Abstract
Background
Fuchs endothelial dystrophy (FED) is a condition in which there is premature degeneration of corneal endothelial cells. When the number of endothelial cells is reduced to a significant degree, fluid begins to accumulate within the cornea. As a result, the cornea loses its transparency and the individual suffers a reduction in vision. The only successful surgical treatment for this condition is replacement of part or all of the cornea with healthy tissue from a donor. The established procedure, penetrating keratoplasty (PKP), has been used for many years and its safety and efficacy are well known. Endothelial keratoplasty (EK) techniques are relatively new surgical procedures and their safety and efficacy relative to PKP are uncertain.
Objectives
The objective of this review was to compare the benefits and complications related to two surgical methods (EK and PKP) of replacing the diseased endothelial layer of the cornea with a healthy layer in people with FED.
Search methods
We searched CENTRAL (which contains the Cochrane Eyes and Vision Group Trials Register) (The Cochrane Library 2014, Issue 1), MEDLINE (January 1950 to January 2014), EMBASE (January 1980 to January 2014), Latin American and Caribbean Health Sciences Literature Database (LILACS) (January 1982 to January 2014), the metaRegister of Controlled Trials (mRCT) (www.controlled‐trials.com) and ClinicalTrials.gov (www.clinicaltrials.gov). There were no date or language restrictions in the electronic searches for trials. The electronic databases were last searched on 27 January 2014.
Selection criteria
We included all randomised controlled trials (RCTs) comparing EK versus PKP for people (of any age and gender) who had been clinically diagnosed with FED.
Data collection and analysis
Two authors independently screened the search results, assessed trial quality and extracted data using the standard methodological procedures expected by The Cochrane Collaboration.
Main results
We included three RCTs that enrolled a total of 139 eyes of 136 participants and analysed 123 (88%) eyes. Two RCTs randomised eyes into either the endothelial keratoplasty (EK) group or penetrating keratoplasty (PKP) group and one RCT randomised eyes into either the femtosecond laser‐assisted endothelial keratoplasty (FLEK) group or PKP group. The RCTs comparing EK with PKP did not show any significant differences between procedures with respect to best corrected visual acuity (BCVA) at two years (mean difference (MD) 0.14 logMAR; 95% confidence interval (CI) ‐0.08 to 0.36; P = 0.23) or at one year (MD 0.09 logMAR; 95% CI ‐0.05 to 0.23; P = 0.22), whereas the trial comparing FLEK with PKP showed significantly better BCVA after PKP (MD 0.20 logMAR; 95% CI 0.10 to 0.30; P = 0.0001). Only one RCT reported on irregular astigmatism (higher‐order aberration), which was less with EK than PKP (MD ‐1.20 µm; 95% CI ‐1.53 to ‐0.87; P < 0.001). Only one RCT reported on endothelial cell counts (lower after FLEK than PKP: MD ‐969 cells/mm²; 95% CI ‐1161 to ‐777; P < 0.001), primary graft failure (higher after FLEK than PKP: RR 7.76; 95% CI 0.41 to 145.22; P = 0.10), and graft rejection (more after FLEK than PKP: RR 1.11; 95% CI 0.07 to 17.12; P = 0.94). Only one RCT reported that 27.8% of participants had graft dislocation, 2.8% had epithelial ingrowth and postoperative pupillary block, and 13.9% had intraocular pressure (IOP)‐related problems in the FLEK group compared with the PKP group, in whom 10% had suture‐related problems, 5% had wound dehiscence and 10% had suture revision to correct astigmatism. Overall, the adverse events in the FLEK group appeared to be more frequent than in the PKP group. No trials reported information about quality of life or economic data. The overall methodological quality of the three trials was not satisfactory as most did not perform allocation concealment or masking of participants and outcome assessors, and all trials had a small sample size.
Authors' conclusions
The rapid growth of endothelial keratoplasty as the treatment of choice for FED is based upon the belief that visual recovery is more rapid, surgically induced astigmatism (regular and irregular) is less and rates of transplant rejection are lower with EK. This change in practice also assumes that the rates of long term transplant survival are equal for the two procedures. The practical differences between the surgical procedures mean that visual recovery is inherently more rapid following EK, but this review found no strong evidence from RCTs of any difference in the final visual outcome between EK and PKP for people with FED. This review also found that higher order aberrations are fewer following EK but endothelial cell loss is greater following EK. The RCTs that we included employed different EK techniques, which may have a bearing on these findings. EK procedures have evolved over the years and can be performed using different techniques, for example deep lamellar endothelial keratoplasty, Descemets stripping endothelial keratoplasty (DSEK), Descemets stripping automated endothelial keratoplasty (DSAEK), femtosecond laser‐assisted endothelial keratoplasty and Descemet membrane endothelial keratoplasty (DMEK). More RCTs are needed to compare PKP with commonly performed EK procedures such as DSEK, DSAEK and DMEK in order to determine the answers to two key questions, whether there is any difference in the final visual outcome between these techniques and whether there are differences in the rates of graft survival in the long term?
Plain language summary
Endothelial keratoplasty versus penetrating keratoplasty for Fuchs endothelial dystrophy
Review question
We compared the benefits and harms of penetrating keratoplasty (PKP) and endothelial keratoplasty (EK) in people with Fuchs endothelial dystrophy (FED) to determine whether one is more effective or safer than the other.
Background
The innermost layer (endothelial cell layer) of the cornea (transparent front of the eye) is essential for maintaining corneal transparency by pumping fluid out and preventing swelling, which leads to opacification. FED is a disease caused by premature degeneration of the endothelial cells leading to fluid in the cornea (oedema), blisters on the surface of the eye (bullous keratopathy) and blurred vision. Severe cases can be treated by corneal transplants, which can be broadly classified into the two types of procedures of PKP (the central cornea is replaced using full thickness corneal tissue from a deceased donor) and EK (where only the innermost layer of the cornea is transplanted).
The EK procedure can be performed using several methods such as deep lamellar endothelial keratoplasty (DLEK), Descemet's stripping endothelial keratoplasty (DSEK), Descemet's stripping automated endothelial keratoplasty (DSAEK) or femtosecond laser‐assisted endothelial keratoplasty (FLEK).
Study characteristics
We found three randomised controlled trials that compared EK with PKP, one of which used the FLEK method. The evidence was current to January 2014. The three trials enrolled a total of 139 eyes of 136 participants, of which 123 eyes were included in the final analyses. The trial on FLEK and PKP was conducted from 2005 to 2007 in the Netherlands; the other two trials were conducted in the United States and were reported in 2008 and 2009 but the study dates were not specified. Over 70% of the included participants were diagnosed with FED, and the remaining participants had other ocular conditions.
Key results
There was no difference in best corrected visual acuity (BCVA) between the two groups in one study at 12 months and another at 24 months. Chances of having an irregular shape of the front of the cornea (astigmatism) was less but endothelial cell loss was higher following EK procedures than after PKP. Only one trial reported harms of the interventions, and indicated that FLEK may result in slightly more complications than PKP (for example, 8% graft failure in the FLEK group versus none in the PKP group; and 3% graft rejection in the FLEK group versus 2% in the PKP group). No trials reported information about quality of life or economic data.
Quality of the evidence
The quality of the evidence was not high due to some limitations with the study designs and because all trials had small numbers of participants with FED.
Background
Description of the condition
The cornea is the transparent tissue at the front of the eye. It is a critical component of the eye for vision as the cornea not only constitutes a clear window for the light rays to reach the retina but also provides most of the refractive power of the eye (Ayres 2006). It consists of five layers, the epithelium, the Bowman's membrane, the stroma, the Descemet's membrane and the endothelium (from the outer towards the inner surface). The clarity of the cornea is of utmost importance to provide a clear visual image; the endothelial cells of the cornea play a vital role in maintaining corneal transparency. They continuously pump fluid out of the cornea and hence keep it in a dehydrated and transparent state.
Fuchs endothelial dystrophy (FED), first described by Ernst Fuchs in 1910, is a condition in which there is premature degeneration of endothelial cells. When endothelial cells are affected in sufficient numbers, fluid begins to accumulate within the cornea. As a result, the cornea loses its transparency and the patient suffers a reduction in vision (Borboli 2002). The condition commonly affects individuals in the fifth and sixth decade of life (Afshari 2006). It affects both eyes although at its onset it is typically asymmetrical. Fuchs endothelial dystrophy occurs more commonly in females compared to males and can be inherited in an autosomal dominant fashion, although not all cases are familial (Cross 1971; Magovern 1979; Rosenblum 1980). The condition is progressive and irreversible.
Description of the intervention
Treatment for FED varies according to the severity of the disease and may range from hypertonic saline drops to surgical intervention. In moderate or severe disease, corneal grafting may be required for visual rehabilitation. For the past 50 years, penetrating keratoplasty (PKP) has been the gold standard surgical procedure for patients with corneal endothelial failure because of FED.
Fuchs endothelial dystrophy accounts for 26% of all corneal transplants in North America (Afshari 2006; Al‐Yousuf 2004; Dobbins 2000; 2012 Report ‐ Eye Bank Association of America). PKP, also known as a full thickness corneal transplant, is a procedure whereby a central circular section between 7.0 mm and 8.5 mm in diameter and spanning the full thickness of the abnormal cornea is removed and replaced with a corresponding full thickness piece of cornea obtained from a cadaveric donor. Although PKP is the gold standard technique for the surgical management of FED, it is not without its drawbacks. Whilst PKP can result in an optically transparent cornea, the cornea may have large amounts of astigmatism or other large refractive errors that require the patient to undergo further surgical procedures for correction, or to wear contact lenses. Indeed, various studies report that 50% of patients require contact lenses to achieve useful vision after PKP (Ing 1998; Muraine 2003; Price FW March 1991; Tuft 1995). Patients with bilateral disease must therefore wait a long time for treatment in the second eye. A second drawback of PKP is that visual recovery can take up to 24 months (Claesson 2002). Before commencing treatment of the second eye, the visual rehabilitation in the first operated eye must be at a sufficient level for the individual to be able to function with that eye alone. In the developing world, these problems are compounded by high rates of suture‐related complications and corneal transplant failure (Dandona 1997). Late rupture of wounds is also a serious risk (Lam 2007).
