Abstract
Cancer patients are commonly transfused with blood products immediately before, during or after major surgery. Blood loss and haemodilution are the most common causes of red blood cells (RBCs) administration and coagulopathies are the indications for the infusion of fresh-frozen plasma (FFP), cryoprecipitates and platelets. Transfusion-related immune modulation is a complication associated with the administration of blood products. A decreased immune surveillance as a consequence of blood transfusions has been linked to cancer recurrence and progression. Moreover, soluble factors present in packed RBCs, platelets and FFP can directly stimulate tumour growth and spread. Two meta-analyses suggest that the administration of blood products is associated with shorter recurrence-free survival and overall survival after colorectal cancer surgery. More studies are needed to show such association in different cancer patient populations.
Keywords: Blood product transfusion, cancer recurrence, immune suppression
INTRODUCTION
Patients undergoing major oncological surgery are at risk for severe bleeding and coagulopathy due to the tumour biology, pre-operative cancer therapies (chemo-radiation and immune-therapies), anatomic features of the surgical area (vascular proximity), complexity of the resection, and perioperative factors (haemodilution, hypothermia and metabolic derangements). A recent study reported that the rate of perioperative blood transfusions (BTs) in colorectal cancer and prostate patients has decreased from 68.6% to 45.6% over the last three decades; however, the rate still remains high.[1,2] Anaesthesiologists, surgeons and critical care physicians must often make the difficult decision on when to administer blood products to patients undergoing cancer surgery. Blood products are usually administered with two goals: (1) Improve oxygen delivery (red blood cells [RBCs]) and/or (2) correct coagulopathies (platelets, fresh-frozen plasma [FFP] and cryoprecipitate). In spite of a substantial amount of research on the, biological consequences, and clinical impact of perioperative blood product transfusions in patients undergoing major oncological surgeries, no clear indications or consensus guidelines exist.
One of the immediate biological consequences of the administration of packed RBCs, FFP and/or platelets is immune suppression; a phenomenon that has been termed transfusion-related immune modulation [TRIM]. It has been hypothesised that TRIM can have a negative impact on short and long-term surgical outcomes in patients who are transfused compared to those who have not received blood products.
In the present review article, we will comment on: (1) the current indications for perioperative blood product transfusions in patients undergoing cancer surgery, (2) TRIM and (3) the impact of BT on long-term oncological outcomes, specifically cancer recurrence and mortality.
PERIOPERATIVE BLOOD TRANSFUSIONS IN CANCER PATIENTS: THE INDICATIONS TO TRANSFUSE
The prevalence of anaemia in cancer patients ranges from 30% to 90%.[3] Perioperative cancer-related anaemia can result from diminished production, increased destruction, or loss of RBCs [Table 1]. Their production may be reduced due to chemotherapeutic agents, radiation therapies, chronic renal disease, iron deficiency, and myelodysplasia or bone metastasis. Patients with myelo- and lymphoproliferative disorders can be anaemic due to increased haemolysis or hypersplenism as a consequence of cirrhosis and portal hypertension. Finally, blood loss and haemodilution are perhaps the most common causes of anaemia during and following cancer surgery.[4] Although healthy subjects are able to tolerate haemoglobin (Hb) values below 6 g/dL, older patients and those with significant comorbidities present an increased risk of mortality with Hb concentrations of 8 g/dL or lower. Most guidelines, therefore, suggest that BTs should be administered to maintain a Hb level between 6.0 and 10 g/dL. Hence, patients’ age, comorbid burden, haemodynamic and oxygenation status, pre-operative Hb levels, and the complexity of surgical intervention (propensity for post-operative anaemia and degree of surgical stress response) should be taken into consideration before transfusing cancer surgical patients.
Table 1.
