: 5.6±2.1 years for C/EBPβ expression +1 and 6.3±1.2 years for C/EBPβ expression +2). These results indicate that C/EBPβ expression is significantly associated with OS (Figure 1b). Interestingly, patients lacking C/EBPβ expression had more often lymph node metastasis (67%) compared with patients with higher C/EBPβ expression (respectively, 38% for C/EBPβ expression +1 and 43% for C/EBPβ expression +2).
Loss of C/EBPβ affects tumor growth and morphology in a murine 4T1 tumor model
C/EBPβ knockdown was confirmed by immunofluorescence staining of the cells and western blot (Figure 2a). Mouse experiments using those cells showed that loss of C/EBPβ expression affects tumor growth and morphology. C/EBPβ-silenced tumors grew smaller compared with non-silenced tumors (133±16 vs 342±150 mm3; P=0.04), although there was no difference in proliferation rate assessed by in vitro assay (Figure 2b).
Figure 2.
Effect of loss of C/EBPβ expression on tumor growth and morphology. (a) Left panel—light microscopy pictures and immunofluorescence staining of 4T1 cells; right panel—western blot showing small interfering RNA (siRNA) knockdown of C/EBPβ. (b) Left panel—4T1 tumor growth (sh control vs sh C/EBPβ) in BALB/c mice (n=8 mice per group); right panel—4T1 tumor cell proliferation (MTT assay). (c) Tumor morphology (sh control on left and sh C/EBPβ on right panel). (d) Tumor vessels stained by endothelial marker CD31 (sh control on upper left and sh C/EBPβ on upper right panel) and average tumor vessel count per field (n), whole-mount immunohistochemistry of tumor vasculature analyzed by Visiopharm software (middle panels), graphs of average tumor vessel area per field, average vessel length per field (in pixels), average number of branch points in tumor vessels per field (n) and average pericyte coverage of tumor vessels per field (in percentage).
Additionally, a striking morphological difference was observed between the tumors. Although C/EBPβ-expressing tumors were characterized by large central necrosis, C/EBPβ-silenced tumors formed solid tumors with extensive, pushing border growing pattern and inflammation around them (Figure 2c).
To further characterize the effect of C/EBPβ on the tumor, tumor vasculature was analyzed by immunohistochemical staining for endothelial cell marker CD31. As indicated in Figure 2d (upper panels), there were more vessels in C/EBPβ-silenced tumors compared with non-silenced tumors (120±18 vs 78±14; P<0.05).
The study of the tumor vasculature was followed by whole-mount immunohistochemistry on tumors, stained for both CD31 and a pericyte marker NG2. Results were analyzed by Visiopharm software (Visiopharm, Hoersholm, Denmark) as shown in Figure 2d (middle panels). Despite the previous results involving differences in vessel number, no significant differences in vessel morphology were found with respect to features such as vessel length, number, area, pericyte coverage and number of branch points, which were similar in both groups (Figure 2d).
Loss of C/EBPβ expression promotes lung metastasis formation in murine 4T1 tumor model
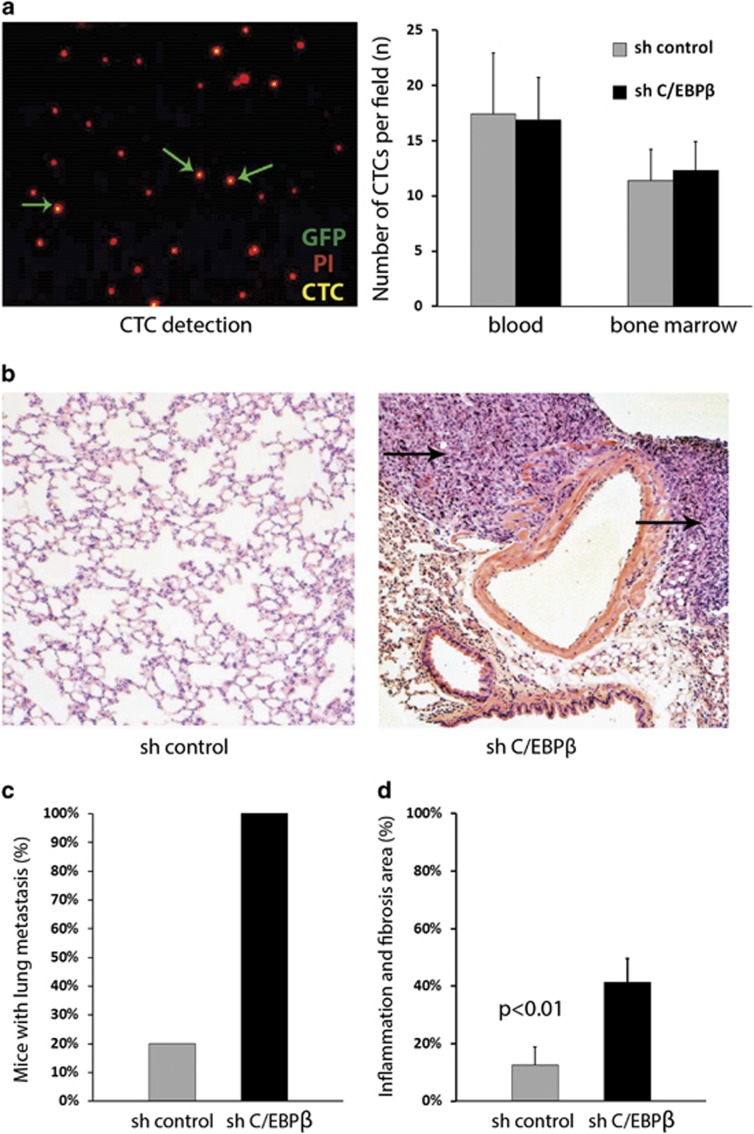
To study the effect of C/EBPβ on tumor spread and metastasis formation, focus was laid on the presence of CTCs in blood and bone marrow and the appearance of metastatic nodules in distant organs. In this model, the cells were labeled with enhanced green fluorescent protein positive, which allowed to calculate the CTC number in blood and bone marrow (Figure 3a, left panel). As shown in Figure 3a (right panel), no statistically significant differences in CTC count in the blood and bone marrow between sh control and sh C/EBPβ tumors were observed at the end point of the experiment.
