The incidence of gestational diabetes mellitus (GDM) has more than doubled in the past decade1 and affects at least 7% of all pregnancies, or 200,000 women per year in the US.2,3 GDM is the most common complication of pregnancy, with incidence paralleling that of type 2 diabetes (T2DM) prevalence in the general population.4 Women with previous gestational diabetes (pGDM) are at elevated risk for cardiovascular disease5 and have a seven-fold increased chance of developing T2DM,6 most commonly within five years following delivery.7 Despite intensive dietary counseling8 for women with GDM during pregnancy, there is poor adherence to general dietary recommendations following delivery. Fruit and vegetable consumption is low in this population,9 with only 5% consuming at least five servings per day of fruit or vegetables.10
Intensive lifestyle interventions with a combined focus on diet and physical activity aimed at moderate weight loss resulted in a 53% reduction in T2DM risk among the cohort of women with pGDM in the Diabetes Prevention Program trial.11 Furthermore, more recent studies have shown that adherence to healthy dietary patterns alone provides protection for T2DM risk in the pGDM population.12,13 Protection was most considerable through the pattern characterized by the Alternate Healthy Eating Index (AHEI) demonstrating a 57% lower T2DM risk.12
The AHEI dietary index, created in 2002, evolved from the Healthy Eating Index as an alternative dietary index to better predict chronic disease risk.14 In addition to the T2DM risk reduction associated with AHEI adherence in women with pGDM, the AHEI dietary pattern has been associated with decreased risk for diabetes,12,15 lower risk for cardiovascular disease,16 cancer,17 and the reversal of metabolic syndrome in other populations.18 Identifying the factors that can be modified to improve adherence to the AHEI dietary pattern is an important next step in mitigating risk reduction. Few studies have examined intrapersonal influences of diet quality in the pGDM population and no study to date has specifically examined the variables that may contribute to greater concordance with the AHEI dietary pattern. The purpose of this study was to examine the association between the intrapersonal factors of socio-demographics, depressive symptoms, perceptions of T2DM risk, benefits and barriers to healthy eating, and self-efficacy with AHEI diet quality in women within five years of a GDM pregnancy.
Theoretical Framework
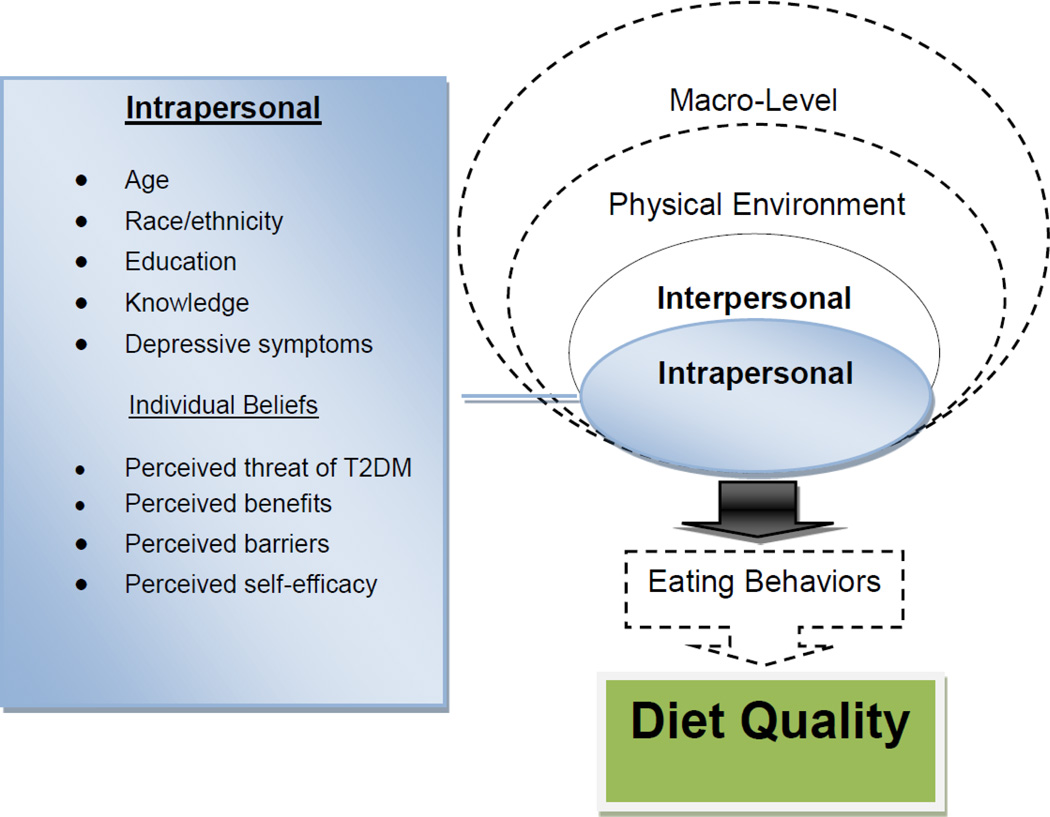
There are multiple determinants that influence eating behavior and the quality of dietary patterns. The determinants can be categorized within contexts of intrapersonal, interpersonal, and environmental factors.19 Although this study focused on the intrapersonal determinants, the investigators recognized the multiple contexts that influence dietary behavior and incorporated the ecological model of eating behavior by Story and colleagues19 to frame the singular intrapersonal contextual focus. The variables examined in this study were specifically guided by the Health Belief Model to understand the intrapersonal factors of perceived threat of T2DM, benefits and barriers to healthy eating, and self-efficacy with AHEI diet quality (Figure 1).
Figure 1. Intrapersonal Influences of Diet Quality in Women with pGDM.
