Abstract
Background
Low levels of moderate-to-vigorous physical activity are associated with adverse health consequences.
Objective
The intent of the study was to determine the feasibility and efficacy of a 12-week physical activity promotion program targeting children, which was delivered to parents through mobile phones.
Methods
Potential participants were recruited through advertisements placed in the newspaper, local hospitals and schools, and an email listserv. Sedentary children aged 6-10 years were randomly assigned to a minimal (MIG) or intensive (IIG) intervention group. Parents in the MIG were given a goal to increase (within 1 month) and maintain their child’s activity at 6000 pedometer steps/day above their baseline levels and to monitor their child’s steps daily. Parents in the IIG were given the same steps/day and monitoring goals, in addition to text messages and articles containing additional behavioral strategies (based on the Social Cognitive Theory) designed to promote their child’s physical activity. The intervention components were delivered via mobile phone. Anthropometrics, body composition, and questionnaires were administered in a clinic. Children wore a New Lifestyles pedometer (NL-1000) each day throughout the intervention and parents were to monitor their child’s step counts daily.
Results
Out of 59 children who screened for the study, a total of 27 children (mean age 8.7, SD 1.4 years; 56%, 15/27 female; 59%, 16/27 African American) were enrolled and completed the study. Overall, 97.90% (2220/2268; 98.20%, 1072/1092 for MIG; 97.60%, 1148/1176 for IIG) of expected step data were successfully entered by the parent or study coordinator. Parents in the MIG and IIG were sent approximately 7 and 13 text messages per week, respectively, averaged over the course of the study. IIG parents accessed an average of 6.1 (SD 4.4) articles over the course of the intervention and accessed a fewer number of articles in the last month compared to the first 2 months of the study (P=.002). Children in both the MIG and IIG significantly increased their physical activity, averaged over 12 weeks, by 1427.6 (SD 583.0; P=.02) and 2832.8 (SD 604.9; P<.001) steps/day above baseline, respectively. The between group difference was not statistically significant (P=.10; effect size=.40), nor was the group by time interaction (P=.57). Regardless of group assignment, children who significantly increased their physical activity reported greater increases in physical activity enjoyment (P=.003). The number of behavioral articles accessed by IIG parents was significantly correlated with change in children’s steps/day (r=.575, P=.04). Changes in children’s steps/day were unrelated to changes in their body composition, mood, and food intake.
Conclusions
Parent-targeted mobile phone interventions are feasible, yet more intense interventions may be needed to support parents’ efforts to increase their children’s physical activity to levels that approximate national recommendations.
Trial Registration
Clinicaltrials.gov NCT01551108; http://clinicaltrials.gov/show/NCT01551108 (Archived by WebCite at http://www.webcitation.org/6TNEOzXNX).
Keywords: mobile health, physical activity intervention, child, parents, pedometers, text messaging
Introduction
Low levels of moderate-to-vigorous physical activity are associated with adverse health consequences. Specifically, epidemiological studies demonstrate that low levels of physical activity are positively associated with childhood obesity [1] . Accumulating evidence suggests that total physical activity levels and time spent in moderate-to-vigorous physical activity are inversely associated with cardiovascular disease (CVD) and diabetes risk factors [2-9]. Therefore, increasing intensity of physical activities or time spent being physically active may have a significant impact on reversing excessive adiposity in children and reducing their risk of developing chronic disease.
Parents have an important role in teaching and encouraging their children to be physically active. For example, cross-sectional and prospective studies provide evidence that parental support and rules, as well as physical activity modeling and co-participation, are positively associated with objectively measured moderate-to-vigorous physical activity levels in children [10]. In addition, favorable parental perceptions of neighborhood safety and reports of frequent family trips to the park are related to parental reports of children’s increased time in free play [11]. Despite these correlational findings, reviews of interventions for children in which physical activity promotion was the main component, or at least one of the intervention components, concluded that family-based interventions have not yet demonstrated strong evidence of effectiveness [12-15]. However, the authors of the reviews noted that many of the family-based interventions have had methodological limitations, including failure to use randomized comparative interventions, high dropout rates, and/or a reliance on self-reported outcome assessments [12-15]. These limitations, coupled with the fact that family-based approaches have shown great success with weight management in children [16-18], suggest that there is a need to improve upon the methods used in family-based interventions targeting physical activity promotion in children.
There has been an increase in the use of mobile phones as an intervention delivery strategy. Mobile phones contain several features appealing to researchers. Mobile phones are portable, which provides the opportunity to collect real-time data [19] and to aid in self-monitoring [20]. Furthermore, participants view text messages as more convenient and effective than other types of communication [21], text messages can be personalized and can augment behavior change strategies [22], and mobile phone-based interventions have been shown to be cost-effective compared to alternative interventions [23]. Several different mobile phone-based interventions have been designed to increase physical activity in children. These interventions were either solely focused on increasing physical activity [24] or offered a physical activity component as part of a larger intervention (eg, weight loss, diabetes management) [25-29]. Importantly, reviews [30-32] have concluded that mobile health interventions can increase physical activity in children, though few mobile phone-based interventions have been conducted. To date, none of these mobile phone studies have delivered the physical activity intervention exclusively to parents. Therefore, interventions delivered through mobile phones promise a novel approach to family-based physical activity promotion.
Few family-based interventions have exclusively targeted children’s physical activity [33-37]. These studies have not consistently produced positive results. Mobile phone-based interventions are promising, yet to the best of our knowledge, no childhood physical activity study has delivered a mobile phone-based intervention exclusively to the child’s parents with the intent of increasing the child’s physical activity. In addition, the clustering of risk factors for CVD develops between 6 and 9 years of age [38], providing an appropriate target age-range for intervention. Therefore, the primary aim of this pilot study, “P-Mobile”, (trial registration NCT01551108) was to determine the feasibility of delivering a physical activity promotion program targeting 6-10 year old children that is delivered to parents through mobile phones. A second aim was to determine whether or not the intervention could elicit objectively determined increases in children’s physical activity.
Methods
Participants
Children who were 6 to 10 years of age, physically capable of exercise, and sedentary were eligible for the study. A parent or legal guardian of each participating child was eligible if they owned a mobile phone with Internet access and text message capabilities. Children were excluded if they were diagnosed with a serious medical disorder (eg, cancer within the last five years, cardiovascular disease). Families were compensated US $200 for their time, mobile phone data use, and travel costs. All study procedures were approved by the Pennington Biomedical Research Center Institutional Review Board.
