Abstract
Endoscopic submucosal dissection (ESD) is a widely accepted treatment for early gastric and esophageal cancer. Compared to endoscopic mucosal resection, ESD has the advantage of enabling en bloc removal of tumors regardless of their size. However, ESD can result in a large artificial ulcer, which may lead to a considerable deformity. Circumferential mucosal defects of more than three-fourths the esophageal circumference, long longitudinal mucosal defects (>30 mm), and lesions in the upper esophagus are significant risk factors for the development of post-ESD strictures of the esophagus. In the stomach, a circumferential mucosal defects more than three-fourths in extent and longitudinal mucosal defects >5 cm are risk factors of post-ESD stricture. If scheduled early, regular endoscopic balloon dilation is effective in controlling and preventing post-ESD stricture. Moreover, intralesional steroid injections or oral steroids can achieve remission of dysphagia or reduce the need for repeated endoscopic balloon dilation. However, further study is needed to improve the prevention of stricture formation.
Keywords: Stricture, Esophagus, Stomach, Endoscopic submucosal dissection
INTRODUCTION
The number of patients with early esophageal and gastric cancer who undergo endoscopic resection is increasing because of the improvement in diagnostic techniques such as narrow-band imaging and the development of various devices, including knives and accessories.1 In particular, endoscopic submucosal dissection (ESD) is a useful, minimally invasive procedure for the management of early esophageal and gastric neoplasms and enables the en bloc resection of large lesions. Such resections cannot be achieved with conventional endoscopic mucosal resection (EMR). Moreover, ESD facilitates accurate histopathological assessment of specimens resected en bloc with tumor-free horizontal/vertical margins, thereby resulting in the prevention of residual disease and local recurrence.2 Consequently, the risk of ESD-related complications, including potentially life-threatening perforation and postprocedural stricture, is also increasing.
The occurrence of post-ESD stricture in the esophagus and stomach can result in dysphagia or gastric outlet obstruction-which substantially decreases patient quality of life, requiring multiple sessions of endoscopic balloon dilation (EBD)3,4-or even aspiration pneumonia.2 Although strictures have been associated with the extent of the circumference and length being resected,5 the exact incidence of and risk factors for luminal stricture after esophageal and gastric ESD are unknown. Additionally, various effective preventive treatments have been reported, including balloon dilation, and local injection or systemic administration of steroids.6,7 However, no definite recommendation for the treatment and prevention of post-ESD stricture exists. In this review, we describe the incidence, risk factors, and currently available treatment modalities for strictures occurring post-ESD in the esophagus and stomach.
POST-ESD STRICTURE IN THE ESOPHAGUS
Incidence of and risk factors for post-ESD stricture
Although the incidence of post-ESD stricture in superficial esophageal neoplasms is 5% to 17% (Table 1),8,9,10,11 the exact incidence remains unknown, and the risk of stricture is reportedly proportional to the extent of mucosal dissection. With large-sized superficial esophageal squamous cell neoplasms now becoming candidates for ESD, post-ESD stricture development has recently become a major and inevitable concern-in particular, regarding the long-term outcomes.
Table 1.
Incidence of and Risk Factors for Post-Endoscopic Submucosal Dissection Stricture in Superficial Squamous Cell Neoplasms
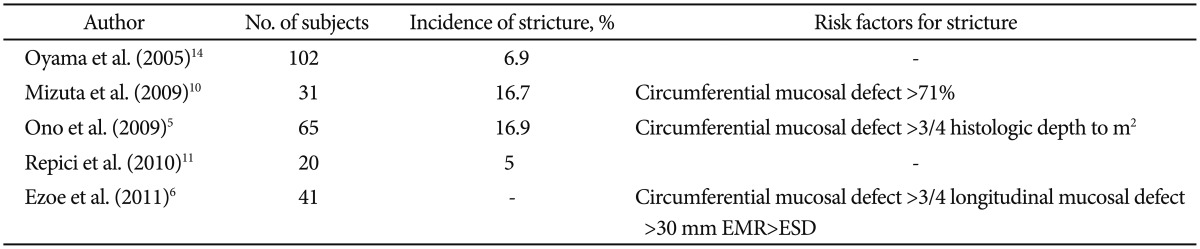
EMR, endoscopic mucosal resection; ESD, endoscopic submucosal dissection.
