Abstract
Background:
The aim of the present study was to determine the relation between neck circumferences (NC), as an indicator of upper body obesity, with anthropometric and cardio-metabolic factors among the first degree relatives of diabetes patients.
Materials and Methods:
This cross-sectional study was performed on first degree relatives of diabetes patients (n = 213). Weight, height, waist circumference (WC), hip circumference (HC), systolic blood pressure (SBP), diastolic blood pressure (DBP) and NC were measured. Laboratory data included oral glucose tolerance test (OGTT) results, high density lipoprotein (HDL), low density lipoprotein, triglyceride (TG) and total cholesterol.
Results:
There was no difference in NC among different results of OGTT in men or women. Factors including weight, body mass index (BMI), WC and HC were strongly associated with NC in both genders (r = 0.420-0.711). NC was weakly associated with SBP in women (r = 0.195) and moderately with DBP in men (r = 0.314). Regarding lipid profile, HDL and TG were associated with NC only in women (r = −0.268-0.325).
Conclusions:
NC has a significant correlation with gender and anthropometric variables including BMI, weight and waist and HCs in both men and women but it does not differ significantly in patients with different status in OGTT.
Keywords: Body mass index, cardiovascular, diabetes, neck circumference, obesity
INTRODUCTION
Now-a-days, obesity is became a major concern and important public health problem in developing countries as well as in developed countries.[1,2] The prevalence of obesity and its associated co-morbidities are increasing.[1] Although several efforts have been performed to control this problem; however, its prevalence has raised to pandemic proportions.[2] There are over a billion overweight and over 400 million obese adults in the world.[3]
There is several health issues related to obesity such as cardiovascular diseases, diabetes, cancers, osteoarthritis and fatty liver disease.[4] In definition, obesity is referred to excess of fat.[5] Until now, a direct method for the measurement of body fat is not available and by this reason body fat in daily practice often assessed by means of indirect methods like anthropometric measures including body mass index (BMI).[5]
Distribution of obesity is one of the major predictors of metabolic and cardiovascular diseases and it is more accurate than whole body obesity which is assessed by BMI.[2] Upper body obesity has more relationship with cardio-metabolic risk factors such as diabetes, glucose intolerance, hyper-insulinemia and hypertriglyceridemia.[6]
Several indices have been described for the assessment of upper body obesity such as waist circumference (WC), waist to hip ratio, waist to thigh ratio and sub-scapular to triceps skin fold ratio.[3,6,7] These indices have some limitations. For instance, WC is used in several studies however its exact location for measurement has been different among studies. In the other hand, WC varies during the day and also it is not applicable for large sample studies.[8,9]
Neck circumference (NC) is recently described as an index for upper body subcutaneous fat.[7] Its measurement is easier than WC and also can be helpful for population based studies with large sample sizes. Data about the relation of NC as an indicator of upper abdominal obesity with cardio-metabolic risk factors is lacking. Most of the studies in this field have been performed on normal population and there are not enough data about close relatives of high risk patients such as diabetic patients.[2,7,10] In this study, we aimed to determine the relation between NC as an indicator of upper body obesity with cardio-metabolic factors.
MATERIALS AND METHODS
Participants and setting
This cross-sectional study was performed at Sedighe Tahere hospital, a referral endocrinology center in Isfahan, Iran. During a period of 6 months, since May 2012 to November 2012, a total number of 213 eligible participants were enrolled in the study. Participants were selected randomly from first degree relatives of diabetes patients who came to our clinic for their diabetes treatment. Individuals aged above 18 years were included in the study. They were excluded if any of the following criteria were present: Severe disability, heart failure, renal failure, consumption of anti-lipid drugs, goiter or other neck lesions and history of neck surgery. Written informed consent has been obtained from all patients for the use of their medical record in research purposes and the protocol of the project has been approved by Ethics Committee of the Isfahan University of Medical Sciences.