Mechanisms of perioperative cancer-related hematologic disorders
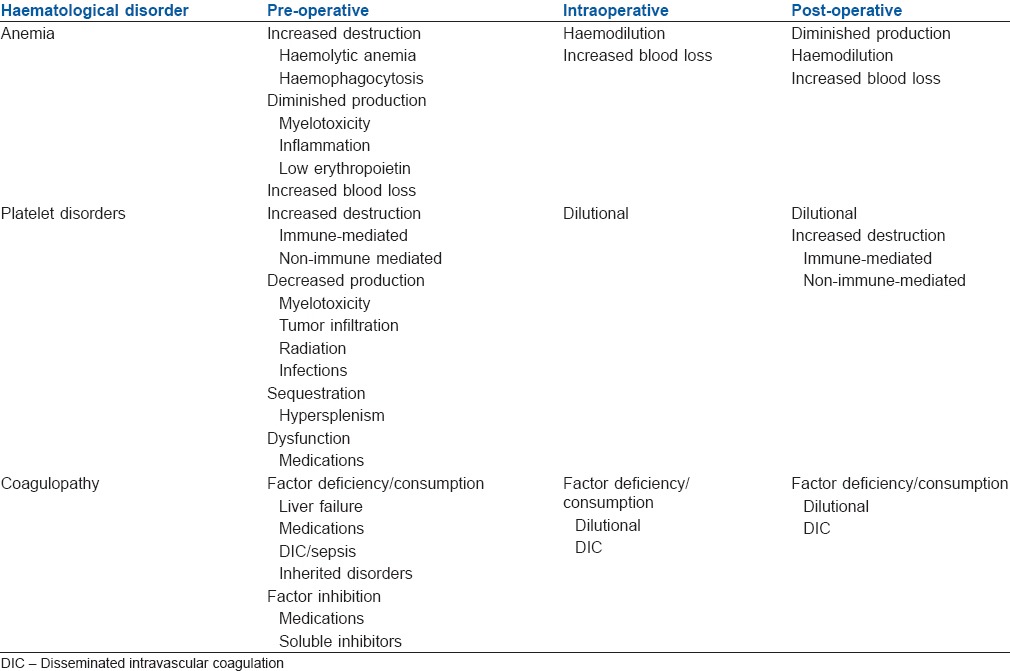
Patients with cancer can also present disorders of the haemostatic function because the tumour per se can induce activation of the coagulation system resulting in a chronic hypercoagulable state, a thrombolytic state, or a condition of chronic disseminated intravascular coagulation (DIC). Thrombocytopenia is a common disorder in cancer patients, mainly in those with myelosuppression. Other mechanisms of thrombocytopenia in this population include increased destruction (immune and non-immune), decrease production, sequestration and dilutional. Dilutional thrombocytopenia (infusion of crystalloids and blood products) and DIC are the most common causes of a low count of platelets during and after cancer surgery.[5] The indications for platelet administration to patients undergoing oncological procedures depend on the number of circulating platelet and the clinical judgment of perioperative physicians. In patients with haematologic malignancies the trigger threshold for prophylactic transfusion is 20,000 platelets/μL; however, it has been indicated that in patients not taking aspirin a count of 10,000 platelets/μL could also be used as a trigger. It is commonly accepted that patients with 50,000 platelets/μL or more could have surgery ‘safely’; unless other disorders in the coagulation system exists including the presence of platelet inhibitors or consumption coagulopathy (DIC) and does not involve high risk surgery for closed cavity bleeding (i.e., neurosurgery).[6]
Coagulation disorders as a consequence of alterations in the so-called intrinsic or extrinsic ‘pathways’ or at the level of any of the ‘phases’ (initiation, amplification and propagation) of the cell-based model of haemostasis can be found in patients who undergo cancer-related surgery. Blood products such as FFP and cryoprecipitate are commonly administered to cancer patients with the goal of preventing bleeding and correcting abnormal coagulation in those acutely bleeding. In the pre-operative period patients may present with abnormalities in the haemostasis as a result of the administration of anticoagulants (warfarin, unfractionated or low molecular heparin and factor Xa inhibitors) or cancer-related complications (sepsis, DIC and primary fibrinolysis). Intra - and post-operatively, coagulopathy is the result of haemodilution or consumption of factors as can be observed during sepsis and less commonly with prostate and neurosurgical procedures. Consensus on the trigger ‘threshold’ to start the administration of products like FFP or cryoprecipitate is still lacking in the surgical oncology literature; however, it is worth remembering that clinical studies demonstrate that the expected correction (per unit of FFP administered) in the international normalized ratio is minimal when pre-transfusion values are minimally elevated. This suggests that patients who really benefit from the administration of FFP are those who present serious coagulation abnormalities.
Taking all together, a large number of patients undergoing oncological procedures will come to the operating room with some degree of anaemia and/or coagulopathy of multifactorial origin. However, intraoperative haemodilution and consumption of factors are the most common causes of anaemia and coagulopathy post-operatively. Unfortunately, no clear triggers have defined to correct perioperative anaemia or disorder in the coagulation pathways.