Note. The Ecological Framework for Eating Influences was adapted from Story et al. (2008) and combined with the Health Belief Model. This study is limited in focus to assessing specific intrapersonal factors as depicted in the colored boxes in this figure. Individual beliefs reflect the perceptions as defined by the Health Belief Model for eating behavior in relation to T2DM development. Adapted and republished with permission, from the Annual Review of Public Health, Volume 29 © 2008 by Annual Reviews www.annualreviews.org.
Individual influences on healthy eating have been widely studied among many populations and multiple intrapersonal factors have been associated with diet quality. As depicted in Story et al.’s ecological framework of the multiple influences of eating behavior, the intrapersonal influences include cognitions, skills and behavior, lifestyle, biological, and demographics.19 Socio-demographic factors influence diet quality, with most studies concluding that increased age, higher education, higher income, and non-minority race/ethnicity are associated with higher diet quality.20–22 Knowledge and self-efficacy are important predictors of diet quality with post-partum and in women with pGDM.10,21,23 Depression has also been associated with lower diet quality,24 with some recent studies suggesting that poor diet quality may predict depressive symptoms, especially in women of childbearing age.25,26
The investigators of this study hypothesized that women with pGDM who had higher perceptions of the threat of T2DM, along with greater perceived self-efficacy and benefits of healthy eating, and lower perceptions of healthy eating barriers would have higher AHEI diet quality, controlling for socio-demographics, dietary knowledge and depressive symptoms.
Methods
Study Design, Setting, and Participants
This was a cross-sectional, descriptive, quantitative study conducted from August 2011 through December 2012. Participants were recruited from the community and through women’s health clinics of an academic health center, an inner-city public hospital, and a public health department. Eligible participants were women who were (a) within 5 years of a GDM pregnancy, (b) aged 18–45 years, (c) fluent in English or Spanish, (d) with no history of polycystic ovary syndrome and no development of T2DM, (e) not currently pregnant or breastfeeding, (f) not following a prescriptive or weight-loss diet, and (g) no more than moderate depressive symptoms (score of ≥ 20 on the Patient Health Questionnaire-9). The study protocol was approved by the university institutional review board and by the clinic sites where recruitment occurred.
Measurements
Participants completed the Block 110-item semi-quantitative food frequency questionnaire (FFQ) to assess usual dietary intake in the past year. The Block FFQ has been validated among other major FFQ’s and has been found to be comparable.27 Reliability and validity have been demonstrated in populations of women.28 Nutrition Quest (Berkeley, CA) provided the FFQ analysis for specific daily nutrient intake and daily food servings and the investigators scored the dietary data into the AHEI. AHEI is scores range from 2.5–87.5, with greater concordance (better diet quality) reflected in higher scores. Eight of the nine AHEI components are scored from 0 (recommendations were not met) to 10 (recommendations were met fully), with intermediate intakes scored proportionately between 0 and 10. The final component of multivitamin use is scored dichotomously as 2.5 points for no use and 7.5 points for use.14
Demographics and basic, pertinent medical history were collected on a form designed for this study and included age, race/ethnicity, education, income, delivery date of most recent GDM pregnancy, and current medications.
Perceived threat of type 2 diabetes (T2DM) was assessed with a 23-item questionnaire incorporating three subscales (Personal Control, Optimistic Bias, Knowledge, and an additional seven items addressing risk perception and lifestyle behaviors) of the Risk Perception Survey for Developing Diabetes (RPS-DD), developed for the Diabetes Prevention Program trial29 and adapted for women with pGDM.30 For all subscales, higher scores are equivalent to higher levels of that component. Beliefs about the benefits of diet and exercise and individual risk perception with an additional seven items on the RPS-DD were assessed, replicating the assessment of risk perception in women with pGDM as conducted by Kim and colleagues.30
Perceived benefits of healthy eating was assessed with a 9-item, 5-point Likert instrument designed specifically for this study. At the time that this study was being designed, there were no published instruments that examined the concept of healthy eating benefits, especially in a population at risk for cardiometabolic diseases. Content validity of the scale was established with an expert review panel and then pilot-tested in a convenience sample (n = 91) of adults who had any cardiometabolic risk factor. Items address benefits such as healthy eating: “can help prevent diabetes,” “can help control my weight,” and “can help me feel better.” Scores range from 9 – 45, with higher score indicating greater perceived benefits. Cronbach’s alpha coefficient in the unpublished pilot study was acceptable at .88 and in this sample was .92.
Perceived barriers of healthy eating was assessed with the Barriers to Healthy Eating Scale (BHES), a 16-item scale originally developed to assess healthy eating barriers in pregnant women.31 It addresses areas related to unavailability of food, expense, inconvenience, preferences and inability to engage in healthy eating. Higher scores indicate greater perceived barriers to healthy eating. The 16-item Cardiac Diet Self-Efficacy Scale was used to measure self-efficacy related to healthy eating. It is a general nutrition self-efficacy scale addressing healthy dietary behavior.32
Knowledge and depressive symptoms are known to influence dietary quality, especially in women of child-bearing age.21,26 Dietary knowledge was assessed with an 11-item questionnaire (10 knowledge questions and 1 Likert questions for perceived level of dietary knowledge) to assess awareness of the 2010 Dietary Guidelines for Americans. This instrument was adapted from a survey designed to test knowledge of the 2005 Dietary Guidelines for Americans from a study with community health advisors.33 For this study, an adapted and updated version of the questionnaire to reflect the 2010 guidelines specifically for women aged 18–45 was used.34 The knowledge questions are each 4-item multiple choice items, which test the participants’ understanding of recommended daily calories, daily servings of grain, fruits and vegetables, dairy, protein, fiber, sodium, and amount and types of fat. Knowledge of diabetes risk factors was assessed with the knowledge subscale of the RPS-DD.
Depressive symptoms were assessed with the Patient Health Questionnaire-9 (PHQ-9), a 9-item scale that was designed to be a brief assessment of depressive symptoms. It has been tested in multiple samples, including women of childbearing age35 and deemed a reliable and valid measure of depression severity. Scores range from 0–27, with higher scores indicating greater depressive symptoms.