Given these drawbacks of PKP, there has been much research into a method for replacing only the endothelial layer of the cornea, without disturbing the other corneal layers. Such a treatment could potentially avoid many of the problems associated with PKP and still deliver excellent visual results for patients with FED. A new subset of corneal transplant techniques called endothelial keratoplasty (EK) has evolved. In EK only the inner‐most layer of the cornea is replaced during surgery. Various subtypes of EK have been described such as deep lamellar endothelial keratoplasty (DLEK), Descemet’s stripping endothelial keratoplasty (DSEK), Descemet's stripping automated endothelial keratoplasty (DSAEK), Descemet's membrane endothelial keratoplasty (DMEK) and femtosecond laser‐assisted endothelial keratoplasty (FLEK). These EK subtypes differ surgically, each with its own pros and cons. The expected benefits of any subtype of the EK technique over PKP are faster visual recovery, less astigmatism and stronger wound integrity (Terry 2001). Graft rejection is an important reason for failure in PKP patients (Pineros 1996a). Theoretically, there is also less risk of immune rejection of the transplanted corneal tissue with EK because a smaller amount of tissue is transplanted and because the endothelium is located in what is normally an immune privileged location. Finally, with EK there is the potential to make more efficient use of transplant tissue, using the posterior layer of the donor cornea for EK in one patient and the anterior layers for an anterior lamellar graft in another patient (Melles 1998).
How the intervention might work
As the cornea ages, there is a gradual decline in the number of endothelial cells that line the inner surface of the cornea. Normally this age‐related gradual decline does not affect the corneal clarity. In FED, the rate at which endothelial cells die is greatly accelerated. The role of endothelial cells is to stop fluid gathering in the cornea and causing corneal swelling. Endothelial cells cannot regenerate so cell death in FED results in corneal swelling, that is corneal oedema, which causes blurring of vision. The fluid in the cornea causes bullae (small blisters on the surface of the cornea) which may rupture causing pain. Medical management of the corneal oedema is limited to regular use of lubrication, hyper‐osmolar agents (such as sodium chloride 5% ointment) and bandage contact lenses that reduce the pain due to rupturing of surface bullae. When the condition becomes intolerable for the patient then corneal transplantation is the treatment of choice. This surgical procedure can restore the vision or alleviate the symptoms, or both. The current surgical options for corneal transplantation are PKP and EK.
For the past 50 years, PKP has been the gold standard surgical procedure for patients with corneal endothelial failure because of FED. In PKP the entire cornea is replaced with a cornea from a deceased donor. EK is a newer surgical procedure that replaces only the inner layer of the cornea. This procedure can be performed through relatively small incisions and does not require the eye to be opened completely. Therefore this procedure may cause fewer serious sight threatening complications intraoperatively (such as suprachoroidal hemorrhage) than PKP. The aim of both procedures is to transplant a healthy endothelial cell layer that will pump the fluid out of the cornea and result in restoration of corneal clarity and improvement in vision (Terry 2003).
Why it is important to do this review
Fuchs endothelial dystrophy (FED) is the indication for up to a quarter of all PKPs performed (Afshari 2006). It is a disease that commonly affects patients in the fifth and sixth decades of life (Afshari 2006). Population demographics are changing in the developed world, with an aging population. It is possible that many cases of subclinical Fuchs will become clinically apparent as people live longer; therefore, the incidence and prevalence may rise. Whilst EK has potential advantages over PKP, both are associated with complications. In this review we aimed to determine the effectiveness and safety of EK in comparison to PKP. We did not compare different techniques of EK with each other, for example DLEK (deep lamellar endothelial keratoplasty), DMEK (Descemet's membrane endothelial keratoplasty) and Descemet's stripping automated endothelial keratoplasty (DSAEK). Although there are significant variations in surgical techniques and complication rates between DSEK, DSAEK, DLEK, DMEK and FLEK, for the purpose of this review they will be broadly classified as EK.
Objectives
The objective of this review was to compare the benefits and complications related to two surgical methods (EK and PKP) of replacing the diseased endothelial layer of the cornea with a healthy layer in people with FED.
Methods
Criteria for considering studies for this review
Types of studies
We included all randomised controlled trials (RCTs) that met the inclusion criteria for the review. We did not include studies in which all or some participants received secondary grafts.
Types of participants
Initially, we intended to include trials in which all participants had a clinical diagnosis of FED and all participants received a primary corneal graft for the treatment of FED. However, given the paucity of trials investigating people with FED only, in this version of the review we decided to include trials with a majority of participants with FED. There were no age or gender restrictions for the inclusion of participants.
Types of interventions
We included trials in which EK was compared with PKP for the surgical management of FED. All variations of EK, such as DSAEK, DMEK or DLEK, were included as the principle of the operation is the same, that is to replace the endothelial layer of the cornea.
Types of outcome measures
Primary outcomes
The primary outcome was the logarithm of the Minimum Angle of Resolution (logMAR) best corrected visual acuity (BCVA) at 24 months or more post‐treatment. When BCVA was expressed in Snellen or a decimal, this was converted to logMAR BCVA using standardised visual acuity conversion tables. We selected 24 months because visual recovery after PKP can take up to 24 months. However, to provide more information to readers, we also narratively reported logMAR BCVA at other time points as described in the included studies, but we did not meta‐analyse the data from other time points.
Secondary outcomes
We reported the degree of irregular astigmatism at 24 months post‐treatment, measured by corneal topography, and endothelial cell counts at six and 12 months after the surgery as reported in the included studies. In future updates of the review we also intend to look at the following outcomes:
logMAR BCVA at five years or more post‐treatment;
unaided logMAR visual acuity at five years or more post‐treatment;
spherical equivalent refraction in diopters (D) at 24 months post‐treatment;
amount of regular astigmatism in diopters (D) at 24 months post‐treatment;
endothelial cell count at 24 months and five years post‐treatment.
Adverse outcomes
We intended to assess complications such as primary graft failure (for PKP and EK), graft dislocation (for EK), globe rupture, endophthalmitis and incidence of corneal graft rejection. We also intended to compare between groups severe visual loss (logMAR BCVA of 1.0 or less) and loss of 10 or more letters (0.2 logMAR units) from the preoperative BCVA within 24 months of treatment.
Quality of life and economic factors
We intended to include data on quality of life and economic factors for analysis.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) 2014, Issue 1, part of The Cochrane Librarywww.thecochranelibrary.com (accessed 27 January 2014), MEDLINE (January 1950 to January 2014), EMBASE (January 1980 to January 2014), Latin American and Caribbean Health Sciences Literature Database (LILACS) (January 1982 to January 2014), the metaRegister of Controlled Trials (mRCT) (www.controlled‐trials.com) and ClinicalTrials.gov (www.clinicaltrials.gov). There were no date or language restrictions in the electronic searches for trials. The electronic databases were last searched on 27 January 2014.
See: Appendices for details of search strategies for CENTRAL (Appendix 1), MEDLINE (Appendix 2), EMBASE (Appendix 3), LILACS (Appendix 4), mRCT (Appendix 5) and ClinicalTrials.gov (Appendix 6).
Searching other resources
We searched the reference lists of the studies included in the review to identify further trials. We used the Science Citation Index to find the studies that have cited the identified trials as of February 2011. We did not handsearch journals or conference proceedings.
Data collection and analysis
Selection of studies
Two review authors worked independently to assess the titles and abstracts resulting from the searches. We then obtained full‐text reports of all possibly or definitely relevant studies for further assessment. The two review authors assessed these full‐text copies to see whether they met the inclusion criteria. We resolved discrepancies through discussion. We excluded trials which were thought to be possibly relevant on the basis of the abstract but were not eligible based on the assessment of the full‐text copy, and recorded the reasons for exclusion in the 'Characteristics of excluded studies' table.
Data extraction and management
Two review authors extracted the data independently using a form developed by the Cochrane Eyes and Vision Group. We extracted study characteristics, characteristics of participants, interventions and comparisons, and all the outcome data we had pre‐specified in our 'Methods' section. We resolved discrepancies through discussion amongst all authors. One review author entered the data into RevMan 5.2 (RevMan 2013), and a second review author checked the entered data for errors and inconsistencies. We contacted study investigators in the event of missing data or information. We documented the cases lost to follow‐up and reported available‐case analyses; we have not imputed any missing data.
Assessment of risk of bias in included studies
Two review authors assessed studies that met the inclusion criteria for methodological quality. We considered the following domains for risks of bias: random sequence generation and allocation concealment (selection bias), masking of participants (performance bias), masking of outcome assessment (detection bias), completeness of follow‐up (attrition bias), selective reporting (reporting bias), and other potential sources of bias. As the two treatments concerned are inherently different, masking of providers was not possible and has not been assessed. We graded each domain of risk of bias as: low risk of bias, high risk of bias or unclear. We resolved any disagreements between the review authors by discussion.
Measures of treatment effect
Effectiveness outcomes
Continuous data
BCVA (logMAR)
Unaided visual acuity (logMAR)
Degree of irregular astigmatism (diopters)
Refractive error (spherical equivalent in diopters and amount of regular astigmatism in diopters)
Endothelial cell count
We summarised the mean differences between treatment groups and 95% confidence intervals for continuous outcomes.
Adverse effects
Dichotomous data
Corneal graft rejection
Primary graft failure
Graft dislocation
Globe rupture
Endophthalmitis
Severe visual loss (logMAR BCVA of 1.0 or less)
Loss of 10 or more letters (logMAR) versus preoperative BCVA
In future updates of this review, we will treat these outcomes as dichotomous data and we will use the risk ratio (RR) between treatment groups and 95% confidence interval to measure the effect size.
Unit of analysis issues
The unit of analysis was the eye. Two trials included both eyes of some participants but did not specify whether the two eyes were assigned to the same or different treatment groups. For future updates of the review, if a study randomised one eye to the EK group and the other eye of the same person to the PKP group, we will include such trials on the basis that the trial design is suitable for the conditions and procedures being studied. We will refer to Chapter 16 of the Cochrane Handbook for Systematic Reviews of Interventions as a guide for any intra‐person correlation between eyes (Higgins 2011).
