Abstract
Therapeutic transfusion techniques such as apheresis and phlebotomy are frequently used in intensive care units. Use of the apheresis technique for the treatment of various diseases in critically ill patients is growing day by day. There are increasing evidences for using apheresis as a primary therapy or as an adjunct to other therapies for various diseases such as thrombotic thrombocytopenic purpura, haemolytic uremic syndrome, drug toxicities, autoimmune disease, sepsis and fulminant hepatic failure. Apheresis is an invasive procedure. It has significant physiologic consequences, so the care of these patients requires continuous supervision. Phlebotomy is performed as an intervention for some disease management. Its use is nowadays restricted to conditions such as polycythaemia, haemochromatosis and porphyria cutanea tarda. In this review, we have looked at various indications, procedure and complications of apheresis and phlebotomy in critical care unit.
Keywords: Apheresis, phlebotomy, plasmapheresis
INTRODUCTION
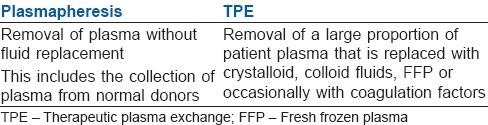
Therapeutic transfusion techniques consist of removal of a blood component from a patient using apheresis technology for removing defective cells or disease mediators. The terminology “Apheresis” stems from Greek verb apairesos or Roman aphairesis meaning to take away by force or withdraw.[1] Apheresis (or Haemapheresis) is the collection of blood from a donor or patient followed by separation and removal of a cellular component(s) and/or plasma and return of the remaining blood components to the donor or patient. Cytapheresis is the procedure by which cellular elements of the blood, platelets, leucocytes, lymphocytes, red blood cells (RBC's), are selectively removed from the blood. Plasmapheresis is a process in which plasma is selectively removed. It is used to collect plasma from healthy donor (without any fluid replacement) or to exchange plasma from a patient to remove a constituent (antibody, immune complexes, inflammatory mediator, paraproteins, lipoproteins and toxins, excess cells) which is causing harm. [Table 1] This allows disease resolution or decrease in morbidity.[1,2] The procedure was first successfully used for the treatment of Waldenstrőm macroglobulinemia in 1959.[3,4] Since then, the efficacy of plasmapheresis has been documented in numerous diseases of various organ systems.
Table 1.
TPE
Sixty three articles were reviewed using keywords such as, therapeutic apheresis, plasmapheresis and therapeutic plasma exchange (TPE), starting from 1952 till date, accessed through search engines PubMed, Google, Google scholar and Medscape.
Role in intensive care unit
Apheresis therapy like plasma exchange and plasma adsorption is emerging as a therapeutic tool in critical care. Apheresis therapy frequently used in intensive care unit (ICU) patients for thrombotic thrombocytopaenic purpura (TTP), haemolytic uraemic syndrome (HUS), autoimmune disease and sepsis. Apheresis therapy is also useful in patients with fulminant hepatic failure for artificial liver support.[2]
Description of apheresis
Apheresis consists of the following:
Circulating blood components can be removed, either cells (cytapheresis) or plasma solutes (plasmapheresis).
-
Circulating substances responsible for certain diseases are removed. Some cells and plasma components are mobilized from their tissue depots and removed.
- Lymphocytes from the spleen and lymph nodes in chronic lymphocytic leukaemia
- Low-density lipoproteins (LDLs) in familial hypercholesterolaemia.
Removal of platelets and lymphocytes.
Reinfusion of a deficient plasma factor as in TTP.
Increases clearance of immune complexes by the spleen, in certain autoimmune disorders.
Types of apheresis
-
Collection of components for transfusion:
- Platelets - Plateletpheresis
- Leucocytes - Leucocytapheresis
- Plasma - Plasmapheresis
- Peripheral blood stem cells (PBSCs)
-
Removal of pathological components, that is, therapeutic apheresis:
- Therapeutic cytapheresis
- TPE.
The procedure involved in apheresis is more extensively used to harvest platelets and plasma from healthy donors than as a therapeutic modality. As a therapeutic procedure, it is not curative and does not change the natural course of the disease; however, it can be life-saving in many situations and buys time to affect more definitive therapy. The main emphasis in this article is on various aspects of therapeutic apheresis.