Procedures
Upon receiving a study letter of invitation or seeing/hearing an advertisement, interested women contacted the lead researcher or bilingual research assistant by email or telephone. The study was fully explained, initial verbal telephone consent completed, and eligibility criteria determined. English-speaking women who chose to enroll were mailed the questionnaire packet. Enrolled Spanish-speaking women completed questionnaires in an interview format with the bilingual research assistant. The research staff met participants in the setting chosen by the participant, usually the home or workplace. Questionnaire completion time ranged from 1 to 2 hours. Participants were compensated with a $25 gift card and presented with individualized cardiometabolic health and nutrition education materials for their participation in the study.
Data Analyses
Data were analyzed with IBM SPSS version 20.0.36 Descriptive statistics were used to review sample characteristics and check underlying distribution assumptions. Race and ethnicity data were dichotomized into categories of non-Hispanic Caucasian women (n = 34) and Minority women (n = 41). The Minority group consisted of 24 African-American, 11 Hispanic, 2 Asian, and 4 multiracial/ethnic women. Bivariate correlation analyses were used to determine significant associations (P ≤ .05) between the contributing and independent variables with diet quality. Mean differences in diet quality were examined with two sample t-tests by race, education status, and level of risk perception. Multiple linear regression modeling was used to examine the contribution of the independent and contributing variables to the variance in diet quality. The control variables of age, race, dietary knowledge, educational attainment, and depressive symptoms were held constant in the model testing, with each of the independent variables added to the model to be examined for contribution and significance in predicting diet quality. Each independent variable was individually tested in regression models regardless of bivariate analysis significance. Independent variables that did not remain significant (P > .05) were excluded from the final model.
Results
The sample included 75 women (45% Caucasian, 55% Minority - 32% African-American, 15% Hispanic), with a mean age of 35.5 years (SD = 5.5), who were 2.6 years (SD = 1.6) since their last GDM delivery, and a mean parity of 2.7 (SD = 2.1). Most were married (73%). More than half (58%) had a Bachelor’s degree or higher and 52% were employed full-time. During their pregnancy, the majority of women (63%) were managed with lifestyle interventions while 24% were also treated with insulin (Table 1).
Table 1.
Characteristics of the Sample (N = 75)
| Characteristic | Study Sample |
|---|---|
| Age, mean years (SD) | 35.5 (5.5) |
| Race/Ethnicity, % | |
| Non-Hispanic Caucasian | 45.0 |
| Minority | 55.0 |
| African-American | 32.0 |
| Hispanic | 15.0 |
| Asian | 3.0 |
| Multiracial | 5.0 |
| Education, % | |
| < 4 years college | 41.3 |
| ≥ Bachelor’s degree | 58.7 |
| Marital status, % | |
| Married | 73.3 |
| Employment Status, % | |
| Unemployed | 33.0 |
| Part-time employed | 16.0 |
| Full-time employed | 51.0 |
| Family History of T2DM, % | 35.0 |
| Family History of CVD, % | 64.0 |
| Current Smoker, % | 12.0 |
| Time since last GDM pregnancy, mean years (SD) | 2.6 (1.6) |
| Parity, mean (SD) | 2.7 (2.1) |
| GDM Pregnancy Treatment, % | |
| Lifestyle | 63.0 |
| Oral Medication | 13.0 |
| Insulin | 24.0 |
Note. T2DM = type 2 diabetes mellitus; CVD = cardiovascular disease; GDM = gestational diabetes mellitus
AHEI scores indicated an average level of diet quality (mean = 47.6, SD = 14.3), with a range of scores from 20.5 – 77.5. No participant fully met the AHEI recommendations. The dietary components with the poorest scores included alcohol consumption and red to white meat ratio, indicating that most women were consuming less than the suggested moderate alcohol intake per day of 0.5 – 1.5 servings per day and that red meat intake was higher than consumption of poultry and fish (Table 2).
Table 2.
Alternate Healthy Eating Index (AHEI) scoring method and total scores
| Component | Criteria for Minimum Scorea |
Criteria for Maximum Scorea |
Participant AHEI scores, mean points (SD) |
|---|---|---|---|
| Vegetables (servings/day) | 0 | 5 | 5.41 (2.84) |
| Fruit (servings/day) | 0 | 4 | 4.96 (2.38) |
| Nuts and soy protein (servings/day) | 0 | 1 | 6.00 (4.93) |
| Ratio of white to red meat | 0 | 4 | 2.44 (2.57) |
| Cereal fiber (grams/day) | 0 | 15 | 8.08 (2.74) |
| trans Fat (% of energy) | ≥4 | ≤0.5 | 7.49 (1.19) |
| Polyunsaturated to Saturated Fat ratio | ≤0.1 | ≥1.0 | 7.29 (1.83) |
| Duration of multivitamin useb | <5 years | ≥5 years | 3.77 (2.19) |
| Alcohol (servings/day) | 0 or >2.5 | 0.5 – 1.5 | 2.13 (3.95) |
| Total Score | 2.5 | 87.5 | 47.58 (14.25) |
Note.
Intermediate intakes were scored proportionately between 0 and 10.
Minimum score is 2.5 and maximum score is 7.5.
Half of the participants (49%) believed that they had a moderate to high chance of developing diabetes in the next ten years, while the other half perceived their risk to be none or slight. There was no difference in diet quality between those with none/slight perception and those with moderate/high (t = −0.23, P = .82). Nearly everyone (97%) believed that regular exercise and diet may prevent T2DM development. While 83% believed that doing regular exercise and following a diet required a lot of effort, 81% also believed that the benefits outweighed the effort of doing it. Participants reported a high level of personal control for preventing diabetes (mean = 3.2, SD = 0.5), and a moderate amount of worry about future T2DM development (mean = 2.7, SD = 0.8). Participants, on average, did not feel that they were any more or less susceptible to the development T2DM or other serious disease compared to other women, with a mean Optimistic Bias score of 2.1 (SD = 0.7).