The possibility of esophageal stricture increases if a circumferential mucosal defect is more than three-fourths the esophageal circumference post-ESD (i.e., if the lesion size is greater than 60%).5,9,10,11 A Japanese study reported that postoperative strictures occurred in 90% of patients with lesions of more than three-fourths the circumferential extension.8 Therefore, a second-look endoscopy is performed routinely at 2 or 3 weeks post-ESD, because esophageal strictures may be evident within a few weeks post-ESD during the mucosal healing process.12 Considering the length of longitudinal mucosal defects, a longitudinal mucosal defect >30 mm is a significant risk factor for stricture development.6
The location of the tumor has also been associated with the occurrence of strictures. Lesions in the upper esophagus are reportedly complicated with post-ESD stricture more frequently than those in the lower esophagus (50% vs. 11%, respectively).10 This finding could be explained by the fact that the luminal diameter of the esophagus differs between the levels: the luminal diameter of the upper esophagus is smaller than that of the lower esophagus. Therefore, it would be natural that the smaller diameter is associated with a higher risk of post-ESD stricture.10 Moreover, histologic depth to m2 with a circumferential diameter >3 cm was also associated with the occurrence of strictures.5
Treatment modalities for post-ESD stricture
Endoscopic balloon dilation
In the setting of benign strictures, EBD has been the treatment of choice. If scheduled early, regular EBD is effective in preventing and controlling post-ESD strictures. In association with dysphagia, post-ESD strictures can be successfully managed with EBD in a median of two sessions;5 however, repetitive, periodic EBD is usually needed for preventing and controlling postprocedural strictures even post-ESD.13 Generally, EBD using a controlled radial expansion balloon dilator is started 3 days post-ESD and performed once or twice weekly for 8 weeks. In each session, the EBD diameter is initially set at 13 to 15 mm. Greater diameters may be required when patients remain symptomatic, and the lumen is dilated to 18 mm.
However, post-ESD strictures are potentially more complex than those arising from other causes. This is a reflection of both the greater extent of the initial mucosal defects treated and the inclusion of more elderly patients, who tend to undergo minimally invasive ESD safely. Furthermore, post-ESD strictures require several dilation procedures despite the short interval before initial dilation therapy. The rate of perforation during dilation has been reportedly as high as 9.0% in the case of post-ESD strictures,14 which is slightly higher than that in the case of strictures secondary to other causes.15 Two known factors for esophageal perforation during dilation are the location of the stricture in the lower esophagus and the need for multiple dilations.14
Endoscopic steroid injection
Although EBD has been the best treatment modality in the setting of benign esophageal stricture, additional intralesional steroid injections into corrosive or anastomotic strictures after EBD can achieve remission of dysphagia or reduce the need for repeated EBD.16,17 Steroids modulate wound healing through their anti-inflammatory effects by decreasing prolyl hydroxylase activity and by amplifying collagenase activity; thus, the tissue collagen content is reduced.18 Steroids inhibit fibrosis by preventing the migration and activation of inflammatory cells and fibroblasts.19 Based on these steroidal effects, the usefulness of intralesional steroid injection into benign esophageal strictures has been suggested for augmenting the effects of endoscopic dilation.16,17
Because fibroblast proliferation begins 3 to 7 days after wound injury,20 endoscopic steroid injection at 3 days post-ESD would suppress inflammatory cell infiltration and fibrosis effectively. A recent retrospective study demonstrated that endoscopic triamcinolone injection resulted in a decreased stricture incidence and a decreased need for EBD in patients who underwent ESD for superficial esophageal squamous cell carcinomas (Table 2).21 In this study, the proportion of patients developing strictures in the endoscopic triamcinolone injection group was significantly lower than that in the control group (19.0% vs. 75.0%). Furthermore, the mean number of EBD procedures required in the endoscopic triamcinolone injection group was significantly lower than that in the control group (1.7 vs. 6.6). No adverse effects, including delayed perforation or mediastinal abscess, were associated with the injection procedure.
Table 2.
Effect of Steroids in the Prevention of Post-Endoscopic Submucosal Dissection Stricture in Superficial Squamous Cell Neoplasms

The suggested protocol for endoscopic steroid injection is as follows.21 Endoscopic steroid injection begins at 3 days post-ESD, and triamcinolone acetonide (10 mg/mL) is used without further dilution. A 1-mL syringe is usually needed to manually inject triamcinolone and facilitates injection administration with consistent pressure. After shallow insertion of the needle to avoid injuring the proper muscle layer, triamcinolone is injected in aliquots of 0.2 mL into the cauterized ulcer base. Injections are performed equally (1 cm apart) in a semi-circumferential fashion. The number of injections per session depends on the resection size. Sessions are usually conducted at 3, 7, and 10 days post-ESD for a total of three sessions.