PERIOPERATIVE BLOOD TRANSFUSIONS IN CANCER PATIENTS: THE BIOLOGICAL CONSEQUENCES
The administration of blood products has been associated with profound negative effects on the immune system. At cellular level, some of the features of TRIM are: (a) a reduction in the function of natural killer (NK) cells, (b) a decrease in the proliferation of T and B lymphocytes, (c) induction of T regulatory cells and (d) a decrease in maturation and antigen presenting activity of dendritic cells.[7] Some of the described cellular and humoral alterations observed after BT are more exaggerated following the administration of ‘older’ blood units (storage lesion) since the exposure of lymphocytes to fresh blood does not affect their proliferative activity. To further illustrate some of the effect of BT on cellular immunity, Guo et al. recently demonstrated that the administration of allogeneic blood to patients undergoing gastrointestinal surgery caused a significant decrease in the number of NK cells that was not observed in patients who received autologous blood.[8] Most of the changes described at the cellular levels are the result of the infusion into the recipient of high concentrations of interleukins (IL-1β, IL-6, IL-8), chemokines, prostaglandin E, thromboxanes, histamine, leukocytes (in non-leucoreduced units or residual leukocytes in leucoreduced units), growth factors (transforming growth factor-β [TGF-β] vascular endothelial growth factor [VEGF] and epidermal growth factor, fibroblast growth factor and platelet-derived growth factor), non-polar lipids, proinflammatory lysophosphatidylcholines, CD40 ligand and microparticles present in RBCs, platelets or FFP units [Figure 1].[9]
Figure 1.
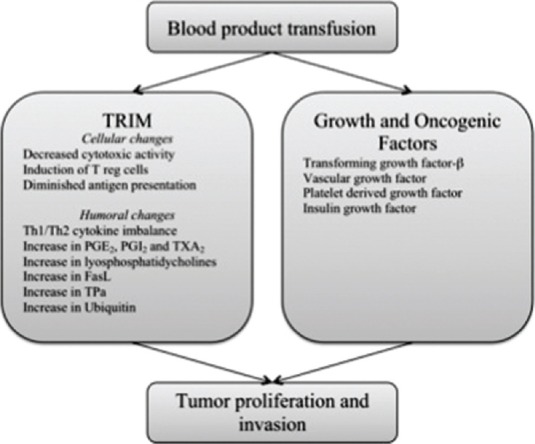
Possible mechanisms associated with tumor growth and spread after blood products administration
Transfusion-related immune suppression can be mechanistically divided in two different types: (1) donor-specific transfusion and (2) ‘generalised’ transfusion-related immune suppression. The former primarily suppress the adaptive immunity (lymphocytes T and B) and has been related to microchimerism, veto cells and cytokines; in contrast, the ‘generalised’ form appears to be mediated by macrophage and neutrophils, and has a significant suppressive impact on the innate immunity. It has been proposed that infections and cancer recurrence would be a consequence of the ‘generalised’ transfusion-related immune suppression rather than the donor- specific form.[10] The timing of transfusion may also have different effects on the inflammatory and immune response. Thus, when blood products are administered during or immediately after surgery (‘second hit’-first hit being surgical trauma), the so-called systemic inflammatory response syndrome can be further exaggerated by transfusions delaying mechanisms of resolutions of inflammation, which can also participate in the pathogenesis of transfusion-related adverse outcomes.[11]
The administration of blood products might promote tumour growth and spread not only by inducing immune suppression but also facilitating the proliferative and metastatic properties of cancer cells via the action of angiogenic and oncogenic factors accumulated during the period of storage.[12] It has been indicated that during storage, 10-15% of the stored platelets become active and able to release growth factors.[13] TGF-β, is one of the stimulating factors that is found in high levels in platelet concentrates; in vitro studies indicate that when supernatants of stored blood products are added to cultured cancer cells, the growth of these cells is stimulated at a faster rate than those non-treated with supernatant. In a similar manner, the supernatant of stored blood products promoted the cell growth (vascular mimicry) of head and neck cancer cells, which was inhibited when the cancer cells were cultured with anti-VEGF antibody.[14]
In summary, the transfusion of blood products may facilitate cancer growth and spread by a direct effect or indirect effects (immune suppression).