Procedures
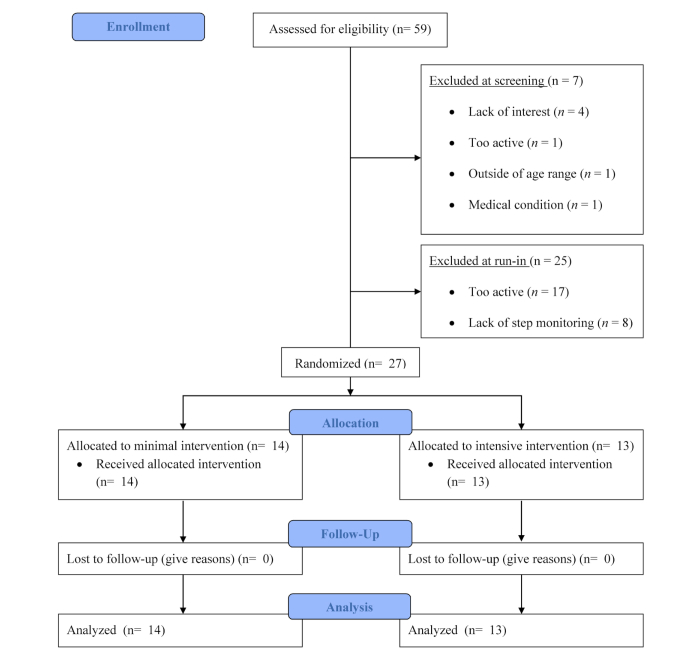
Potential participants were recruited through advertisements placed in the newspaper, posted in local hospitals and schools, and delivered through a Pennington Biomedical Research Center email listserv targeting registered individuals interested in participating in research. Once self-identified, one parent completed an initial telephone screen to determine eligibility for themselves and their child. If the parent-child dyad was eligible following the phone screen, they attended a clinic screening visit at the Pennington Biomedical Research Center (Louisiana). The dyad was oriented to the study and then written informed consent was obtained from the parent and written assent was obtained from the targeted child. The baseline assessment (see Measures below) was then conducted. At the end of the clinic visit, the targeted child was fitted with a pedometer (New Lifestyles 1000/NL-1000), the parent was required to use their mobile phone to respond to a text message sent from the study coordinator, and the parent had to access the study website. The dyad was sent home with the following instructions: the child was to engage in their normal level of activity and the parent was instructed to use their mobile phone to access the study website [39] to record their child’s step count each night after the child laid down to go to bed. This website was formatted for a mobile phone and contained a webpage to enter the date and the child’s step count. Following the clinic visit, the dyad was sent home to begin the 7-day run-in period the following morning. The run-in period was designed to assess the targeted child’s baseline physical activity levels and the parent’s compliance with monitoring the child’s step counts. The dyad was eligible for the study if girls averaged <9500 steps/day or boys averaged <12,500 steps/day (sex-specific cut points indicative of sedentary behavior in children) [40] and parents entered at least 5 days of step counts into the study website across the 7-day run-in period (evidence of ability to comply with data recording requirements). The dyad was not made aware of these eligibility criteria so that they did not alter their behavior in order to qualify for the study. Those dyads meeting eligibility criteria at the end of the run-in period were randomly assigned to either the minimal (MIG) or intensive (IIG) intervention group. Among the 59 dyads showing interest, there were 27 dyads eligible for the study, 14 were randomized into the MIG and 13 into IIG (Figure 1).
Figure 1.
Study flowchart.
Interventions
Overview
This study was a randomized comparative behavioral trial of a minimal versus an intensive intervention delivered to parents via mobile phone with the purpose of increasing physical activity in sedentary children. A block randomization procedure was generated by a study statistician (HH) utilizing SAS software, with a block size of four. The randomization sequence was placed in sealed, numbered envelopes. The clinic coordinator opened the next envelope in the sequence after a participant successfully completed all eligibility criteria. Children in both study groups were instructed to wear a study-provided pedometer every day during the course of the 12-week intervention.
Minimal Intervention Group
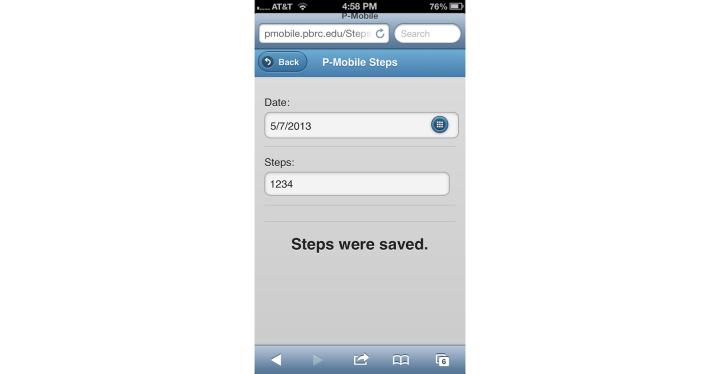
Parents in the MIG were given access to a version of the website (formatted for a mobile phone) in which they could view their child’s daily step goal, monitor their child’s step counts, and receive monthly nutrition tips (Table 1). The website provided parents with a target steps/day goal for their child, which was intended to increase their child’s physical activity by 1000, 3000, and 6000 steps/day above the child’s individualized baseline during the first, third, and fourth week of the intervention, respectively. The additional 6000 steps/day above the baseline level was to be maintained from weeks 4-12. This total increase of 6000 steps/day above baseline was selected to approximate the current national recommendation of 60 minutes of physical activity per day for children [40]. Parents in the MIG were instructed to use their mobile phone to access the study website to record their child’s step count each night after the child laid down to go to bed (Figure 2). Parents in the MIG were also sent monthly healthy nutrition tips via text message targeting the child in order to provide these families with potentially health promoting information.
Table 1.
Components of the minimal (MIG) and intensive (IIG) intervention groups.
| Intervention component | MIG | IIG |
| Access to mobile phone formatted website | X | X |
| 6000 steps/day goal | X | X |
| Daily step monitoring | X | X |
| Monthly nutrition tips | X |
|
| Weekly behavioral articles |
|
X |
| Behavioral text messages |
|
X |
| Steps/day graph |
|
X |
Figure 2.
Mobile phone screenshot showing pedometer step count entry on P-Mobile website.
Intensive Intervention Group
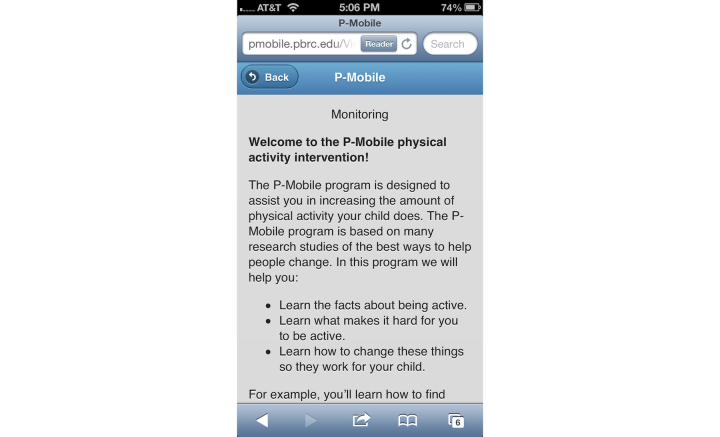
Parents in the IIG were given access to a version of the website in which they could view their child’s daily step goal, monitor their child’s step counts, view a steps/day graph, and read weekly behavioral articles, and they also received text messages. The step monitoring and steps/day website components and goals were identical to the MIG. The steps/day graph was color-coded to illustrate how their child’s daily steps compared to the target step goal: red bars represented days in which the child’s step count was below baseline, yellow represented step counts between baseline and the goal, and green represented step counts at or above the goal (Figure 3). Behavioral strategies based on the Social Cognitive Theory (Table 2) were adapted from previous interventions [41-43] and were delivered through weekly articles posted on the website (Figure 4) and via text messages. The average length of each behavioral article was 621 words. Each text message was ≤160 characters. Text messages were designed to prompt parents to encourage their child’s physical activity (eg, “This is a reminder for your child to be physically active!”), remind parents of behavioral concepts presented in the articles (article tip; eg, “A slip is a time where your child goes several days without reaching their activity goal. Try to stop slips as soon as you can.”), and motivate parents to foster behavioral change in their child (eg, “By engaging in regular physical activity, your child will reduce their risk of gaining weight.”).
