Abstract
From the conception of HTA in the 1970s it has been argued that addressing ethical issues is an element of HTA, and many methods for integrating ethics in HTA have become available. However, despite almost 40 years with repeated intentions, only few HTA reports include ethical analysis. Why is this so? How come, ethics is a constituent part of HTA, there are many methods available, but ethics is rarely part of practical HTA work?
This is the key question of this article and several reasons why ethics is not a part of HTA are identified. A) Ethicists are professional strangers in HTA. B) A common agreed methodology for integrating ethics is lacking. Ethics methodology appears to be C) deficient, D) insufficient, or E) unsuitable. F) Integrating ethics in HTA is neither efficient nor needed for successful HTA. G) Most moral issues are general, and are not specific to a given technology. H) All relevant ethical issues can be handled within other frameworks, e.g., within economics. I) Ethics can undermine or burst the foundation of HTA.
Hence, there are many reasons why ethics is not an integrated part of HTA so many years after identifying ethics as constitutive to HTA. These reasons may all explain why it is so, but on closer scrutiny, they do not work as compelling arguments for not addressing ethical issues in HTA. Hence, the identified reasons may work well as explanations, but not as justifications.
In order to move on from a situation of failure we can:
Exclude ethics from definitions of HTA, and as a consequence, establish a separate kind of evaluation (Health Technology Evaluation – HTE).
Take the existing definition seriously and actually integrate ethics in the performance of HTA practice.
Amend, expand or change HTA so that ethics is more genuinely incorporated.
Which of these options to choose is open for discussion, but we need to move away from a situation where we have a definition of HTA which does not correspond with HTA practice.
Keywords: ethics, methodology, HTE, evaluation, technology, moral philosophy
Introduction
From the conception in the 1970s it has been argued that ethics is part of health technology assessment (HTA) [1]. Early definitions of technology assessment explicitly include ethical issues: “Technology assessment is comprehensive in scope, examining impacts on social, ethical, legal, and other systems . . .” [2], and so do more recent definitions of HTA [3], [4], [5]. E.g., HTA is defined as:
Identifying evidence, or lack of evidence, on the benefits and costs of health interventions
Synthesizing health research findings about the effectiveness of different health interventions
Evaluating the economic implications and analysing cost and cost-effectiveness
Appraising social and ethical implications of the diffusion and use of health technologies as well as their organisational implications [5].
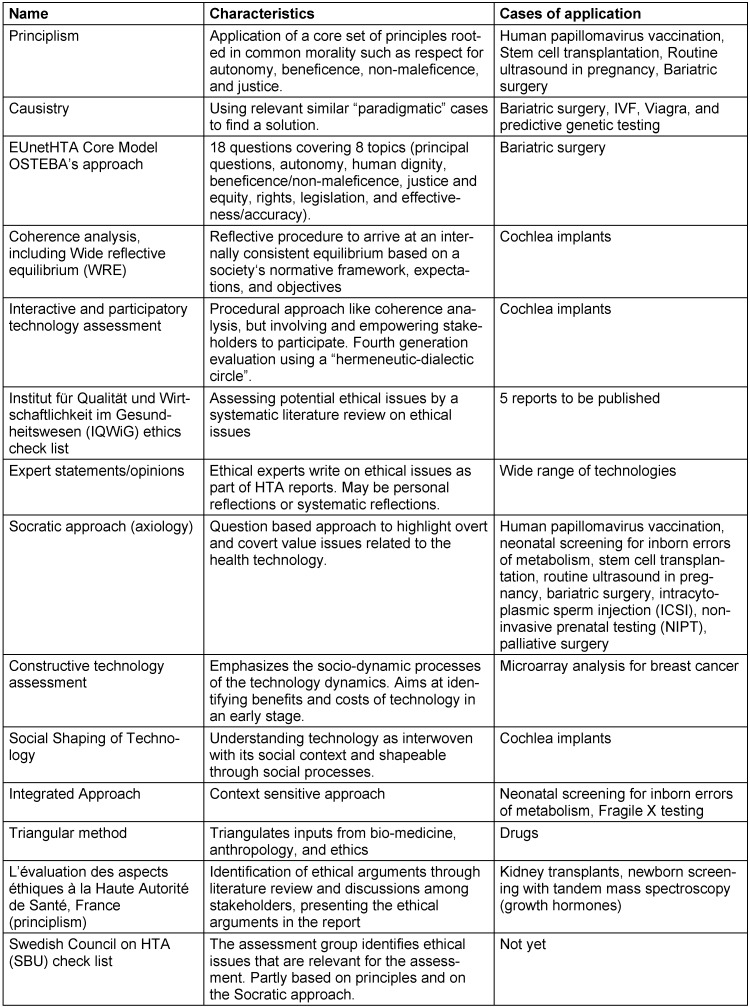
A variety of methods in ethics are available, and some have been developed specially for integrating ethics in HTA [6], [7], [8]. Table 1 (Tab. 1) gives an overview of some of the approaches.
Table 1. Approaches for addressing ethical issues in HTA.