However, some esophageal strictures are recalcitrant despite the use of intralesional steroid injection followed by endoscopic dilation.22,23 Moreover, the potential risks for esophageal perforation, pleural effusion, or mediastinitis are associated with local therapy.16 However, this risk seems to increase when steroids are injected directly onto the ulcer bed immediately after esophageal ESD. Hence, further study would be useful to determine the optimal timing and dose for the effective and safe action of triamcinolone.
Oral steroid administration
A recent retrospective study demonstrated that oral prednisolone reduced the need for EBD even after complete circular ESD for superficial esophageal squamous cell carcinomas (Table 2).7 In this study, post-ESD esophageal strictures were observed significantly more frequently in the preemptive EBD group than in the oral prednisolone group (31.8% vs. 5.3%). Additionally, the mean number of EBD sessions required in the oral prednisolone group was significantly lower than that in the control group (1.7 vs. 15.6). Oral prednisolone administration was started at a dose of 30 mg/day on day 3 post-ESD, tapered gradually (30, 30, 25, 25, 20, 15, 10, and 5 mg for 7 days each), and then discontinued after 8 weeks. In the case of oral prednisolone administration, EBD was not performed preemptively, but on demand, whenever patients reported dysphagia.
The mechanisms how systemic prednisolone controls post-ESD stricture and reduces EBD sessions remain unclear. Steroids can not only inhibit collagen synthesis but also enhance collagen breakdown; as a result, stricture formation can be inhibited.16 Furthermore, steroids possess anti-inflammatory properties.18 Because acute esophagitis with fibrosis and abundant inflammatory cell infiltration is found in histological observation of benign strictures,19 systemic steroid administration at an earlier stage (at 3 days post-ESD) can inhibit initial inflammation, which might have an additional impact on stricture prevention.
Nevertheless, steroid treatment may be associated with various adverse effects, including immunosuppression, osteoporosis, diabetes, peptic ulceration, psychiatric disturbances, and optical damage.24 In addition, steroid administration can further increase the risk of esophageal candidiasis, to which patients with stenotic esophageal lesions are already predisposed.16 Recently, several cases of persistent esophageal stricture resistant to intralesional steroid injection were successfully managed with systemic steroid administration.23 Systemic administration could deliver the steroid into the fibrotic tissue of the stricture more effectively compared to endoscopic injection. Therefore, oral prednisolone administration could be a novel, useful option for preventing post-ESD stricture and thus could potentially reduce the need for EBD even after complete circumferential ESD. However, further evaluation in a larger series is clearly needed before this strategy can be widely accepted in clinical settings.
New treatment modalities
Stenting
Temporary stent placement may also be a promising strategy for the prevention of post-ESD strictures. Self-expandable metal stents (SEMSs) or biodegradable stents have been used for the treatment of benign strictures such as anastomotic stricture and cicatricial stricture secondary to esophagitis.25 Although recent studies reported the usefulness of SEMSs for the treatment of benign esophageal stricture,26,27,28 potential late-onset complications are related to long-term stent placement.26,27,28,29,30 Moreover, there is no removal mechanism in currently available SEMSs, which may result in difficult stent removal after long-term placement. Currently, no consensus on the appropriate duration of SEMS placement exists. In previous studies, the duration of SEMS placement varied from 3 days to several months.26,27,28,29 However, no report on SEMS placement for the treatment of post-ESD cicatricial stricture has existed until now. To overcome the difficulty in removing stents, the use of self-expanding Polyflex plastic stents (Willy Ruesch GMBH, Kernen, Germany),25 fully covered retrievable SEMSs,31 or biodegradable stents32,33 has been suggested.
Thus far, the use of self-expandable removable stents for the prevention of post-ESD strictures has not been described. Reportedly, biodegradable stents have been applied for the prevention of post-EMR/ESD strictures; however, high frequencies of stent migration, small numbers of patients, and short-term follow-up periods limit the usefulness of these studies.32,33 Thus, further evaluation of these methods is required to compare the usefulness of these stents with EBD.