Figure 3.
Mobile phone screenshot showing steps/day graph on P-Mobile website.
Table 2.
Behavioral articles provided to parents in the intensive intervention group (IIG).
| Week | Title | Content |
| 1 | Self-monitoring | Parental monitoring of child activity, role of parent in child’s activity, increase steps/day by additional 1000. |
| 2 | Making time for exercise | Goal setting, scheduling time for activity, what is moderate intensity activity, maintain increased step/day of additional 1000. |
| 3 | Increasing activity outdoors | Benefits of outdoor play, role of the parents in child’s physical activity, increase steps/day by additional 2000. |
| 4 | Increasing activity indoors | Cues to activity, changing the home environment, increase steps/day by additional 3000 (achieve ≥ 6000 steps/day above baseline). |
| 5 | Checking-in #1 | Identify barriers to achieving goal. |
| 6 | Problem solving | 5-step problem-solving process. |
| 7 | Rewarding your child | Principles of positive reinforcement, rewards for increased activity. |
| 8 | Reducing sedentary time | Defining and identifying sedentary behavior, ways to reduce sedentary behaviors, substituting physical activity. |
| 9 | Checking-in #2 | Identify barriers to achieving goal. |
| 10 | Lifestyle exercise | Incorporating activity that is part of daily living. |
| 11 | Parental modeling/social support | Parents as a role model for physical activity, obtaining social support from family members. |
| 12 | Relapse prevention | Defining and anticipating slips and relapses, ways to respond to slips. |
Figure 4.
Mobile phone screenshot showing an article on P-Mobile website.
Measures
Overview
All measures, with the exception of the pedometers and the Home and Neighborhood Environment Questionnaire, were assessed at baseline and 12-weeks. The assessment staff was not blinded to the participant assignment.
Pedometer
Children in both groups were asked to wear a NL-1000 pedometer for the duration of the study. The device has a 7-day memory and steps are also digitally displayed on an immediately accessible screen. The NL-1000 contains the same internal mechanism as the NL-2000, which has been previously validated for counting steps in children [44]. Children were instructed to wear the pedometer during all waking hours except during water-based activities.
Anthropometrics
Height and weight were measured with the child dressed in normal street clothes, but without shoes and socks. Height was measured to the nearest 0.1 cm using a wall-mounted stadiometer (Holtain Ltd, Crymych, Dyfed, United Kingdom). Weight was measured to the nearest 0.1 kg using a digital scale (Indiana Scale Company model GSE 450). Waist circumference was measured to the nearest 0.1 cm at the natural waist, with clothing moved out of the way. The circumference was taken twice, with a third measurement taken if the first two were more than 0.5 cm apart. Body mass index (BMI) was calculated by dividing the participant’s average weight in kilograms by the square of their height in meters (kg/m2). BMI was converted to a z-score using gender and age data from the Centers for Disease Control and Prevention, to account for the fact that children of this age are still growing. Blood pressure and pulse were taken after the participant sat quietly for 5 minutes.
Body Composition
The Tanita Body Composition Analyzer (model TBF-240) was used to estimate body fat. The child stood on the scale with bare feet, and impedance data were recorded using a laptop computer. The Tanita has a mean difference of −1.0% with DXA and is considered to be very reliable in children [45].
Questionnaires
Children completed two questionnaires, with the assistance of a study staff member to ensure the child understood all questions. Parents were allowed to be present during the questionnaire administration if the child preferred. The 12-item Physical Activity Enjoyment Questionnaire (PACES) [46] was used to assess the level of a child’s enjoyment of various physical activities. The Child Depression Inventory-Short Form (CDI-S) [47] contains 10 items to assess symptoms of childhood depression and was used to measure self-reported depressed mood.
Parents completed three questionnaires. The Sedentary Behavior Questionnaire was completed to describe the amount of time their child spent watching TV, playing video games, playing on the computer, and doing other sedentary activities. The Home and Neighborhood Environment Questionnaire, adapted from the Neighborhood Impact on Kids study [48,49], assessed parent’s perceptions of their home and neighborhood environment, including safety, availability of destinations, and suitability of the neighborhood for walking and physical activity. The Food Frequency Questionnaire (FFQ) [50] was completed to describe their child’s food intake, including information about macro/micronutrients and food group servings.
Statistical Analysis
Weekly steps/day means analyzed across all 12 weeks of the study were analyzed using a repeated measures analysis of variance. Change in the secondary outcome data (eg, BMI, body composition, questionnaires, website usage, etc) were analyzed using dependent samples t tests. Correlation coefficients were used to assess the relationships between secondary outcome measures and steps/day data. Effect sizes were calculated using Cohen’s d. All statistical analyses were conducted using SAS version 9.3.
Results
Baseline Characteristics
Characteristics of the participating children are summarized in Table 3. A total of 27 children (mean age 8.7, SD 1.4 years; 56%, 15/27, female; 59%, 16/27, African American) successfully completed the run-in period and were randomly assigned to the MIG (n=14) or IIG (n=13). The sample of 27 children had a mean BMI equal to 23.1 (SD 7.7) kg/m2, a mean BMI z-score equal to 1.5 (SD 1.0), a mean BMI percentile of 85.6 (SD 20.2) kg/m2, and mean waist circumference equal to 72.4 (SD 18.1) cm. Participating children across both intervention groups averaged 8621.8 steps/day and the difference in steps/day between the intervention groups was not statistically significant (MIG: 9042.5 vs IIG: 8168.6, P=.25). The only significant difference between intervention groups was percent of reported calories consumed from protein (MIG: 16.7% vs IIG: 19.1%; P=.047).
Table 3.
Baseline demographic characteristics for all children.
| Characteristic | All children (N=27) |
Minimal intervention (n=14) |
Intensive intervention (n=13) |
| n (%) or mean (SD) | n (%) or mean (SD) | n (%) or mean (SD) | |
| Age (years) | 8.7 (1.4) | 9.1 (1.3) | 8.3 (1.5) |
| Gender (% female) | 15/27 (56%) | 7/14 (50%) | 8/13 (62%) |
| Ethnicity (% African American) | 16/27 (59%) | 8/14 (57%) | 8/13 (62%) |
| Height (cm) | 138.1 (10.7) | 140.0 (8.3) | 135.9 (12.9) |
| Weight (kg) | 45.5 (19.7) | 44.5 (18.3) | 46.5 (21.9) |
| BMIa (kg/m2) | 23.1 (7.7) | 22.3 (7.4) | 24.1 (8.1) |
| BMI z-score | 1.5 (1.0) | 1.3 (0.9) | 1.7 (1.0) |
| BMI percentile | 85.6 (20.2) | 83.7 (21.0) | 87.6 (20.1) |
| Waist circumference (cm) | 72.4 (18.1) | 70.5 (17.0) | 74.5 (19.7) |
| Body fat percent | 31.1 (11.2) | 29.0 (10.3) | 33.4 (12.1) |
| CDI-Sa | 47.1 (9.2) | 47.3 (8.9) | 46.8 (9.9) |
| Physical activity enjoyment | 66.6 (7.0) | 67.5 (7.9) | 65.6 (6.2) |
| Sedentary time (weekday hours) | 5.1 (4.0) | 4.9 (4.1) | 5.4 (3.9) |
| Sedentary time (weekend hours) | 8.3 (5.4) | 8.2 (5.0) | 8.4 (5.9) |
| TV in room | 16/27 (59%) yes | 5/14 (36%) yes | 11/13 (85%) yes |
| Total calorie consumption | 1587.1 (647.5) | 1520.6 (628.7) | 1658.7 (685.1) |
| Steps/day | 8621.8 (1955.0) | 9042.5 (1930.5) | 8168.6 (1953.2) |
aBMI: body mass index
bCDI-S: Child Depression Inventory-Short Form
Website Data
Parents across both groups logged into the website an average of 76.7 (SD 20.1) times over the course of the study (6.3 times/week). Parents were instructed to enter their child’s step counts daily, and parents in the MIG and IIG, respectively, entered 44.20% (520/1176) and 62.80% (686/1092) of their child’s step counts daily as instructed. Parents could also enter step count data for up to 7 days past the date the activity occurred. Another 40.60% (478/1176) and 27.00% (295/1092) of data was entered on a subsequent day for a total of 84.80% (997/1176) and 89.80% (981/1092) of step counts being entered by the parents in the MIG and IIG, respectively. The remaining 13.40% (158/1176; MIG) and 7.80% (85/1092; IIG) of the data were entered by the study coordinator because either the parents sent this information to the coordinator (via text message) or because the study coordinator contacted the parents (via phone) to retrieve missing data when identified. Overall, 97.90% (2220/2268; 98.20%, 1155/1176 for MIG; 97.60%, 1066/1092 for IIG) of expected step data were successfully entered by the parent or study coordinator.