Barriers to healthy eating were low (mean = 27.3, SD = 6.5), with items related to distance greater than two miles for food and fresh fruits/vegetables as the more commonly reported barriers. Participants also reported a high level of perceived benefit to healthy eating (mean = 42.2, SD = 3.1), and had relatively high levels of dietary self-efficacy (mean = 21.9, SD = 12.7).
Despite a high level of education among participants, knowledge of dietary guidelines was rather poor, with an average test score of 42.2% (SD = 24.6). While 89% of the participants recognized that having had GDM increased risk for T2DM, overall risk knowledge was moderate with a mean test score of 60.7% (SD = 18.4). Most participants reported minimal depressive symptoms (68%), with scores ranging from 0 – 15 (mean = 4.1, SD = 4.1).
Bivariate associations were examined between diet quality, demographics, dietary knowledge, depressive symptoms, and perceived beliefs. Non-Hispanic Caucasian race, higher levels of education, and higher self-efficacy were all significantly associated with higher levels of diet quality (Table 4).
Table 4.
Summary of Bivariate Associations with AHEI Diet Quality
| Variable | Correlation Association |
Two-sample T- test |
|---|---|---|
| Age | .18 | |
| Minority versus Non-Hispanic Caucasian | −2.41* | |
| Education (<Bachelor’s degree versus ≥ Bachelors) | −5.00** | |
| Depressive Symptoms (PHQ-9) | −.10 | |
| Dietary Knowledge | .21 | |
| Threat of T2DM | ||
| Personal Control | .17 | |
| Worry | .00 | |
| Optimistic Bias | .16 | |
| Risk Knowledge | .22 | |
| 10-year Risk (No/slight chance versus Moderate/High chance) | −.23 | |
| Perceived dietary benefits | .20 | |
| Perceived dietary barriers | −.18 | |
| Dietary Self-Efficacy | .33** |
Note.
P < .05;
P < .001.
PHQ-9 = Patient Health Questionnaire; T2DM = type 2 diabetes.
Non-Hispanic Caucasian women had higher AHEI scores compared to Minority women (t = −2.4, P = .02). The greatest mean difference in diet quality was between women with a Bachelor’s degree or higher, compared to those who did not complete college (t = −5.0, P = < .0001), with a mean AHEI score difference of 14.5 points.
Each of the seven independent variables (Personal Control, Worry, Optimistic Bias subscale scores, Diabetes Risk Knowledge score, perceived benefit score, perceived barrier score and dietary self-efficacy score) were entered individually into a multiple regression model with all four control variables (race, education status, depressive symptoms and dietary knowledge). Personal Control, Worry, Optimistic Bias, Diabetes Risk Knowledge, perceived benefits and barriers did not contribute to variance in diet quality. Controlling for all other variables, only higher levels self-efficacy significantly predicted better AHEI diet concordance (R2 = .36, F(6, 66) = 6.19, P = <.0001). The final model with education status and self-efficacy as significant predictors, explained 36% of the variance in diet quality. The parameter estimates of the predictors in the regression model further suggest that education status was the strongest predictor of AHEI diet quality (Table 5).
Table 5.
Multiple Linear Regression Analysis Summary for Intrapersonal Variables and AHEI Diet Quality
| Variable | B | SE B | β | t | P |
|---|---|---|---|---|---|
| Age | −0.23 | 0.28 | −.09 | −0.82 | .41 |
| Non-Hispanic Caucasian Race | 3.93 | 3.31 | .14 | 1.19 | .24 |
| Education Status | 3.51 | 0.89 | .08 | 3.18 | <.001 |
| Depressive Symptoms | 0.28 | 0.36 | .51 | 0.76 | .45 |
| Dietary Knowledge | −0.08 | 0.07 | −.13 | −1.05 | .30 |
| Dietary Self Efficacy | 0.37 | 0.12 | .33 | 3.18 | 002 |
Note. R2 = .36, F (6, 66) = 6.19, P = <.0001
Implications
Diet quality in this sample of women with pGDM was moderate, with a substantial opportunity to improve intake to be consistent with protective diets such as the AHEI. Inadequate diet quality in the pGDM population has been reported previously,9,10 with one other study examining AHEI dietary concordance in pGDM women.12 The increasingly beneficial T2DM risk reduction demonstrated along the continuum of AHEI scores by Tobias and colleagues (2012) suggests the significant need to improve diet quality in women with pGDM. Identifying the important factors that predict diet quality is an important next step in designing diet improvement interventions. The findings of this study highlight the importance of educational attainment and dietary self-efficacy in promoting better diet quality, supporting components of the study hypotheses. However, neither the perceptions of T2DM threat, nor the perceptions of healthy eating benefits and barriers contributed to the variance in diet quality in this sample. The finding that risk perception is not a significant predictor of diet quality supports previous findings in women with pGDM.30
Higher levels of education were demonstrated in this study to be predictive of higher diet quality, which likely contributes to overall better dietary and disease risk/health promotion knowledge.37 In a recent study specifically examining women with pGDM, higher levels of education were associated with better adherence to dietary recommendations.38 In this sample, education levels were highly correlated with T2DM risk knowledge (Spearman’s rho = .42, p = <.0001) and dietary knowledge (Spearman’s rho = .52, p = <.0001). Although education level may not be a modifiable factor easily addressed in adult populations, diabetes risk knowledge and dietary knowledge can certainly be improved through education interventions. Improving health knowledge and health literacy at levels appropriate for individual educational attainment has been demonstrated to improve health behavior.39 Enhancing diabetes and diet specific knowledge and health literacy may be an important component in designing multi-strategy dietary interventions for pGDM women.40,41
Discussion
This study’s finding regarding the influence of dietary self-efficacy with diet quality supports previous findings in the pGDM population10 and in general adult populations.42 These findings are promising for designing nutritional interventions, since self-efficacy can be modified to improve diet quality.43 Intervention studies that have specifically developed dietary self-efficacy through education, problem-solving, role-playing, and planning have demonstrated improvements in diet quality.44–46
The demographic factors of age and ethnicity had no associations with diet quality in this sample and race did not remain a significant predictor of diet quality in the regression modeling. These findings are in contrast with multiple studies that have demonstrated the significant influence of age, race, and ethnicity with diet quality.37,47,48 This study sample ranged in age from 18 – 48 years, with the largest subset (50%) of the participants between 32 and 37 years. This limited age variance may explain the lack of association with diet quality. Similarly, Hispanic women comprised 15% of the sample, which may not have represented a sufficient sub-sample size to observe any variance in diet quality by ethnicity. Non-Hispanic Caucasian women had higher diet quality than the minority participants however, non-minority race was also significantly associated with higher levels of education. This relationship may explain the bivariate association between race and diet quality, but when entered into a regression model, educational attainment became the stronger demographic predictor of diet quality in this sample.