Other methods under investigation
In recent years, new technologies such as autologous oral mucosal sheets12 or extracellular matrix scaffold material34 have been suggested to manage esophageal strictures. In previous experiments, effective treatment resulting in re-epithelialization of post-ESD esophageal ulcers was shown by the transplantation of cultured autologous canine oral mucosal epithelial cell sheets,35 noncultured autologous swine oral mucosal epithelial cells,36 and cultured human oral mucosal epithelial cell sheets.37 Recently, re-epithelialization of the esophagus post-ESD in nine patients with superficial esophageal neoplasms was promoted safely and effectively by using sutureless, endoscopic transplantation of carrier-free cell sheets composed of autologous oral mucosal epithelial cells.38 Moreover, local administration of a controlled-release anti-scarring agent can prevent further esophageal stricture development post-ESD. According to a recent publication, 5-fluorouracil, which is used as an anti-scarring agent for the treatment of hypertrophic skin scars, prevented postoperative esophageal strictures in a canine model.39 These methods could be used to prevent stricture formation following ESD and to improve patient quality of life. However, further study will be needed to assess the efficacy and safety of such methods for the prevention of stricture formation.
POST-ESD STRICTURE IN THE STOMACH
Incidence of and risk factors for post-ESD stricture
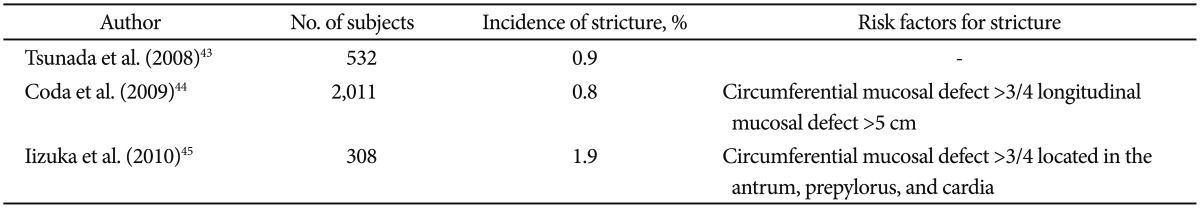
Perforation and bleeding are common complications of ESD in the stomach,40,41 and a case of extensive gastric ischemia post-ESD for early gastric cancer was found in the literature.42 However, reports regarding the development of strictures post-ESD for gastric neoplasm are few in number (Table 3).43,44,45 This scarcity of reports is probably because the incidence of post-ESD strictures in gastric neoplasm is very low (0.8% to 1.9%). Coda et al.44 reported that of the post-ESD stricture cases in the stomach, 17% occurred in the cardia and 7% occurred in the pylorus. Circumferential mucosal defects more than three-fourths in extent and longitudinal mucosal defects >5 cm were considered risk factors of post-ESD stricture. In another study, the incidence of post-ESD stricture in the cardia, antrum, and prepylorus was 4.3%, 2.0%, and 18.8%, respectively.45 No reports have demonstrated post-ESD strictures in the body, angle, or fundus. In this study, ESD of more than three-fourths the circumference in the prepylorus, antrum, and cardia was considered a risk factor for stricture formation.
Table 3.
Incidence of and Risk Factors for Post-Endoscopic Submucosal Dissection Stricture in Gastric Neoplasms
Treatment modalities for post-ESD stricture
Endoscopic balloon dilation
Balloon dilation is considered to be useful for the treatment of post-ESD stricture. Coda et al.44 reported that stricture-related symptoms were completely resolved in all patients as a result of EBD. The median number of dilations in patients with post-ESD strictures following cardiac and pyloric resections was 5 and 9, respectively. The median period from ESD to the diagnosis of post-ESD stricture was 22 days in cases of cardiac resection and 27 days in cases of pyloric resection. There were no complications after any of the balloon dilations. The authors indicated that it was advisable to start balloon dilation before the stricture actually developed.
In a case series of five patients with post-ESD stricture, one patient required surgery because of a severe stricture that could not be resolved by balloon dilation, and two patients required emergency surgery because of perforations caused by balloon dilation.43 This case series stressed the importance of starting the dilation in the early stage of the healing process post-ESD.