Figure 5 shows the number of parents in the IIG who accessed each of the weekly behavioral articles. Approximately 38% (10/27) of the parents accessed 9 or more articles, 23% (6/27) accessed between 4 and 8, and 38% (10/27) accessed less than 4 articles, with two parents never accessing an article. Overall, IIG parents accessed 70% (8/12) of the articles in Month 1, 60% (7/12) in Month 2, and 37.5% (5/12) in Month 3. Article accessing decreased significantly over the course of the study (P=.002).
Figure 5.
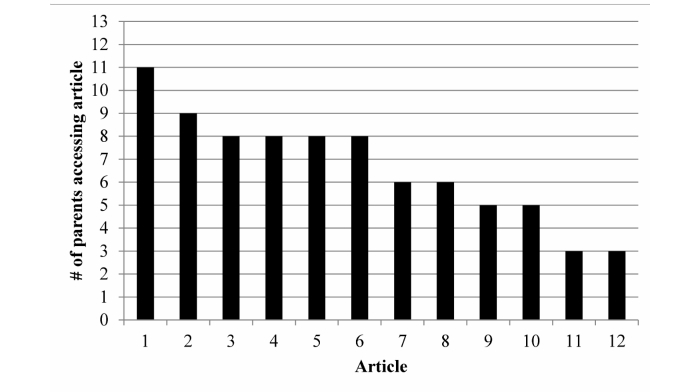
Number of parents in the Intensive Intervention Group (n=13) who accessed each of the 12 articles.
Parents in the IIG visited the steps/day graph an average of 25.3 (SD 24.5) times over the course of the study (2.1 times/week). There was a clear dichotomy in access, with six participants accessing the graph fewer than 8 times, and seven accessing the graph more than 21 times.
Text Messages
Parents in the MIG were sent 1-2 text messages and parents in the IIG were sent 7-8 text messages per week during the first 6 months of the study. However, daily text message reminders were implemented after the first four participants completed the study in an attempt to increase compliance with parent monitoring of the child’s daily steps. Therefore, parents in the MIG and IIG were sent approximately 7 and 13 text messages per week, respectively, averaged over the course of the study.
Parents in the MIG sent 162 (0.96/week) and parents in the IIG sent 419 (2.7/week) text messages over the course of the study. Approximately half of the text messages sent by parents in both groups were communications with the study coordinator regarding missing step data. The other text messages sent by the parents were related to equipment/resource issues (eg, pedometer, website), requests for further information (eg, spontaneous questions, scheduling), or responses to a text message they had received.
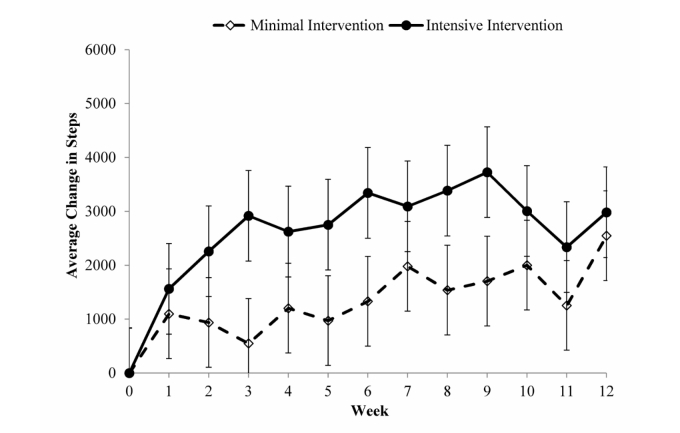
Step Counts
All randomized children attended the Week 12 visit and thus completed the 12-week study. Figure 6 graphically illustrates the weekly changes in steps/day for the two intervention groups. Children in the MIG and IIG both demonstrated significant increases across the 12 weeks by 1427.6 (SD 583.0; P=.02) and 2832.8 (SD 604.9) steps/day (P<.001) above baseline, respectively. The between-group difference was not statistically significant (P=.10) yet the effect size was d=.40. The group by time interaction was not significant (P=.57).
Figure 6.
Average change in child’s steps per week by intervention group.
Secondary Analyses
Table 4 shows that none of the changes in body composition variables, including BMI, BMI z, waist circumference, body fat percent, and fat free mass were significant (all P values >.22). Further, there were no significant within or between-group differences in the parent proxy-reported measures, including sedentary behavior and food intake, or child self-reported physical activity enjoyment, and depressive symptoms (all P values >.38). Therefore, the data from the groups were combined to assess the relationship between the change in these secondary outcome measures and change in steps/day. The correlation between change in physical activity enjoyment and change in steps/day was statistically significant (r=.469; P=.003). For participants in the IIG, a significant correlation (r=.575, P=.04) was observed between the number of articles accessed by the parent and average change in their child’s steps/day.
Table 4.
Change in outcome variables from baseline to 12 weeks.