PERIOPERATIVE BLOOD TRANSFUSIONS IN CANCER PATIENTS: THE CLINICAL IMPACT
Several authors have tried to demonstrate causality or association between the administration of blood products in the perioperative period and cancer recurrence or cancer-related mortality. In 2006, a meta-analysis by Amato and Pescatori demonstrated that transfusions of RBCs were an independent factor for colorectal cancer recurrence.[15] More recently, a larger meta-analysis (n = 20,795) that included data from randomized controlled trials and retrospective studies (and a moderate degree of heterogeneity for all outcomes) confirmed the findings reported by Amato and Pescatori. That study showed that transfused patients had higher risk for all-cause mortality (odds ratio [OR]: 1.72), cancer-related mortality (OR: 1.71) and recurrence-metastasis-death (OR: 1.66) compared to non-transfused controls.[1] BTs are also commonly given to patients who undergo liver resections for hepatocellular carcinoma. A recent meta-analysis of retrospectives studies that included data from 5635 patients indicate that patients who received allogeneic RBCs perioperatively had a 16% and 60% higher risk of mortality and cancer recurrence than those non-transfused during the 5 years after surgery. The authors reported that a significant heterogeneity across the studies was found for tumour recurrence but not for mortality.[16] In agreement with the results in colorectal and hepatocarcinoma patients, Yao et al. reported that the relative risk of an adverse outcome (5 years survival) was 2.55 in those patients with ampullary cancer of pancreas who received intraoperative allogeneic BTs compared to non-transfused patients.[17] RBC transfusions are also associated with worse outcomes in lung cancer patients. A meta-analysis (n = 5915) by Luan et al. also found that those patients who received RBCs transfusions had a 25% and 42% increased risk of mortality and cancer recurrence than those not transfused. It is worth noticing that the heterogeneity (I2) across studies was significantly high for both outcomes.[18]
Several retrospective studies have addressed the question of whether BTs are associated with a higher risk of cancer recurrence after prostate cancer surgery. In a recent study, Yeoh et al. reported that patients (n = 379) who received allogeneic non-leucoreduced RBCs perioperatively (mostly post-operatively) did not have a higher risk of systemic progression, prostate cancer-related death or all-cause death than non-transfused patients (n = 758).[19] In a similar manner, Boehm et al. could not find an association between BT and biochemical cancer recurrence.[2] One retrospective study addressed the question of whether the ‘storage age’ of RBCs influenced biochemical recurrence after prostate cancer surgery. The authors could not show an association between the age of the blood and worse oncological outcomes.[20] In patients with renal cancer, the results from the current studies are conflicting.[21,22,23] The largest study (n = 2318), although retrospective, showed an association between allogeneic BT and shorter overall survival, but no change in recurrence-free or cancer-specific survival.[24] The rate of BT during and after cystectomies can be as high as 60%. Three retrospective studies tried to address the possible association between BT and shorter RFS, CSS and/or OS but only two of them demonstrated that patients who were transfused perioperatively had a significantly higher risk for recurrence (hazard ratio [HR]: 1.2), cancer-related mortality (HR: 1.31) and/or all-cause mortality (HR: 1.27) compared with non-transfused patients.[25,26,27]
The results of studies in gynaecological cancers are mixed. Tumour staging or quality of post-operative cytoreduction might be more important predictors of mortality and cancer recurrence than BTs per se. Two retrospective studies have investigated the association between perioperative BTs and ovarian cancer recurrence; in the de Oliveira et al. study the authors found an increase risk (OR: 1.62) for cancer recurrence after allogeneic BT but one argument against this work is that the authors did not adjust for residual disease after surgery.[28] When, the post-operative residual disease was taken into consideration, BTs were not an independent risk factor for cancer recurrence.[29]
Currently, there is no compelling evidence to conclude that the transfusion of FFP or platelet concentrates to patients undergoing cancer surgery worsens oncological outcomes. Only a small retrospective study in which patients were given platelet concentrates during surgery for the hepatic adenocarcinoma had a higher risk of recurrence.
Summarising, perioperative allogeneic BTs are associated with poor oncological outcomes in patients with colorectal, lung and hepatobiliary cancers. It remains controversial in ovarian, renal and bladder cancers. No clear association has been found after prostate cancer surgery.