TECHNICAL ASPECT OF APHERESIS
Apheresis instruments separate the blood into components, then selectively remove one component and return the remaining to the patient. By running this procedure by one or more blood volumes, a significant amount of pathologic components is removed. Anticoagulation of the circuit is required.
Centrifugation apheresis instruments use either a continuous or an intermittent flow method to drive the blood to the separation device. Continuous flow methods draw blood into the extracorporeal circuit, separate blood into components in the centrifugation chamber, channelizes the unwanted portion into a collection bag, and thereafter return the nonpathologic elements back to the patient without interruption. Dual venous access is required for this. Intermittent flow methods have the same steps but with a discrete volume of blood at a time. This takes a longer time but requires only single venous access.[5]
THERAPEUTIC CYTAPHERESIS
The purpose was to deplete over-abundant or abnormal cellular components.
Common indications are as follows:
-
Erythrocytapheresis (the patient's RBCs are removed and replacement with donor red cells if required)
- Sickle cell disease: Goal of exchanging the sickle red cells for red cells containing haemoglobin A is to interrupt the vicious cycle of stasis, sickling and hypoxia. This procedure has also been used prophylactically in pregnancy with sickle cell disease and prior to general anaesthesia in these patients[6]
- Hyperparasitaemia: To lower parasite loads in Malaria, Babesiosis.
-
Leucocytapheresis
- Leukaemia with hyperleucocytosis syndrome: Leukostasis results from microvascular obstruction and may lead to endothelial injury, thrombosis and/or haemorrhage. Once total leucocyte count is above 200,000/mm3 in acute myeloid leukaemia and above 300,000/mm3 in chronic myeloid leukaemia, organ dysfunction is likely:
- Pulmonary dysfunction (hypoxemia, diffuse lung infiltrates)
- Cerebral dysfunction (confusion, mental status changes, altered level of consciousness).
- Extracorporeal photopheresis is also a type of leukopheresis in which the white blood cells are exposed to ultraviolet A light to induce an immunomodulatory effect. It can achieve sustained remission in CTCL.[9]
- PBSC collection
-
Thrombocytapheresis: Acute management of patients with symptomatic thrombocythaemia where a rapid reduction in platelet count is required.
- Thrombocytosis (platelet count > 450,000-500,000/μl) like polycythaemia vera (PV), essential thrombocythaemia, idiopathic myelofibrosis or unclassified myeloproliferative neoplasm, with an acute and severe thrombotic or haemorrhagic event. Platelets are reduced for symptomatic relief while waiting for cytoreductive therapy to take effect.
- Management of peri-operative thrombohaemorrhagic complications in patients with myeloproliferative neoplasms undergoing splenectomy.[12]
- Pregnancy with thrombocythaemia, as drug therapy is contraindicated, and it prevents placental infarction and foetal death.[13]
Therapeutic plasma exchange
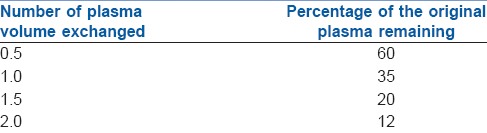
A wide variety of diseases seen in different medical specialties can be treated with TPE and it can be used as a first line of treatment in some diseases (example: TTP or as an adjunct to other therapies (example: Goodpasture syndrome). TPE removes the pathogenic substances such as antibodies, immune complexes, monoclonal proteins, cryoglobulins, lipoproteins, protein-bound toxins and cytokines. Additional evidence suggests that TPE may have an immunomodulatory effect beyond the removal of immunoglobulins (Igs).[14,15] In TPE, two plasma volumes can be exchanged within 3 h and levels of intravascular solutes can be lowered by 50-60% with each exchange. Due to the dilution of the plasma, the substance cannot be removed completely. Treating volumes beyond 1.5 plasma volumes removes smaller amounts of pathologic substance while prolonging the procedure and exposing the patient to more replacement fluid and anticoagulant.
The theoretical efficacy of TPE is shown in Table 2.[2] Role of plasmapheresis in various disease conditions/syndromes are enlisted along with the factors to be removed in each:
Table 2.