This study did not find any association between depressive symptoms and diet quality. Variance in depressive symptoms was limited (PHQ-9 scores ranged from 0 – 15), with 88% reporting minimal or mild symptoms. The association between depressive symptoms and diet quality is well-established, with studies demonstrating both that poor diet quality predicts depression49 and that higher levels of depressive symptoms contribute to poor diet.50 The lack of association in this study’s findings is likely due to the low variance and minimal depressive symptoms reported by the participants.
Risk perception or threat of T2DM did not have an influence in predicting variance in diet quality. In general, participants had realistic risk perceptions with half believing that they had none/slight chance of T2DM within ten years. A higher percentage of women in this study sample believed their risk to be moderate/high than in a previous study with pGDM women.30 The higher perception of risk in this sample may be due to selection bias– those with higher risk perceptions may be more likely to enroll in a study about diet quality and cardiometabolic risk. However, those that believed they had a moderate/high risk did not have any difference in diet quality as compared to those with lower perceived risk. Furthermore, neither perceptions about personal control, worry, nor optimistic bias contributed to variance in AHEI diet scores. These findings are similar to those reported in other studies in which risk perception did not influence health behavior in women with pGDM.51
Perceptions about barriers or benefits to healthy eating also were not associated with diet quality. Participants reported high levels of perceived benefits and low levels of barriers to healthy eating, but similar to another study,52 these factors did not contribute to variance in diet quality. Investigators from another study about healthy eating benefits and barriers found that these perceptions were related to levels of education.53 An association between lower perceived barriers and higher levels of education (r = −.26, P = .03) was found in this study sample, but there was no association with perceived benefits.
The importance of self- efficacy in health promoting behavior has been demonstrated both in this population and in other populations. The association of self-efficacy with diet quality supports part of this study’s hypotheses and one component of the Health Belief Model. However, the lack of association between T2DM risk perception, barriers, and benefits of healthy eating with diet quality refutes the other hypotheses and does not support these constructs of the Health Belief Model. Perceptions or beliefs seem to have less influence on dietary outcomes than self-efficacy and knowledge.42 Although this study was largely guided by the Health Belief Model and focused on examining individual influences and perceptions, it was embedded within an ecological model with recognition that achieving optimal dietary quality is complex and multifactorial.
In addition to the potential social and environmental influences that were beyond the investigative scope of this study, there may be other important individual influences that impact diet quality in women with pGDM. Time constraints, fatigue, work obstacles, and childcare duties have been identified as major barriers to diet and exercise activities in a qualitative investigation with women with pGDM.54 These identified barriers require further study to test their contribution to diet outcomes. Additionally, dietary restraint,55 perceived stress56 and sleep quality57 have been associated with diet quality in other populations of women, but have not been investigated in women with pGDM.
Limitations
There are a few limitations of this study which are worth noting. First, as a cross-sectional study, only associations could be identified between the variables, but no causality could be determined. Longitudinal studies in women with pGDM are needed to identify and understand the directionality of potential influences of diet quality. Second, while this sample size was adequate to determine the effect size of individual perceptions on diet quality, it was too small to detect differences by specific socio-demographic characteristics. The convenience sampling approach should be considered when generalizing the study findings to other studies in women with pGDM.
Strengths
This study has several strengths as well. It is one of few studies that have examined overall diet quality in pGDM women in addition to investigating associated socio-demographic and intrapersonal beliefs. Inadequate diet quality in pGDM women has been established in previous studies, but little was known about what might influence dietary adherence in this population. This study suggests that self-efficacy and education in particular may be important predictors of diet quality in pGDM women. Although a convenience sample, the study participants were recruited from multiple community and health care settings, which resulted in a socio-demographically diverse group of women. This diversity enhances the generalizability of these findings to pGDM women of multiple races, Hispanic ethnicity, and a wide range of education and income levels.
Conclusion
Level of education and dietary self-efficacy are important predictors of AHEI diet quality in women with pGDM. Interventions aimed at improving diet quality in these high-risk women should address strategies to increase dietary self-efficacy and address dietary knowledge and T2DM risk knowledge appropriate to individual health literacy and education levels. There is a considerable need to improve diet quality in pGDM women as this study supports previous work confirming that these at-risk women are not adhering fully to protective diets to prevent T2DM development. In addition to physical activity, a healthful diet is a critical component in preventing the progression to T2DM in at-risk populations. Future studies of diet quality among pGDM women should investigate intrapersonal influences of diet quality with a longitudinal design and expand the scope of influence beyond the individual to potential family/social and environmental factors.
Table 3.