Dealing with missing data
In the event of missing data we contacted study investigators, documented the cases for follow‐up, and reported available‐case analyses. We did not impute any missing data. We extracted the data from each study that were pertinent to the outcomes we outlined for the review.
Assessment of heterogeneity
In order to decide whether it was appropriate to carry out a meta‐analysis on the results of the trials found, we checked for heterogeneity by examining characteristics of the studies. For future updates of the review, if the study characteristics for different studies are similar enough for outcome data to be synthesised we also plan to check the following:
a forest plot of the results of the studies;
results of the Chi² test for statistical heterogeneity;
I² statistic, which will be computed to quantify inconsistencies between study results.
Whenever substantial heterogeneity is identified (defined as I² ≥ 50%) we will not combine results but report a descriptive summary of results. When no heterogeneity is detected, we will calculate summary measures using the random‐effects model, or possibly the fixed‐effect model if we have a very small number of trials.
Assessment of reporting biases
No protocol was available for any of the studies included in this review. In future updates of this review, we will compare the outcomes in the published trial report versus the trial protocol. We will investigate the possibility of publication bias by examining the signs of asymmetry of funnel plots when there are 10 or more included studies.
Data synthesis
We will examine the study characteristics and I² statistic as described above. Whenever the I² statistic suggests substantial statistical heterogeneity, we will present results in a narrative summary. If the I² statistic is less than 50% (indicating there is no substantial heterogeneity) we will combine the study results. Where data are available for four or more RCTs, we will calculate summary measures using the random‐effects model. Whenever data are available for three or less trials then we will use a fixed‐effect model.
Subgroup analysis and investigation of heterogeneity
For future updates of the review, we will consider stratifying participants as per age < 50 years and ≥ 50 years. For the current review, as the numbers of studies and participants were limited, we did not attempt to do this.
Sensitivity analysis
In future updates of this review, we plan to conduct sensitivity analyses to examine how strongly our review results are related to the decisions and assumptions that have been made during the review process. We will initially include all trials in our analysis, then examine the effect of excluding trials assessed as high risk of bias on any parameter, unpublished trials or data, and industry funded studies by repeating the analysis without these studies.
Results
Description of studies
Results of the search
The initial electronic searches in February 2011 yielded a total of 592 titles and abstracts. After removing duplicates the Trials Search Co‐ordinator scanned 459 records and discarded 127 records as they were not relevant to the scope of the review. We screened the title and abstracts of the remaining 332 references. We rejected 292 abstracts as not eligible for inclusion in the review. We identified only one RCT that compared EK and PKP for treatment of FED (McLaren 2009).
An updated search conducted on 27 January 2014 yielded 305 additional titles and abstracts and nine records from ClinicalTrials.gov after duplicates were removed. We screened the results and found four records that were relevant to the scope of the review. One record was a conference abstract where the corresponding full length publication was already included in our original review. We obtained full‐text copies of the other three records and all of them met our inclusion criteria. Among these three reports, two of them were from the same trial (Figure 1).
1.
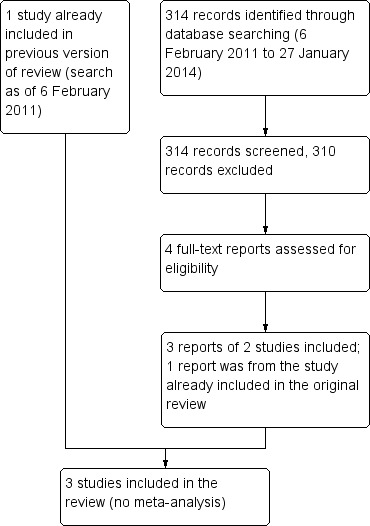
Study flow diagram.
We did not identify any reported ongoing RCTs comparing outcomes with EK and PKP.
Included studies
We included a total of three studies. Detailed characteristics of the included studies are presented in the 'Characteristics of included studies' table. A descriptive summary is listed below.
Type of participants
The three studies enrolled a total of 139 eyes of 136 participants and analysed 123 eyes (in which 94 eyes were with FED). All participants in McLaren 2009 were diagnosed with FED. In the Cheng 2009 study, 41/76 (53.9%) eyes had FED, 34/76 (44.7%) eyes had pseudophakic bullous keratopathy, and 1/76 (1.3%) eye had posterior polymorphous dystrophy. In the Patel 2008 study, 25/28 (89.2%) eyes had FED, 2/28 (7.1%) eyes had pseudophakic corneal edema, and 1/28 (0.36%) eye had unilateral endotheliopathy of uncertain cause. We contacted the authors of Cheng 2009 and Patel 2008 in an attempt to obtain outcome data for FED eyes alone but they were unable to provide these data. Given the paucity of studies in this area and considering the fact that FED accounted for the majority of the results we included these trials in this review.
Type of interventions
McLaren 2009 and Patel 2008 both randomised eyes into either the deep lamellar endothelial keratoplasty (DLEK) group or PKP group. Cheng 2009 randomised eyes into either the femtosecond laser‐assisted endothelial keratoplasty (FLEK) group or PKP group.
Type of outcomes
Primary outcome
BCVA at 24 months (shown as logMAR) was reported only by McLaren 2009.
Secondary outcomes
McLaren 2009 examined the degree of irregular astigmatism (higher‐order aberrations) at 24 months whereas Cheng 2009 reported endothelial counts at six and 12 months.
None of the studies reported logMAR UCVA or BCVA, or both, at five years or more post‐treatment, spherical equivalent refraction in diopters (D) at 24 months post‐treatment, or amount of regular astigmatism in diopters (D) at 24 months post‐treatment.
Adverse outcomes including primary graft failure, graft rejection, graft dislocation and intraocular pressure (IOP)‐related problems were reported in Cheng 2009 only.
Funding sources and declarations of interest
Cheng 2009 was funded by a grant from the Netherlands Organization for Health Research and Development (ZonMw) in the program Health Care Efficiency Research. The authors declared no conflict of interest.
McLaren 2009 was funded by the Mayo Clinic Department of Ophthalmology and Dr Patel as an Olga Keith Wiess Scholar from Research to Prevent Blindness Inc, New York and the Mayo Foundation, Rochester, Minnesota. The authors indicated that no financial conflict of interest was involved in the design and conduct of the study.
Patel 2008 was funded by Research to Prevent Blindness Inc, New York (Dr Patel as Olga Keith Wiess Scholar and an Unrestricted Grant to the Department of Ophthalmology at Mayo Clinic, Rochester, Minnesota) and Mayo Foundation, Rochester, Minnesota. The authors indicated no financial conflict of interest involved in the design and conduct of the study.
Excluded studies
Excluded studies and reasons for exclusion were recorded in the 'Characteristics of excluded studies' table.
Risk of bias in included studies
The detailed risk of bias summary for the included studies is presented in Figure 2.
2.
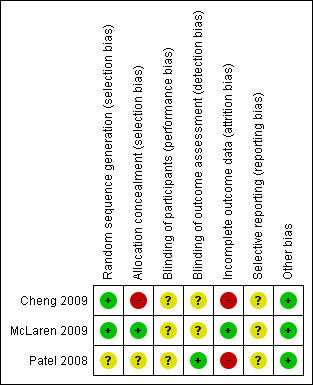
Risk of bias summary: review authors' judgements about each risk of bias domain for each included study.
Allocation
Random sequence generation
Two trials employed a method for random sequence generation and we assessed them as low risk of bias. McLaren 2009 performed randomisation using a web‐based dynamic randomisation process to stratify participants prospectively by age (<70 years versus ≥70 years) and by best corrected visual acuity (VA) (<20/80 Snellen equivalent versus ≥20/80 Snellen equivalent). Cheng 2009 generated their randomisation code by using a permuted block size of two. Patel 2008 did not specify the methods for randomisation, therefore, we assessed its risk of bias as unclear for selection bias parameters.
Allocation concealment
None of the included studies stated explicitly that they used methods for allocation concealment, however, McLaren 2009 used a web‐based randomisation system which should have provided allocation concealment. Cheng 2009 used block randomisation as described above, and we considered that allocation could not be concealed by a block size of two.
Masking (performance bias and detection bias)
As the two treatments concerned were inherently different, masking of providers was not possible and has not been assessed. Here we have assessed risk of bias for masking of participants and outcome assessors for the included studies. None of the trials reported whether masking of participants was performed. Only Patel 2008 performed masking of outcome assessors: outcomes (high‐contrast visual acuity, manifest refraction, keratometric astigmatism, contrast sensitivity, intraocular forward light scatter, and corneal backscatter) were measured by observers masked to treatment assignment. McLaren 2009 stated that videokeratography maps of the cornea were examined by masked assessors but did not report this for other outcomes; Cheng 2009 also did not report whether outcome assessors were masked, so their risk of detection bias remained unclear.
Incomplete outcome data
We assessed McLaren 2009 to be at low risk for attrition bias as there was only one out of 25 participants lost to follow‐up. Patel 2008 had three out of 16 eyes in the EK group converted to the PKP group but did not mention how the analyses accounted for the crossover of treatments; Cheng 2009 had 39/40 participants analysed for the PKP group but only 29/40 participants were analysed for the FLEK group. In the FLEK group, excluded patients included two with keratitis and two with corneal ulcers before the surgery, three with primary graft failures, two who died, one with immunologic graft failure and one with corneal fold in the endothelial graft after the surgery. In the PKP group, one was excluded due to loss to follow‐up for health‐related issues. Given the unclear reason for treatment group change for Patel 2008 and the high proportion of losses to follow‐up in one treatment group for Cheng 2009, we assessed these two studies as at high risk of attrition bias.
Selective reporting
We did not have access to the protocol for any of the three included studies, so the risk of selective reporting was unclear.
Other potential sources of bias
No other potential sources of bias were identified.
Effects of interventions
We did not perform meta‐analysis as the data could not be appropriated synthesized. Instead, we provided details regarding two sets of comparisons from three included studies.