Measurements
Demographic data about age and sex were obtained from each participant. Height was measured to nearest 0.1 cm and weight measured using a digital scale to nearest 0.1 kg. WC was measured at the umbilicus level after normal breath to the nearest 0.1 cm. BMI was calculated using the formula: Weight/height2 (kilogram/m2). Hip circumference (HC) was measured at the most salient point between the waist and the thigh. Blood pressure (BP) was measured by one of the study investigators using standard mercury sphygmomanometer. In each patient's BP was measured twice after each individual after a 10-15 min rest and the average was used in the analysis. The NC was measured using a plastic tape with head in erect position and eyes facing forward, horizontally at the upper margin of the laryngeal prominence.
Blood sample were obtained after 12 h fasting to measure the fasting plasma glucose (FPG), high density lipoprotein (HDL), low density lipoprotein (LDL), triglyceride (TG) and total cholesterol (TC) concentrations (by commercial available kits; Chemi Enzyme and Pars Azmoon, Iran). Oral glucose tolerance test (OGTT) was performed and blood sample were taken 2 h after administration of 75 g glucose. Test results were categorized to:[8] first: Impaired fasting glucose was considered as FPG from 100 to 125 mg/dL; second: Impaired glucose tolerance was defined as 2-h plasma glucose from 140 to 199 mg/dL; third: Diabetes was defined by FPG more than 126 mg/dL or abnormal OGTT with plasma glucose ≥200 mg/dL measured 2 h after consuming 75 g glucose.
Sample size and statistical analyses
Sample size was calculated as 210 patients considering α = 0.05 and β = 0.2. Statistical analyzes were performed using statistical software (SPSS version 16.0; SPSS, Inc., Chicago, IL) and P < 0.05 was considered to be significant.
RESULTS
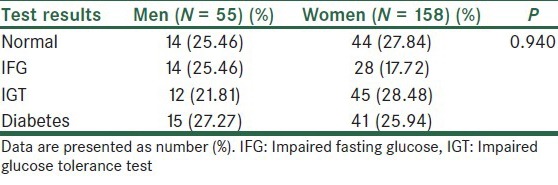
A total number of 213 patients were enrolled during the study period including 55 men and 158 women with age ranged from 18 to 75 years; mean age = 44.7 ± 8.5 years. Comparison of demographic, anthropometric and laboratory data between men and women are shown in Table 1. Compared with women, men had lower BMI, greater WC, smaller HC, greater waist to hip ratio, greater NC and lower HDL and higher TG concentrations [Table 1]. There was no statistically significant difference among men and women in OGTT results [Table 2].
Table 1.
Comparison of demographic, anthropometric and laboratory data between men and women
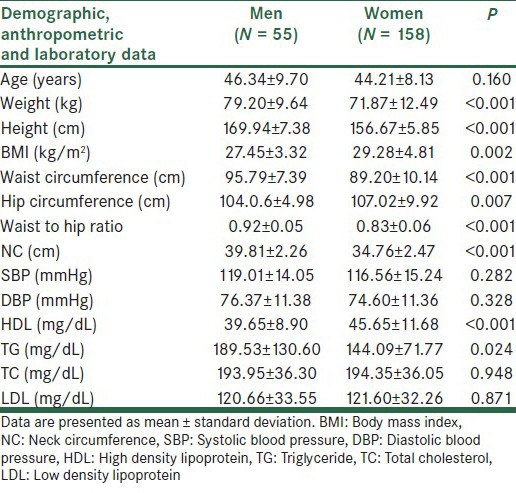
Table 2.