Figure 3.
C/EBPβ influence on spreading and metastasis formation. (a) Blood cells of tumor-bearing mouse, stained with propidium iodide. Green arrows represent green fluorescent protein-positive (GFP+) CTCs (left panel); the number of CTCs in the blood and bone marrow of tumor-bearing mice 2 months after primary tumor excision is seen in the right panel. (b) Lungs of tumor-bearing mice stained for hematoxylin and eosin (sh control in the left vs sh C/EBPβ in the right panel). Arrow represents the metastasis area. (c) Percentage of tumor-bearing mice developing lung metastasis. (d) Lung area of tumor-bearing mice with chronic inflammation.
Next, morphological analysis of the lungs of tumor-bearing mice was performed to study if C/EBPβ knockdown affected metastatic spread (Figure 3b). All mice with silenced expression of C/EBPβ developed metastases in the lungs, which appeared only in 20% of mice in the non-silenced group (P<0.01), which indicated that C/EBPβ loss promotes metastatic spread of mammary 4T1 tumors (Figure 3c). Moreover, morphological analysis showed that lungs of mice carrying C/EBPβ knockdown had more prominent chronic inflammation with interstitial fibrosis vs lungs of C/EBPβ-expressing mice (0.4±0.1 vs 0.1±0.1; P<0.01) (Figure 3d). This observation is in agreement with the fact that C/EBPβ affects the formation of inflammatory process, as was previously found in human tissue microarrays analysis (Figure 1a).
C/EBPβ controls inflammation in murine 4T1 model
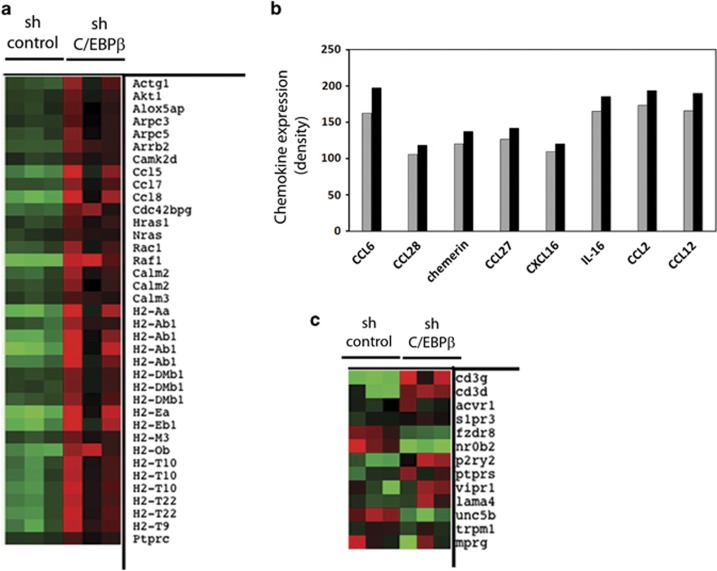
To unravel the mechanism of how C/EBPβ affects metastasis formation, a microarray analysis was performed using RNA extracts from 4T1 in vitro cells expressing C/EBPβ shRNA or control shRNA. Gene profiling revealed a set of 559 genes having statistically (P⩽0.05) different expression level in sh control vs sh C/EBPβ cells. The analysis carried out by Panther DB service (Los Angeles, CA, USA) indicated that, among the genes mentioned, genes encoding proteins involved in inflammation were the most significant group compared with gene groups related to other pathways. Thus, as shown in Figure 4a, the main focus was laid on the analysis of these genes. Representative genes included MHCIIα, MHCIIβ and HLACIIγ. Additionally, chemokines such as CCL5, CCL7 and CCL8 were affected.
Figure 4.
C/EBPβ controls inflammation. (a) Microarray analysis of 4T1 cells, (b) chemokine protein array in 4T1 cells and (c) microarray analysis of 4T1 tumors.
Following the chemokine analysis, the cells were further analyzed by chemokine protein array, which did not confirm the previous finding. However, many chemokines were upregulated in the sh C/EBPβ cells compared with sh control cells, such as CCL2, CCL6, CCL12, CCL27, CCL28, chemerin, CXCL16 and interleukin-16 (Figure 4b).
To distinguish the direct and indirect effects of C/EBPβ on tumors and to find if a similar pattern of gene expression could be observed in vivo, tumors dissected from mice were also profiled by microarray analysis, using RNA extracts from 4T1 tumors expressing C/EBPβ shRNA (n=3), or control tumors shRNA (n=3) (Figure 4c). It was important as tumors were composed not only of tumor cells but also of stromal cells and lymphocytes. In this setup, only 135 genes were upregulated in sh C/EBPβ vs sh control >1.3-fold. The results were further processed with Panther DB service, and, similar to previous findings on cells, inflammation-related group of genes was the most representative. Many of those genes are still uncharacterized and have unknown function; however, it is striking that CD3 was upregulated fivefold in sh C/EBPβ tumors vs sh control tumors. These results suggest that C/EBPβ is involved in the modulation of immunologic response in the tumors directly by controlling MHCII expression and indirectly by accumulating CD3+ lymphocytes in the tumor.