Participant Scores on Intrapersonal Measures
| Instrument | Study Sample |
|---|---|
| 10 year Risk Perception | |
| Almost no/Slight chance, % | 50.7 |
| Moderate/High chance, % | 49.3 |
| Personal Control (RPS-DD), mean (SD) | 3.15 (0.5) |
| Worry (RPS-DD), mean (SD) | 2.73 (0.75) |
| Optimistic Bias (RPS-DD), mean (SD) | 2.10 (0.65) |
| Barriers to Healthy Eating, mean (SD) | 27.29 (6.52) |
| Benefits to Healthy Eating, mean (SD) | 42.23 (3.07) |
| Dietary Self Efficacy, mean (SD) | 51.89 (12.72) |
| Knowledge | |
| Diabetes Risk, mean (SD) | 60.96 (18.43) |
| Dietary Guidelines, mean (SD) | 42.23 (24.64) |
| Depressive Symptoms (PHQ-9), mean (SD) | 4.08 (4.06) |
| Minimal, % | 68.0 |
| Mild, % | 20.0 |
| Moderate, % | 10.7 |
| Moderately Severe, % | 1.3 |
Note. RPS-DD = Risk Perception Survey for Developing Diabetes; PHQ-9 = Patient Health Questionnaire.
Acknowledgement
This work was supported by an award from the American Heart Association. Research reported in this publication was also supported by the National Institute of Nursing Research of the National Institutes of Health under Award Number 1F31NR012605-01. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Contributor Information
Erin Poe Ferranti, Nell Hodgson Woodruff School of Nursing, Emory University, 1520 Clifton Road, NE, Atlanta, GA, Ph: 404-808-3685, Fax: 404-727-6945, epoe@emory.edu.
K. M. Venkat Narayan, Rollins School of Public Health and School of Medicine, Emory University Atlanta, GA.
Carolyn M. Reilly, Nell Hodgson Woodruff School of Nursing, Emory University Atlanta, GA.
Jennifer Foster, Nell Hodgson Woodruff School of Nursing, Emory University Atlanta, GA.
Marjorie McCullough, American Cancer Society, Inc. Atlanta, GA.
Thomas R. Ziegler, School of Medicine, Emory University Atlanta, GA.
Ying Guo, Rollins School of Public Health and Nell Hodgson Woodruff School of Nursing, Emory University Atlanta, GA.
Sandra B. Dunbar, Nell Hodgson Woodruff School of Nursing, Emory University Atlanta, GA.
References
- 1.Barbour LA, McCurdy CE, Hernandez TL, Kirwan JP, Catalano PM, Friedman JE. Cellular mechanisms for insulin resistance in normal pregnancy and gestational diabetes. Diabetes Care. 2007;30(Suppl 2):S112–S119. doi: 10.2337/dc07-s202. [DOI] [PubMed] [Google Scholar]
- 2.Nicholson WK, Wilson LM, Witkop CT, et al. Therapeutic management, delivery, and postpartum risk assessment and screening in gestational diabetes. Evid Rep Technol Assess (Full Rep) 2008;(162):1–96. [PMC free article] [PubMed] [Google Scholar]
- 3.American Diabetes Association. Gestational Diabetes Mellitus. Diabetes Care. 2003;26(Supplement 1):S103–S105. doi: 10.2337/diacare.26.2007.s103. [DOI] [PubMed] [Google Scholar]
- 4.Hunt KJ, Schuller KL. The increasing prevalence of diabetes in pregnancy. Obstet. Gynecol. Clin. North Am. 2007;34(2):173–199. doi: 10.1016/j.ogc.2007.03.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bentley-Lewis R. Late cardiovascular consequences of gestational diabetes mellitus. Semin Reprod Med. 2009;27(4):322–329. doi: 10.1055/s-0029-1225260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bellamy L, Casas JP, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet. 2009;373(9677):1773–1779. doi: 10.1016/S0140-6736(09)60731-5. [DOI] [PubMed] [Google Scholar]
- 7.Kim C, Newton KM, Knopp RH. Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care. 2002;25(10):1862–1868. doi: 10.2337/diacare.25.10.1862. [DOI] [PubMed] [Google Scholar]
- 8.Bantle JP, Wylie-Rosett J, Albright AL, et al. Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2008;31(Suppl 1):S61–S78. doi: 10.2337/dc08-S061. [DOI] [PubMed] [Google Scholar]
- 9.Kieffer EC, Sinco B, Kim C. Health behaviors among women of reproductive age with and without a history of gestational diabetes mellitus. Diabetes Care. 2006;29(8):1788–1793. doi: 10.2337/dc06-0199. [DOI] [PubMed] [Google Scholar]
- 10.Zehle K, Smith BJ, Chey T, McLean M, Bauman AE, Cheung NW. Psychosocial factors related to diet among women with recent gestational diabetes: opportunities for intervention. Diabetes Educ. 2008;34(5):807–814. doi: 10.1177/0145721708323641. [DOI] [PubMed] [Google Scholar]
- 11.Ratner RE, Christophi CA, Metzger BE, et al. Prevention of diabetes in women with a history of gestational diabetes: effects of metformin and lifestyle interventions. J. Clin. Endocrinol. Metab. 2008;93(12):4774–4779. doi: 10.1210/jc.2008-0772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tobias DK, Hu FB, Chavarro J, Rosner B, Mozaffarian D, Zhang C. Healthful Dietary Patterns and Type 2 Diabetes Mellitus Risk Among Women With a History of Gestational Diabetes Mellitus. Arch. Intern. Med. 2012:1–7. doi: 10.1001/archinternmed.2012.3747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shyam S, Arshad F, Abdul Ghani R, et al. Low glycaemic index diets improve glucose tolerance and body weight in women with previous history of gestational diabetes: a six months randomized trial. Nutr J. 2013;12:68. doi: 10.1186/1475-2891-12-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McCullough ML, Feskanich D, Stampfer MJ, et al. Diet quality and major chronic disease risk in men and women: moving toward improved dietary guidance. Am. J. Clin. Nutr. 2002;76(6):1261–1271. doi: 10.1093/ajcn/76.6.1261. [DOI] [PubMed] [Google Scholar]