Despite the many available methods, HTA reports seldom include ethics, i.e., there appear to be more methods than applications [9]. Regardless of the explicit definitions of HTA who include ethics, “[i]n practice, HTAs are frequently more narrowly defined” [10]. 17% of 680 HTA reports from six Canadian agencies addressed ethical issues between 1997 and 2006 [11] and 5% of 223 HTA reports published from nine HTA agencies between 2003 and 2006 in four different countries considered ethical, social and organizational issues, in addition to clinical and economic evaluations [12]. Only few articles in International Journal of Health Technology Assessment are about ethics [13].
How come if ethics is a constituent part of HTA, and there are many methods available, ethics is rarely part of practical HTA work? This is the key question in this article. There must be some quite compelling reasons for NOT integrating ethics, as ethics still plays a modest role in HTA, more than 30 years after its conception.
In this article I identify several of the reasons why ethics is not an integrated part of HTA. Although these reasons may work well as explanations for why ethics is not integrated, closer scrutiny reveals that they are not sound as justifications for not integrating ethics. At the end alternative strategies for addressing ethical issues in HTA are discussed. The identified reasons for not to integrate ethics in HTA are:
A) Ethicists are professional strangers in HTA.
B) A common agreed methodology for integrating ethics is lacking.
Ethics methodology appears to be C) deficient, D) insufficient, or E) unsuitable.
F) Integrating ethics in HTA is neither efficient nor needed for successful HTA.
G) Most moral issues are general, and are not specific to a given technology.
H) All relevant ethical issues can be handled within other frameworks, e.g., within economics.
I) Ethics can undermine or burst the foundation of HTA.
Why not integrate ethics in HTA?
There appear to be many reasons why ethics is not integrated in HTA. In the following the identified reasons will be presented. Whether these explanations also work as justifications, will be discussed below.
However, first a short clarification. The question “why not integrate ethics in HTA” can mean “why ethics as a discipline should not be integrated into HTA,” “why ethicists should not be part of HTA staff,” “why ethicists should not take part in HTA procedures,” or “why methods or approaches in ethics should not be integrated into HTA.” The focus of attention in this article is the reasons why ethical issues are not addressed in the HTA process of those agencies who define ethics as a constituent part of HTA.
A) Strangers from other professional cultures
One of them is that ethics and HTA are profoundly different activities. The goals, methods, models, and modes of rationality of HTA and ethics are categorically dissimilar. HTA has a stringent methodological basis that appears incompatible with ethics and that is hard to change in order to facilitate integration. HTA and ethics are based in quite distinct cultures. While HTA originates from the natural sciences, ethics is firmly based in the humanities. HTA may see ethics as yet another tool [14], [15] or handmaiden [16], while ethics as a discipline does not easily fit in such formulas.
Accordingly, ethicists are professional strangers in the field of HTA.
B) No methodology
Moreover, there is no agreement on (ethical) method which could be integrated in HTA. A series of traditional ethical approaches have been applied, such as principlism [17], [18], [19], casuistry [20], utilitarianism, and coherence analysis [21], [22], [23], [24]. In addition, a wide variety of methods have been developed specially for handling ethical issues in HTA, such as an interactive (participatory) HTA [25], [26], [27], [28], a context sensitive approach [29], an eclectic approach [30], a complex systems approach [31], various approaches within the framework of Social Shaping of Technology [32], [33], and several axiological approaches [6], [34], [35], [36]. See Table 1 (Tab. 1). Although there have been serious attempts to come to agreements on methodology in working groups on ethics in INHTA [7], HTAi, and EUnetHTA there is still no univocal agreement. We lack methodological guidelines for addressing ethical issues [37]. Addressing ethical issues may therefore be left out, because there are too many methods and to little agreement.
Hence, the lack of agreed methodology may be one reason why ethics is left out.
C) Deficient methodology
There may be many roots to this lack of agreement on methodology. It may be because available ethics methodology is flawed or deficient [38], [39], [40], the methods are underdeveloped [41], poorly adapted to HTA, or because ethical approaches may always be subjective and biased [41]. Accordingly, one can argue that ethics methodology is unsuitable for HTA.
D) It is not worth the effort
A corresponding pragmatic argument goes like this: it has taken so long to try to integrate ethics in HTA and so many resources has been spent; it obviously cannot be worth the effort. There is no evidence of the effectiveness and efficiency of HTA when integrating ethics. It is hard to design studies showing the outcome of integrating ethics, but even if such obstacles would be overcome; there are reasons to believe that the efficiency is low. Having to address ethical issues (explicitly) may hamper the decision making process. The forecasted or promised increased diffusion of HTA results when integrating ethics has not been observed [6]. Moreover, ethicists tend to mess things up more than sort them out. We need clear answers, not muddled questions. Letting one ethicist into the room is the same as letting in a pile of incoherent opinions. Moreover, a survey revealed that most HTA professionals believe that ethical assessments could be performed by HTA experts [13]. This means including ethicists in the HTA process is not necessary.
Hence, it is not efficient to integrate ethics in HTA, as it does not pay off, especially not when involving ethicists.
E) Not needed
In a survey among 104 authors in International Journal of Technology Assessment between 2005 and 2007, more than 90 percent of respondents agreed that healthcare decisions involved value judgments and that ethical analysis was important to HTA [13]. However, less than half of them considered ethical analysis and recommendations to be necessary.
In the search for evidence, moral issues are avoided [10]. Accordingly, ethical analysis is not needed in HTA.