CONCLUSION
The indications for perioperative administration of blood products in the context of oncological surgery should be targeted to improve the delivery of oxygen and correct clinically relevant abnormalities in the coagulation system. Protocols created by a multidisciplinary team of perioperative physicians with the goal of adequately managing blood product transfusions should be instituted in hospitals that take care of cancer patients. To date, there is not a specific transfusion trigger; however, minimising perioperative blood loss and use of technologies to guide fluid administration and appropriately assess the coagulation system are warranted.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Acheson AG, Brookes MJ, Spahn DR. Effects of allogeneic red blood cell transfusions on clinical outcomes in patients undergoing colorectal cancer surgery: A systematic review and meta-analysis. Ann Surg. 2012;256:235–44. doi: 10.1097/SLA.0b013e31825b35d5. [DOI] [PubMed] [Google Scholar]
- 2.Boehm K, Beyer B, Tennstedt P, Schiffmann J, Budaeus L, Haese A, et al. No impact of blood transfusion on oncological outcome after radical prostatectomy in patients with prostate cancer. World J Urol. 2014 doi: 10.1007/s00345-014-1351-0. [DOI] [PubMed] [Google Scholar]
- 3.Knight K, Wade S, Balducci L. Prevalence and outcomes of anemia in cancer: A systematic review of the literature. Am J Med. 2004;116(Suppl 7A):11S–26S. doi: 10.1016/j.amjmed.2003.12.008. [DOI] [PubMed] [Google Scholar]
- 4.Gilreath JA, Stenehjem DD, Rodgers GM. Diagnosis and treatment of cancer-related anemia. Am J Hematol. 2014;89:203–12. doi: 10.1002/ajh.23628. [DOI] [PubMed] [Google Scholar]
- 5.Wong EY, Rose MG. Why does my patient have thrombocytopenia? Hematol Oncol Clin North Am. 2012;26:231–52. doi: 10.1016/j.hoc.2012.02.006. vii. [DOI] [PubMed] [Google Scholar]
- 6.Thiagarajan P, Afshar-Kharghan V. Platelet transfusion therapy. Hematol Oncol Clin North Am. 2013;27:629–43. doi: 10.1016/j.hoc.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 7.Long K, Meier C, Ward M, Williams D, Woodward J, Bernard A. Immunologic profiles of red blood cells using in vitro models of transfusion. J Surg Res. 2013;184:567–71. doi: 10.1016/j.jss.2013.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guo JR, Xu F, Jin XJ, Shen HC, Liu Y, Zhang YW, et al. Impact of allogenic and autologous transfusion on immune function in patients with tumors. Asian Pac J Cancer Prev. 2014;15:467–74. doi: 10.7314/apjcp.2014.15.1.467. [DOI] [PubMed] [Google Scholar]
- 9.Durante C, Agostini F, Abbruzzese L, Toffola RT, Zanolin S, Suine C, et al. Growth factor release from platelet concentrates: Analytic quantification and characterization for clinical applications. Vox Sang. 2013;105:129–36. doi: 10.1111/vox.12039. [DOI] [PubMed] [Google Scholar]
- 10.Dzik WH, Mincheff M, Puppo F. An alternative mechanism for the immunosuppressive effect of transfusion. Vox Sang. 2002;83(Suppl 1):417–9. doi: 10.1111/j.1423-0410.2002.tb05344.x. [DOI] [PubMed] [Google Scholar]
- 11.Bilgin YM, Brand A. Transfusion-related immunomodulation: A second hit in an inflammatory cascade? Vox Sang. 2008;95:261–71. doi: 10.1111/j.1423-0410.2008.01100.x. [DOI] [PubMed] [Google Scholar]
- 12.Kanter J, Khan SY, Kelher M, Gore L, Silliman CC. Oncogenic and angiogenic growth factors accumulate during routine storage of apheresis platelet concentrates. Clin Cancer Res. 2008;14:3942–7. doi: 10.1158/1078-0432.CCR-07-4824. [DOI] [PubMed] [Google Scholar]
- 13.Anitua E, Andia I, Ardanza B, Nurden P, Nurden AT. Autologous platelets as a source of proteins for healing and tissue regeneration. Thromb Haemost. 2004;91:4–15. doi: 10.1160/TH03-07-0440. [DOI] [PubMed] [Google Scholar]