In another report on six cases of symptomatic strictures, EBD was successful and all patients experienced relief from stricture symptoms.45 One case was complicated by perforation, although the patient recovered following conservative treatment. The number of balloon dilations was 1 to 7 (average, 2.8), and the duration between relief from stricture symptoms and the initial dilation ranged from 1 to 5 months (average, 2.5).
Local steroid injection
Several studies recommended the use of oral steroids or endoscopic steroid injections in cases of post-ESD esophageal strictures.7,16,17,19,21,22,23 In a previous study, the presence of granulation tissue over the ulcer floor led to contraction and deformity of the ulcer.46 During the healing process of post-ESD gastric ulcers, ulcer granulation and contraction as well as regenerative mucosa extension toward the center of the ulcer led to protruded granulation tissue formation. Steroids can modulate the process of wound healing in a post-ESD ulcer through their anti-inflammatory effects. The local injection of steroids into the post-ESD ulcer promotes the formation of flat and abundant granulation tissue without fibrotic contraction. Consequently, the formation of granulation tissue prevents convergence around the ulcer edge toward the center, thus avoiding gastric deformity.
A recent study suggested that local injection of triamcinolone into the artificial ulcer may prevent post-ESD gastric deformity.47 At 5 and 12 days post-ESD, triamcinolone was injected in sites 5 mm apart in three straight lines, which quadrisected the post-ESD ulcer across its maximum diameter. Measurements of clip-to-clip distance and ulcer diameter were recorded at 5, 12, 30, and 60 days post-ESD. The total doses of triamcinolone per session ranged from 40 to 72 mg. Local triamcinolone injection did not alter the clip-to-clip distance at 60 days post-ESD, and flat granulation tissue formation over the ulcer was followed by regenerative mucosa formation without any gastric deformity. No patient experienced triamcinolone injection-associated complications. The local injection of triamcinolone into a post-ESD ulcer promotes granulation tissue formation at an early stage of the healing process, thus leading to gastric mucosa regeneration without mucosal convergence or gastric deformity.
New treatment modalities
A recent report described the use of a biodegradable esophageal stent in patients with post-ESD esophageal strictures, which may be beneficial in preventing post-ESD strictures in patients with cardiac or pyloric resections.35 Temporary insertion of the removable stent could be another treatment modality if dilation is not effective.
CONCLUSIONS
The incidence of post-ESD strictures in esophageal neoplasms is 5% to 17%. In the esophagus, circumferential mucosal defects of more than three-fourths the esophageal circumference, longitudinal mucosal defects >3 cm, and lesions located in the upper esophagus are risk factors for stricture development. Thus far, EBD has been the treatment of choice for esophageal strictures. However, intralesional steroid injection or oral steroid administration has been reported to promote remission of dysphagia or reduce the need for repeated EBD. The incidence of post-ESD strictures in gastric neoplasm is 0.8% to 1.9%. In the stomach, circumferential mucosal defects of more than three-fourths in extent and longitudinal mucosal defects >5 cm are risk factors for post-ESD stricture. Although local steroid injection can also be helpful in preventing and treating post-ESD strictures in the stomach, early EBD has proven effective for their control and prevention. Furthermore, temporary stent placement may also be a promising strategy for preventing post-ESD stricture in the upper gastrointestinal tract.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Yoshida T, Inoue H, Usui S, Satodate H, Fukami N, Kudo SE. Narrow-band imaging system with magnifying endoscopy for superficial esophageal lesions. Gastrointest Endosc. 2004;59:288–295. doi: 10.1016/s0016-5107(03)02532-x. [DOI] [PubMed] [Google Scholar]