F) Too narrow scope
Moreover, there appear to be profound limitation in ethics reducing its relevance for HTA. A core characteristic of technology is its unintended and surprising applications. E.g. radiological services developed for diagnosing somatic diseases, are used also for treating mental conditions in patients, such as fear and health anxiety, to confirm people’s health, and (sometimes, but not insignificantly) to treat mental conditions of referring physicians, e.g., professional uncertainty and uneasiness as well as fear of litigation. Moreover, normative issues important to decision makers, such as political pressure on vaccines and screening programs, may not be covered by ethics approaches.
Hence, ethics may be too limited in scope to address the important moral aspects of health technology.
G) Business as usual
Additionally, most technologies are not morally challenging, and need no ethical analysis [21]. Ethical analyses have been developed and used for curious technologies such as cochlea implants, assistive reproductive technologies (ARTs), and genetic tests (GTs). These technologies pose general moral issues and not issues related to the specific technology. E.g., cochlea implants pose issues with respecting sign language communities, ARTs raise questions of how far we should go in creating and selecting human embryos, and GTs actualize issues on how we should handle predictive information. These are general moral questions, which are made topical by the technology [42]. With regards to diagnostic ultrasound machines, statins, and bypass surgery, there is little disagreement. There may of course be moral issues with regards to prioritization, but it can be argued that these are mainly political issues, or ethical issues related to the decision making context, and are not genuine to the technology to be assessed. Hence, there are few moral issues related to specific technologies, as most moral issues are general issues that should be debated on a general level in society, and not related to the assessment of specific technologies.
H) Economy covers it all
Correspondingly, one can argue that economic analysis is sufficient for handling ethical issues in HTA. The morally relevant issues, such as benefit (clinical effectiveness), safety (harm), equity and distributive justice, can be exhaustively handled in terms of economic evaluation. Other moral issues may of course be relevant, but are not part of HTA. The utilitarianism at the bedrock of economics is sufficient for handling all relevant ethical issues with health technology, especially if we include compensations for some of its adverse effects, such as age discrimination. Hence, economics covers all relevant ethical issues, and no extra ethical analysis is needed.
I) Bursting the HTA framework
One more reason why ethicical issues have not obtained a more noticeable place in HTA is that ethics may burst the limits to what kind of issues that then could be addressed. Health technology can have a wide range of ethical implications. It is well known that health technology can challenge human autonomy, integrity, dignity, human rights, moral status, equity, justice, and that safety issues can be morally challenging [6], [8], [34]. However, the normative issues are much wider, and include challenges with definitions of health care ends (end points), definitions and classification of disease entities, corresponding stigmatization of patient groups, medicalization, turf wars, and defensive medicine. It involves cultural and societal values such as linguistic identity (deaf community), research ethics (ways of gaining knowledge), and implications for legal and political systems (challenges with consumer liability) [43].
Hence, ethics may challenge the foundation of HTA. Ethics may contest HTA’s scientific aspirations and influence or even undermine its methodological bedrock. It challenges the scientific purity of systematic reviews by questioning end-points, challenges evidence paradigms [43], [44], [45], discloses stakeholders’ interests, queries the role of HTA agencies and their agents, and promotes patient participation. Ethics could revolutionize HTA, and come to integrate HTA in ethics rather than integrating ethics in HTA. It would move HTA from assessing technology to shaping technology, from observing the application of technology to intervening in its implementation, and from a unilateral to a bilateral conception of the relationship between technology and society [43].
Hence, there is no limit to or control of what could be integrated in HTA, so ethics could undermine or burst the foundation of HTA.
Correspondingly, it can be argued that ethical issues are better dealt with in the framework of (Parliamentary) Technology Assessment (PTA) than in HTA. HTA is more preoccupied with the “clinical perspective” than with the “societal perspective” of PTA [10], [46]. The most relevant and pressing ethical issues will not be addressed within the HTA framework, but only those selected by the HTA ideology [25], [27], [28], [32], [33], [34], [37], [38], [46], [47]. ”Biomedicine appears to have been more of a task for parliamentary TA than for classical Health Technology Assessment.” ([46], p. 215) Hence, if moral issues should be handled, it will be more effectively done in the framework of TA or other frameworks.
In other words ethics would promote a transfer of HTA to (Parliamentary) Technology Assessment framework [46]. Instead of assessing the implications of a technology within a given social framework, it may reframe the conception of disease, health, technology, and health care ends. The (health) conditions, end-points, assessment perspectives are to depend on and be shaped by our social values. Such a “normative contamination” could harm HTA methodology, and avoiding integrating ethics in HTA, would be a way to keep HTA clean. Letting ethics into HTA can adjourn the differentiation between various kinds of norms (moral norms, scientific norms, technological norms, policy making norms, political norms) and consequently disguise power-knowledge relationships. [On the other hand one can argue that one should prevent to integrate ethics in HTA in order to avoid contaminating ethics. There is a substantial danger that ethics is applied as a tool or device in HTA in order to handle normative issues [15], reducing ethics to a normative technology.]
Discussion
Hence, there are many reasons for not integrating ethics in HTA, many of which provide reasonable explanations for why ethics is not yet an effectively integrated part of HTA. The following have been identified:
A) Ethicists are professional strangers in HTA.