Plasma exchange: Theoretical efficiency
Anti-glomerular basement membrane (anti-GBM) disease[16] - Anti GBM antibody
Guillain-Barre syndrome (GBS) - Antimyelin antibody[17]
Hyperviscosity syndrome - IgM
Cryoglobulinemia - Cryoglobulins
Microangiopathic thrombocytopaenia (TTP/HUS) - Von Willebrand factor multimers/anti-endothelial cell antigen[18,19,20]
Homozygous familial hypercholesterolaemia - LDL cholesterol[21]
Myasthenia gravis (MG) crisis - Ach receptor antibody
Coagulation factor inhibitors - Factor VIII inhibitor
Haemolytic disease of newborn - IgM
Overdose of certain drugs - e.g. digitalis (digitalis antibody)
Poisoning involving protein-bound toxins - e.g. Amanita phalloides
In hyperviscosity syndrome, due to monoclonal gammopathies, TPE is particularly effective as IgM is largely distributed in the intravascular compartment. Reduction in viscosity can be achieved even with the exchange of as little as 500-1000 ml of plasma by manual bag techniques, which relieves both haemorrhagic and ischemic symptoms.
Therapeutic plasma exchange is a therapy of choice for TTP, if not available temporarily, plasma infusion can be given till transfer to an appropriate facility. Results with TPE are better due to two-fold action of TPE: Removal of IgM autoantibody which acts as a specific protease inhibitor and replacement of deficient factors.[18,19,20]
In familial hypercholesterolaemia, chronic TPE can reduce total plasma LDL levels and lead to regression of atherosclerotic changes in blood vessels and promotes resorption of xanthomas and atheromas.[21] LDL levels are reduced to more than 50%. VLDL and triglyceride levels are also reduced, but HDL is spared. In Refsum's disease, removal of phytanic acid by TPE helps prevent or reverse the neurological manifestations.[22] In cold agglutinin-induced autoimmune haemolytic anaemia (AIHA), TPE is useful in a reduction of haemolysis as antibody titres falls. In warm antibody (IgG) AIHA, TPE is used as an adjunct to therapy with intravenous Ig (IVIG) and/or cyclophosphamide in refractory cases. In haemophiliacs, development of both auto and allo-antibodies is a major therapeutic challenge. These patients have to undergo surgery after achieving adequate factor VIII levels which are difficult due to the presence of coagulation factor inhibitors. TPE has an important role in removing these. In ABO incompatible marrow transplants, the alloantibodies to RBCs can be removed by TPE.[23] In Rh-negative pregnant women, maternal IgG antibodies to the foetus can lead to destruction of foetal red cells. TPE can help remove these antibodies.
Therapeutic plasma exchange is used in the treatment of neuro-immunological diseases such as GBS, chronic inflammatory demyelinating polyneuropathy (CIDP), MG and Lambert-Eaton syndrome. Antibodies responsible for these diseases are effectively removed by TPE and help in the amelioration of the disease.[17,24] The efficacy of plasmapheresis or administration of IVIG appears to be equal in GBS, AIDP and CIDP.[25,26] In MG, plasmapheresis is reserved for myasthenic crisis and refractory cases.
In Goodpasture syndrome, early institution of TPE and cyclophosphamide is very effective.[16] Plasmapheresis causes removal of anti-GBM antibodies after diagnosis by renal biopsy or detection of anti-GBM antibodies.[27] Systemic lupus erythematosus with nephritis does not respond well by adding TPE to cyclophosphamide.[28] TPE has been beneficial in rapidly progressive glomerulonephritis with dialysis dependent renal failure.[29]
The disease/disorders treated with TPE that have been categorized by the American Society for Apheresis are enlisted in Appendix 1.[30]
PROCEDURE CONSIDERATIONS
Replacement fluid
In most cell collection and cell depletion procedures, no replacement fluid beyond the anticoagulant and saline priming solution is required. But in plasma exchange, 1-1.5 plasma volumes are typically removed, and replacement of intravascular volume is necessary. The main goal of replacement fluid is to maintain intravascular volume, maintenance of colloid oncotic pressure and electrolyte balance and restoration of deficient factors. The solutions used are 5% serum albumin, plasma, starches and crystalloids.