C/EBPβ is involved in MHCII activation and accumulation of CD4+ lymphocytes in the murine 4T1 tumor model
Taken together, the results of human breast cancer study, morphologic analysis of mouse tissue and tumor growth supported the microarray data and suggested that C/EBPβ is involved in metastatic process by controlling the expression of genes involved in inflammatory response. To confirm this finding, sh C/EBPβ and sh control tumors were stained for CD45, CD3, CD4 and MHCII and the number of positive cells was calculated (Figures 5a–d). C/EBPβ inhibition led to increased MHCII expression (142 ±17 vs 92±8; P<0.01), followed by accumulation of CD45 (897±112 vs 363±52; P<0.01), CD3 (126±27 vs 52±11; P<0.01) and CD4+ lymphocytes (496±240 vs 25±6; P<0.01) in the tumors. That finding showed the most striking and significant difference between the tumors, confirmed by both morphologic and microarray analysis.
Figure 5.
C/EBPβ is involved in the activation of MHCII and CD4+ lymphocytes. (a) Immunohistochemical staining of tumors for CD45, (b) for CD3, (c) for CD4 and (d) for MHCII. All graphs show calculated numbers of stained cells per field (n).
Lack of CD4+ T cells in sh C/EBPβ tumor-bearing mice attenuates the effect of C/EBPβ on tumor growth and metastasis formation
To study if the effect of C/EBPβ on tumor growth and metastasis can be reversed by specific treatment, mice bearing sh C/EBPβ tumors were treated with anti-CD3 or anti-CD4 antibodies. The results showed that sh C/EBPβ tumors grew much bigger when treated with either CD3 or CD4 antibodies (Figure 6a) compared with non-treated sh C/EBPβ tumors (227±28 and 229±18 mm3 vs 52±5 mm3; P<0.01), even though in wild-type mice C/EBPβ knockdown decreases tumor growth. Although no effect of treatment on the CTC count in the blood or bone marrow was observed in this model (Figure 6b), the experiment confirmed involvement of CD4 T cells in C/EBPβ-dependent tumor growth. Similar conclusion was drawn from a study in T-cell-deprived nude mice, where C/EBPβ-silenced tumors grew bigger than non-silenced tumors (3433±446 vs 2040±367 mm3; P<0.05) (Figure 6c, left panel). Furthermore, both groups had similar ratio of lung metastasis (Figure 6c, right panel), which confirms that in this model, C/EBPβ has a CD4-dependent effect on metastasis formation. Moreover, we have analyzed in detail human samples and found a confirmation for this hypothesis. Human samples negative for C/EBPβ were found to be positive for MHCII (Figure 6d).
Figure 6.
Lack of CD4+ T cells in sh C/EBPβ tumor-bearing mice attenuates the effect of C/EBPβ on tumor growth and metastasis formation. (a) 4T1 tumor growth (non-treated sh C/EBPβ, anti-CD3-treated sh C/EBPβ, anti-CD4-treated sh C/EBPβ) in BALB/c mice (n=8 mice per group). (b) Number of CTCs in the blood (left panel) and bone marrow (right panel) of tumor-bearing mice. (c) Tumor volume in nude mice 14 days after implantation (left panel) and percentage of nude tumor-bearing mice developing lung metastasis (right panel). (d) Human breast cancer tissue stained for MHCII (DAB) and C/EBPβ (Alexa 594).
Discussion
Here we report that C/EBPβ is a predictor of OS in breast cancer patients, and affects tumor growth, morphology and lung metastasis formation in murine 4T1 model. The mechanism of metastasis formation involves immunologic response depending on C/EBPβ-mediated activation of MHCII and accumulation of CD4+ lymphocytes in the tumor.
Tissue microarray analysis showed that C/EBPβ is a factor associated with tumor progression from in situ form to invasive cancer, and predictor of OS of breast cancer patients. Additionally, patients lacking C/EBPβ expression develop more often lymph node metastasis compared with patients bearing higher C/EBPβ expression in the tumors. A drawback of the presented study is that the immunohistochemical staining for C/EBPβ does not allow for distinguishing between different C/EBPβ isoforms. For example, it has already been observed that a high liver inhibitory protein:liver-activating protein ratio in human breast carcinomas correlates with more aggressive phenotype and poor prognosis.10, 11, 12 Surprisingly, this study does not confirm previously reported association of C/EBPβ with triple-negative breast cancer phenotype, and therefore epithelial–mesenchymal transition.4 However, owing to differences in clinical characteristics of the patient samples and their numbers used for immunohistochemistry, the experiments cannot be easily compared, and thus no valid conclusions can be drawn out of the study.