|
|
Minimal intervention | Intensive intervention | P value (between group differences) |
|
|
mean (SD) | mean (SD) | |
| Height (cm) | 1.5 (1.0) | 1.6 (1.1) | .843 |
| Weight (kg) | 0.94 (2.1) | 1.4 (1.7) | .536 |
| BMIa (kg/m2) | −0.86 (1.1) | 0.28 (1.0) | .369 |
| BMI z-score | 0.016 (0.19) | 0.00 (0.14) | .773 |
| BMI percentile | 1.01 (6.1) | 0.27 (1.9) | .455 |
| Waist circumference (cm) | 0.85 (4.0) | 1.3 (2.8) | .764 |
| Body fat percent | −0.24 (1.9) | 0.69 (2.4) | .275 |
| CDI-Sb | −1.1 (4.0) | −3.4 (8.4) | .378 |
| Physical activity enjoyment | −0.09 (0.17) | −0.01 (0.29) | .391 |
| Sedentary time (weekday hours) | 0.0 (3.2) | −0.59 (3.9) | .617 |
| Sedentary time (weekend hours) | −1.2 (4.0) | −1.1 (5.5) | .941 |
| Total calorie consumption | 96.2 (682.4) | −310.6 (569.1) | .200 |
| % calories from fat | −1.8 (6.7) | −0.06 (7.2) | .483 |
| % calories from protein | 0.78 (2.6) | 0.59 (2.3) | .976 |
| % calories from carb | 1.0 (5.7) | −0.37 (7.2) | .323 |
| Steps/dayc, mean (SE) | 1427.6 (583.0) | 2832.8 (604.9) | .102 |
aBMI: body mass index
bCDI-S: Child Depression Inventory-Short Form
cRepresents the average change in weekly steps/day across 12 weeks
Discussion
Principal Results
The P-Mobile study demonstrated that it is feasible to deliver a child-targeted physical activity promotion program to parents through their mobile phones. Feasibility was demonstrated by parental utilization of the components of the intervention, including entering their child’s step counts, responding to text messages, and accessing the behavioral articles. The intervention also resulted in increased physical activity in both study groups. Step counts increased significantly in both the MIG and the IIG over the course of the 12-week intervention. These findings suggest that mobile phone-based physical activity promotion interventions delivered to parents have the potential to be utilized and may positively affect physical activity levels in children.
Parental use of the intervention components varied by the component assessed. Concerning step count data, only half of the parents complied with the study requirement to enter step counts each night. This required the study coordinator to prompt parents for about half of the data and enter 10%-15% of the data. Therefore, the large volume of step data entered was the result of combined efforts by both the parents and the study coordinator, which may be difficult for participants and burdensome on study staff to sustain over a period longer than 12 weeks. Bluetooth capable activity monitors (eg, FitBits, Jawbone, Garmin Vivofit, etc) may lessen this burden and increase compliance. Concerning text messages, on average, parents in the IIG received approximately 13 automated text messages per week. This level appears to be tolerable because only one parent (4%, 1/27) requested a decrease in the frequency of text messages. Parents sent between 1 and 3 text messages per week to the study coordinator, but this was largely related to obtaining missing step data. Text messaging appears to be an acceptable form of communication, but it did not appear to be utilized by parents to increase their child’s physical activity levels. Concerning articles, accessing article content was positively associated with change in steps/day for families in the IIG. However, accessing article content decreased significantly over the course of the study. This finding is consistent with Internet-based studies reporting incrementally reduced usage of websites across the study duration [51,52] and suggests that this type of intervention may not be ideally suited for all parents. In sum, although the components of the intervention were utilized, they were not utilized as anticipated. Based on our results, future studies should find ways to maintain consistent engagement of participants in mobile phone-based interventions because performance is positively associated with engagement.
The P-Mobile study demonstrated that children in both the MIG and IIG significantly increased steps/day above baseline levels. The intervention where parents received additional behavioral strategies and text messages (IIG) resulted in steps/day increases that were two-fold greater than steps/day levels reported with only daily monitoring and goal setting (MIG). Though this difference was not statistically significant, suggestion of a moderate treatment effect was observed. However, the children in P-Mobile were unable to achieve the study goal (increasing 6000 steps/day above individualized baseline levels) directed to their parents. Children in the MIG were able to reach approximately 24%, while children in the IIG were able to reach approximately 50% of this goal. A 6000 steps/day increase from baseline levels would have amounted to ~13,500 steps/day for girls and ~16,000 steps/day for boys. Surveillance studies of free-living behavior demonstrate that only 25% of girls and 15% of boys aged 6-10 years achieve this level of habitual daily physical activity [53]. Therefore, the goals promoted herein were achievable, but require intervention support for those not habitually inclined toward a physically active lifestyle. Given the results of the current study combined with those of previous investigations, it suggests that interventions need to be further strengthened in order for sedentary children to achieve this level of activity. Interventions can potentially be further strengthened by engaging both parents (eg, providing behavior strategies to both parents, encouraging both parents to exercise with their child), incorporating siblings into the intervention (eg, delivering the intervention to all children in the family), and/or gathering real-time data (eg, through ecological momentary assessment) to better understand the physical activity patterns to determine optimal times/ways to incorporate physical activity in each individual child’s life [54]. A potential downside to such strengthening efforts is the possible increase in staff and participant burden, and the potential for increased non-compliance due to the more intense strategies and requirements. Further research will help illuminate the optimal approach to using this technology to promote children’s physical activity by targeting parents. For example, a multiphase optimization strategy [55,56] can be used to develop the ideal approach from the many intervention components (eg, pedometers, text messages, lesson plans, etc) of P-Mobile.
Comparison to Prior Work
Family-based studies that have used pedometers to increase physical activity in children have typically delivered the intervention through group sessions [57-60]. A consistent finding across these interventions is that they realize increases in children’s physical activity [15], anywhere from ~1500 [59,60] to ~3000 [57] steps/day above baseline levels. One study showed a significant differential increase of ~1000 steps between the intervention and control groups [58]. In two studies that utilized mobile phones to deliver behavioral change strategies and pedometers as monitoring tools to increase physical activity in children [24,29], neither resulted in significant within or between-group differences in steps/day. P-Mobile showed increases in physical activity for children in both groups (~1400 to ~2800 steps/day) and resulted in differences between groups (~1400 steps/day) that are within the range of values of similar family-based interventions that delivered the intervention through face-to-face contact. To our knowledge, P-Mobile is the only mobile phone-delivered physical activity intervention in children that has resulted in significant within group increases in steps/day. Therefore, it appears that mobile phone interventions can be delivered to parents and result in increases in physical activity in their children. Our findings are in need of replication with larger samples, over longer durations, and with more diverse populations.
Limitations
The P-Mobile findings should be interpreted within the context of the study’s limitations. One major limitation was the small sample size. This may have provided insufficient power for detecting statistical significance between the observed group differences. The study had 17% power to detect differences and would have needed a sample size of 105 children/group to detect a 1400 steps/day difference. In addition, the study was limited to only 12 weeks; therefore, the long-term effectiveness of the study is unknown. The mobile phone components utilized in this study were limited to text messages and accessing a website through the mobile phone. Smartphones offer increased functionality, such as specially designed apps that could have fostered automated uploading of step data, thereby reducing participant burden and potentially increasing utilization. Apps also allow for location-based services that can be used to assist participants in identifying nearby facilities conducive for physical activity. Concerning measurement, although we used an objective measure of activity, pedometers do not capture all activity such as biking and swimming, and dietary intake was assessed using the FFQ, which is known to provide biased estimates compared to gold standard techniques, such as doubly labeled water. Finally, P-Mobile did not contain a control group. Our comparison group, the MIG, increased their average steps/day across the study, while control groups in previous studies have not significantly increased steps/day or have resulted in decreased steps/day [61,62].
Conclusions
P-Mobile was able to demonstrate that it is both feasible and effective to deliver a physical activity promotion program utilizing mobile phones. The study also showed that parents can be the exclusive targets and thus agents of their children’s behavior change. Our findings add to the literature indicating that pedometers can be used to help increase physical activity in children. Our program relied on text messages, a website, involved few families, and was of a moderate duration. Researchers can build upon this foundation to develop more effective mobile phone-based interventions targeting childhood physical activity.
Acknowledgments
RLNJr was supported by unrestricted funds from the Coca Cola Foundation. RM and WDJ were supported in part by 1 U54 GM104940 from the National Institute of General Medical Sciences of the National Institutes of Health, which funds the Louisiana Clinical and Translational Science Center.