- 14.Upile T, Jerjes W, Singh S, Al-Khawalde M, Hamdoon Z, Radhi H, et al. The use of specific anti-growth factor antibodies to abrogate the oncological consequences of transfusion in head and neck squamous cell carcinoma: An in vitro study. Head Neck Oncol. 2012;4:22. doi: 10.1186/1758-3284-4-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Amato A, Pescatori M. Perioperative blood transfusions for the recurrence of colorectal cancer. Cochrane Database Syst Rev. 2006:CD005033. doi: 10.1002/14651858.CD005033.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu L, Wang Z, Jiang S, Shao B, Liu J, Zhang S, et al. Perioperative allogenenic blood transfusion is associated with worse clinical outcomes for hepatocellular carcinoma: A meta-analysis. PLoS One. 2013;8:e64261. doi: 10.1371/journal.pone.0064261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yao HS, Wang Q, Wang WJ, Hu ZQ. Intraoperative allogeneic red blood cell transfusion in ampullary cancer outcome after curative pancreatoduodenectomy: A clinical study and meta-analysis. World J Surg. 2008;32:2038–46. doi: 10.1007/s00268-008-9675-9. [DOI] [PubMed] [Google Scholar]
- 18.Luan H, Ye F, Wu L, Zhou Y, Jiang J. Perioperative blood transfusion adversely affects prognosis after resection of lung cancer: A systematic review and a meta-analysis. BMC Surg. 2014;14:34. doi: 10.1186/1471-2482-14-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yeoh TY, Scavonetto F, Weingarten TN, Karnes RJ, van Buskirk CM, Hanson AC, et al. Perioperative allogeneic nonleukoreduced blood transfusion and prostate cancer outcomes after radical prostatectomy. Transfusion. 2014;54:2175–81. doi: 10.1111/trf.12595. [DOI] [PubMed] [Google Scholar]
- 20.Cata JP, Klein EA, Hoeltge GA, Dalton JE, Mascha E, O’Hara J, et al. Blood storage duration and biochemical recurrence of cancer after radical prostatectomy. Mayo Clin Proc. 2011;86:120–7. doi: 10.4065/mcp.2010.0313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Edna TH, Vada K, Hesselberg F, Mjølnerød OK. Blood transfusion and survival following surgery for renal carcinoma. Br J Urol. 1992;70:135–8. doi: 10.1111/j.1464-410x.1992.tb15690.x. [DOI] [PubMed] [Google Scholar]
- 22.Jakobsen EB, Eickhoff JH, Andersen JP, Ottesen M. Perioperative blood transfusion does not affect survival after operation for renal cell cancer. Eur Urol. 1994;26:145–8. doi: 10.1159/000475365. [DOI] [PubMed] [Google Scholar]
- 23.Moffat LE, Sunderland GT, Lamont D. Blood transfusion and survival following nephrectomy for carcinoma of kidney. Br J Urol. 1987;60:316–9. doi: 10.1111/j.1464-410x.1987.tb04975.x. [DOI] [PubMed] [Google Scholar]
- 24.Linder BJ, Thompson RH, Leibovich BC, Cheville JC, Lohse CM, Gastineau DA, et al. The impact of perioperative blood transfusion on survival after nephrectomy for non-metastatic renal cell carcinoma (RCC) BJU Int. 2014;114:368–74. doi: 10.1111/bju.12535. [DOI] [PubMed] [Google Scholar]
- 25.Morgan TM, Barocas DA, Chang SS, Phillips SE, Salem S, Clark PE, et al. The relationship between perioperative blood transfusion and overall mortality in patients undergoing radical cystectomy for bladder cancer. Urol Oncol. 2013;31:871–7. doi: 10.1016/j.urolonc.2011.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jahnson S, Bergström R, Pedersen J. Extent of blood transfusion and cancer-related mortality after cystectomy and urinary diversion for bladder cancer. Br J Urol. 1994;74:779–84. doi: 10.1111/j.1464-410x.1994.tb07125.x. [DOI] [PubMed] [Google Scholar]
- 27.Linder BJ, Frank I, Cheville JC, Tollefson MK, Thompson RH, Tarrell RF, et al. The impact of perioperative blood transfusion on cancer recurrence and survival following radical cystectomy. Eur Urol. 2013;63:839–45. doi: 10.1016/j.eururo.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 28.de Oliveira GS, Jr, Schink JC, Buoy C, Ahmad S, Fitzgerald PC, McCarthy RJ. The association between allogeneic perioperative blood transfusion on tumour recurrence and survival in patients with advanced ovarian cancer. Transfus Med. 2012;22:97–103. doi: 10.1111/j.1365-3148.2011.01122.x. [DOI] [PubMed] [Google Scholar]
- 29.Morgenstern L, Dowdy S, Martin J, Lemens M, McGree M, Weaver A, et al. The impact of perioperative packed red blood cell transfusion on survival in epithelial ovarian cancer. Gynecol Oncol. 2012;127:S27. doi: 10.1097/01.IGC.0000436089.03581.6b. [DOI] [PMC free article] [PubMed] [Google Scholar]