Oral glucose tolerance test results among study patients
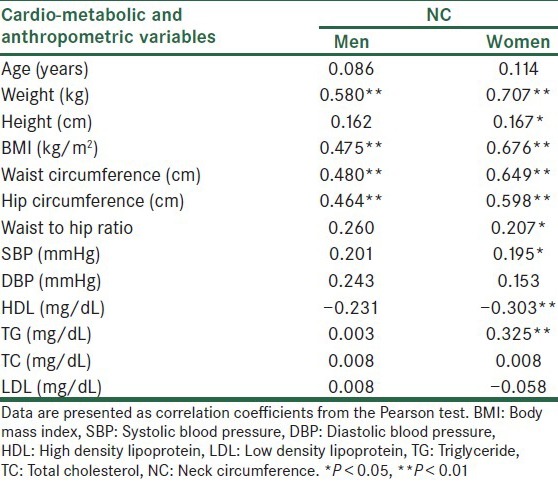
The correlation of NC with the demographic, cardio-metabolic and anthropometric variables among men and women are presented in Table 3. Those factors which were strongly associated with NC in both genders included weight, BMI, WC and HP (r = 0.420-0.711). There was a weak association between NC with systolic blood pressure in women (r = 0.195) and moderately between NC and diastolic blood pressure in men (r = 0.314). Regarding lipid profile, HDL and TG were associated with NC but only in women (r = −0.268-0.325).
Table 3.
Correlation coefficients of NC with the cardio-metabolic and anthropometric variables
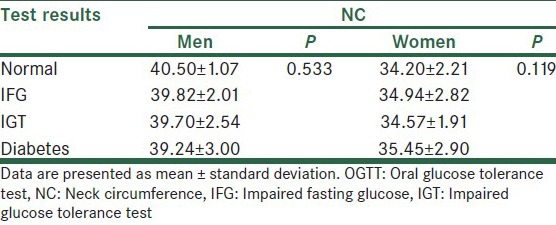
Analyzing the relation between NC and OGTT results showed no statistical significant difference in NC among different results of OGTT in men or women [Table 4].
Table 4.
NC-U and NC-L in different OGTT results among men and women
DISCUSSION
The aim of the present study was to investigate the relationship between NC and the demographic, cardio-metabolic and anthropometric characteristics in the first degree relatives of diabetes patients. Our results showed that NC has strong correlations with BMI, weight and waist and HCs in both men and women. None of the cardio-metabolic risk factors had significant relation with NC in both men and women. However, a significant relation between NC and TG and HDL was found only in women.
Previous studies in this field which carried out in different societies showed different results. A study performed in the Middle East by Ben-Noun et al.[9] showed that NC has a significant correlation with BMI, WC and waist to hip ratio similar to our study. However, this study also showed a correlation between NC with LDL, TG, TC in both men and women which was against our results.[9] In another study performed in western countries by Nafiu et al.,[10] a significant relation was reported between NC and age, BMI and WC. In this study, the cardio-metabolic factors were not evaluated and the study focused on demographic and anthropometric variables.[10] Another study in Brazilian population revealed that NC has relation with BMI, WC, HDL and TG in both genders.[11] Some other studies also revealed controversial issues; however, in line with our study most of them found the relation between NC with gender and anthropometric characteristics rather than cardio-metabolic variables.[7,10,12]
Regarding the relation of FPG and glucose intolerance with NC, previous studies evaluated the relation between FPG and glycated hemoglobin with NC. In a study by Zhou et al. evaluated the association between some anthropometric indices and cardio-metabolic risk factors and they found a significant relation between NC and FPG.[11] In another study by Stabe et al., results showed significant relation of NC with FPG, but the relation between NC and glycated hemoglobin was not statistically significant.[7] However, these studies had a limitation as none of them performed OGTT and included only the FPG and glycated hemoglobin. Aswathappa et al. evaluated NC in diabetic and non-diabetic patients based on their medical history and found that NC in diabetic patients is significantly higher than non-diabetic ones.[12] In contrast with the mentioned study, we found no statistically significant difference in the NC among different results of OGTT.
Our study had a limitation about its sample size and we suggest further multi center studies with larger sample size to evaluate the relation of NC with demographic, anthropometric and cardio-metabolic variables.