- 2.Fujishiro M. Perspective on the practical indications of endoscopic submucosal dissection of gastrointestinal neoplasms. World J Gastroenterol. 2008;14:4289–4295. doi: 10.3748/wjg.14.4289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fujishiro M, Yahagi N, Kakushima N, Kodashima S, Ichinose M, Omata M. En bloc resection of a large semicircular esophageal cancer by endoscopic submucosal dissection. Surg Laparosc Endosc Percutan Tech. 2006;16:237–241. doi: 10.1097/00129689-200608000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Katada C, Muto M, Manabe T, Boku N, Ohtsu A, Yoshida S. Esophageal stenosis after endoscopic mucosal resection of superficial esophageal lesions. Gastrointest Endosc. 2003;57:165–169. doi: 10.1067/mge.2003.73. [DOI] [PubMed] [Google Scholar]
- 5.Ono S, Fujishiro M, Niimi K, et al. Predictors of postoperative stricture after esophageal endoscopic submucosal dissection for superficial squamous cell neoplasms. Endoscopy. 2009;41:661–665. doi: 10.1055/s-0029-1214867. [DOI] [PubMed] [Google Scholar]
- 6.Ezoe Y, Muto M, Horimatsu T, et al. Efficacy of preventive endoscopic balloon dilation for esophageal stricture after endoscopic resection. J Clin Gastroenterol. 2011;45:222–227. doi: 10.1097/MCG.0b013e3181f39f4e. [DOI] [PubMed] [Google Scholar]
- 7.Yamaguchi N, Isomoto H, Nakayama T, et al. Usefulness of oral prednisolone in the treatment of esophageal stricture after endoscopic submucosal dissection for superficial esophageal squamous cell carcinoma. Gastrointest Endosc. 2011;73:1115–1121. doi: 10.1016/j.gie.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 8.Ono S, Fujishiro M, Niimi K, et al. Long-term outcomes of endoscopic submucosal dissection for superficial esophageal squamous cell neoplasms. Gastrointest Endosc. 2009;70:860–866. doi: 10.1016/j.gie.2009.04.044. [DOI] [PubMed] [Google Scholar]
- 9.Takahashi H, Arimura Y, Okahara S, et al. Risk of perforation during dilation for esophageal strictures after endoscopic resection in patients with early squamous cell carcinoma. Endoscopy. 2011;43:184–189. doi: 10.1055/s-0030-1256109. [DOI] [PubMed] [Google Scholar]
- 10.Mizuta H, Nishimori I, Kuratani Y, Higashidani Y, Kohsaki T, Onishi S. Predictive factors for esophageal stenosis after endoscopic submucosal dissection for superficial esophageal cancer. Dis Esophagus. 2009;22:626–631. doi: 10.1111/j.1442-2050.2009.00954.x. [DOI] [PubMed] [Google Scholar]
- 11.Repici A, Hassan C, Carlino A, et al. Endoscopic submucosal dissection in patients with early esophageal squamous cell carcinoma: results from a prospective Western series. Gastrointest Endosc. 2010;71:715–721. doi: 10.1016/j.gie.2009.11.020. [DOI] [PubMed] [Google Scholar]
- 12.Fujishiro M, Yahagi N, Kakushima N, et al. Endoscopic submucosal dissection of esophageal squamous cell neoplasms. Clin Gastroenterol Hepatol. 2006;4:688–694. doi: 10.1016/j.cgh.2006.03.024. [DOI] [PubMed] [Google Scholar]
- 13.Isomoto H, Yamaguchi N, Nakayama T, et al. Management of esophageal stricture after complete circular endoscopic submucosal dissection for superficial esophageal squamous cell carcinoma. BMC Gastroenterol. 2011;11:46. doi: 10.1186/1471-230X-11-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oyama T, Tomori A, Hotta K, et al. Endoscopic submucosal dissection of early esophageal cancer. Clin Gastroenterol Hepatol. 2005;3(7 Suppl 1):S67–S70. doi: 10.1016/s1542-3565(05)00291-0. [DOI] [PubMed] [Google Scholar]
- 15.Silvis SE, Nebel O, Rogers G, Sugawa C, Mandelstam P. Endoscopic complications. Results of the 1974 American Society for Gastrointestinal Endoscopy Survey. JAMA. 1976;235:928–930. doi: 10.1001/jama.235.9.928. [DOI] [PubMed] [Google Scholar]