Vascular access
Vascular access through peripheral vein is the preferred route as it is associated with fewer infectious, haemorrhagic and thrombotic complications. When frequent procedures over a prolonged period are required, a double lumen central venous catheter designed for apheresis or haemodialysis should be inserted.
COMPLICATIONS
The rate of complication is variable, and ranges from 4% to 36% but most of the events are mild and easily treatable. Estimated mortality is 3 in 10,000 procedures, and most reported deaths have been due to cardiac and respiratory causes in critically ill patients.[31] The most common adverse effect of apheresis is symptomatic hypocalcaemia due to infusion calcium chelating citrate ions in the anticoagulants. Hypotension occurs in 0.5-2.9% cases.[32] Citrate toxicity occurs in approximately 0.8-1.2% cases.[33]
Complications related to vascular access account for about 1% and include haematoma, pneumothorax, bleeding, thrombosis and infection. Haemostatic alterations and bleeding may occur in patients with baseline coagulopathy or severe thrombocytopaenia. Furthermore, there is depletion of coagulation factors during large volume plasma exchanges, wherein depletion of approximately 25-45% can occur.[34] There is also depletion of platelets and fibrinogen.
Other effects
Additional substances removed include inhibitors of coagulation[32] and the pseudocholinesterase necessary for the metabolism of some drugs.[35] Removal of inhibitors of coagulation could predispose patients to thrombosis. Prolongation of actions of neuromuscular blocking drugs has been seen due to reduced activity of the enzymes after TPE. It can also remove drugs which are highly protein bound. Hence, caution is adviced if patient is on life-saving drugs.
PHLEBOTOMY
Phlebotomy (also known as bloodletting) means the removal of blood from the body. Therapeutic phlebotomy is the treatment of choice for blood disorders in which the removal of RBCs or serum iron is the most efficient method of managing disease symptoms and complications. Currently, therapeutic phlebotomy is approved for three main indications: Haemochromatosis, polycythaemia and porphyria cutanea tarda.
Polycythaemia
Polycythaemia is a disorder where too many red cells are produced in bone marrow, which increase the blood volume and viscosity. There is also increase in platelet and white cell production. Patient with polycythaemia tends to develop thrombotic events such as cerebrovascular, cardiovascular accidents and arterial and venous thromboembolism. In primary polycythaemia (PV), one of the major goals of treatment is to reduce these thrombotic events. PV study group prospective trial suggests that patients treated with phlebotomy had a lower incidence of haematological malignancies and solid tumours. Some studies showed that patients maintained at a target haematocrit of <45% had a significantly lower rate of cardiovascular morbidity and major thrombosis.[36,37]
Phlebotomy can be performed in hypoxic conditions such as chronic lung diseases and cyanotic heart disease. Patients with hypoxic pulmonary disease who have hyperviscosity symptoms or a haematocrit >56% should have phlebotomy to reduce this to 50-52%,[38,39,40] AHA recommends performing therapeutic phlebotomy for symptomatic patients of cyanotic congenital heart disease like Eisenmenger's syndrome or tetralogy of Fallot with haemoglobin >20 g/dl and haematocrit >65%.[41]
Haemochromatosis
Phlebotomy does not improve haemochromatosis clinically, but prevents complications in symptomatic patients or those who have already developed end-organ damage, with a serum ferritin > 300 μg/L for men or post-menopausal women and >200 μg/L for pregnant females.[42] Phlebotomy sessions are continued until the serum ferritin concentration drops to <50 ng/ml and transferrin saturation is <50%.[43]
Porphyris cutanea tarda
Porphyria cutanea tarda is caused by uroporphyrinogen decarboxylase deficiency leading to the accumulation of uroporphyrinogen. Therapeutic phlebotomy is the treatment of choice with hydroxychloroquine as a good alternative.[44] Phlebotomy sessions are repeated every 2 weeks until the haemoglobin level is below 20 ng/ml.[45] Some studies showed potential for erythrocyte apheresis as a replacement for standard phlebotomy.[46]
Therapeutic transfusion techniques such as therapeutic cytapheresis, plasmapheresis and phlebotomy are an integral part of ICU procedures, which require intensive monitoring and supervision. There are numerous conditions where this procedure is performed, but decisions should be individualised for optimum use of resources.