B) A common agreed methodology is lacking.
C) Ethics methodology appears to be deficient,
D) insufficient, and unsuitable.
E) Integrating ethics in HTA is neither efficient nor needed.
F) Ethical analysis has a too narrow scope.
G) There are few ethical issues which are technology specific.
H) All relevant ethical issues can be handled within economics.
I) Ethics can contaminate, undermine or burst the foundation of HTA.
There may of course also be other reasons, explaining why ethics is so peripheral in HTA, e.g., that it makes HTA more expensive, that professional ethicists with HTA expertize are hard to find etc. However, the reasons presented above are considered to be the most plausible reasons why ethics is not integrated in HTA, and those reasons that may also serve as arguments for not integrating ethics in HTA.
However, are these reasons, also good arguments against integrating ethics? Do they justify not addressing ethical issues in HTA reports?
A) Ethicists being professional strangers in HTA is hardly a good argument. HTA does not comprise a professional unity, and there are other “strangers” in HTA as well, who are well assimilated. HTA agencies hire statisticians, epidemiologists, MDs, biologists, economists, physiotherapists, midwifes, anthropologists, and social scientists, to mention but a few. Within each of these, there are many schools.
B) The lack of common methodology is hardly a convincing argument either, as there are debates and disagreements on methodological issues within HTA, and multiple methods are applied in statistics, economics, and in ethics. A lack of standard or guidance does hardly justify not addressing ethical issues. Besides it is argued (by ethicists) that the important thing is not which method is used, but that ethical issues are addressed [7], [8], [34], [35].
C) Whether ethics methodology is deficient, insufficient or unsuitable strongly depends on the purpose of ethical analysis, e.g., whether the goal is assessment, appraisal, or elaborating guidelines. It is difficult to see why all ethical methods should be unsuitable for all purposes.
D) It is of course difficult to assess the effectiveness and efficiency of integrating ethics in HTA. However, there is little assessment of HTA itself. How effective is HTA as a decision making support system? If this is a good argument against ethics in HTA, it is a good argument against many forms of HTA as well. If one does not require evidence of the effectiveness and efficiency of HTA itself, it is hard to see why one should require evidence for the effectiveness and efficiency of integrating ethics in HTA. The other way around: if one had methods to assess the effectiveness and efficiency of HTA, it would be reasonable to assess HTA with integrated ethics in the same manner. Moreover, if HTA experts could address ethical issues in HTA [13], then this actually could be a way to integrate ethics in HTA and an argument for doing so.
E) Although most authors in IJHTAHC did not find ethical analyses or recommendations necessary, this does not mean that such analysis and recommendations are not important for the decision process. Besides they appear to be inconsistent when finding that value judgments are important to HTA, but that analysis of such value issues are not [13].
F) It may well be that some approaches in ethics have too narrow scopes to address all relevant moral aspects of health technologies. However, it is hard to see how this is a convincing argument against addressing ethical issues in HTA, as the problem appears to be the opposite. HTA agencies do not find it compelling to address ethical issues. Besides, existing HTA methodology is not able to address unforeseen implications of technology. On the contrary, several of the ethical approaches explicitly focus on unforeseen implications (see Table 1 (Tab. 1)) [35]. Moreover, the fact that ethical analyses may overlook some aspects, does not mean that they systematically overlook the most important ethical aspects.
G) Although, many of the moral issues discussed with respect to health technology are generic or general, it does not make it irrelevant to highlight, analyze, and discuss them when assessing particular technologies. Moreover, issues of prioritization may be political, or ethical issues related to the decision making process. They are nevertheless ethical issues related to the implementation of the health technology.
H) While economy has come to be ever more important, it is far from obvious that all moral questions can be discussed within the framework of economics. Economic analysis has, as mentioned above, a series with limitations in addressing ethical issues. Moreover, the conclusions from utilitarianism as a moral theory may diverge significantly from those of economic analysis.
I) It is hard to believe that ethics would be able to undermine HTA methodology and identity. Besides, HTA has been influenced from many fields (statistics, economics, study design, health policy making) and has been evolving rapidly, integrating perspectives and methodologies from various areas. Although somewhat different, it is difficult to see that ethics cannot be part of the HTA development. Ethics is about evaluation. So is HTA. Hence, ethics should not be a stranger to HTA more than other integrated disciplines. Moreover, HTA is in continuous development and is influenced from a wide range of general trends and theories. Ethics may well be one of them. Additionally, the claim that ethics could undermine or burst the foundation of HTA is only true for perspectives of “ethics of HTA” and not for “ethics in HTA.” Hence, there are a wide range of approaches available that do not threaten HTA, see Table 1 (Tab. 1).
Hence, although the identified reasons why ethics is not part of HTA may well explain why there is so little ethics in HTA practice, they do not represent convincing arguments that ethics should not be part of HTA and are not supported by such arguments. That is, they do not justify excluding addressing ethical issues in HTA.
The arguments for integrating ethics in HTA still appear to have some weight. The major reason for the relevance of ethics is that health care is a moral endeavor, and that ethics is a reflection on this moral endeavor. Correspondingly, HTA is a reflection on certain aspects of health care, and therefore, HTA cannot escape the moral issues that are embedded in its subject matter.