Mouse studies showed that, although no difference in proliferation rate in vitro was observed, C/EBPβ-silenced tumors grew smaller compared with non-silenced tumors. This suggests that 4T1 tumor growth is not directly regulated by C/EBPβ, but rather affected by in vivo factors. Namely, while C/EBPβ-expressing tumors had large central necrosis, C/EBPβ-silenced tumors were solid, intact and infiltrated with lymphocytes. This finding was related to changes in the number of vessels, which may be partly explained by the previously demonstrated involvement of the C/EBP family in vessel formation, where C/EBPδ has been shown to regulate vascular endothelial growth factor C autocrine signaling in lymphangiogenesis in lung cancer.13
Our animal experiments indicated that loss of C/EBPβ promotes metastatic spread of mammary 4T1 tumors. A direct link between C/EBPβ and metastasis has only been demonstrated in one previous in vivo study, where deletion of C/EBPβ in hematopoietic cell lineage led to a decrease in the number of pulmonary metastases in MN-MCA1 sarcoma-bearing mice.14
Here we show that inflammation-related group of genes was indicated by microarray as the most representative of all genes, which were statistically different between both examined cell and tumor tissue samples (C/EBPβ-silenced vs non-silenced). This gene group included, among others, genes such as MHCIIα, MHCIIβ, HLACIIγ, CCL5, CCL7 and CCL8. Additional immunohistochemical analyses indicated that inhibition of C/EBPβ leads to an increased expression of MHCII, followed by the accumulation of CD45+, CD3+ and CD4+ lymphocytes in the tumors. Hence, we concluded that C/EBPβ controls the immunologic response in murine 4T1 tumors via activation of MHCII and CD4+ lymphocytes.
Inflammation has a key role in the process of cancer growth and progression. Tumors can induce a T-cell tolerance against tumor antigens, creating an immunosuppressive environment that is highly beneficial for the tumor development. For example, profound changes in myelopoiesis induced by tumor growth15 lead to the recruitment of myeloid-derived suppressor cells, whose immunoregulatory activity depends on C/EBPβ.14, 16 Although the mechanisms of myeloid-derived suppressor cell-mediated CD8+ T-cell suppression have already been shown in a mouse tumor model,17 it remains unclear if similar antigen-specific mechanisms of myeloid-derived suppressor cell-mediated suppression act on CD4+ T cells.
CD4+ T cells have a central role in antitumor immunity. They provide regulatory signals necessary for the priming of MHCI-restricted CD8+ lymphocytes, which act as effectors for the tumor. Moreover, it has been proven that T helper type 1 and T helper type 2 responses are required for maximal systemic antitumor immunity.18 These types of T cells produce cytokines such as interferon γ and interleukin-4, which activate eosinophils and macrophages, contributing to tumor destruction.19 Many of these mechanisms depend on tumor phagocytosis by antigen-presenting cells, and consequently presentation on MHCII.
Even though CD4+ T cells are responsible for antitumor immunity, in other cellular contexts they also contribute to the development of tumor immunotolerance. Namely, high numbers of T helper type 17 and T regulatory cells (Tregs) have been observed in invasive ductal carcinoma patients and associated with tumor aggressiveness.20 Furthermore, stage IV breast cancer patients have more Tregs and a lower T helper/Tregs ratio compared with lower-stage breast cancer patients.21 High numbers of CD25+CD4+ regulatory cells were also correlated with higher Nottingham grade status and larger tumor size.22 Moreover, tumor-infiltrating Tregs can stimulate breast cancer metastasis to the lungs via the RANKL-RANK signaling pathway.23 Interestingly, RANKL expression is regulated by C/EBPβ,24 which suggests involvement of C/EBPβ in inflammation-related lung metastasis in breast cancer. This mechanism could explain the results observed in this study and point to Tregs as a potential therapeutic target for metastatic breast cancer. However, the results presented here do not provide information on which particular CD4+ T-cell subset is associated with C/EBPβ expression and metastasis.
A possible link between C/EBPβ, inflammation and metastasis may provide chemokines. Many studies showed that tumor-associated chemokines and their receptors have a fundamental role in determining metastatic destination of cancer cells.25, 26 Furthermore, chemokines have been shown to regulate inflammation within tumors and prevent the host's immune system from rejecting cancer.27 In this study, protein and DNA microarray analyses indicated that chemokines such as CCL2 (MCP-1) or CCL5 were upregulated in sh C/EBPβ cells compared with sh control cells. Interestingly, both chemokines have already been implicated in breast cancer metastasis. CCL2, produced by stromal tumor cells, not only has a crucial role in initiation and progression of cancer but also promotes lung metastasis of 4T1 cells.28 The CCL5/CCR5 axis on the other hand promotes invasiveness and metastasis in the aggressive, basal subtype of breast cancer.29
C/EBPβ is not the only member of the C/EBP family that is considered to be a tumor-related factor. For example, C/EBPα is often downregulated in breast cancer and has a role in its development and progression.30 C/EBPδ on the other hand regulates critical cell fate-determining programs, including growth arrest, migration and differentiation.31 Both C/EBPα and C/EBPδ genes are inactivated in acute myeloid leukemia, where the C/EBPα function is blocked by phosphorylation in acute myeloid leukemia patients carrying FLT3-activating mutations,32 whereas C/EBPδ is silenced by hypermethylation.33
According to our studies tumor growth and metastasis are controlled by C/EBPβ in an inflammation-dependent manner. We show that in wild-type mouse model, CD4+ T cells are responsible for immunosurveillance and inhibition of tumor growth, as well as control of tumor metastatic properties. In contrast, in CD4− nude mouse model, C/EBPβ regulates tumor growth and, simultaneously, loses control over tumor metastatic properties. Altogether, the obtained results contribute to the discovery of a new C/EBPβ-mediated immunoregulatory network controlling both tumor growth and metastasis.