APPENDIX
Appendix 1: Disease conditions enlisted as Category 1-4
Category 1
Apheresis as primary therapy or first line adjunct to other therapy.
Examples:
Thrombotic thrombocytopenic purpura
Haemolytic uraemic syndrome atypical
Acute inflammatory demyelinating polyradiculopathy (Guillain- Barre syndrome)
Anti neutrophil cytoplasmic antibodies associated rapidly progressive glomerulonephritis/vasculitis
(Wegener granulomatosis)
Antiglomerular basement membrane disease (Goodpasture syndrome)
Chronic inflammatory demyelinating polyradiculopathy
Paraproteinemic demyelinating polyneuropathies (IgG, IgM, IgA)
Paediatric autoimmune neuropsychiatric disorders associated with
Streptococcal infections (PANDAS)
Renal transplantation, Ab mediated rejection
Myasthenia gravis
Polycythaemia vera
Sickle cell disease with acute stroke
Category 2
Apheresis is used as second line therapy for some disease conditions.
Examples:
ABO incompatible haematopoietic stem cell transplantation
ABO incompatible solid organ transplantation (heart, kidney)
Cold agglutinin autoimmune haemolytic anaemia
Catastrophic antiphospholipid Ab syndrome
Chronic focal encephalitis (Rasmussen encephalitis)
Multiple sclerosis
Phytanic acid storage disease (Refsum disease)
Red blood cell alloimmunization in pregnancy
Renal transplantation desensitization
Category 3
This includes diseases for which adequate role of apheresis is not established, and treatment with apheresis is individualized.
Examples:
ABO incompatible liver transplantation, aplastic anaemia, warm agglutinin autoimmune haemolytic anaemia, hypertriglyceridemic pancreatitis, multiple myeloma, sepsis with multiorgan failure, thyroid storm
Category 4
This category includes diseases in which apheresis is ineffective or harmful.
Examples:
Dialysis dependent Goodpasture syndrome, scleroderma, amyloidosis, amyotrophic lateral sclerosis, polymyositis, psoriasis
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Nair V. Apheresis. In: Choudhry VP, Saxena R, Pati HP, editors. Recent Advances in Haematology. Ch. 3. New Delhi: JayPee Brothers Medical Publishers (P) Ltd; 2004. pp. 56–9. [Google Scholar]
- 2.Hirasawa H, Sugai T, Oda S, Shiga H, Matsuda K, Ueno H, et al. Efficacy and limitation of apheresis therapy in critical care. Ther Apher. 1997;1:228–32. doi: 10.1111/j.1744-9987.1997.tb00143.x. [DOI] [PubMed] [Google Scholar]
- 3.Solomon A, Fahey JL. Plasmapheresis therapy in macroglobulinemia. Ann Intern Med. 1963;58:789–800. doi: 10.7326/0003-4819-58-5-789. [DOI] [PubMed] [Google Scholar]
- 4.Adams WS, Blahd WH, Bassett SH. A method of human plasmapheresis. Proc Soc Exp Biol Med. 1952;80:377–9. doi: 10.3181/00379727-80-19629. [DOI] [PubMed] [Google Scholar]
- 5.Burgstaler EA. Current instrumentation for apheresis. In: McLeod BC, Price TH, Weinstein R, editors. Apheresis: Principle and Practice. 2nd ed. Bethesda, MD: AABB; 2003. pp. 95–130. [Google Scholar]
- 6.Koshy M, Weiner SJ, Miller ST, Sleeper LA, Vichinsky E, Brown AK, et al. Surgery and anesthesia in sickle cell disease. Cooperative Study of Sickle Cell Diseases. Blood. 1995;86:3676–84. [PubMed] [Google Scholar]