Furthermore, health technology is related to values [6], [47], [48], [49], [50], [51], [52], [53] and is a way to improve the life of human individuals. This involves questions of what the good life is, and hence ethical issues (in terms of endpoints of health interventions). Trying to ignore such questions may inflict with the moral foundation of health care: to help people.
Additionally, ethics is systematic reflection on values. HTA is an evaluation, and as such also a reflection on values. As HTA shares the aim of health care, i.e., the good and healthy life of individual citizens, HTA also includes assessment of moral values. And as HTA cannot free itself from dealing with moral values (underpinning its professional and methodological values), there is a profound affinity between HTA and ethics.
Hence, there are still relevant arguments for integrating ethics in HTA [54].
So what should we do after more than 30 years of intentions with few implications?
There are several options. We can:
Exclude ethics from definitions of HTA, and consequently, establish a separate kind of evaluation (Health Technology Evaluation – HTE) focusing on ethics.
Take the existing definition seriously and actually integrate ethics in the performance of HTA today, e.g., by using one or more of the approaches listed in Table 1 (Tab. 1).
Amend, expand or change HTA to incorporate ethics, e.g. through fourth generation evaluation [54], Parliamentary Technology Assessment, PTA [46], or a series of other options.
The first option is obviously the purest and easiest. If health technology assessments, decision making, and health policy making will benefit from this, is open for discussion.
The second option demands that we translate words into actions, i.e., we have to take the definitions of HTA seriously. It may make HTAs more complicated. However, it may also make the HTA process and decisions more open and transparent. The third option is most challenging for traditional HTA. However, a revision of HTA through input from ethics and other disciplines may be mutually fruitful. “Given the profound societal changes associated with the integration of health technologies, HTA producers have a particular responsibility to enlighten and inform technology-related policy and public debate. Fulfilling this role, though, requires making social and ethical dimensions explicit in HTA processes and products.” [55]
Other options than those mentioned here, may also be relevant. One can abandon HTA altogether and replace it by other forms of evaluation, or by particular perspectives in moral philosophy or in science and technology studies (STS). Discussing such alternatives is beyond the scope of this article.
Moreover, it may be argued that the definitions of HTA quoted in the introduction only argue that ethical aspects have to be regarded as well as social and legal aspects. In a strict sense they do not say that ethics, e.g. as a discipline, has to be part of HTA. However, as pointed out at the outset of this article, the important point is whether ethical issues are addressed. Introducing ethics is of course but one way to addressing ethical issues.
It may also be maintained that the arguments in favor of addressing ethical issues in HTA presented above (health care being evaluative, aiming at “the good life,” technology being value laden, and HTA itself being evaluative) are general arguments for integrating ethics in many fields of decision making, such as politics, but not specific arguments for integrating ethics in HTA. Here we may reply that whether an argument also has general implications, does not necessarily weaken its specific relevance. Moreover, the arguments for integrating ethics in HTA have been addressed in detail elsewhere [56]. The point here has been to examine the reasons why ethical issues have not been integrated in HTA.
The point here is not to promote one of the options in particular, but only to indicate that we need to move on from a situation where we have definitions of HTA which are not in correspondence with our practice.
Conclusion
There are many reasons why ethics is not an integrated part of HTA today, more than 30 years after identifying ethics as constitutive to HTA. These reasons can explain why it is so, but they do not work as compelling arguments for not addressing ethical issues in HTA. Health is a matter of the good life, i.e., an ethical issue. This makes technology to improve health an issue for ethics as well. The same goes for methods to evaluate health technology.
In the current situation we can either exclude ethics from definitions of HTA, and as a consequence, establish a separate kind of evaluation (Health Technology Evaluation – HTE), or we can take the existing definition seriously and actually integrate ethics in the performance of HTA today, e.g., by implementing one of the approaches mentioned in Table 1 (Tab. 1), or we can amend, expand or change HTA so that ethics is more genuinely incorporated.
Which of the options to choose is open for discussion, but we need to move on from a situation where we have a definition of HTA which is not in correspondence with HTA practice.
Notes
Acknowledgements
Although the manuscript was written before the start of the EU-funded project INTEGRATE HTA (http://www.integrate-hta.eu/, Seventh Framework Programme FP7-Health-2012-Innovation with grant agreement number 306141), the revision of the manuscript has been partly funded by this project. I am also most thankful to two anonymous reviewers for valuable comments and fruitful suggestions.
Competing interests
The author declares that he has no competing interests.
References
- 1.Banta HD. Foreword. Poiesis Prax. 2004;2:93–5. doi: 10.1007/s10202-003-0044-3. Available from: http://dx.doi.org/10.1007/s10202-003-0044-3. [DOI] [Google Scholar]
- 2.Office of Technology Assessment (OTA) Development of medical technologies: Opportunities for assessment. Washington: United States Congress; 1976. [Google Scholar]
- 3.Liberati A, Sheldon TA, Banta HD. EUR-ASSESS Project Subgroup report on Methodology. Methodological guidance for the conduct of health technology assessment. Int J Technol Assess Health Care. 1997;13(2):186–219. doi: 10.1017/S0266462300010369. Available from: http://dx.doi.org/10.1017/S0266462300010369. [DOI] [PubMed] [Google Scholar]
- 4.International Network of Agencies for Health Technology Assessment. Technology Assessment. HTA Resources. 2011. Available from: http://www.inahta.org.