Deep lamellar endothelial keratoplasty (DLEK) versus penetrating keratoplasty (PKP)
Primary outcome (best corrected visual acuity (BCVA))
Two studies (McLaren 2009; Patel 2008) that included 55 eyes contributed to this outcome. Only McLaren 2009 reported our pre‐specified primary outcome, BCVA at 24 months. It reported that the BCVA at 24 months was 0.34 ± 0.35 logMAR for the EK group and 0.20 ± 0.20 logMAR for the PKP group (mean difference (MD) 0.14 logMAR; 95% CI ‐0.08 to 0.36; P = 0.23). This study was limited by the small sample size, and the power of detection was not reported. Patel 2008 only had follow‐up of 12 months. At 12 months, Patel 2008 reported that the BCVA was 0.34 ± 0.16 logMAR for the DLEK group and 0.25 ± 0.21 logMAR for the PKP group (MD 0.09 logMAR; 95% CI ‐0.05 to 0.23; P = 0.22), with 80% power to detect a difference of 0.23 logMAR (2 lines) of BSCVA.
Secondary outcomes
Degree of irregular astigmatism
One study (McLaren 2009) that included 27 eyes contributed to this outcome. Higher‐order aberrations (HOAs) from the anterior corneal surface were calculated from corneal topography and decomposed into Zernike polynomials. Values from before and after surgery were compared. The total HOAs at 24 months after EK (0.48 ± 0.15 µm) were similar to before surgery (0.44 ± 0.23 µm) (P = 0.10). In PKP, however, the total HOAs increased from 0.49 ± 0.27 µm preoperatively to 1.68 ± 0.58 µm postoperatively (P < 0.005). In addition, when postoperative HOAs in the EK participants were compared with the postoperative HOAs in the PKP participants, the EK group had significantly fewer HOAs (MD ‐1.20 µm; 95% CI ‐1.53 to ‐0.87; P < 0.001). The study authors examined whether this difference in postoperative levels of HOAs at 24 months post‐surgery was visually significant but there was no correlation between HOAs and high‐contrast BCVA, low‐contrast BCVA or contrast sensitivity.
All other pre‐specified secondary outcomes, including endothelial cell counts, logMAR UCVA and BCVA at five years or more post‐treatment, spherical equivalent refraction in diopters (D) at 24 months post‐treatment, and amount of regular astigmatism in diopters (D) at 24 months post‐treatment, were not reported in these two studies.
Adverse events
Adverse events were not reported in these two studies.
Quality of life and economic factors
No study reported quality of life or economic outcomes.
Femtosecond laser‐assisted endothelial keratoplasty (FLEK) versus penetrating keratoplasty (PKP)
Primary outcome (best corrected visual acuity (BCVA))
One study (Cheng 2009) including 68 eyes contributed to this outcome; however, as the study only had 12 months follow‐up the pre‐specified 24 months data were not available. Cheng 2009 reported that conventional PKP had significantly better BCVA compared to the FLEK group, with 90% power to detect an amount of astigmastism less than 3.0 D of 30% for the PK group and 70% for the FLEK group. BCVA at 12 months was 0.55 ± 0.20 for the FLEK group and 0.35 ± 0.20 for the PKP group (MD 0.20 logMAR; 95% CI 0.10 to 0.30; P = 0.0001).
Secondary outcomes
Endothelial cell counts
Cheng 2009 had 68 eyes contributing to this outcome. It reported that endothelial cell counts were 1095 ± 423 cells/mm2 after FLEK versus 2064 ± 365 cells/mm2after PKP (MD ‐969 cells/mm2; 95% CI ‐1161 to ‐777; P < 0.001) at six months; and 1067 ± 423 cells/mm2 after FLEK versus 2028 ± 483 cells/mm2after PKP (MD ‐961 cells/mm2; 95% CI ‐1177 to ‐745; P < 0.001) at 12 months. Both FLEK and PKP surgery result in the death and loss of endothelial cells, but this data demonstrates that FLEK results in significantly more endothelial cell loss than PKP.
All other pre‐specified secondary outcomes, including degree of irregular astigmatism, logMAR UCVA and BCVA at five years or more post‐treatment, spherical equivalent refraction in diopters (D) at 24 months post‐treatment, and amount of regular astigmatism in diopters (D) at 24 months post‐treatment, were not reported in Cheng 2009.
Adverse events
Cheng 2009 randomised 80 eyes of 80 participants at the beginning of the study (40 eyes of 40 patients in each group), but only 76 eyes contributed to the adverse event data because four patients developed keratitis and corneal ulcers (two keratitis and two corneal ulcers) after randomisation and were excluded from the study before the surgery. Primary graft failure was 8% (3/36 eyes) in the FLEK group compared to none in the PKP group (RR 7.76; 95% CI 0.41 to 145.22; P = 0.10); graft rejection was 3% (1/36 eyes) in the FLEK group compared to 2% (1/40 eyes) in the PKP group (RR 1.11; 95% CI 0.07 to 17.12; P = 0.94); and graft dislocation was 28% (10/36 eyes) in the FLEK group. Other complications reported by Cheng 2009 included 3% (1/36 eyes) with epithelial ingrowth and postoperative pupillary block, and 14% (5/36 eyes) had IOP‐related problems in the FLEK group. In the PKP group they reported that 10% (4/40 eyes) had suture‐related problems, 5% (2/40 eyes) had wound dehiscence, and 10% (4/40 eyes) had suture revision to correct astigmatism. These data indicated that both procedures have associated complications but the most serious of these, primary graft failure, was more common in the FLEK group. Graft dislocation was relatively frequent (28%), possibly related to the high rate of primary graft failure. The proportion of endothelial rejection episodes was similar in both groups (2.8% in the FLEK group and 2.5% in the PKP group; RR 1.11; 95% CI 0.07 to 17.12; P = 0.94), an interesting finding given the seriousness of this complication and the fact it can lead to secondary graft failure. Other complications were less serious and less likely to result in graft failure but may have required further minor interventions. It was not possible to compare the relative impact of graft dislocation and IOP‐related problems in FLEK with wound dehiscence and suture‐related problems in PKP in a meaningful way.
Quality of life and economic factors
Cheng 2009 did not report quality of life and economic outcomes.
Discussion
Summary of main results
In our original review (Nanavaty 2011), we included an RCT that reported data for our primary outcome measure. We also performed a descriptive analysis of a study of either EK or PKP with over 50 cases. For this update we have modified our inclusion criteria to include RCTs that reported any of our primary or secondary outcomes. We also included one study that had compared femtosecond laser‐assisted endothelial keratoplasty (FLEK) versus PKP.
The aim of this review was to compare two techniques of full thickness corneal transplant (PKP) versus partial thickness corneal transplant (EK) in cases of Fuchs endothelial dystrophy (FED). We identified three RCTs of EK versus PKP for the treatment of FED (Cheng 2009; McLaren 2009; Patel 2008). Two (McLaren 2009; Patel 2008) of three studies showed no statistically significant difference in the best corrected visual acuity (BCVA) between groups post‐treatment whereas one (Cheng 2009) reported better BCVA with PKP at 12 months (Cheng 2009 and Patel 2008 had power of 90% and 80% respectively; McLaren 2009 did not report the power of detection). The degree of irregular astigmatism in one trial (McLaren 2009) was found to be significantly less following EK than PKP, and the endothelial cell counts were significantly lower with EK procedures in another trial (Cheng 2009). In terms of adverse outcomes, Cheng 2009 reported that graft dislocation, acute IOP elevation, primary graft failure and endothelial cell loss were more common in the EK group, whereas wound and suture‐related problems were more common in the PKP group. There was no important difference in the rate of endothelial rejection episodes between groups.
Overall completeness and applicability of evidence
The searches identified only three RCTs, Cheng 2009, Patel 2008, and McLaren 2009, which enrolled a total of 139 eyes of 136 participants (with 94 FED eyes). This number is disappointingly small for such a common disease and procedure. Only one study enrolled patients with FED alone (McLaren 2009). The other studies (Cheng 2009; Patel 2008) enrolled patients with FED as well as other causes of corneal endothelial failure. Despite contacting the study authors we were unsuccessful in securing data for FED eyes alone. Given the paucity of studies in this area and considering the fact that FED cases accounted for the majority of the participants, we decided to include these trials in this review. Despite this limitation of our review, we have chosen to proceed with the caveat that these results may apply to a varied case mix of etiologies and not purely to FED alone.
Another consideration is that this review includes all forms of EK. EK is a new and evolving procedure and there are many variants and technical approaches. Techniques such as deep lamellar endothelial keratoplasty (DLEK), with a large incision, are not performed routinely and they have been superseded by other techniques with smaller incisions. However, the only RCTs that met our inclusion criteria employed DLEK (McLaren 2009; Patel 2008) or femtosecond laser‐assisted endothelial keratoplasty (FLEK) (Cheng 2009). The commonest EK procedure currently performed is Descemet's stripping automated endothelial keratoplasty (DSAEK) or Descemet’s stripping endothelial keratoplasty (DSEK) rather than DLEK. None of the three RCTs in this review evaluated DSAEK or DSEK techniques and therefore extrapolation of the findings to DSAEK or DSEK should be undertaken with caution. It should be noted that along with all the above limitations of this review, the surgeon's learning curve for EK procedures also may also have influenced the results in the included studies. It is very well established that the outcomes and complication rates after EK procedures get better with increasing experience of the surgeon.
FLEK was performed in one RCT (Cheng 2009). Femtosecond corneal graft trephination and dissection is still in its primitive evolution phase. One study (Heinzelmann 2013) showed poorer outcomes in eyes in which femtosecond laser was used to cut the EK tissue compared to microkeratome‐assisted DSAEK. Cheng 2009 reported relatively higher dislocation rates and endothelial cell loss, which may be attributed to the use of the femtosecond laser in the EK groups (Vetter 2013). Vetter 2013 showed the superiority of a microkeratome‐assisted preparation of the stromal‐endothelial lamella before DSAEK surgery compared with the curved interface femtosecond laser‐assisted processing. Therefore, whether the findings of the femtosecond laser‐assisted corneal transplant procedure can be directly compared to the existing non‐femtosecond laser‐assisted techniques is debatable.
In addition, there are only three RCTs that met our inclusion criteria, and two different comparisons were employed. In terms of outcomes specification, the completeness of outcome data were not satisfactory. For the primary outcome, where we intended to evaluate BCVA at 24 months, only two out of the three studies (Cheng 2009; Patel 2008) had follow‐up at one year. In terms of disease or condition, although we intended to assess patients with FED only, two out of the three studies (Cheng 2009; Patel 2008) had a small portion of patients with other conditions; however, as most patients had FED, we still decided to include these studies to provide a broader view of this research field to readers.