- 7.Edelson R, Facktor M, Andrews A, Lutzner M, Schein P. Successful management of the Sézary syndrome. Mobilization and removal of extravascular neoplastic T cells by leukapheresis. N Engl J Med. 1974;291:293–4. doi: 10.1056/NEJM197408082910608. [DOI] [PubMed] [Google Scholar]
- 8.Bongiovanni MB, Katz RS, Tomaszewski JE, Ziselman EM, Goldwein MI, Wurzel HA. Cytapheresis in a patient with Sezary syndrome. Transfusion. 1981;21:332–4. doi: 10.1046/j.1537-2995.1981.21381201808.x. [DOI] [PubMed] [Google Scholar]
- 9.Lim HW, Edelson RL. Photopheresis for the treatment of cutaneous T-cell lymphoma. Hematol Oncol Clin North Am. 1995;9:1117–26. [PubMed] [Google Scholar]
- 10.Pineda AA, Brzica SM, Jr, Taswell HF. Continuous- and semi-continuous-flow blood centrifugation systems: Therapeutic applications, with plasma-, platelet-, lympha-, and eosinapheresis. Transfusion. 1977;17:407–16. doi: 10.1046/j.1537-2995.1977.17578014576.x. [DOI] [PubMed] [Google Scholar]
- 11.Taft EG. Apheresis in platelet disorder. Plasma Ther. 1982;2:181. [Google Scholar]
- 12.Mesa RA, Nagorney DS, Schwager S, Allred J, Tefferi A. Palliative goals, patient selection, and perioperative platelet management: Outcomes and lessons from 3 decades of splenectomy for myelofibrosis with myeloid metaplasia at the Mayo Clinic. Cancer. 2006;107:361–70. doi: 10.1002/cncr.22021. [DOI] [PubMed] [Google Scholar]
- 13.Mercer B, Drouin J, Jolly E, d’Anjou G. Primary thrombocythemia in pregnancy: A report of two cases. Am J Obstet Gynecol. 1988;159:127–8. doi: 10.1016/0002-9378(88)90507-8. [DOI] [PubMed] [Google Scholar]
- 14.Kambara C, Matsuo H, Fukudome T, Goto H, Shibuya N. Miller Fisher syndrome and plasmapheresis. Ther Apher. 2002;6:450–3. doi: 10.1046/j.1526-0968.2002.00466.x. [DOI] [PubMed] [Google Scholar]
- 15.Shariatmadar S, Nassiri M, Vincek V. Effect of plasma exchange on cytokines measured by multianalyte bead array in thrombotic thrombocytopenic purpura. Am J Hematol. 2005;79:83–8. doi: 10.1002/ajh.20342. [DOI] [PubMed] [Google Scholar]
- 16.Kalluri R, Gunwar S, Reeders ST, Morrison KC, Mariyama M, Ebner KE, et al. Goodpasture syndrome. Localization of the epitope for the autoantibodies to the carboxyl-terminal region of the alpha 3(IV) chain of basement membrane collagen. J Biol Chem. 1991;266:24018–24. [PubMed] [Google Scholar]
- 17.Connolly AM, Pestronk A, Trotter JL, Feldman EL, Cornblath DR, Olney RK. High-titer selective serum anti-beta-tubulin antibodies in chronic inflammatory demyelinating polyneuropathy. Neurology. 1993;43:557–62. doi: 10.1212/wnl.43.3_part_1.557. [DOI] [PubMed] [Google Scholar]
- 18.Rock GA, Shumak KH, Buskard NA, Blanchette VS, Kelton JG, Nair RC, et al. Comparison of plasma exchange with plasma infusion in the treatment of thrombotic thrombocytopenic purpura. Canadian Apheresis Study Group. N Engl J Med. 1991;325:393–7. doi: 10.1056/NEJM199108083250604. [DOI] [PubMed] [Google Scholar]
- 19.Furlan M, Robles R, Galbusera M, Remuzzi G, Kyrle PA, Brenner B, et al. von Willebrand factor-cleaving protease in thrombotic thrombocytopenic purpura and the hemolytic-uremic syndrome. N Engl J Med. 1998;339:1578–84. doi: 10.1056/NEJM199811263392202. [DOI] [PubMed] [Google Scholar]