Abbreviations
- BMI
body mass index
- CDI-S
Child Depression Inventory-Short Form
- CVD
cardiovascular disease
- FFQ
Food Frequency Questionnaire
- IIG
intensive intervention group
- MIG
minimal intervention group
- NL-1000
New Lifestyles 1000 pedometer
- PACES
Physical Activity Enjoyment Questionnaire
- P-Mobile
Parent-Targeted Mobile Phone Intervention to Increase Physical Activity in Sedentary Children
- TBF
Tanita Body Composition Analyzer
Footnotes
Authors' Contributions: RLNJr conceived and designed the study, interpreted the data, drafted, and critically revised the manuscript. AMM, HRA, and JMSJr acquired and interpreted the data, and critically revised the manuscript. RM, HH, and WDJ conducted the statistical analyses and critically revised the manuscript. STB and CT-L designed the study, interpreted the data, and critically revised the manuscript. TSC conceived the study, interpreted the data, and critically revised the manuscript. All authors provided final approval.
Conflicts of Interest: HRA, a co-author, developed the software that was utilized in the study.
References
- 1.Trinh A, Campbell M, Ukoumunne OC, Gerner B, Wake M. Physical activity and 3-year BMI change in overweight and obese children. Pediatrics. 2013 Feb;131(2):e470–7. doi: 10.1542/peds.2012-1092. http://pediatrics.aappublications.org/cgi/pmidlookup?view=long&pmid=23319527. [DOI] [PubMed] [Google Scholar]
- 2.Giussani M, Antolini L, Brambilla P, Pagani M, Zuccotti G, Valsecchi MG, Lucini D, Genovesi S. Cardiovascular risk assessment in children: role of physical activity, family history and parental smoking on BMI and blood pressure. J Hypertens. 2013 May;31(5):983–92. doi: 10.1097/HJH.0b013e32835f17c7. [DOI] [PubMed] [Google Scholar]
- 3.Hay J, Maximova K, Durksen A, Carson V, Rinaldi RL, Torrance B, Ball GD, Majumdar SR, Plotnikoff RC, Veugelers P, Boulé NG, Wozny P, McCargar L, Downs S, Lewanczuk R, McGavock J. Physical activity intensity and cardiometabolic risk in youth. Arch Pediatr Adolesc Med. 2012 Nov;166(11):1022–9. doi: 10.1001/archpediatrics.2012.1028. [DOI] [PubMed] [Google Scholar]
- 4.Henderson M, Gray-Donald K, Rabasa-Lhoret R, Bastard JP, Barnett TA, Benedetti A, Chaput JP, Tremblay A, Lambert M. Insulin secretion and its association with physical activity, fitness and screen time in children. Obesity (Silver Spring) 2014 Feb;22(2):504–11. doi: 10.1002/oby.20619. [DOI] [PubMed] [Google Scholar]
- 5.Chaput JP, Saunders TJ, Mathieu MÈ, Henderson M, Tremblay MS, O'Loughlin J, Tremblay A. Combined associations between moderate to vigorous physical activity and sedentary behaviour with cardiometabolic risk factors in children. Appl Physiol Nutr Metab. 2013 May;38(5):477–83. doi: 10.1139/apnm-2012-0382. [DOI] [PubMed] [Google Scholar]
- 6.Sääkslahti A, Numminen P, Varstala V, Helenius H, Tammi A, Viikari J, Välimäki I. Physical activity as a preventive measure for coronary heart disease risk factors in early childhood. Scand J Med Sci Sports. 2004 Jun;14(3):143–9. doi: 10.1111/j.1600-0838.2004.00347.x. [DOI] [PubMed] [Google Scholar]
- 7.Ekelund U, Griffin SJ, Wareham NJ. Physical activity and metabolic risk in individuals with a family history of type 2 diabetes. Diabetes Care. 2007 Feb;30(2):337–42. doi: 10.2337/dc06-1883. [DOI] [PubMed] [Google Scholar]
- 8.Jiménez-Pavón D, Konstabel K, Bergman P, Ahrens W, Pohlabeln H, Hadjigeorgiou C, Siani A, Iacoviello L, Molnár D, De Henauw S, Pitsiladis Y, Moreno LA, IDEFICS consortium Physical activity and clustered cardiovascular disease risk factors in young children: a cross-sectional study (the IDEFICS study) BMC Med. 2013 Jul;11:172. doi: 10.1186/1741-7015-11-172. http://www.biomedcentral.com/1741-7015/11/172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jago R, Wedderkopp N, Kristensen PL, Møller NC, Andersen LB, Cooper AR, Froberg K. Six-year change in youth physical activity and effect on fasting insulin and HOMA-IR. Am J Prev Med. 2008 Dec;35(6):554–60. doi: 10.1016/j.amepre.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 10.Maitland C, Stratton G, Foster S, Braham R, Rosenberg M. A place for play? The influence of the home physical environment on children's physical activity and sedentary behaviour. Int J Behav Nutr Phys Act. 2013 Aug;10:99. doi: 10.1186/1479-5868-10-99. http://www.ijbnpa.org/content/10//99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tappe KA, Glanz K, Sallis JF, Zhou C, Saelens BE. Children's physical activity and parents' perception of the neighborhood environment: neighborhood impact on kids study. Int J Behav Nutr Phys Act. 2013 Mar;10:39. doi: 10.1186/1479-5868-10-39. http://www.ijbnpa.org/content/10//39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van Sluijs EM, McMinn AM, Griffin SJ. Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. BMJ. 2007 Oct 6;335(7622):703. doi: 10.1136/bmj.39320.843947.BE. http://www.bmj.com/cgi/pmidlookup?view=long&pmid=17884863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Sluijs EM, Kriemler S, McMinn AM. The effect of community and family interventions on young people's physical activity levels: a review of reviews and updated systematic review. Br J Sports Med. 2011 Sep;45(11):914–22. doi: 10.1136/bjsports-2011-090187. http://europepmc.org/abstract/MED/21836175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O'Connor TM, Jago R, Baranowski T. Engaging parents to increase youth physical activity: a systematic review. Am J Prev Med. 2009 Aug;37(2):141–9. doi: 10.1016/j.amepre.2009.04.020. [DOI] [PubMed] [Google Scholar]
- 15.Lubans DR, Morgan PJ, Tudor-Locke C. A systematic review of studies using pedometers to promote physical activity among youth. Prev Med. 2009 Apr;48(4):307–15. doi: 10.1016/j.ypmed.2009.02.014. [DOI] [PubMed] [Google Scholar]
- 16.Sung-Chan P, Sung YW, Zhao X, Brownson RC. Family-based models for childhood-obesity intervention: a systematic review of randomized controlled trials. Obes Rev. 2013 Apr;14(4):265–78. doi: 10.1111/obr.12000. [DOI] [PubMed] [Google Scholar]
- 17.Golan M, Crow S. Parents are key players in the prevention and treatment of weight-related problems. Nutr Rev. 2004 Jan;62(1):39–50. doi: 10.1111/j.1753-4887.2004.tb00005.x. [DOI] [PubMed] [Google Scholar]
- 18.Epstein LH, Valoski A, Wing RR, McCurley J. Ten-year outcomes of behavioral family-based treatment for childhood obesity. Health Psychol. 1994 Sep;13(5):373–83. doi: 10.1037//0278-6133.13.5.373. [DOI] [PubMed] [Google Scholar]