- 16.Kochhar R, Makharia GK. Usefulness of intralesional triamcinolone in treatment of benign esophageal strictures. Gastrointest Endosc. 2002;56:829–834. doi: 10.1067/mge.2002.129871. [DOI] [PubMed] [Google Scholar]
- 17.Lee M, Kubik CM, Polhamus CD, Brady CE, 3rd, Kadakia SC. Preliminary experience with endoscopic intralesional steroid injection therapy for refractory upper gastrointestinal strictures. Gastrointest Endosc. 1995;41:598–601. doi: 10.1016/s0016-5107(95)70199-0. [DOI] [PubMed] [Google Scholar]
- 18.Carrico TJ, Mehrhof AI, Jr, Cohen IK. Biology of wound healing. Surg Clin North Am. 1984;64:721–733. doi: 10.1016/s0039-6109(16)43388-8. [DOI] [PubMed] [Google Scholar]
- 19.Miyashita M, Onda M, Okawa K, et al. Endoscopic dexamethasone injection following balloon dilatation of anastomotic stricture after esophagogastrostomy. Am J Surg. 1997;174:442–444. doi: 10.1016/s0002-9610(97)00116-5. [DOI] [PubMed] [Google Scholar]
- 20.Werner S, Grose R. Regulation of wound healing by growth factors and cytokines. Physiol Rev. 2003;83:835–870. doi: 10.1152/physrev.2003.83.3.835. [DOI] [PubMed] [Google Scholar]
- 21.Hashimoto S, Kobayashi M, Takeuchi M, Sato Y, Narisawa R, Aoyagi Y. The efficacy of endoscopic triamcinolone injection for the prevention of esophageal stricture after endoscopic submucosal dissection. Gastrointest Endosc. 2011;74:1389–1393. doi: 10.1016/j.gie.2011.07.070. [DOI] [PubMed] [Google Scholar]
- 22.Hishiki T, Kouchi K, Saito T, et al. Successful treatment of severe refractory anastomotic stricture in an infant after esophageal atresia repair by endoscopic balloon dilation combined with systemic administration of dexamethasone. Pediatr Surg Int. 2009;25:531–533. doi: 10.1007/s00383-009-2367-1. [DOI] [PubMed] [Google Scholar]
- 23.Morikawa N, Honna T, Kuroda T, et al. High dose intravenous methylprednisolone resolves esophageal stricture resistant to balloon dilatation with intralesional injection of dexamethasone. Pediatr Surg Int. 2008;24:1161–1164. doi: 10.1007/s00383-008-2224-7. [DOI] [PubMed] [Google Scholar]
- 24.Melillo N, Corrado A, Quarta L, Cantatore FP. Corticosteroids, a review. Panminerva Med. 2007;49:29–33. [PubMed] [Google Scholar]
- 25.Karbowski M, Schembre D, Kozarek R, Ayub K, Low D. Polyflex self-expanding, removable plastic stents: assessment of treatment efficacy and safety in a variety of benign and malignant conditions of the esophagus. Surg Endosc. 2008;22:1326–1333. doi: 10.1007/s00464-007-9644-7. [DOI] [PubMed] [Google Scholar]
- 26.Wadhwa RP, Kozarek RA, France RE, et al. Use of self-expandable metallic stents in benign GI diseases. Gastrointest Endosc. 2003;58:207–212. doi: 10.1067/mge.2003.343. [DOI] [PubMed] [Google Scholar]
- 27.Song HY, Park SI, Do YS, et al. Expandable metallic stent placement in patients with benign esophageal strictures: results of long-term follow-up. Radiology. 1997;203:131–136. doi: 10.1148/radiology.203.1.9122381. [DOI] [PubMed] [Google Scholar]
- 28.Kim JH, Song HY, Choi EK, Kim KR, Shin JH, Lim JO. Temporary metallic stent placement in the treatment of refractory benign esophageal strictures: results and factors associated with outcome in 55 patients. Eur Radiol. 2009;19:384–390. doi: 10.1007/s00330-008-1151-2. [DOI] [PubMed] [Google Scholar]
- 29.Low DE, Kozarek RA. Removal of esophageal expandable metal stents: description of technique and review of potential applications. Surg Endosc. 2003;17:990–996. doi: 10.1007/s00464-002-8528-0. [DOI] [PubMed] [Google Scholar]
- 30.Sandha GS, Marcon NE. Expandable metal stents for benign esophageal obstruction. Gastrointest Endosc Clin N Am. 1999;9:437–446. [PubMed] [Google Scholar]
- 31.Eloubeidi MA, Lopes TL. Novel removable internally fully covered self-expanding metal esophageal stent: feasibility, technique of removal, and tissue response in humans. Am J Gastroenterol. 2009;104:1374–1381. doi: 10.1038/ajg.2009.133. [DOI] [PubMed] [Google Scholar]