- 15.Fung TT, McCullough M, van Dam RM, Hu FB. A prospective study of overall diet quality and risk of type 2 diabetes in women. Diabetes Care. 2007;30(7):1753–1757. doi: 10.2337/dc06-2581. [DOI] [PubMed] [Google Scholar]
- 16.Belin RJ, Greenland P, Allison M, et al. Diet quality and the risk of cardiovascular disease: the Women's Health Initiative (WHI) Am. J. Clin. Nutr. 2011;94(1):49–57. doi: 10.3945/ajcn.110.011221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reedy J, Mitrou PN, Krebs-Smith SM, et al. Index-based dietary patterns and risk of colorectal cancer: the NIH-AARP Diet and Health Study. Am. J. Epidemiol. 2008;168(1):38–48. doi: 10.1093/aje/kwn097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Akbaraly TN, Singh-Manoux A, Tabak AG, et al. Overall diet history and reversibility of the metabolic syndrome over 5 years: the Whitehall II prospective cohort study. Diabetes Care. 2010;33(11):2339–2341. doi: 10.2337/dc09-2200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Story M, Kaphingst KM, Robinson-O'Brien R, Glanz K. Creating healthy food and eating environments: policy and environmental approaches. Annu. Rev. Public Health. 2008;29:253–272. doi: 10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- 20.Rifas-Shiman SL, Rich-Edwards JW, Kleinman KP, Oken E, Gillman MW. Dietary quality during pregnancy varies by maternal characteristics in Project Viva: a US cohort. J. Am. Diet. Assoc. 2009;109(6):1004–1011. doi: 10.1016/j.jada.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nuss H, Freeland-Graves J, Clarke K, Klohe-Lehman D, Milani TJ. Greater nutrition knowledge is associated with lower 1-year postpartum weight retention in low-income women. J. Am. Diet. Assoc. 2007;107(10):1801–1806. doi: 10.1016/j.jada.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 22.Barker M, Lawrence W, Crozier S, et al. Educational attainment, perceived control and the quality of women's diets. Appetite. 2009;52(3):631–636. doi: 10.1016/j.appet.2009.02.011. [DOI] [PubMed] [Google Scholar]
- 23.Campbell MK, McLerran D, Turner-McGrievy G, et al. Mediation of adult fruit and vegetable consumption in the National 5 A Day for Better Health community studies. Ann. Behav. Med. 2008;35(1):49–60. doi: 10.1007/s12160-007-9002-y. [DOI] [PubMed] [Google Scholar]
- 24.Jacka FN, Pasco JA, Mykletun A, et al. Association of Western and Traditional Diets With Depression and Anxiety in Women. Am. J. Psychiatry. 2010;167(3):305–311. doi: 10.1176/appi.ajp.2009.09060881. [DOI] [PubMed] [Google Scholar]
- 25.Leung BM, Kaplan BJ. Perinatal depression: prevalence, risks, and the nutrition link--a review of the literature. J. Am. Diet. Assoc. 2009;109(9):1566–1575. doi: 10.1016/j.jada.2009.06.368. [DOI] [PubMed] [Google Scholar]
- 26.Bodnar LM, Wisner KL. Nutrition and depression: implications for improving mental health among childbearing-aged women. Biol. Psychiatry. 2005;58(9):679–685. doi: 10.1016/j.biopsych.2005.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Subar AF, Thompson FE, Kipnis V, Midthune D, Hurwitz P, McNutt S, McIntosh A, Rosenfeld S. Comparative Validation of the Block, Willett, and National Cancer Institue Food Frequency Questionnaires. Am. J. Epidemiol. 2001;154(12):1089–1099. doi: 10.1093/aje/154.12.1089. [DOI] [PubMed] [Google Scholar]
- 28.Boucher B, Cotterchio M, Kreiger N, Nadalin V, Block T, Block G. Validity and reliability of the Block98 food-frequency questionnaire in a sample of Canadian women. Public Health Nutr. 2006;9(1):84–93. doi: 10.1079/phn2005763. [DOI] [PubMed] [Google Scholar]
- 29.Walker EA, Fisher E, Marrero DG, McNabb W. Comparative risk judgements among participants in the Diabetes Prevention Program (Abstract) Diabetes. 2001;50:A397. [Google Scholar]
- 30.Kim C, McEwen LN, Piette JD, Goewey J, Ferrara A, Walker EA. Risk perception for diabetes among women with histories of gestational diabetes mellitus. Diabetes Care. 2007;30(9):2281–2286. doi: 10.2337/dc07-0618. [DOI] [PubMed] [Google Scholar]
- 31.Fowles ER, Feucht J. Testing the barriers to healthy eating scale. West. J. Nurs. Res. 2004;26(4):429–443. doi: 10.1177/0193945904263281. [DOI] [PubMed] [Google Scholar]
- 32.Hickey ML, Owen SV, Froman RD. Instrument development: cardiac diet and exercise self-efficacy. Nurs. Res. 1992;41(6):347–351. [PubMed] [Google Scholar]
- 33.Zoellner J, Bounds W, Connell C. Community Health Advisors' Perceptions of the 2005 Dietary Guidelines and MyPyramid. Journal of Extension. 2009;47(2) [Google Scholar]
- 34.U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans. 7th ed. Washington D.C.: U.S. Government Printing Office; 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.IBM SPSS Statistics for Windows, Version 20.0 [computer program] Armonk, NY: IBM, Corp.; Released 2011. [Google Scholar]
- 37.Hiza HA, Casavale KO, Guenther PM, Davis CA. Diet Quality of Americans Differs by Age, Sex, Race/Ethnicity, Income, and Education Level. J. Acad. Nutr. Diet. 2012;113(12):297–306. doi: 10.1016/j.jand.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 38.Morrison MK, Koh D, Lowe JM, et al. Postpartum diet quality in Australian women following a gestational diabetes pregnancy. Eur. J. Clin. Nutr. 2012;66(10):1160–1165. doi: 10.1038/ejcn.2012.84. [DOI] [PubMed] [Google Scholar]