- 19.Tate EB, Spruijt-Metz D, O'Reilly G, Jordan-Marsh M, Gotsis M, Pentz MA, Dunton GF. mHealth approaches to child obesity prevention: successes, unique challenges, and next directions. Transl Behav Med. 2013 Dec;3(4):406–15. doi: 10.1007/s13142-013-0222-3. http://europepmc.org/abstract/MED/24294329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol Rev. 2010 Apr;32(1):56–69. doi: 10.1093/epirev/mxq004. http://europepmc.org/abstract/MED/20354039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sharifi M, Dryden EM, Horan CM, Price S, Marshall R, Hacker K, Finkelstein JA, Taveras EM. Leveraging text messaging and mobile technology to support pediatric obesity-related behavior change: a qualitative study using parent focus groups and interviews. J Med Internet Res. 2013 Dec;15(12):e272. doi: 10.2196/jmir.2780. http://www.jmir.org/2013/12/e272/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Burner ER, Menchine MD, Kubicek K, Robles M, Arora S. Perceptions of successful cues to action and opportunities to augment behavioral triggers in diabetes self-management: qualitative analysis of a mobile intervention for low-income Latinos with diabetes. J Med Internet Res. 2014 Jan;16(1):e25. doi: 10.2196/jmir.2881. http://www.jmir.org/2014/1/e25/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guerriero C, Cairns J, Roberts I, Rodgers A, Whittaker R, Free C. The cost-effectiveness of smoking cessation support delivered by mobile phone text messaging: Txt2stop. Eur J Health Econ. 2013 Oct;14(5):789–97. doi: 10.1007/s10198-012-0424-5. http://europepmc.org/abstract/MED/22961230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Newton KH, Wiltshire EJ, Elley CR. Pedometers and text messaging to increase physical activity: randomized controlled trial of adolescents with type 1 diabetes. Diabetes Care. 2009 May;32(5):813–5. doi: 10.2337/dc08-1974. http://europepmc.org/abstract/MED/19228863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Franklin VL, Waller A, Pagliari C, Greene SA. A randomized controlled trial of Sweet Talk, a text-messaging system to support young people with diabetes. Diabet Med. 2006 Dec;23(12):1332–8. doi: 10.1111/j.1464-5491.2006.01989.x. [DOI] [PubMed] [Google Scholar]
- 26.Frøisland DH, Arsand E, Skårderud F. Improving diabetes care for young people with type 1 diabetes through visual learning on mobile phones: mixed-methods study. J Med Internet Res. 2012 Aug;14(4):e111. doi: 10.2196/jmir.2155. http://www.jmir.org/2012/4/e111/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Woolford SJ, Khan S, Barr KL, Clark SJ, Strecher VJ, Resnicow K. A picture may be worth a thousand texts: obese adolescents' perspectives on a modified photovoice activity to aid weight loss. Child Obes. 2012 Jun;8(3):230–6. doi: 10.1089/chi.2011.0095. http://europepmc.org/abstract/MED/22799549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de Niet J, Timman R, Bauer S, van den Akker E, Buijks H, de Klerk C, Kordy H, Passchier J. The effect of a short message service maintenance treatment on body mass index and psychological well-being in overweight and obese children: a randomized controlled trial. Pediatr Obes. 2012 Jun;7(3):205–19. doi: 10.1111/j.2047-6310.2012.00048.x. [DOI] [PubMed] [Google Scholar]
- 29.Shapiro JR, Bauer S, Hamer RM, Kordy H, Ward D, Bulik CM. Use of text messaging for monitoring sugar-sweetened beverages, physical activity, and screen time in children: a pilot study. J Nutr Educ Behav. 2008 Nov-Dec;40(6):385–91. doi: 10.1016/j.jneb.2007.09.014. http://europepmc.org/abstract/MED/18984496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lau PW, Lau EY, Wong del P, Ransdell L. A systematic review of information and communication technology-based interventions for promoting physical activity behavior change in children and adolescents. J Med Internet Res. 2011 Jul;13(3):e48. doi: 10.2196/jmir.1533. http://www.jmir.org/2011/3/e48/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fanning J, Mullen SP, McAuley E. Increasing physical activity with mobile devices: a meta-analysis. J Med Internet Res. 2012 Nov;14(6):e161. doi: 10.2196/jmir.2171. http://www.jmir.org/2012/6/e161/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bort-Roig J, Gilson ND, Puig-Ribera A, Contreras RS, Trost SG. Measuring and influencing physical activity with smartphone technology: a systematic review. Sports Med. 2014 May;44(5):671–86. doi: 10.1007/s40279-014-0142-5. [DOI] [PubMed] [Google Scholar]
- 33.Baranowski T, Simons-Morton B, Hooks P, Henske J, Tiernan K, Dunn JK, Burkhalter H, Harper J, Palmer J. A center-based program for exercise change among black-American families. Health Educ Q. 1990;17(2):179–96. doi: 10.1177/109019819001700205. [DOI] [PubMed] [Google Scholar]
- 34.Ransdell LB, Dratt J, Kennedy C, O'Neill S, DeVoe D. Daughters and mothers exercising together (DAMET): a 12-week pilot project designed to improve physical self-perception and increase recreational physical activity. Women Health. 2001;33(3-4):101–16. [PubMed] [Google Scholar]
- 35.Ransdell LB, Robertson L, Ornes L, Moyer-Mileur L. Generations Exercising Together to Improve Fitness (GET FIT): a pilot study designed to increase physical activity and improve health-related fitness in three generations of women. Women Health. 2004;40(3):77–94. doi: 10.1300/j013v40n03_06. [DOI] [PubMed] [Google Scholar]
- 36.Ransdell LB, Taylor A, Oakland D, Schmidt J, Moyer-Mileur L, Shultz B. Daughters and mothers exercising together: effects of home- and community-based programs. Med Sci Sports Exerc. 2003 Feb;35(2):286–96. doi: 10.1249/01.MSS.0000048836.67270.1F. [DOI] [PubMed] [Google Scholar]
- 37.Rhodes RE, Naylor PJ, McKay HA. Pilot study of a family physical activity planning intervention among parents and their children. J Behav Med. 2010 Apr;33(2):91–100. doi: 10.1007/s10865-009-9237-0. [DOI] [PubMed] [Google Scholar]
- 38.Andersen LB, Bugge A, Dencker M, Eiberg S, El-Naaman B. The association between physical activity, physical fitness and development of metabolic disorders. Int J Pediatr Obes. 2011 Sep;6 Suppl 1:29–34. doi: 10.3109/17477166.2011.606816. [DOI] [PubMed] [Google Scholar]
- 39.P-Mobile Intervention. [2014-10-17]. http://pmobile.pbrc.edu/
- 40.Tudor-Locke C, Hatano Y, Pangrazi RP, Kang M. Revisiting "how many steps are enough?". Med Sci Sports Exerc. 2008 Jul;40(7 Suppl):S537–43. doi: 10.1249/MSS.0b013e31817c7133. [DOI] [PubMed] [Google Scholar]