Materials and methods
Clinical samples of human breast cancer
Tissue microarrays containing 137 samples of human metastatic breast cancer, previously described in Svensson et al.34 study, were kindly provided by Karin Jirström (Lund University, Lund, Sweden). The Research Ethics Review Board approved all studies. The study was carried out according to the principles embodied in the Declaration of Helsinki. According to the current guidelines, tumors were considered HER2+ if more than 10% of the tumor cells test positive for HER2 protein overexpression or HER2 gene amplification. Tumors that showed nuclear staining >10% were considered estrogen receptor or progesterone receptor positive, as this was and still is the routinely used cutoff in Sweden.
Cell lines
Two derivatives of green fluorescent protein-labeled 4T1 (CRL-2539; ATCC) cells were kindly provided by Professor Jonas Fuxe (Karolinska Institute, Solna, Sweden). Lentivirus-mediated knockdown of C/EBPβ was described previously in Johansson et al.4 Sh C/EBPβ cell line expressed C/EBPβ shRNA, whereas sh control expressed control shRNA. Both cell lines were cultured in RPMI-1640 (Gibco, Waltham, MA, USA) supplemented with 10% fetal calf serum and 1% penicillin and streptomycin in a humidified incubator at 37 °C in an atmosphere containing 5% CO2 and 95% O2.
Immunofluorescence staining
Immunofluorescence staining of cultured 4T1 cells was performed on cells grown on coverslips, which were fixed in absolute ethanol, permeabilized and stained with primary antibodies (rabbit α-C/EBPβ Santa Cruz Biotechnology, Santa Cruz, CA, USA; sc-150; 1:100), followed by incubation in secondary Alexa 488-conjugated anti-rabbit antibodies (1:500; Jackson ImmunoResearch, Suffolk, UK). Additionally, cells were stained with Alexa 647 Phalloidin (Life Technologies, Waltham, MA, USA) to visualize actin and counterstained with DAPI (4′,6-diamidino-2-phenylindole). Slides were examined and photographed using a Zeiss Axiophot fluorescence microscope (Carl Zeiss AG, Oberkochen, Germany).
Western blot analysis
Immunoblotting analysis of cell lysates from sh control and sh CEBPβ cells was performed according to standard procedures. Briefly, cells were lysed in RIPA buffer (50 mM Tris–HCl, pH 7.5, 150 mM NaCl, 1 mM EDTA, 1% NP-40, 0.5% sodium deoxycholate, 0.1% sodium dodecyl sulfate supplemented with protease inhibitors (Complete; Roche, Penzberg, Germany)) and total protein extracts were boiled in Laemmli sample buffer (Bio-Rad, Hercules, CA, USA), separated by sodium dodecyl sulfate–polyacrylamide gel electrophoresis under reducing conditions and transferred to nitrocellulose. Antibodies used in immunoblotting included rabbit α-C/EBPβ sc-150 (1:500; Santa Cruz Biotechnology) and rabbit α-Calnexin (1:2000; Santa Cruz Biotechnology). Immunoreactive bands were visualized by chemiluminescence (Supersignal; Pierce/Thermo Scientific/Nordic Biolabs, Waltham, MA, USA) and developed using an LAS1000 system (Fuji Photo Film Co., Tokyo, Japan).
Mouse tumor models
Approximately 2 × 106 of tumor cells (sh control or sh C/EBPβ) were subcutaneously implanted in the dorsal back of 6- to 8-week-old female wild-type BALB/c or nude BALB/c mice (n=8 per group) and tumor sizes were measured with a caliper every 2 days, starting from day 5 after implantation.
At certain timepoints after tumor implantation, mice were anesthetized with isoflurane before cardiac puncture, which was used as a method for blood collection. Subsequently, the mice were killed by cervical dislocation and their bone marrow and tumors were collected for further analysis. Samples of blood and bone marrow were hemolyzed, washed with phosphate-buffered saline (PBS) and stained with propidium iodide. Samples were then put on microscope slides and analyzed with a confocal microscope to count the number of circulating tumor cells per field, where green fluorescent protein was used to determine the CTC and propidium iodide the nucleus.
To study metastasis, primary tumors were surgically removed under analgesia and anesthesia 14 days after implantation. The experiment was continued for 2 months after tumor excision. Then, after blood collection, the animals were killed as previously described and their blood, bone marrow and lungs were collected for further analysis.
To study the effect of immunosuppression on tumor growth, BALB/c mice were subcutaneously implanted with sh C/EBPβ tumor cells as described previously and organized into non-treated, anti-CD3- or anti-CD4-treated group (n=8 mice per group). Mice were treated with intraperitoneal injections of 0.5 mg of CD3 or CD4 monoclonal antibody every 4 days, starting from 2 days before tumor implantation. The experiment lasted for 2 weeks and then the mice were killed and their blood and bone marrow collected.
Wild-type BALB/c mice were obtained from the Department of Microbiology, Tumor and Cell Biology (Karolinska Institute, Stockholm, Sweden) and nude BALB/c mice were obtained from Harlan Laboratories (Indianapolis, IN, USA). All animal studies were performed in accordance with international guidelines and Swedish law and approved by the Northern Stockholm Animal Welfare Committee, as well as by Karolinska Institute.
Microarray analysis
Tumor tissue was frozen immediately after excision from the animals and subsequently used for RNA extraction and microarray analysis. Cell pellets and well as four tissue samples were used for analyzing each group (sh control vs sh C/EBPβ). Gene expression profiles were analyzed using Nimblegen array (Basel, Switzerland).