- 20.Tsai HM, Lian EC. Antibodies to von Willebrand factor-cleaving protease in acute thrombotic thrombocytopenic purpura. N Engl J Med. 1998;339:1585–94. doi: 10.1056/NEJM199811263392203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ginsberg HN. Update on the treatment of hypercholesterolemia, with a focus on HMG-CoA reductase inhibitors and combination regimens. Clin Cardiol. 1995;18:307–15. doi: 10.1002/clc.4960180605. [DOI] [PubMed] [Google Scholar]
- 22.Gibberd FB. Plasma exchange for Refsum's disease. Transfus Sci. 1993;14:23–6. doi: 10.1016/0955-3886(93)90049-Z. [DOI] [PubMed] [Google Scholar]
- 23.Bensinger WI, Baker DA, Buckner CD, Clift RA, Thomas ED. In vitro and in vivo removal of anti-A erythrocyte antibody by adsorption to a synthetic immunoadsorbent. Transfusion. 1981;21:335–42. doi: 10.1046/j.1537-2995.1981.21381201809.x. [DOI] [PubMed] [Google Scholar]
- 24.Seybold ME. Plasmapheresis in myasthenia gravis. Ann N Y Acad Sci. 1987;505:584–7. doi: 10.1111/j.1749-6632.1987.tb51326.x. [DOI] [PubMed] [Google Scholar]
- 25.Dalakas MC. Intravenous immunoglobulin in the treatment of autoimmune neuromuscular diseases: Present status and practical therapeutic guidelines. Muscle Nerve. 1999;22:1479–97. doi: 10.1002/(sici)1097-4598(199911)22:11<1479::aid-mus3>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 26.Jayasena YA, Mudalige SP, Manchanayake GS, Dharmapala HL, Kumarasiri RP, Weerasinghe VS, et al. Physiological changes during and outcome following ’filtration’ based continuous plasma exchange in Guillain Barre Syndrome. Transfus Apher Sci. 2010;42:109–13. doi: 10.1016/j.transci.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 27.Levy JB, Turner AN, Rees AJ, Pusey CD. Long-term outcome of anti-glomerular basement membrane antibody disease treated with plasma exchange and immunosuppression. Ann Intern Med. 2001;134:1033–42. doi: 10.7326/0003-4819-134-11-200106050-00009. [DOI] [PubMed] [Google Scholar]
- 28.Lewis EJ, Hunsicker LG, Lan SP, Rohde RD, Lachin JM. A controlled trial of plasmapheresis therapy in severe lupus nephritis. The Lupus Nephritis Collaborative Study Group. N Engl J Med. 1992;326:1373–9. doi: 10.1056/NEJM199205213262101. [DOI] [PubMed] [Google Scholar]
- 29.Pusey CD, Rees AJ, Evans DJ, Peters DK, Lockwood CM. Plasma exchange in focal necrotizing glomerulonephritis without anti-GBM antibodies. Kidney Int. 1991;40:757–63. doi: 10.1038/ki.1991.272. [DOI] [PubMed] [Google Scholar]
- 30.Schwartz J, Winters JL, Padmanabhan A, Balogun RA, Delaney M, Linenberger ML, et al. Guidelines on the use of therapeutic apheresis in clinical practice-evidence-based approach from the Writing Committee of the American Society for Apheresis: The sixth special issue. J Clin Apher. 2013;28:145–284. doi: 10.1002/jca.21276. [DOI] [PubMed] [Google Scholar]
- 31.Sutton DM, Nair RC, Rock G. Complications of plasma exchange. Transfusion. 1989;29:124–7. doi: 10.1046/j.1537-2995.1989.29289146829.x. [DOI] [PubMed] [Google Scholar]
- 32.Bramlage CP, Schröder K, Bramlage P, Ahrens K, Zapf A, Müller GA, et al. Predictors of complications in therapeutic plasma exchange. J Clin Apher. 2009;24:225–31. doi: 10.1002/jca.20217. [DOI] [PubMed] [Google Scholar]
- 33.McLeod BC, Sniecinski I, Ciavarella D, Owen H, Price TH, Randels MJ, et al. Frequency of immediate adverse effects associated with therapeutic apheresis. Transfusion. 1999;39:282–8. doi: 10.1046/j.1537-2995.1999.39399219285.x. [DOI] [PubMed] [Google Scholar]