- 41.Newton RL Jr, Han H, Anton SD, Martin CK, Stewart TM, Lewis L, Champagne CM, Sothern M, Ryan D, Williamson DA. An environmental intervention to prevent excess weight gain in African-American students: a pilot study. Am J Health Promot. 2010 May-Jun;24(5):340–3. doi: 10.4278/ajhp.08031224. http://europepmc.org/abstract/MED/20465148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Williamson DA, Champagne CM, Harsha DW, Han H, Martin CK, Newton RL Jr, Sothern MS, Stewart TM, Webber LS, Ryan DH. Effect of an environmental school-based obesity prevention program on changes in body fat and body weight: a randomized trial. Obesity (Silver Spring) 2012 Aug;20(8):1653–61. doi: 10.1038/oby.2012.60. http://europepmc.org/abstract/MED/22402733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Williamson DA, Copeland AL, Anton SD, Champagne C, Han H, Lewis L, Martin C, Newton RL, Sothern M, Stewart T, Ryan D. Wise Mind project: a school-based environmental approach for preventing weight gain in children. Obesity (Silver Spring) 2007 Apr;15(4):906–17. doi: 10.1038/oby.2007.597. [DOI] [PubMed] [Google Scholar]
- 44.Duncan JS, Schofield G, Duncan EK, Hinckson EA. Effects of age, walking speed, and body composition on pedometer accuracy in children. Res Q Exerc Sport. 2007 Dec;78(5):420–8. doi: 10.1080/02701367.2007.10599442. [DOI] [PubMed] [Google Scholar]
- 45.Barreira TV, Staiano AE, Katzmarzyk PT. Validity assessment of a portable bioimpedance scale to estimate body fat percentage in white and African-American children and adolescents. Pediatr Obes. 2013 Apr;8(2):e29–32. doi: 10.1111/j.2047-6310.2012.00122.x. http://europepmc.org/abstract/MED/23239610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Moore JB, Yin Z, Hanes J, Duda J, Gutin B, Barbeau P. Measuring enjoyment of physical activity in children: validation of the Physical Activity Enjoyment Scale. J Appl Sport Psychol. 2009 Jan 1;21(S1):S116–S129. doi: 10.1080/10413200802593612. http://europepmc.org/abstract/MED/20209028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kovacs M. Children's Depression Inventory (CDI): The Technical Manual. North Tonawada, NY: Multi-Health Systems; 2001. [Google Scholar]
- 48.Saelens BE, Sallis JF, Frank LD, Couch SC, Zhou C, Colburn T, Cain KL, Chapman J, Glanz K. Obesogenic neighborhood environments, child and parent obesity: the Neighborhood Impact on Kids study. Am J Prev Med. 2012 May;42(5):e57–64. doi: 10.1016/j.amepre.2012.02.008. http://europepmc.org/abstract/MED/22516504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Katzmarzyk PT, Barreira TV, Broyles ST, Champagne CM, Chaput JP, Fogelholm M, Hu G, Johnson WD, Kuriyan R, Kurpad A, Lambert EV, Maher C, Maia J, Matsudo V, Olds T, Onywera V, Sarmiento OL, Standage M, Tremblay MS, Tudor-Locke C, Zhao P, Church TS. The International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE): design and methods. BMC Public Health. 2013 Sep;13:900. doi: 10.1186/1471-2458-13-900. http://www.biomedcentral.com/1471-2458/13/900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Block G, Woods M, Potosky A, Clifford C. Validation of a self-administered diet history questionnaire using multiple diet records. J Clin Epidemiol. 1990;43(12):1327–35. doi: 10.1016/0895-4356(90)90099-b. [DOI] [PubMed] [Google Scholar]
- 51.Arem H, Irwin M. A review of web-based weight loss interventions in adults. Obes Rev. 2011 May;12(5):e236–43. doi: 10.1111/j.1467-789X.2010.00787.x. http://europepmc.org/abstract/MED/20804523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vandelanotte C, Spathonis KM, Eakin EG, Owen N. Website-delivered physical activity interventions a review of the literature. Am J Prev Med. 2007 Jul;33(1):54–64. doi: 10.1016/j.amepre.2007.02.041. [DOI] [PubMed] [Google Scholar]
- 53.Craig CL, Cameron C, Tudor-Locke C. CANPLAY pedometer normative reference data for 21,271 children and 12,956 adolescents. Med Sci Sports Exerc. 2013 Jan;45(1):123–9. doi: 10.1249/MSS.0b013e31826a0f3a. [DOI] [PubMed] [Google Scholar]
- 54.Dunton GF, Liao Y, Intille SS, Spruijt-Metz D, Pentz M. Investigating children's physical activity and sedentary behavior using ecological momentary assessment with mobile phones. Obesity (Silver Spring) 2011 Jun;19(6):1205–12. doi: 10.1038/oby.2010.302. [DOI] [PubMed] [Google Scholar]
- 55.Baker TB, Mermelstein R, Collins LM, Piper ME, Jorenby DE, Smith SS, Christiansen BA, Schlam TR, Cook JW, Fiore MC. New methods for tobacco dependence treatment research. Ann Behav Med. 2011 Apr;41(2):192–207. doi: 10.1007/s12160-010-9252-y. http://europepmc.org/abstract/MED/21128037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Collins LM, Baker TB, Mermelstein RJ, Piper ME, Jorenby DE, Smith SS, Christiansen BA, Schlam TR, Cook JW, Fiore MC. The multiphase optimization strategy for engineering effective tobacco use interventions. Ann Behav Med. 2011 Apr;41(2):208–26. doi: 10.1007/s12160-010-9253-x. http://europepmc.org/abstract/MED/21132416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Berry D, Savoye M, Melkus G, Grey M. An intervention for multiethnic obese parents and overweight children. Appl Nurs Res. 2007 May;20(2):63–71. doi: 10.1016/j.apnr.2006.01.007. http://europepmc.org/abstract/MED/17481469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Finkelstein EA, Tan YT, Malhotra R, Lee CF, Goh SS, Saw SM. A cluster randomized controlled trial of an incentive-based outdoor physical activity program. J Pediatr. 2013 Jul;163(1):167–72.e1. doi: 10.1016/j.jpeds.2013.01.009. [DOI] [PubMed] [Google Scholar]
- 59.Rodearmel SJ, Wyatt HR, Stroebele N, Smith SM, Ogden LG, Hill JO. Small changes in dietary sugar and physical activity as an approach to preventing excessive weight gain: the America on the Move family study. Pediatrics. 2007 Oct;120(4):e869–79. doi: 10.1542/peds.2006-2927. http://pediatrics.aappublications.org/cgi/pmidlookup?view=long&pmid=17908743. [DOI] [PubMed] [Google Scholar]
- 60.Walders-Abramson N, Wamboldt FS, Curran-Everett D, Zhang L. Encouraging physical activity in pediatric asthma: a case-control study of the wonders of walking (WOW) program. Pediatr Pulmonol. 2009 Sep;44(9):909–16. doi: 10.1002/ppul.21077. http://europepmc.org/abstract/MED/19658109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sigmund E, El Ansari W, Sigmundová D. Does school-based physical activity decrease overweight and obesity in children aged 6-9 years? A two-year non-randomized longitudinal intervention study in the Czech Republic. BMC Public Health. 2012 Jul;12:570. doi: 10.1186/1471-2458-12-570. http://www.biomedcentral.com/1471-2458/12/570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hyndman BP, Benson AC, Ullah S, Telford A. Evaluating the effects of the Lunchtime Enjoyment Activity and Play (LEAP) school playground intervention on children's quality of life, enjoyment and participation in physical activity. BMC Public Health. 2014 Feb;14:164. doi: 10.1186/1471-2458-14-164. http://www.biomedcentral.com/1471-2458/14/164. [DOI] [PMC free article] [PubMed] [Google Scholar]