- 5.Jonsson E, Banta HD, Henshall C, Sampietro-Colom L. Summary report of the ECHTA/ECAHI project. European Collaboration for Health Technology Assessment/Assessment of Health Interventions. Int J Technol Assess Health Care. 2002;18(2):218–237. doi: 10.1017/s0266462302000247. [DOI] [PubMed] [Google Scholar]
- 6.Hofmann B. On value-judgements and ethics in health technology assessment. Poiesis Prax. 2005;3(4):277–295. doi: 10.1007/s10202-005-0073-1. Available from: http://dx.doi.org/10.1007/s10202-005-0073-1. [DOI] [Google Scholar]
- 7.Burls A, Caron L, Cleret de Langavant G, Dondorp W, Harstall C, Pathak-Sen E, Hofmann B. Tackling ethical issues in health technology assessment: a proposed framework. Int J Technol Assess Health Care. 2011 Jul;27(3):230–237. doi: 10.1017/S0266462311000250. Available from: http://dx.doi.org/10.1017/S0266462311000250. [DOI] [PubMed] [Google Scholar]
- 8.Saarni SI, Braunack-Mayer A, Hofmann B, van der Wilt GJ. Different methods for ethical analysis in health technology assessment: an empirical study. Int J Technol Assess Health Care. 2011 Oct;27(4):305–312. doi: 10.1017/S0266462311000444. Available from: http://dx.doi.org/10.1017/S0266462311000444. [DOI] [PubMed] [Google Scholar]
- 9.Droste S, Dintsios CM, Gerber A, Rüther A. Integrating ethical issues in HTAs: More methods than applications?. Maximizing the Value of HTA. Book of Abstracts; HTAi 7th Annual Meeting; 2010 Jun 6-9; Dublin, Ireland. p. 169. [Google Scholar]
- 10.Draborg E, Gyrd-Hansen D, Poulsen PB, Horder M. International comparison of the definition and the practical application of health technology assessment. Int J Technol Assess Health Care. 2005;21(1):89–95. doi: 10.1017/S0266462305050117. Available from: http://dx.doi.org/10.1017/S0266462305050117. [DOI] [PubMed] [Google Scholar]
- 11.DeJean D, Giacomini M, Schwartz L, Miller FA. Ethics in Canadian health technology assessment: a descriptive review. Int J Technol Assess Health Care. 2009 Oct;25(4):463–469. doi: 10.1017/S0266462309990390. Available from: http://dx.doi.org/10.1017/S0266462309990390. [DOI] [PubMed] [Google Scholar]
- 12.Lavis J, Wilson M, Grimshaw J, et al. Towards optimally packaged and relevance assessed health technology assessments. Report Submitted to the Canadian Agency for Drugs and Technologies in Healthcare. Hamilton, Ontario: McMaster University Program in Policy Decision-Making; 2007. [Google Scholar]
- 13.Arellano LE, Willett JM, Borry P. International survey on attitudes toward ethics in health technology assessment: An exploratory study. Int J Technol Assess Health Care. 2011 Jan;27(1):50–54. doi: 10.1017/S0266462310001182. Available from: http://dx.doi.org/10.1017/S0266462310001182. [DOI] [PubMed] [Google Scholar]
- 14.ten Have H. Ethical perspectives on health technology assessment. Int J Technol Assess Health Care. 2004;20(1):71–76. doi: 10.1017/S0266462304000819. Available from: http://dx.doi.org/10.1017/S0266462304000819. [DOI] [PubMed] [Google Scholar]
- 15.ten Have HA. Medical technology assessment and ethics. Ambivalent relations. Hastings Cent Rep. 1995 Sep-Oct;25(5):13–19. doi: 10.2307/3562789. Available from: http://dx.doi.org/10.2307/3562789. [DOI] [PubMed] [Google Scholar]
- 16.Braunack-Mayer AJ. Ethics and health technology assessment: handmaiden and/or critic? Int J Technol Assess Health Care. 2006;22(3):307–312. doi: 10.1017/S0266462306051191. Available from: http://dx.doi.org/10.1017/S0266462306051191. [DOI] [PubMed] [Google Scholar]
- 17.Andersen S. MTV og etik. organisation og sundhedsøkonomi. In: Sigmund H, Kristensen FB, editors. MTV, sundhedstjenesteforskning og klinisk praksis. Rapport fra symposium om evidensbaseret sundhedsvæsen. København: Statens Institut for Medicinsk Teknologivurdering; 2000. Available from: htpp://www.mtv-instituttet.dk. [Google Scholar]
- 18.Andersen S. Patienten. Etikken. Medicinsk Teknologivurdering – puljeprojekter. 2002;2(1):75–100. Available from: http://sundhedsstyrelsen.dk/publ/Publ2002/Praeimplant/Praeimplant.pdf. [Google Scholar]
- 19.Royal Commission on New Reproductive Technologies. Proceed with care: final report of the Royal Commission on New Reproductive Technologies. Ottawa: Canada Communications Group-Publishing; 1993. [Google Scholar]