CONCLUSIONS
NC has significant correlation with gender and anthropometric variables including BMI, weight and waist and HCs in both men and women. However, NC does not differ significantly in patients with different status in OGTT. According to ease of assessment, NC is a potential alternative index for BMI or other anthropometric measures but further studies with larger sample size are required in this regard.
ACKNOWLEDGMENTS
The authors would like to thank Isfahan University of Medical Sciences. Authors are thankful to Dr. Asgari, Mrs. Zare and Mr. Abyar who helped us in conducting the study and also appreciate the assistance from Dr. Gholamrezaei for editing this report.
Footnotes
Source of Support: This study was supported by the Isfahan University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Dietz WH, Robinson TN. Clinical practice. Overweight children and adolescents. N Engl J Med. 2005;352:2100–9. doi: 10.1056/NEJMcp043052. [DOI] [PubMed] [Google Scholar]
- 2.Cornier MA, Després JP, Davis N, Grossniklaus DA, Klein S, Lamarche B, et al. Assessing adiposity: A scientific statement from the American Heart Association. Circulation. 2011;124:1996–2019. doi: 10.1161/CIR.0b013e318233bc6a. [DOI] [PubMed] [Google Scholar]
- 3.Adeboye B, Bermano G, Rolland C. Obesity and its health impact in Africa: A systematic review. Cardiovasc J Afr. 2012;23:512–21. doi: 10.5830/CVJA-2012-040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vucenik I, Stains JP. Obesity and cancer risk: Evidence, mechanisms, and recommendations. Ann N Y Acad Sci. 2012;1271:37–43. doi: 10.1111/j.1749-6632.2012.06750.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flodmark CE, Lissau I, Moreno LA, Pietrobelli A, Widhalm K. New insights into the field of children and adolescents’ obesity: The European perspective. Int J Obes Relat Metab Disord. 2004;28:1189–96. doi: 10.1038/sj.ijo.0802787. [DOI] [PubMed] [Google Scholar]
- 6.Ben-Noun LL, Laor A. Relationship between changes in neck circumference and cardiovascular risk factors. Exp Clin Cardiol. 2006;11:14–20. [PMC free article] [PubMed] [Google Scholar]
- 7.Stabe C, Vasques AC, Lima MM, Tambascia MA, Pareja JC, Yamanaka A, et al. Neck circumference as a simple tool for identifying the metabolic syndrome and insulin resistance: Results from the Brazilian Metabolic Syndrome Study. Clin Endocrinol (Oxf) 2013;78:874–81. doi: 10.1111/j.1365-2265.2012.04487.x. [DOI] [PubMed] [Google Scholar]
- 8.Laffel L, Svoren B. Epidemiology, presentations, and diagnosis of type 2 diabetes mellitus in children and adolescents. In: Basow DS, editor. Waltham, MA: UpToDate; 2013. [Google Scholar]
- 9.Ben-Noun L, Sohar E, Laor A. Neck circumference as a simple screening measure for identifying overweight and obese patients. Obes Res. 2001;9:470–7. doi: 10.1038/oby.2001.61. [DOI] [PubMed] [Google Scholar]
- 10.Nafiu OO, Burke C, Lee J, Voepel-Lewis T, Malviya S, Tremper KK. Neck circumference as a screening measure for identifying children with high body mass index. Pediatrics. 2010;126:e306–10. doi: 10.1542/peds.2010-0242. [DOI] [PubMed] [Google Scholar]
- 11.Zhou JY, Ge H, Zhu MF, Wang LJ, Chen L, Tan YZ, et al. Neck circumference as an independent predictive contributor to cardio-metabolic syndrome. Cardiovasc Diabetol. 2013;12:76. doi: 10.1186/1475-2840-12-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aswathappa J, Garg S, Kutty K, Shankar V. Neck circumference as an anthropometric measure of obesity in diabetics. N Am J Med Sci. 2013;5:28–31. doi: 10.4103/1947-2714.106188. [DOI] [PMC free article] [PubMed] [Google Scholar]