Immunohistochemical stainings
Tumors as well as other murine tissues (brain, liver and lungs) were fixed in 4% paraformaldehyde for 24 h and then embedded in paraffin. Sections (4 μm) were cut, deparaffinized in Tissue Clear (Sakura, Alphen aan den Rijn, The Netherlands) and hydrated in a descending alcohol series. Subsequently, sections were stained with hematoxylin and eosin to perform morphological analysis of the tissue. Tumor sections were also stained with CD3, CD4, CD31, CD45, CD68, C/EBPβ or MHCII. Antigen retrieval was obtained by heating the sections in Citra Plus Solution (Biogenex, San Ramon, CA, USA) in the microwave for 20 min. After cooling down, sections were washed with PBS and sequentially incubated with 3% hydrogen peroxidase (Merck, Whitehouse Station, NJ, USA) for 30 min at room temperature to block nonspecific binding and with avidin and biotin (CD45; DakoCytomation, Glostrup, Denmark) for 20 min at room temperature or 5% serum for 1 h. To minimize the background signal, sections were also incubated with FC Receptor Blocker (Innovex, Richmond, CA, USA) for 30 min and with Background Buster (Innovex) for 30 min. Then, the slides were incubated with primary antibodies overnight at 4 °C. Positive cells were detected with VectaStain Solution (Vector Laboratories, Burlingame, CA, USA). Briefly, slides were incubated with a biotinylated goat anti-rat or goat anti-mouse antibody for 1 h and then with Vectastain detection system horseradish peroxidase-labeled streptavidin. Antigens were visualized with diaminobenzidine (Innovex). Then, the slides were counterstained with hematoxylin (Vector Laboratories) and mounted with Permount (Dako, Glostrup, Denmark) mounting medium.
Antibodies
The following antibodies were used for immunohistochemical stainings of tissues: rabbit anti-mouse CD3 (1:100; Genetex, Hsinchu City, Taiwan; GTX25690), mouse anti-mouse CD4 (1:100; Abcam, Cambridge, UK; ab51312), rat anti-mouse CD31 (1:100; Dianova, Hamburg, Germany; DIA-310), rat anti-mouse CD45 (1:100; Abcam; ab25386), mouse anti-human C/EBPβ (1:100; Abcam; 18336) and rat anti-mouse MHCII (1:1000; eBioscience, San Diego, CA, USA; 14-5321).
For whole-mount immunohistochemistry, the following antibodies were used: biotinylated anti-mouse CD31 (1:100; BD Biosciences, San Jose, CA, USA; 553371), rabbit anti-mouse NG2 (1:100; Millipore, Billerica, MA, USA; AB5320), streptavidin-phycoerythrin (1:300; BD Biosciences; 554061) and swine anti-rabbit FITC (1:300; Dako; F0054).
Chemokine array
Sh control or sh C/EBPβ cells were seeded on a 24-well plate with 70% confluency. Their medium was changed soon after they adhered and cells were then cultured for 2 days in previously described conditions. Five hundred microliters of cell supernates were collected and centrifuged at 1500 r.p.m. for 5 min. Subsequently, pellets were discarded and supernates were used for chemokine analysis with Mouse Chemokine Array Kit (R&D Systems, Minneapolis, MN, USA; cat. no. ARY020), according to the manufacturer's protocol.
MTT proliferation assay
Sh control or sh C/EBPβ cells were seeded in 96-well plates with a density of 25000 cells per well. Additionally, wells with culture medium without the cells were used as a negative control for the experiment. After 1, 2, 3, 4 and 5 days, plates were analyzed for proliferation with MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl-tetrazolium bromide) assay. MTT solution (5 mg/ml MTT in PBS) was added to each well and incubated for 3.5 h at 37 °C. Then, the media were removed and MTT solvent (4 mM HCl, 0.1% Nonidet P-40 (NP40) in isopropanol) was added. The plate was covered with an aluminum foil, agitated on a shaker for 15 min and then the absorbance was read by a spectrophotometer at 590 nm with a reference filter of 620 nm.
Whole-mount immunohistochemistry
After 24 h fixation, tumors were cut into thin slices and put in PBS for 30 min on a rocking board at room temperature. In same conditions, tissues were digested with proteinase K solution (20 μg/ml) for 5 min, permeabilized in 100% methanol for 30 min, washed with PBS and then blocked with 3% milk in PBST overnight at 4 °C. The next day, tissues were subjected to incubation with primary antibodies diluted in 0.1% milk in PBST (1:100) overnight at 4 °C on a rocking board. Next steps included washing in PBST for 1.5 h, blocking in 3% milk in PBST for 1.5 h and incubation with a mix of secondary antibodies diluted in 0.1% milk in PBST (1:300) for 2 h at 4 °C on a rocking board. Subsequently, the samples were washed in 0.1% milk in PBST for 1 h at room temperature and overnight in PBST at 4 °C on a rocking board. Slides were then mounted and further analyzed by the Leica confocal microscope (Leica Microsystems, Wetzlar, Germany).
Tumor vasculature analysis
Tumors stained with CD31 and NG2 were analyzed with VisioMorph software (Visiopharm). The following factors were calculated according to the fixed protocols: average vessel length, vessel area, number of branch points and pericyte coverage. From each tumor sample, four randomized photos were analyzed.