- 39.Taggart J, Williams A, Dennis S, et al. A systematic review of interventions in primary care to improve health literacy for chronic disease behavioral risk factors. BMC Fam. Pract. 2012;13:49. doi: 10.1186/1471-2296-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dickson-Spillmann M, Siegrist M. Consumers' knowledge of healthy diets and its correlation with dietary behaviour. J. Hum. Nutr. Diet. 2011;24(1):54–60. doi: 10.1111/j.1365-277X.2010.01124.x. [DOI] [PubMed] [Google Scholar]
- 41.Baptiste-Roberts K, Gary TL, Beckles GL, et al. Family history of diabetes, awareness of risk factors, and health behaviors among African Americans. Am. J. Public Health. 2007;97(5):907–912. doi: 10.2105/AJPH.2005.077032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shaikh AR, Yaroch AL, Nebeling L, Yeh MC, Resnicow K. Psychosocial predictors of fruit and vegetable consumption in adults: A review of the literature. Am. J. Prev. Med. 2008;34(6):535–543. doi: 10.1016/j.amepre.2007.12.028. [DOI] [PubMed] [Google Scholar]
- 43.Wright K, Norris K, Newman Giger J, Suro Z. Improving healthy dietary behaviors, nutrition knowledge, and self-efficacy among underserved school children with parent and community involvement. Child. Obes. 2012;8(4):347–356. doi: 10.1089/chi.2012.0045. [DOI] [PubMed] [Google Scholar]
- 44.Shin H, Shin J, Liu PY, Dutton GR, Abood DA, Ilich JZ. Self-efficacy improves weight loss in overweight/obese postmenopausal women during a 6-month weight loss intervention. Nutr. Res. 2011;31(11):822–828. doi: 10.1016/j.nutres.2011.09.022. [DOI] [PubMed] [Google Scholar]
- 45.Kreausukon P, Gellert P, Lippke S, Schwarzer R. Planning and self-efficacy can increase fruit and vegetable consumption: a randomized controlled trial. J. Behav. Med. 2012;35(4):443–451. doi: 10.1007/s10865-011-9373-1. [DOI] [PubMed] [Google Scholar]
- 46.Luszczynska A, Tryburcy M, Schwarzer R. Improving fruit and vegetable consumption: a self-efficacy intervention compared with a combined self-efficacy and planning intervention. Health Educ. Res. 2007;22(5):630–638. doi: 10.1093/her/cyl133. [DOI] [PubMed] [Google Scholar]
- 47.Ervin RB. Healthy Eating Index--2005 total and component scores for adults aged 20 and over: National Health and Nutrition Examination Survey, 2003–2004. Natl. Health. Stat. Report. 2011;(44):1–9. [PubMed] [Google Scholar]
- 48.Shannon J, Shikany JM, Barrett-Connor E, et al. Demographic factors associated with the diet quality of older US men: baseline data from the Osteoporotic Fractures in Men (MrOS) study. Public Health Nutr. 2007;10(8):810–818. doi: 10.1017/S1368980007258604. [DOI] [PubMed] [Google Scholar]
- 49.Akbaraly TN, Brunner EJ, Ferrie JE, Marmot MG, Kivimaki M, Singh-Manoux A. Dietary pattern and depressive symptoms in middle age. Br. J. Psychiatry. 2009;195(5):408–413. doi: 10.1192/bjp.bp.108.058925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Appelhans BM, Whited MC, Schneider KL, et al. Depression severity, diet quality, and physical activity in women with obesity and depression. J. Acad. Nutr. Diet. 2012;112(5):693–698. doi: 10.1016/j.jand.2012.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kaiser B, Razurel C. Determinants of postpartum physical activity, dietary habits and weight loss after gestational diabetes mellitus. J. Nurs. Manag. 2013;21(1):58–69. doi: 10.1111/jonm.12006. [DOI] [PubMed] [Google Scholar]
- 52.Pawlak R, Colby S. Benefits, barriers, self-efficacy and knowledge regarding healthy foods; perception of African Americans living in eastern North Carolina. Nutr. Res. Pract. 2009;3(1):56–63. doi: 10.4162/nrp.2009.3.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Holgado B, de Irala-Estevez J, Martinez-Gonzalez MA, Gibney M, Kearney J, Martinez JA. Barriers and benefits of a healthy diet in spain: comparison with other European member states. Eur. J. Clin. Nutr. 2000;54(6):453–459. doi: 10.1038/sj.ejcn.1600996. [DOI] [PubMed] [Google Scholar]
- 54.Nicklas JM, Zera CA, Seely EW, Abdul-Rahim ZS, Rudloff ND, Levkoff SE. Identifying postpartum intervention approaches to prevent type 2 diabetes in women with a history of gestational diabetes. BMC Pregnancy Childbirth. 2011;11:23. doi: 10.1186/1471-2393-11-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mumford SL, Siega-Riz AM, Herring A, Evenson KR. Dietary restraint and gestational weight gain. J. Am. Diet. Assoc. 2008;108(10):1646–1653. doi: 10.1016/j.jada.2008.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fowles ER, Bryant M, Kim S, et al. Predictors of dietary quality in low-income pregnant women: a path analysis. Nurs. Res. 2011;60(5):286–294. doi: 10.1097/NNR.0b013e3182266461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Haghighatdoost F, Karimi G, Esmaillzadeh A, Azadbakht L. Sleep deprivation is associated with lower diet quality indices and higher rate of general and central obesity among young female students in Iran. Nutrition. 2012;28(11–12):1146–1150. doi: 10.1016/j.nut.2012.04.015. [DOI] [PubMed] [Google Scholar]