Quality of the evidence
One of the limitations of this review is that none of the three identified RCTs had a large sample size. In terms of risk of bias, although the sequence generation was satisfactory for two of the three trials, two trials did not perform allocation concealment and none reported performing masking of participants. Masking of the investigators collecting the postoperative data were unclear for two out of the three trials. Two trials (Cheng 2009; Patel 2008) had relatively high risk of attrition bias. These are inherent problems with RCTs of surgical procedures.
Agreements and disagreements with other studies or reviews
Randomised controlled trials (RCTs) provide high quality data with low risk of bias, but performing an RCT comparing surgical procedures is difficult. It requires large numbers of participants to detect rare adverse events, long follow‐up periods, and is logistically challenging. Although non‐randomised comparative studies were not included in the analysis of the efficacy of the surgical techniques, these studies provide valuable information. In the previous version of this review (Nanavaty 2011) we searched for and analysed five such studies. Two studies (Bahar 2008; Heidemann 2008) reported no difference in BCVA and one study (Hjortdal 2009) reported significantly better BCVA in the EK group than the PKP group at 12 months. Only one study (Bahar 2008) reported data on unaided logMAR visual acuity, showing no significant difference between the groups at 12 months. Two studies (Bahar 2008; Hjortdal 2009) found no significant difference in the spherical equivalent between the groups at 12 months. Bahar 2008 reported significantly less regular astigmatism following EK at 12 months. Following EK and PKP, Heidemann 2008 and Hjortdal 2009 found less mean astigmatism with EK at 12 months. These findings on visual acuity and astigmatism are largely consistent with the findings from our updated review. However, the endothelial cell count data were very different between Cheng 2009 and the data from a non‐randomised comparative case series (Nanavaty 2011). Cheng 2009 found a very significant reduction in endothelial cell count (ECC) in the EK group and a normal ECC in the PKP group at 12 months. The majority of comparative case series (Bahar 2008; Heidemann 2008;Hjortdal 2009) found no significant difference in ECCs at 12 months although one study by Price MO March 2010 found a significantly lower endothelial cell density in eyes with EK at 12 months.
Nanavaty 2011 also examined a large case series (> 50 cases) of PKP or EK and evaluated safety outcomes. The key safety issues are primary graft failure, EK graft dislocation, endothelial cell loss, and endothelial rejection. EK is well known to involve a learning curve during which excessive manipulation of the graft may result in endothelial trauma and cell loss and may result in either primary EK graft failure or a shortened lifespan of an initially successful graft. As reported previously, there was no difference in primary graft failure in the non‐randomised comparative case series, but in the case series (> 50 cases) of EK alone there was up to 10% graft failure reported whereas none of the PKP case series reported this complication. However, Cheng 2009 found the rate to be 8%. The techniques for ensuring EK graft attachment using air bubbling require experience, and inexperience may lead to high graft dislocation rates. As reported by us in our previous version of this review (Nanavaty 2011), the proportion with EK graft dislocation varied markedly between studies. It is not possible to provide the exact reasons but other than being related to a learning curve the likely causes are differences in graft preparation or surgical techniques. Endothelial rejection is another major factor influencing the long‐term graft outcome. It is hypothesized that the risk of rejection may be lower following EK than following PKP due to the fact that less antigenic material is transplanted in EK. Nanavaty 2011 found some low quality confirmatory evidence. Case series with EK in general showed smaller proportions of endothelial rejection (range 0.7% to 9.6%) compared to case series with PKP (range 1.4% to 30.2%). If the differences between these procedures are as large as suggested by these data, it should be possible to power a study to detect differences in primary graft failure, endothelial cell loss and endothelial rejection rates. The current review did not find any difference in rejection rates between EK and PKP.
Based on the literature, the following are the proposed advantages of EK over PKP. The evidence, or lack of, is discussed for each.
Endothelial keratoplasty (EK) results in superior long‐term visual outcomes: two (McLaren 2009; Patel 2008) out of three studies showed no difference in the BCVA between groups post‐treatment whereas one (Cheng 2009) reported better BCVA with PKP compared to femtosecond laser‐assisted endothelial keratoplasty (FLEK). In Nanavaty 2011, non‐randomised comparative case series failed to demonstrate any difference in BCVA and uncorrected visual acuity (UCVA) in the long term.
EK is associated with less postoperative astigmatism: McLaren 2009 and Nanavaty 2011 found that in the long term (12 to 24 months) there appears to be less regular and irregular astigmatism following EK.
It is widely believed that EK results in faster visual recovery than with PKP and there are several case series that support this belief: neither in this update nor in Nanavaty 2011 did we examine this outcome.
EK results in early stability of refraction whereas PKP results in unstable refraction as long as sutures are present and even after their removal (Akova 1999; Davis 1998; Pineros 1996a; Riddle 1998): this variable was not evaluated either in this update nor our previous review. As noted by Nanavaty 2011, anecdotally and based on case series this advantage would appear to be the case but there is no high quality evidence to confirm it.
The rate of endothelial rejection is lower following EK: there is no evidence to support this from the three RCTs; however, as we reported in Nanavaty 2011, there was limited, weak supportive evidence based on one non‐randomised comparative case series and several cohort studies.
Perioperative endothelial cell injury and cell loss are greater following EK: one RCT (Cheng 2009) showed significantly lower endothelial cell counts after FLEK compared to PKP.
The amount of steroid drops required following EK is less than after PKP, therefore the incidence of secondary glaucoma may be less: this outcome has not been assessed.
The number of postoperative follow‐up visits is less with EK: this outcome has not been assessed.
The very nature of EK carries with it the risk of graft dislocation, and that of PKP the issues of suture management and suture complications. It is difficult but not impossible to measure the relative inconvenience and risk that these pose to the patient and, even more so, the demand on physicians' time and resources. In the first case, patient satisfaction and other aspects in the realm of 'quality of life' should be measured. In the latter case, careful record keeping would be sufficient.
There are no other systematic reviews comparing surgical technique for FED. The findings of this review were compared with summary data from two frequently cited reviews. The findings are presented in the table below and show strong agreement.
| Study characteristics | BCVA | Spherical equivalent refraction | Amount of regular astigmatism | Degree of irregular astigmatism | Endothelial cell (EC) count or loss | Primary graft failure | EK graft dislocation | Incidence of graft rejection | |
| AAO Technology Assessment (Lee WB 2009) | Review of DSEK literature | Mean range 20/34 to 20/66 at 9 months | Induced hyperopia of 0.7 D to 1.5 D | Induced astigmatism of 0.4 to 0.6 D | ‐ | Mean EC loss of 37% at 6 months and 42% at 12 months | Mean, 5% (range 0% to 29%) | Mean 14% (range 0% to 82%) | Mean 10% (range 0% to 45%) |
| Price MO February 2010 | Review of EK literature | Visual recovery more rapid following EK | Hyperopic shift of 0.5 to 1.5 D | Mean postoperative cylinder of 0.85 to 1.6 D in EK versus 3.2 to 4.9 D with PKP | ‐ | Mean EC loss of between 24% to 61% at 12 months | Between 0% to 29% | Mean 15% (range 0% to 82%) | Mean 12% |
| Nanavaty 2011 | Systematic review of EK versus PKP for FED | No difference in BSCVA between EK and PKP | Insufficient data to compare between EK and PKP | Significantly less postoperative regular astigmatism following EK (low quality data) | Significantly less irregular astigmatism following EK (RCT data) | Weak evidence of greater loss of EC following EK than PKP (low quality data) | Rate 0 to 10% of EK cases. No difference between EK and PKP (low quality data) | Range 3% to 63% (low quality data) | Weak evidence of reduced risk in EK (0 to 7.5%) versus PKP (5.3% to 23.3%) (low quality data) |
| Present review | Systematic review of EK versus PKP for FED | One RCT showed difference | Insufficient data to compare between EK and PKP | Insufficient data from RCTs | One RCT showed significantly less irregular astigmatism following EK | One RCT showed more endothelial cell loss with EK | Insufficient data from RCTs | Insufficient data from RCTs | Insufficient data from RCTs |
Finally, in 2012 the Australian Graft registry data published their annual report which included eight year follow‐up data on patients undergoing PKP and EK for bullous keratopathy due to pseudophakic bulbous keratopathy or FED. The rate of graft survival for PKP was 94% at one year, 88% at two years, 74% at four years, and 51% at six years. In comparison the rate of graft survival reported in the Australian Graft registry data for EK was 77% at one year and 70% at two years. More concerning though are the data on the mean and median survival of these grafts. For PKP the mean graft survival in the Australian Graft registry data was 63.51 months (SE 1.46; 95% CI 60.65 to 66.37) and the median survival was 84 months (seven years). In stark contrast, for EK the mean survival was only 27.60 months (SE 0.90; 95% CI 25.84 to 29.36) and the median survival only 38 months (3.2 years). It is not clear from the Australian Graft registry data whether these data reflect a learning effect or whether EK grafts in general have a short lifespan relative to PKP. However, it is clear that future research is required in this area.
Authors' conclusions
Implications for practice.
The rapid uptake of endothelial keratoplasty (EK) as the treatment of choice for FED is based upon the belief that visual recovery is more rapid, surgically induced astigmatism (regular and irregular) is less, and rates of transplant rejection are less with EK. This change in practice also assumes that the rates of long term transplant survival are equal for the two procedures. The practical differences between the surgical procedures mean that visual recovery is inherently more rapid following EK, but two of the three RCTs showed little or no evidence that EK gives superior visual outcomes compared to PKP. This review also found that higher‐order aberrations were fewer following EK but endothelial cell loss was greater. The RCTs that we included employed different EK techniques, which may have a bearing on these findings.
Implications for research.
More RCTs of visual and refractive outcomes are needed in the future to compare PKP with commonly performed EK procedures such as DSEK, DSAEK and DMEK in order to determine the answers to two key questions, whether there is any difference in the final visual outcome between these techniques and whether there are differences in the rates of graft survival in the long term?