Statistical analysis
Human studies
Differences in categorical factors were determined with the χ2 test, whereas differences in continuous factors were determined by one-way analysis of variance. For univariate analysis of all factors, Cox proportional hazards models were used. All factors that met the significance criterion (P=0.1) were considered for inclusion in the final model of multivariable analysis. Survival curves were calculated for the various groups using the Kaplan–Meier method and compared by the log-rank test. All values are reported as mean and s.d. or percentages; 95% confidence intervals are provided where appropriate. SPSS Statistic version 22 software (IBM Corporation, Armonk, NY, USA) was used for all analyses.
Animal studies
Differences in obtained values between the groups (sh control vs sh CEBPβ) were assessed with t-test, where P<0.05 was considered statistically significant.
Acknowledgments
This work was supported by grants from National Science Center 2011/01/B/NZ4/06635, Foundation for Polish Science (International PhD Projects cofinanced from European Union, Regional Development Fund), European Union, FP 7, BASTION, Swedish Cancer Society and Karolinska Institute.
Louis Boon is the chief, scientific officer in Bioceros Holding BV. The other authors declare no conflict of interest.
References
- Robinson GW, Johnson PF, Hennighausen L, Sterneck E. The C/EBPbeta transcription factor regulates epithelial cell proliferation and differentiation in the mammary gland. Genes Dev. 1998;12:1907–1916. doi: 10.1101/gad.12.12.1907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seagroves TN, Krnacik S, Raught B, Gay J, Burgess-Beusse B, Darlington GJ, et al. C/EBP beta, but not C/EBP alpha, is essential for ductal morphogenesis, lobuloalveolar proliferation, and functional differentiation in the mouse mammary gland. Genes Dev. 1998;12:1917–1928. doi: 10.1101/gad.12.12.1917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahnow CA. CCAAT/enhancer-binding protein beta: its role in breast cancer and associations with receptor tyrosine kinases. Expert Rev Mol Med. 2009;11:e12. doi: 10.1017/S1462399409001033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson JBT, Kurzejamska E, Pang MF, Jansson M, Roswall P, Pietras K. MiR-155-mediated loss of C/EBPβ shifts the TGF-β response from growth inhibition to epithelial–mesenchymal transition, invasion and metastasis in breast cancer. Oncogene. 2013;32:5614–5624. doi: 10.1038/onc.2013.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homma J, Yamanaka R, Yajima N, Tsuchiya N, Genkai N, Sano M, et al. Increased expression of CCAAT/enhancer binding protein beta correlates with prognosis in glioma patients. Oncol Rep. 2006;15:595–601. [PubMed] [Google Scholar]
- Jundt F, Raetzel N, Muller C, Calkhoven CF, Kley K, Mathas S, et al. A rapamycin derivative (everolimus) controls proliferation through down-regulation of truncated CCAAT enhancer binding protein beta and NF-kappa B activity in Hodgkin and anaplastic large cell lymphomas. Blood. 2005;106:1801–1807. doi: 10.1182/blood-2004-11-4513. [DOI] [PubMed] [Google Scholar]
- Sebastian T, Johnson PF. Stop and go: anti-proliferative and mitogenic functions of the transcription factor C/EBPbeta. Cell Cycle. 2006;5:953–957. doi: 10.4161/cc.5.9.2733. [DOI] [PubMed] [Google Scholar]
- Gomis RR, Alarcon C, Nadal C, Van Poznak C, Massague J. C/EBPbeta at the core of the TGFbeta cytostatic response and its evasion in metastatic breast cancer cells. Cancer Cell. 2006;10:203–214. doi: 10.1016/j.ccr.2006.07.019. [DOI] [PubMed] [Google Scholar]
- Zahnow CA, Cardiff RD, Laucirica R, Medina D, Rosen JM. A role for CCAAT/enhancer binding protein beta-liver-enriched inhibitory protein in mammary epithelial cell proliferation. Cancer Res. 2001;61:261–269. [PubMed] [Google Scholar]
- Milde-Langosch K, Loning T, Bamberger AM. Expression of the CCAAT/enhancer-binding proteins C/EBPalpha, C/EBPbeta and C/EBPdelta in breast cancer: correlations with clinicopathologic parameters and cell-cycle regulatory proteins. Breast Cancer Res Treat. 2003;79:175–185. doi: 10.1023/a:1023929504884. [DOI] [PubMed] [Google Scholar]
- Raught B, Gingras AC, James A, Medina D, Sonenberg N, Rosen JM. Expression of a translationally regulated, dominant-negative CCAAT/enhancer-binding protein beta isoform and up-regulation of the eukaryotic translation initiation factor 2alpha are correlated with neoplastic transformation of mammary epithelial cells. Cancer Res. 1996;56:4382–4386. [PubMed] [Google Scholar]
- Zahnow CA, Younes P, Laucirica R, Rosen JM. Overexpression of C/EBPbeta-LIP, a naturally occurring, dominant-negative transcription factor, in human breast cancer. J Natl Cancer Inst. 1997;89:1887–1891. doi: 10.1093/jnci/89.24.1887. [DOI] [PubMed] [Google Scholar]
- Min Y, Ghose S, Boelte K, Li J, Yang L, Lin PC. C/EBP-delta regulates VEGF-C autocrine signaling in lymphangiogenesis and metastasis of lung cancer through HIF-1alpha. Oncogene. 2011;30:4901–4909. doi: 10.1038/onc.2011.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marigo I, Bosio E, Solito S, Mesa C, Fernandez A, Dolcetti L, et al. Tumor-induced tolerance and immune suppression depend on the C/EBPbeta transcription factor. Immunity. 2010;32:790–802. doi: 10.1016/j.immuni.2010.05.010. [DOI] [PubMed] [Google Scholar]