- 32.Nieponice A, McGrath K, Qureshi I, et al. An extracellular matrix scaffold for esophageal stricture prevention after circumferential EMR. Gastrointest Endosc. 2009;69:289–296. doi: 10.1016/j.gie.2008.04.022. [DOI] [PubMed] [Google Scholar]
- 33.Ohki T, Yamato M, Murakami D, et al. Treatment of oesophageal ulcerations using endoscopic transplantation of tissue-engineered autologous oral mucosal epithelial cell sheets in a canine model. Gut. 2006;55:1704–1710. doi: 10.1136/gut.2005.088518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Saito Y, Tanaka T, Andoh A, et al. Usefulness of biodegradable stents constructed of poly-l-lactic acid monofilaments in patients with benign esophageal stenosis. World J Gastroenterol. 2007;13:3977–3980. doi: 10.3748/wjg.v13.i29.3977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Saito Y, Tanaka T, Andoh A, et al. Novel biodegradable stents for benign esophageal strictures following endoscopic submucosal dissection. Dig Dis Sci. 2008;53:330–333. doi: 10.1007/s10620-007-9873-6. [DOI] [PubMed] [Google Scholar]
- 36.Sakurai T, Miyazaki S, Miyata G, Satomi S, Hori Y. Autologous buccal keratinocyte implantation for the prevention of stenosis after EMR of the esophagus. Gastrointest Endosc. 2007;66:167–173. doi: 10.1016/j.gie.2006.12.062. [DOI] [PubMed] [Google Scholar]
- 37.Takagi R, Murakami D, Kondo M, et al. Fabrication of human oral mucosal epithelial cell sheets for treatment of esophageal ulceration by endoscopic submucosal dissection. Gastrointest Endosc. 2010;72:1253–1259. doi: 10.1016/j.gie.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 38.Ohki T, Yamato M, Ota M, et al. Prevention of esophageal stricture after endoscopic submucosal dissection using tissue-engineered cell sheets. Gastroenterology. 2012;143:582–588. doi: 10.1053/j.gastro.2012.04.050. [DOI] [PubMed] [Google Scholar]
- 39.Mizutani T, Tadauchi A, Arinobe M, et al. Novel strategy for prevention of esophageal stricture after endoscopic surgery. Hepatogastroenterology. 2010;57:1150–1156. [PubMed] [Google Scholar]
- 40.Adachi Y, Shiraishi N, Kitano S. Modern treatment of early gastric cancer: review of the Japanese experience. Dig Surg. 2002;19:333–339. doi: 10.1159/000065829. [DOI] [PubMed] [Google Scholar]
- 41.Fujishiro M. Endoscopic submucosal dissection for stomach neoplasms. World J Gastroenterol. 2006;12:5108–5112. doi: 10.3748/wjg.v12.i32.5108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Probst A, Maerkl B, Bittinger M, Messmann H. Gastric ischemia following endoscopic submucosal dissection of early gastric cancer. Gastric Cancer. 2010;13:58–61. doi: 10.1007/s10120-009-0539-2. [DOI] [PubMed] [Google Scholar]
- 43.Tsunada S, Ogata S, Mannen K, et al. Case series of endoscopic balloon dilation to treat a stricture caused by circumferential resection of the gastric antrum by endoscopic submucosal dissection. Gastrointest Endosc. 2008;67:979–983. doi: 10.1016/j.gie.2007.12.023. [DOI] [PubMed] [Google Scholar]
- 44.Coda S, Oda I, Gotoda T, Yokoi C, Kikuchi T, Ono H. Risk factors for cardiac and pyloric stenosis after endoscopic submucosal dissection, and efficacy of endoscopic balloon dilation treatment. Endoscopy. 2009;41:421–426. doi: 10.1055/s-0029-1214642. [DOI] [PubMed] [Google Scholar]
- 45.Iizuka H, Kakizaki S, Sohara N, et al. Stricture after endoscopic submucosal dissection for early gastric cancers and adenomas. Dig Endosc. 2010;22:282–288. doi: 10.1111/j.1443-1661.2010.01008.x. [DOI] [PubMed] [Google Scholar]
- 46.Kakushima N, Yahagi N, Fujishiro M, et al. The healing process of gastric artificial ulcers after endoscopic submucosal dissection. Dig Endosc. 2004;16:327–331. [Google Scholar]
- 47.Mori H, Rafiq K, Kobara H, et al. Local steroid injection into the artificial ulcer created by endoscopic submucosal dissection for gastric cancer: prevention of gastric deformity. Endoscopy. 2012;44:641–648. doi: 10.1055/s-0032-1309815. [DOI] [PubMed] [Google Scholar]