Ideally these RCTs should be large, high quality studies with a low risk of bias and at least five years of follow‐up so that rates of long term graft survival can be compared. Masking of outcome measures can be challenging in surgical trials but attempts to overcome these difficulties, such as masked examiners evaluating visual acuity and endothelial cell counts, would be welcome. Future trials should compare the commonest current EK procedures. Whilst surgical techniques have evolved rapidly since the first report of EK, the pace of development has slowed with DSAEK and DMEK now the most widely performed procedures. Quality of life and vision also should be evaluated in future trials. Adverse events, including the risk of endothelial rejection, and cost‐effectiveness should be reported by these RCTs.
What's new
| Date | Event | Description |
|---|---|---|
| 3 February 2014 | New search has been performed | Issue 2, 2014: For this update we have modified our inclusion criteria to include all RCTs that fulfilled any of our primary or secondary outcomes. We also included studies comparing femtosecond laser endothelial keratoplasty (FLEK) versus penetrating keratoplasty (PKP). |
| 3 February 2014 | New citation required but conclusions have not changed | Issue 2, 2014: Two new RCTs (Cheng 2009; Patel 2008) have been included in this update. |
Acknowledgements
We would like to acknowledge the help of the Cochrane Eyes and Vision Group, in particular Ms Anupa Shah. We also thank Shahram Kashani for the preparation of the protocol of this review (Kashani 2010).
Appendices
Appendix 1. CENTRAL search strategy
#1 MeSH descriptor Fuchs' Endothelial Dystrophy #2 fuchs* near/3 endothelial near/3 dystroph* #3 fuchs* near/3 dystroph* #4 (#1 OR #2 OR #3) #5 MeSH descriptor Keratoplasty, Penetrating #6 penetrat* near/3 keratoplast* #7 PKP #8 endothelial near/3 keratoplast* #9 MeSH descriptor Descemet Membrane #10 descemet* near/6 keratoplast* #11 DSEK or DLEK or DMEK or DSAEK #12 (#5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11) #13 (#4 AND #12)
Appendix 2. MEDLINE search strategy
1. Fuchs' Endothelial Dystrophy/ 2. (fuchs$ adj3 endothelial adj3 dystroph$).tw. 3. (fuchs$ adj3 dystroph$).tw. 4. or/1‐3 5. Keratoplasty, Penetrating/ 6. (penetrat$ adj3 keratoplast$).tw. 7. PKP.tw. 8. (endothelial adj3 keratoplast$).tw. 9. Descemet Membrane/ 10. (descemet$ adj6 keratoplast$).tw. 11. (DSEK or DLEK or DMEK or DSAEK).tw. 12. or/5‐11 13. 4 and 12
Appendix 3. EMBASE search strategy
1. congenital cornea dystrophy/ 2. (fuchs$ adj3 endothelial adj3 dystroph$).tw. 3. (fuchs$ adj3 dystroph$).tw. 4. or/1‐3 5. penetrating keratoplasty/ 6. (penetrat$ adj3 keratoplast$).tw. 7. PKP.tw. 8. (endothelial adj3 keratoplast$).tw. 9. Descemet Membrane/ 10. (descemet$ adj6 keratoplast$).tw. 11. (DSEK or DLEK or DMEK or DSAEK).tw. 12. or/5‐11 13. 4 and 12
Appendix 4. LILACS search strategy
fuchs$ or endothelial dystroph$ and keratoplast$
Appendix 5. metaRegister of Controlled Trials search strategy
(fuchs or endothelial dystrophy) and keratoplasty
Appendix 6. ClinicalTrials.gov search strategy
fuch AND keratoplasty
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Cheng 2009.
| Methods | Study design: randomised multicenter clinical trial Number randomised (total and per group): total 80 eyes of 80 patients; 40 eyes of 40 patients in each group Number analysed (total and per group): total 68 eyes of 68 patients; 29 eyes in the FLEK group and 39 eyes in the PKP group Exclusions and loss to follow‐up: In the FLEK group, excluded patients include two keratitis and two corneal ulcers before the surgery, three primary graft failures, two died, one immunologic graft failure and one corneal fold in the endothelial graft after the surgery; In the PKP group, one was excluded due to lost to follow‐up for health‐related issues Study follow‐up: 12 months |
|
| Participants | Country: the Netherlands Age (mean ± SD, range): 69.0 ± 8.8 in the FLEK group (n = 36); 71.4 ± 11.3 in the PKP group (n = 40); four patients in the FLEK group were excluded due to keratitis and corneal ulcers before receiving the intervention Gender: 21/36 (58.3%) in the FLEK group and 27/40 (67.5%) in the PK group were women Inclusion criteria: Fuchs’ endothelial dystrophy, pseudophakic bullous keratopathy, or posterior polymorphous dystrophy, age ≥ 18 years, and best spectacle‐corrected visual acuity (BSCVA) < 20/50 Exclusion criteria: mental retardation, previous PK, and human leukocyte antigen typed keratoplasty |
|
| Interventions | Treatment or intervention 1: femtosecond laser‐assisted endothelial keratoplasty (FLEK) Control or intervention 2: penetrating keratoplasty (PKP) General procedures: “In the FLEK group, the donor endothelial graft was prepared with the 30‐kHz femtosecond laser (AMO‐Intralase, Irvine, CA) as previously described. In the recipient, a 5.0‐mm corneoscleral incision and two limbal paracenteses were made. The Descemet membrane was scored with a Price‐Sinskey hook (Moria, Anthony, France), and a circle of 7.5‐mm Descemet membrane and endothelium was stripped from the posterior stroma. A 15‐degree blade was used to make four transcorneal incisions in the midperipheral recipient cornea to drain fluid between the recipient cornea and endothelial graft. An 8.0‐mm donor corneal disc was trephined from the corneoscleral button, and the endothelial graft was removed from the anterior cornea. The endothelial surface of the endothelial graft was coated with a small layer of viscoelastic material (Healon, AMO, Uppsala, Sweden), gently folded into a taco‐configuration, and inserted using a Goosey forceps (Moria, Anthony, France). The corneoscleral incision was closed with four 10‐0 nylon sutures. An air bubble was injected to unfold the endothelial graft and press the endothelial graft against the recipient cornea. After 20 min, the bubble was partly removed, and two drops of tropicamide minims 0.5% (Chauvin Benelux, Brussel, Belgium) were instilled to avoid a pupillary block. However, after two cases of pupillary block had occurred, a peripheral iridectomy was routinely performed. Patients were instructed to lie in supine position during 24 hr, to maximize the pressure of the remaining air bubble against the endothelial graft. Postoperatively, all patients received topical dexamethasone 0.1% drops (Ratiopharm, Zaandam, The Netherlands) 6 times daily and chloramphenicol 0.5% drops (Ratiopharm, Zaandam, The Netherlands) three times daily in a tapering dose." "In the PK group, the recipient cornea was trephined using a 7.75‐ or 8.0‐mm Hessburg‐Barron vacuum trephine, and the donor cornea was trephined with an 8.0‐ or 8.25‐mm disposable trephine. In all cases, a combined suturing technique of a running 11‐0 nylon suture with eight interrupted 10‐0 nylon sutures was used. Selective suture removal was based on topographic astigmatism pattern. Postoperatively, all patients received topical dexamethasone 0.1% drops (Ratiopharm, Zaandam, The Netherlands) six times daily and chloramphenicol 0.5% drops (Ratiopharm, Zaandam, The Netherlands) three times daily in a tapering dose.” |
|
| Outcomes | Primary outcome(s): per cent of eyes with postoperative refractive astigmatism ≤ 3.0 diopters (D) Secondary outcome(s): topographical astigmatism (EyeMap EH‐290, Alcon), uncorrected visual acuity (UCVA), best spectacle‐corrected visual acuity (BSCVA), manifest refraction, endothelial cell density (Noncon Robo, SP 8000, Konan, Hyogo, Japan), and intraoperative and postoperative complications Measurements taken, and intervals at which outcomes assessed: "The UCVA and BSCVA were determined using the Early Treatment of Diabetic Retinopathy Study letter charts and were converted to logarithm of the minimum angle of resolution measurements. Vision levels of counting fingers, hand movements, light perception, and no light perception were substituted by logarithm of the minimum angle of resolution values of 1.7, 2.0, 2.5, and 3.0, respectively. Preoperatively, and at 3, 6, and 12 months follow‐up, all visual parameters were recorded, and the endothelial cell density was measured at 3, 6, and 12 months follow‐up." Unit of analysis (individual or eye): eye Other issues with outcome assessment (e.g., quality control for outcomes if any): None |
|
| Notes | Study dates: patients were recruited between April 2005 and April 2007 Funding source(s): a grant of the Netherlands Organization for Health Research and Development (ZonMw) in the program Health Care Efficiency Research Declaration of interest: the authors declared no conflicts of interest Publication language: English |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Consecutive cases from each clinical population were randomly assigned to treatment by FLEK or by PK. The randomization code was generated using a permuted block size of 2.” |
| Allocation concealment (selection bias) | High risk | Allocation cannot be concealed with a block size of 2 |
| Blinding of participants (performance bias) | Unclear risk | Not specified |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not specified |
| Incomplete outcome data (attrition bias) All outcomes | High risk | “In the FLEK group, four patients did not receive the allocated treatment due to significant preoperative events and were eventually excluded from the study analysis. All patients in the PK group received the allocated treatment.” The proportions lost to follow‐up were not low: 29/40 in FLEK group and 39/40 in PKP group and the study investigators did not perform intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available |
| Other bias | Low risk | No other source of bias identified |
McLaren 2009.