- Sica A, Bronte V. Altered macrophage differentiation and immune dysfunction in tumor development. J Clin Invest. 2007;117:1155–1166. doi: 10.1172/JCI31422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nat Rev Immunol. 2009;9:162–174. doi: 10.1038/nri2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kusmartsev S, Nagaraj S, Gabrilovich DI. Tumor-associated CD8+ T cell tolerance induced by bone marrow-derived immature myeloid cells. J Immunol. 2005;175:4583–4592. doi: 10.4049/jimmunol.175.7.4583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung K, Hayashi R, Lafond-Walker A, Lowenstein C, Pardoll D, Levitsky H. The central role of CD4(+) T cells in the antitumor immune response. J Exp Med. 1998;188:2357–2368. doi: 10.1084/jem.188.12.2357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dranoff G, Jaffee E, Lazenby A, Golumbek P, Levitsky H, Brose K, et al. Vaccination with irradiated tumor cells engineered to secrete murine granulocyte–macrophage colony-stimulating factor stimulates potent, specific, and long-lasting anti-tumor immunity. Proc Natl Acad Sci USA. 1993;90:3539–3543. doi: 10.1073/pnas.90.8.3539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benevides L, Cardoso CR, Tiezzi DG, Marana HR, Andrade JM, Silva JS. Enrichment of regulatory T cells in invasive breast tumor correlates with the upregulation of IL-17A expression and invasiveness of the tumor. Eur J Immunol. 2013;43:1518–1528. doi: 10.1002/eji.201242951. [DOI] [PubMed] [Google Scholar]
- Wang ZK, Yang B, Liu H, Hu Y, Yang JL, Wu LL, et al. Regulatory T cells increase in breast cancer and in stage IV breast cancer. Cancer Immunol Immunother. 2012;61:911–916. doi: 10.1007/s00262-011-1158-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohling SD, Allison KH. Immunosuppressive regulatory T cells are associated with aggressive breast cancer phenotypes: a potential therapeutic target. Mod Pathol. 2008;21:1527–1532. doi: 10.1038/modpathol.2008.160. [DOI] [PubMed] [Google Scholar]
- Tan W, Zhang WZ, Strasner A, Grivennikov S, Cheng JQ, Hoffman RM, et al. Tumour-infiltrating regulatory T cells stimulate mammary cancer metastasis through RANKL-RANK signalling. Nature. 2011;470:548–553. doi: 10.1038/nature09707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng PKS, Tsui SKW, Lau CPY, Wong CH, Wong WHT, Huang L, et al. CCAAT/enhancer binding protein beta is up-regulated in giant cell tumor of bone and regulates RANKL expression. J Cell Biochem. 2010;110:438–446. doi: 10.1002/jcb.22556. [DOI] [PubMed] [Google Scholar]
- Muller A, Homey B, Soto H, Ge N, Catron D, Buchanan ME, et al. Involvement of chemokine receptors in breast cancer metastasis. Nature. 2001;410:50–56. doi: 10.1038/35065016. [DOI] [PubMed] [Google Scholar]
- Kakinuma T, Hwang ST. Chemokines, chemokine receptors, and cancer metastasis. J Leukoc Biol. 2006;79:639–651. doi: 10.1189/jlb.1105633. [DOI] [PubMed] [Google Scholar]
- Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420:860–867. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshimura T, Howard OM, Ito T, Kuwabara M, Matsukawa A, Chen K, et al. Monocyte chemoattractant protein-1/CCL2 produced by stromal cells promotes lung metastasis of 4T1 murine breast cancer cells. PLoS ONE. 2013;8:e58791. doi: 10.1371/journal.pone.0058791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velasco-Velazquez M, Pestell RG. The CCL5/CCR5 axis promotes metastasis in basal breast cancer. Oncoimmunology. 2013;2:e23660. doi: 10.4161/onci.23660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gery S, Tanosaki S, Bose S, Bose N, Vadgama J, Koeffler HP. Down-regulation and growth inhibitory role of C/EBPalpha in breast cancer. Clin Cancer Res. 2005;11:3184–3190. doi: 10.1158/1078-0432.CCR-04-2625. [DOI] [PubMed] [Google Scholar]
- Yu X, Si J, Zhang Y, Dewille JW. CCAAT/enhancer binding protein-delta (C/EBP-delta) regulates cell growth, migration and differentiation. Cancer Cell Int. 2010;10:48. doi: 10.1186/1475-2867-10-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radomska HS, Basseres DS, Zheng R, Zhang P, Dayaram T, Yamamoto Y, et al. Block of C/EBP alpha function by phosphorylation in acute myeloid leukemia with FLT3 activating mutations. J Exp Med. 2006;203:371–381. doi: 10.1084/jem.20052242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal S, Hofmann WK, Tidow N, Ehrich M, van den Boom D, Koschmieder S, et al. The C/EBP delta tumor suppressor is silenced by hypermethylation in acute myeloid leukemia. Blood. 2007;109:3895–3905. doi: 10.1182/blood-2006-08-040147. [DOI] [PubMed] [Google Scholar]
- Svensson KJ, Christianson HC, Kucharzewska P, Fagerstrom V, Lundstedt L, Borgquist S, et al. Chondroitin sulfate expression predicts poor outcome in breast cancer. Int J Oncol. 2011;39:1421–1428. doi: 10.3892/ijo.2011.1164. [DOI] [PubMed] [Google Scholar]