- 20.Giacomini M. One of these things is not like the others: the idea of precedence in health technology assessment and coverage decisions. Milbank Q. 2005;83(2):193–223. doi: 10.1111/j.1468-0009.2005.00344.x. Available from: http://dx.doi.org/10.1111/j.1468-0009.2005.00344.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grunwald A. The normative basis of (health) technology assessment and the role of ethical expertise. Poiesis Prax. 2004;2:175–193. doi: 10.1007/s10202-003-0050-5. Available from: http://dx.doi.org/10.1007/s10202-003-0050-5. [DOI] [Google Scholar]
- 22.Musschenga AW. Empirical ethics, context-sensitivity, and contextualism. J Med Philos. 2005 Oct;30(5):467–490. doi: 10.1080/03605310500253030. Available from: http://dx.doi.org/10.1080/03605310500253030. [DOI] [PubMed] [Google Scholar]
- 23.Krones T, Neuwohner E, Bock K, Manolopoulos K, Tinneberg HR, Richter G. Attitudes of patients, healthcare professionals and ethicists towards embryonic stem cell research and donation of gametes and embryos in Germany. Reprod Biomed Online. 2006 Nov;13(5):607–617. doi: 10.1016/S1472-6483(10)60650-5. Available from: http://dx.doi.org/10.1016/S1472-6483(10)60650-5. [DOI] [PubMed] [Google Scholar]
- 24.Krones T, Schlüter E, Manolopoulos K, Bock K, Tinneberg HR, Koch MC, Lindner M, Hoffmann GF, Mayatepek E, Huels G, Neuwohner E, El Ansari S, Wissner T, Richter G. Public, expert and patients’ opinions on preimplantation genetic diagnosis (PGD) in Germany. Reprod Biomed Online. 2005 Jan;10(1):116–123. doi: 10.1016/S1472-6483(10)60812-7. Available from: http://dx.doi.org/10.1016/S1472-6483(10)60812-7. [DOI] [PubMed] [Google Scholar]
- 25.Reuzel RP, van der Wilt GJ, ten Have HA, de Vries Robbé PF. Reducing normative bias in health technology assessment: interactive evaluation and casuistry. Med Health Care Philos. 1999;2(3):255–263. doi: 10.1023/A:1009963018813. Available from: http://dx.doi.org/10.1023/A:1009963018813. [DOI] [PubMed] [Google Scholar]
- 26.Reuzel RPB. Interactive technology assessment of paediatric cochlear implantation. Poiesis Prax. 2004;2:119–137. doi: 10.1007/s10202-003-0052-3. Available from: http://dx.doi.org/10.1007/s10202-003-0052-3. [DOI] [Google Scholar]
- 27.Reuzel R, Van der Wilt GJ. Health Technology Assessment and evaluation: back to the basics? Evaluation. 2000;6(4):383–398. doi: 10.1177/13563890022209389. Available from: http://dx.doi.org/10.1177/13563890022209389. [DOI] [Google Scholar]
- 28.Skorupinski B, Ott K. Technology assessment and ethics. Poiesis Prax. 2002;1:95–122. doi: 10.1007/s102020100010. Available from: http://dx.doi.org/10.1007/s102020100010. [DOI] [Google Scholar]
- 29.Caron L. Integrating ethics into HTA. HTAi conference; 2005 Jun 20th; Rome, Italy. [Google Scholar]
- 30.Autti-Rämö I, Mäkelä M. Ethical evaluation in health technology assessment reports: an eclectic approach. Int J Technol Assess Health Care. 2007 Winter;23(1):1–8. doi: 10.1017/S0266462307051501. [DOI] [PubMed] [Google Scholar]
- 31.Cleret de Langavant G. Bioéthique: Méthode et complexité. Québec: Les Presses de l’Université du Québec; 2001. [Google Scholar]
- 32.Rip A, Misa TJ, Schot J, editors. Managing technology in society: the approach of constructive technology assessment. London: Pinter; 1995. [Google Scholar]
- 33.Clausen C, Yoshinaka Y. Social shaping of technology in TA and HTA. Poiesis Prax. 2004;2(2,3):221–46. doi: 10.1007/s10202-003-0046-1. Available from: http://dx.doi.org/10.1007/s10202-003-0046-1. [DOI] [Google Scholar]
- 34.Hofmann B. Toward a procedure for integrating moral issues in health technology assessment. Int J Technol Assess Health Care. 2005 Summer;21(3):312–318. doi: 10.1017/S0266462305050415. Available from: http://dx.doi.org/10.1017/S0266462305050415. [DOI] [PubMed] [Google Scholar]
- 35.Hofmann B, Droste S, Oortwijn W, Cleemput I, Sacchini D. Harmonization of ethics in health technology assessment: a revision of the Socratic approach. Int J Technol Assess Health Care. 2014 Jan;30(1):3–9. doi: 10.1017/S0266462313000688. Available from: http://dx.doi.org/10.1017/S0266462313000688. [DOI] [PubMed] [Google Scholar]
- 36.European Network for Health Technology Assessment (EUnetHTA) HTA Core Model® online. Available from: http://meka.thl.fi/htacore/