| Methods | Study design: Prospective, randomised clinical trial Number randomised (total and per group): Total 28 eyes of 25 patients; 13 eyes in the deep lamellar endothelial keratoplasty (DLEK) group and 15 eyes in the penetrating keratoplasty (PK) group Number analysed (total and per group): Total 27 eyes; 12 eyes in the DLEK group and 15 eyes in the PK group Exclusions and loss to follow‐up: “One eye in the DLEK group required repeat surgery for graft failure after the 6‐month visit, and subsequent data for this eye were excluded from the analysis.” Study follow‐up: All patients were examined before surgery and at 1, 3, 6, 12, and 24 months after surgery. |
|
| Participants | Country: United States Age (mean ± SD, range): Not reported Gender: Not reported Inclusion criteria: participants with corneal oedema resulting from Fuchs dystrophy Exclusion criteria: Not reported |
|
| Interventions | Treatment or intervention 1: deep lamellar endothelial keratoplasty Control or intervention 2: penetrating keratoplasty General procedures: "Penetrating keratoplasty was performed by incising the host central cornea with a vacuum trephine system (Hanna Trephine; Moria, Antony, France) with a diameter of 7.5 or 7.75 mm (mean, 7.55 mm). Donor tissue was punched from the endothelial side by using a trephine with diameter of 7.5 or 7.75 mm (mean, 7.63 mm). The donor tissue was secured to the host by using a double‐running technique consisting of a 12‐bite running 10‐0 nylon suture and a 12‐bite running 11‐0 nylon suture over a viscoelastic‐filled anterior chamber." "Deep lamellar endothelial keratoplasty was performed by using a method similar to that described by Terry and Ousley through a 9‐ to 10‐mm scleral tunnel incision. The donor lenticule was prepared over an artificial anterior chamber by using a manual technique for the first 11 eyes or by using a mechanical microkeratome (ALTK; Moria) with 300‐µm head depth for the last 2 eyes." |
|
| Outcomes | Primary outcome(s): High‐order aberrations (HOA) at months 1, 3, 12, and 24 Secondary outcome(s): best spectacle‐corrected, high‐contrast visual acuity (HCVA), mesopic and phtopic low‐contrast visual acuity (LCVA), and contrast sensitivity Measurements taken, and intervals at which outcomes assessed: “HOA was measured from the anterior corneal surface calculated from corneal topography and decomposed into Zernike polynomials to the sixth order, high‐ and low‐contrast visual acuity (VA), and contrast sensitivity.” “HCVA was measured by the electronic Early Treatment Diabetic Retinopathy Study protocol.” “LCVA was measured in a darkened room at a distance of 4 m from a backlit 10% Sloan Translucent Low Contrast Chart (Precision Vision, La Salle, Illinois, USA). Mesopic LCVA was measured first, by placing a neutral density (2 ND) filter in front of the low‐contrast chart (screen brightness, 1.1 cd/m2). Photopic LCVA was measured after removing the filter (screen brightness, 139 cd/m2).” “Contrast sensitivity was measured at 1.5, 3, 6, 12, and 18 cycles/degree by using the Functional Acuity Contrast Test (Vision Sciences Research Corporation, San Ramon, California, USA). 12 Subjects were asked to identify the orientation (right, left, or vertical) of bars of decreasing contrast until they could no longer identify the bars. This was repeated at each spatial frequency. Manual keratometry was measured by using a Bausch & Lomb Keratometer (Bausch & Lomb Inc, Rochester, New York, USA).” “All patients were examined before surgery and at 1, 3, 6, 12, and 24 months after surgery. At each visit, we measured contrast sensitivity, manual keratometry, VA, and corneal topography.” Unit of analysis (individual or eye): eye Other issues with outcome assessment (e.g., quality control for outcomes if any): None |
|
| Notes | Study dates: Not reported Funding source(s): Mayo Clinic Department of Ophthalmology and Dr Patel as an Olga Keith Wiess Scholar from Research to Prevent Blindness Inc, New York, New York; and the Mayo Foundation, Rochester, Minnesota Declaration of interest: the authors indicated no financial conflict of interest involved in design and conduct of study Publication language: English |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization was performed by using a web‐based dynamic randomisation process to stratify prospectively by age (< 70 years vs ≥ 70 years) and by best‐corrected visual acuity (VA) (< 20/80 Snellen equivalent vs ≥ 20/80 equivalent)." |
| Allocation concealment (selection bias) | Low risk | Same as above. It is likely a web‐based randomisation process includes allocation concealment |
| Blinding of participants (performance bias) | Unclear risk | Not specified |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | “All videokeratography maps of each cornea were examined by 1 masked observer (S.V.P.), and from each visit” Masking of other outcome assessors was not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Only one eye was excluded in the final analysis |
| Selective reporting (reporting bias) | Unclear risk | This information was not available in the report |
| Other bias | Low risk | No other source of bias identified |
Patel 2008.
| Methods | Study design: RCT Number randomised (total and per group): total: 31 eyes of 28 patients; DLEK group: 16 eyes of 14 patients; PKP group: 15 eyes of 14 patients Number analysed (total and per group): total: 28 eyes of 26 patients; DLEK group: 13 eyes of 12 patients; PKP group: 15 eyes of 14 patients Exclusions and loss to follow‐up: 3 eyes of DLEK group were converted to PKP intraoperatively for inadvertent perforation Study follow‐up: 12 months |
|
| Participants | Country: United States Age (mean ± SD, range): 75 ± 8 years in the DLEK group (n = 12; range, 56 to 85 years); 74 ± 8 years in the PKP group (n = 14; range, 62 to 86 years) Gender: Not reported Inclusion criteria: corneal edema attributable to endothelial dysfunction, and were either pseudophakic or had a cataract requiring extraction, entrance BSCVA was 20/40 or worse (with the fellow eye better than the study eye) Exclusion criteria: central corneal scarring, as determined by slit‐lamp biomicroscopy, the presence of a filtering bleb or uncontrolled glaucoma, or a history of herpetic keratitis |
|
| Interventions | Treatment or intervention 1: deep lamellar endothelial keratoplasty (DLEK) Control or intervention 2: penetrating keratoplasty (PKP) General procedures: “Deep lamellar endothelial keratoplasty was performed under general or local anesthesia by using a method similar to that described by Terry and Ousley. A 9 to 10 mm scleral tunnel incision was created superiorly using a guarded diamond blade set to a depth of 350 µm. In procedures combined with cataract surgery, phacoemulsification, and intraocular lens insertion was performed through a separate temporal clear corneal incision. The donor lenticule was prepared over an artificial anterior chamber by using a manual technique for the first 11 eyes, or by using a mechanical microkeratome (ALTK; Moria, Antony, France) with 300 µm head depth for the last two eyes.” “Penetrating keratoplasty was performed by using vacuum trephination of the host cornea (Hanna trephine; Moria, Antony, France) after marking the host with 12 equally spaced radial marks. In cases combined with cataract surgery, crystalline lens extraction, and intraocular lens insertion were performed via an open‐sky technique. A similar‐sized donor button was prepared by punching the tissue from the endothelial side and placing 12 equally spaced marks on the epithelial surface. The donor tissue was sutured to the host by using a double‐running technique (12 bites each of a 10‐0 and 11‐0 nylon suture) over a viscoelastic‐filled anterior chamber.” |
|
| Outcomes | Primary outcome(s): high‐contrast visual acuity Secondary outcome(s): manifest refraction, keratometric astigmatism, contrast sensitivity, intraocular forward light scatter, and corneal backscatter Measurements taken, and intervals at which outcomes assessed: “Patients were examined before surgery and at one, three, six, and 12 months after surgery.” “High‐contrast visual acuity was measured by using the e‐ETDRS testing protocol.” “Contrast sensitivity was examined by using the Functional Acuity Contrast Test (FACT: Vision Sciences Research Corporation, San Ramon, California, USA) with best‐spectacle correction in place.” “Intraocular forward light scatter was measured with a stray light meter, which used the direct compensation method to measure stray light at the retina.” “Central corneal backscatter (haze) was measured by using a custom scatterometer.” Unit of analysis (individual or eye): eye Other issues with outcome assessment (e.g., quality control for outcomes if any): None |
|
| Notes | Study dates: Not reported Funding source(s): Research to Prevent Blindness, Inc., New York, New York (Dr Patel as Olga Keith Wiess Scholar and an Unrestricted Grant to the Department of Ophthalmology at Mayo Clinic, Rochester, Minnesota) and Mayo Foundation, Rochester, Minnesota Declaration of interest: the authors indicated no financial conflict of interest involved in design and conduct of study Publication language: English |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Eyes were then randomly assigned to either DLEK or PK.” |
| Allocation concealment (selection bias) | Unclear risk | Not specified |
| Blinding of participants (performance bias) | Unclear risk | Not specified |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “At each examination, high‐contrast visual acuity, manifest refraction, keratometric astigmatism, contrast sensitivity, intraocular forward light scatter, and corneal backscatter were measured by observers masked as to which treatment was received.” Outcomes were measured by masked observers |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 3 eyes of DLEK group were converted to PKP intraoperatively for inadvertent perforation. Not sure whether the analyses accounted for the crossover of treatments |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available |
| Other bias | Low risk | No other sources of bias identified |
BCVA: best corrected visual acuity BSCVA: best spectacle‐corrected visual acuity DLEK: deep lamellar endothelial keratoplasty FED: Fuchs endothelial dystrophy FLEK: femtosecond laser‐assisted endothelial keratoplasty HCVA: high contrast visual acuity HOA: higher order aberration LCVA: low contrast visual acuity MDD: minimum detectable difference PKP: penetrating keratoplasty R: correlation coefficient RCT: randomised controlled trial UCVA: uncorrected visual acuity VA: visual acuity
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Allan 2007 | Non‐randomised comparative studies comparing EK versus PK |
| Bahar 2008 | Non‐randomised comparative studies comparing EK versus PK |
| Bohringer 2006 | Retrospective questionnaire |
| Chen 2008 | Retrospective case series |
| Das 2006 | Retrospective case series |
| Dobbins 2000 | Retrospective case series |
| Droutsas 2010 | Non‐randomised prospective clinical trial |
| Erdumus 2009 | Retrospective case series |
| Foster 2011 | Retrospective study |
| Graupner 2000 | Prospective case series |
| Ham 2009 | Prospective case series |
| Heidemann 2008 | Non‐randomised comparative studies comparing EK versus PK |
| Hjortdal 2009 | Non‐randomised comparative studies comparing EK versus PK |
| Langenbucher 2000 | Retrospective case series |
| Langenbucher 2002 | Prospective case series |
| Langenbucher 2003 | Retrospective case series |
| Lee JS 2009 | Retrospective case series |
| Nguyen 2002 | Prospective case series |
| Nguyen 2004 | Prospective case series |
| Nguyen 2009 | Retrospective case series |
| Pineros 1996b | Retrospective case series |
| Polack 1988 | Retrospective case series |
| Price FW August 1991 | Retrospective case series |
| Price FW March 1991 | Retrospective consecutive case series |
| Price MO 2011 | Retrospective, interventional case series |
| Price MO December 2009 | Prospective, multicenter, consecutive case series |
| Price MO March 2009 | Retrospective case series |
| Price MO March 2010 | Non‐randomised comparative studies comparing EK versus PK |
| Price MO May 2010 | Retrospective, interventional case series |
| Reinhard 2002 | Retrospective case series |
| Seitz 1999 | Prospective RCT of manual versus laser trephination in PKP |
| Seitz 2002 | Prospective RCT of laser versus mechanical trephination in PKP |
| Seitz 2003 | Prospective non‐randomised comparative case series of two suture techniques |
| Seitz January 2001 | Prospective RCT of manual versus laser trephination in PKP |
| Seitz November 2001 | Prospective RCT of manual versus laser trephination in PKP |
| Terry 2005 | Prospective case series |
| Terry 2006 | Retrospective review of consecutive case series |
| Terry 2009 | Prospective case series |
| Thompson 2003 | Retrospective non‐comparative case series |
Differences between protocol and review
In the protocol, we intended to include studies with FED patients only. Cheng 2009 and Patel 2008 both included some participants with other conditions. We contacted the authors of Cheng 2009 and Patel 2008 in an attempt to obtain outcome data for FED eyes alone but they were unable to provide these data. Given the paucity of studies in this area and considering the fact that FED accounted for the majority of the results we included these trials in this review.