- 34.Chirnside A, Urbaniak SJ, Prowse CV, Keller AJ. Coagulation abnormalities following intensive plasma exchange on the cell separator. II. Effects on factors I, II, V, VII, VIII, IX, X and antithrombin III. Br J Haematol. 1981;48:627–34. doi: 10.1111/j.1365-2141.1981.00627.x. [DOI] [PubMed] [Google Scholar]
- 35.Naik B, Hirshhorn S, Dharnidharka VR. Prolonged neuromuscular block due to cholinesterase depletion by plasmapheresis. J Clin Anesth. 2002;14:381–4. doi: 10.1016/s0952-8180(02)00382-3. [DOI] [PubMed] [Google Scholar]
- 36.Marchioli R, Finazzi G, Specchia G, Masciulli A, Mennitto MR, Barbui T. The CYTO-PV: A Large-Scale Trial Testing the Intensity of CYTOreductive Therapy to Prevent Cardiovascular Events in Patients with Polycythemia Vera. Thrombosis 2011. 2011:794240. doi: 10.1155/2011/794240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marchioli R, Finazzi G, Specchia G, Cacciola R, Cavazzina R, Cilloni D, et al. Cardiovascular events and intensity of treatment in polycythemia vera. N Engl J Med. 2013;368:22–33. doi: 10.1056/NEJMoa1208500. [DOI] [PubMed] [Google Scholar]
- 38.Bornstein R, Menon D, York E, Sproule B, Zak C. Effects of venesection on cerebral function in chronic lung disease. Can J Neurol Sci. 1980;7:293–6. doi: 10.1017/s0317167100022770. [DOI] [PubMed] [Google Scholar]
- 39.Chetty KG, Light RW, Stansbury DW, Milne N. Exercise performance of polycythemic chronic obstructive pulmonary disease patients. Effect of phlebotomies. Chest. 1990;98:1073–7. doi: 10.1378/chest.98.5.1073. [DOI] [PubMed] [Google Scholar]
- 40.Piccirillo G, Fimognari FL, Valdivia JL, Marigliano V. Effects of phlebotomy on a patient with secondary polycythemia and angina pectoris. Int J Cardiol. 1994;44:175–7. doi: 10.1016/0167-5273(94)90023-x. [DOI] [PubMed] [Google Scholar]
- 41.Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA, et al. ACC/AHA 2008 Guidelines for the Management of Adults with Congenital Heart Disease: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to develop guidelines on the management of adults with congenital heart disease) Circulation. 2008;118:e714–833. doi: 10.1161/CIRCULATIONAHA.108.190690. [DOI] [PubMed] [Google Scholar]
- 42.Andersen RV, Tybjaerg-Hansen A, Appleyard M, Birgens H, Nordestgaard BG. Hemochromatosis mutations in the general population: Iron overload progression rate. Blood. 2004;103:2914–9. doi: 10.1182/blood-2003-10-3564. [DOI] [PubMed] [Google Scholar]
- 43.Adams PC, Barton JC. How I treat hemochromatosis. Blood. 2010;116:317–25. doi: 10.1182/blood-2010-01-261875. [DOI] [PubMed] [Google Scholar]
- 44.Ramsay CA, Magnus IA, Turnbull A, Baker H. The treatment of porphyria cutanea tarda by venesection. Q J Med. 1974;43:1–24. [PubMed] [Google Scholar]
- 45.Rocchi E, Gibertini P, Cassanelli M, Pietrangelo A, Borghi A, Ventura E. Serum ferritin in the assessment of liver iron overload and iron removal therapy in porphyria cutanea tarda. J Lab Clin Med. 1986;107:36–42. [PubMed] [Google Scholar]
- 46.ClinicalTrials.gov. Erythrocyte Apheresis Versus Phlebotomy in Hemochromatosis. [Last Updated on 2007 Jul 27]. Available from: http://www.clinicaltrials.gov/ct2/show/NCT00509652 .