- 37.Potter BK, Avard D, Graham ID, Entwistle VA, Caulfield TA, Chakraborty P, Kennedy C, McGuire M, Griener GG, Montgomery M, Wells GA, Wilson BJ. Guidance for considering ethical, legal, and social issues in health technology assessment: application to genetic screening. Int J Technol Assess Health Care. 2008;24(4):412–422. doi: 10.1017/S0266462308080549. Available from: http://dx.doi.org/10.1017/S0266462308080549. [DOI] [PubMed] [Google Scholar]
- 38.ten Have H. Ethical perspectives on health technology assessment. Int J Technol Assess Health Care. 2004 Winter;20(1):71–76. doi: 10.1017/s0266462304000819. [DOI] [PubMed] [Google Scholar]
- 39.Duthie K, Bond K. Improving ethics analysis in health technology assessment. Int J Technol Assess Health Care. 2011 Jan;27(1):64–70. doi: 10.1017/S0266462310001303. Available from: http://dx.doi.org/10.1017/S0266462310001303. [DOI] [PubMed] [Google Scholar]
- 40.Reuzel R, Oortwijn W, Decker M, Clausen C, Gallo P, Grin J, Grunwald A, Hennen L, van der Wilt GJ, Yoshinaka Y. Ethics and HTA: some lessons and challenges for the future. Poiesis Prax. 2004;2(2-3):247–256. doi: 10.1007/s10202-003-0054-1. Available from: http://dx.doi.org/10.1007/s10202-003-0054-1. [DOI] [Google Scholar]
- 41.Van der Wilt GJ, Reuzel R, Banta HD. The ethics of assessing health technologies. Theor Med Bioeth. 2000 Jan;21(1):103–115. doi: 10.1023/a:1009934700930. [DOI] [PubMed] [Google Scholar]
- 42.Hofmann B. The technological invention of disease - on disease, technology and values [Thesis] Oslo: University of Oslo; 2002. [Google Scholar]
- 43.Lehoux P, Blume S. Technology assessment and the sociopolitics of health technologies. J Health Polit Policy Law. 2000 Dec;25(6):1083–1120. doi: 10.1215/03616878-25-6-1083. Available from: http://dx.doi.org/10.1215/03616878-25-6-1083. [DOI] [PubMed] [Google Scholar]
- 44.Dickenson D, Vineis P. Evidence-based medicine and quality of care. Health Care Anal. 2002;10(3):243–259. doi: 10.1023/A:1022995623172. Available from: http://dx.doi.org/10.1023/A:1022995623172. [DOI] [PubMed] [Google Scholar]
- 45.Vineis P. Evidence-based medicine and ethics: a practical approach. J Med Ethics. 2004 Apr;30(2):126–130. doi: 10.1136/jme.2003.007211. Available from: http://dx.doi.org/10.1136/jme.2003.007211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hennen, L Biomedical and bioethical issues in Parliamentary TA and in Health Technology Assessment. Poiesis Prax. 2004;2:207–220. doi: 10.1007/s10202-003-0051-4. Available from: http://dx.doi.org/10.1007/s10202-003-0051-4. [DOI] [Google Scholar]
- 47.Schrader-Frechette K, Westra L. Technology and values. New York: Rowman & Littlefield Publishers; 1997. [Google Scholar]
- 48.Hofmann B. When means become ends: technology producing values. Seminar.net - Media, technology and lifelong learning. 2006;2(2) Available from: http://seminar.net/images/stories/vol2-issue2/bjorn_hofmann.pdf. [Google Scholar]
- 49.Hofmann B. Technological medicine and the autonomy of man. Eur J Med Health Care Philos. 2002;5:157–167. doi: 10.1023/A:1016070531526. Available from: http://dx.doi.org/10.1023/A:1016070531526. [DOI] [PubMed] [Google Scholar]
- 50.Hofmann B. Health Technology Assessment – science or art? GMS Health Technology Assessment. 2013;9:Doc08. doi: 10.3205/hta000114. Available from: http://dx.doi.org/10.3205/hta000114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hofmann B. Is there a technological imperative in health care? Int J Technol Assess Health Care. 2002;18(3):675–689. [PubMed] [Google Scholar]
- 52.Dreyfus HL. Heidegger on Gaining a Free Realtion to Technology. In: Schrader-Frechette K, Westra L, editors. Technology and values. New York: Rowman & Littlefield Publishers; 1997. pp. 107–114. [Google Scholar]
- 53.Ihde D. Technology and The Lifeworld: From Garden to Earth. Bloomington and Indianapolis: Indiana University Press; 1990. [Google Scholar]
- 54.Guba EG, Lincoln YS. Fourth Generation Evaluation. Newbury Park: SAGE; 1989. [Google Scholar]
- 55.Lehoux P, Williams-Jones B. Mapping the integration of social and ethical issues in health technology assessment. Int J Technol Assess Health Care. 2007;23(1):9–16. doi: 10.1017/S0266462307051513. Available from: http://dx.doi.org/10.1017/S0266462307051513. [DOI] [PubMed] [Google Scholar]
- 56.Hofmann B. Why ethics should be part of health technology assessment. Int J Technol Assess Health Care. 2008;24(4):423–429. doi: 10.1017/S0266462308080550. Available from: http://dx.doi.org/10.1017/S0266462308080550. [DOI] [PubMed] [Google Scholar]