Contributions of authors
Conceiving the review: MN, AS Designing the review: MN, AS Coordinating the review: MN Data collection for review ‐ Designing electronic search strategies: Cochrane Eyes and Vision Trials Search Co‐ordinator ‐ Designing manual search strategies: MN, XW ‐ Undertaking manual searches: MN, XW ‐ Screening search results: MN, XW, AS ‐ Organising retrieval of papers: MN, XW ‐ Screening retrieved papers against eligibility criteria: MN, XW, AS ‐ Appraising quality of papers: MN, XW, AS ‐ Extracting data from papers: MN, XW ‐ Writing to authors for additional information: XW ‐ Providing additional data about papers: XW ‐ Obtaining and screening data on unpublished studies: XW, MN Data management for the review ‐ Entering data into Revman: MN, XW, AS Analysis of data: MN, XW, AS Interpretation of data: MN, XW, AS Providing a methodological perspective: MN, XW, AS Providing a clinical perspective: MN, AS Providing a policy perspective: MN, XW, AS Providing a consumer perspective: MN, XW, AS Writting the review: MN, XW, AS Providing general advice on the review: MN, XW, AS
Guarantor of the review: MN
Sources of support
Internal sources
No sources of support supplied
External sources
-
NIHR Biomedical Research Centre for Ophthalmology, UK.
This research has received a proportion of its funding from the Department of Health's NIHR Biomedical Research Centre for Ophthalmology at Moorfields Eye Hospital and University College London (UCL) Institute of Ophthalmology. The views expressed in the publication are those of the authors and not necessarily those of the Department of Health.
-
National Eye Institute, National Institutes of Health, USA.
Xue Wang is supported by the Cochrane Eyes and Vision Group US Project through the National Eye Institute Grant 1 U01 EY020522‐01.
Declarations of interest
The authors have no conflicts of interest to report.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Cheng 2009 {published data only}
- Cheng YY, Schouten JS, Tahzib NG, Wijdh RJ, Pels E, Cleynenbreugel H, et al. Efficacy and safety of femtosecond laser‐assisted corneal endothelial keratoplasty: a randomized multicenter clinical trial. Transplantation 2009;88(11):1294‐302. [DOI] [PubMed] [Google Scholar]
- Cheng YY, Berg TJ, Schouten JS, Pels E, Wijdh RJ, Cleynenbreugel H, et al. Quality of vision after femtosecond laser‐assisted descemet stripping endothelial keratoplasty and penetrating keratoplasty: a randomized, multicenter clinical trial. American Journal of Ophthalmology 2011;152(4):556‐66. [DOI] [PubMed] [Google Scholar]
McLaren 2009 {published data only}
- Baratz KH, McLaren JW, Patel SV, Winter EJ, Nau CB, Bourne WM. Wavefront analysis of the corneal surface in deep lamellar keratoplasty versus penetrating keratoplasty. Investigative Ophthalmology and Visual Science. 2007; Vol. 48:ARVO E‐Abstract 3527.
- McLaren JW, Patel SV, Bourne WM, Baratz KH. Corneal wavefront errors 24 months after deep lamellar endothelial keratoplasty and penetrating keratoplasty. American Journal of Ophthalmology 2009;147(6):959‐65. [DOI] [PubMed] [Google Scholar]
Patel 2008 {published data only}
- Patel SV, McLaren JW, Hodge DO, Baratz KH. Scattered light and visual function in a randomized trial of deep lamellar endothelial keratoplasty and penetrating keratoplasty. American Journal of Ophthalmology 2008;145(1):97‐105. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Allan 2007 {published data only}
- Allan BD, Terry MA, Price FW Jr, Price MO, Griffin NB, Claesson M. Corneal transplant rejection rate and severity after endothelial keratoplasty. Cornea 2007;26(9):1039‐42. [DOI] [PubMed] [Google Scholar]
Bahar 2008 {published data only}
- Bahar I, Kaiserman I, McAllum P, Slomovic A, Rootman D. Comparison of posterior lamellar keratoplasty techniques to penetrating keratoplasty. Ophthalmology 2008;115(9):1525‐33. [DOI] [PubMed] [Google Scholar]
Bohringer 2006 {published data only}
- Bohringer D, Schindler A, Reinhard T. Satisfaction with penetrating keratoplasty. Results of a questionnaire census. Ophthalmologe 2006;103(8):677‐81. [DOI] [PubMed] [Google Scholar]
Chen 2008 {published data only}
- Chen ES, Terry MA, Shamie N, Hoar KL, Friend DJ. Descemet stripping automated endothelial keratoplasty: Six‐month results in a prospective study of 100 eyes. Cornea 2008;27(5):514‐20. [DOI] [PubMed] [Google Scholar]
Das 2006 {published data only}
- Das S, Langenbucher A, Jacobi C, Nguyen NX, Kruse FE, Naumann GO, et al. Long‐term refractive and visual outcome after penetrating keratoplasty only versus the triple procedure in Fuchs' dystrophy. Graefes Archive for Clinical and Experimental Ophthalmology 2006;244(9):1089‐95. [DOI] [PubMed] [Google Scholar]
Dobbins 2000 {published data only}
- Dobbins KR, Price FW Jr, Whitson WE. Trends in the indications for penetrating keratoplasty in the midwestern United States. Cornea 2000;19(6):813‐6. [DOI] [PubMed] [Google Scholar]
Droutsas 2010 {published data only}
- Droutsas K, Ham L, Dapena I, Geerling G, Oellerich S, Melles G. Visual acuity following Descemet‐membrane endothelial keratoplasty (DMEK): first 100 cases operated on for Fuchs endothelial dystrophy [Visus nach Descemet‐membran endothelkeratoplastik (DMEK): ergebnisse der ersten 100 eingriffe bei Fuchs'scher endotheldystrophie]. Klinische Monatsblatter fur Augenheilkunde 2010;227(6):467‐77. [DOI] [PubMed] [Google Scholar]
Erdumus 2009 {published data only}
- Erdurmus M, Cohen EJ, Yildiz EH, Hammersmith KM, Laibson PR, Varssano D, et al. Steroid‐induced intraocular pressure elevation or glaucoma after penetrating keratoplasty in patients with keratoconus or Fuchs dystrophy. Cornea 2009;28(7):759‐64. [DOI] [PubMed] [Google Scholar]
Foster 2011 {published data only}
- Foster JB, Vasan R, Walter KA. Three‐millimeter incision descemet stripping endothelial keratoplasty using sodium hyaluronate (healon): a survey of 105 eyes. Cornea 2011;30(2):150‐3. [DOI] [PubMed] [Google Scholar]
Graupner 2000 {published data only}
- Graupner M, Seitz B, Langenbucher A, Martus P, Blüthner K, Nguyen NX, et al. Interim results from the prospective "Erlanger Non‐high‐risk Penetrating Keratoplasty Study" in 207 patients [Zwischenergebnisse der prospektiven "Erlanger Nicht‐Hochrisiko‐Keratoplastik‐Studie" bei 207 Patienten]. Klinische Monatsblatter fur Augenheilkunde 2000;217(3):163‐70. [DOI] [PubMed] [Google Scholar]
Ham 2009 {published data only}
- Ham L, Dapena I, Luijk C, Wees J, Melles GR. Descemet membrane endothelial keratoplasty (DMEK) for Fuchs endothelial dystrophy: Review of the first 50 consecutive cases. Eye 2009;23(10):1990‐8. [DOI] [PubMed] [Google Scholar]
Heidemann 2008 {published data only}
- Heidemann DG, Dunn SP, Chow CY. Comparison of deep lamellar endothelial keratoplasty and penetrating keratoplasty in patients with Fuchs endothelial dystrophy. Cornea 2008;27(2):161‐7. [DOI] [PubMed] [Google Scholar]
Hjortdal 2009 {published data only}
- Hjortdal J, Ehlers N. Descemet's stripping automated endothelial keratoplasty and penetrating keratoplasty for Fuchs' endothelial dystrophy. Acta Opthalmologica 2009;87(3):310‐4. [DOI] [PubMed] [Google Scholar]
Langenbucher 2000 {published data only}
- Langenbucher A, Nguyen NX, Kus MM, Bluthner K, Kuchle M, Seitz B. Regression analysis of corneal endothelium after nonmechanical penetrating keratoplasty [Regressionsverhalten des hornhautendothels nach nichtmechanischer perforierender keratoplastik]. Klinische Monatsblatter fur Augenheilkunde 2000;216(6):393‐9. [DOI] [PubMed] [Google Scholar]
Langenbucher 2002 {published data only}
- Langenbucher A, Seitz B, Nguyen NX, Naumann GO. Corneal endothelial cell loss after nonmechanical penetrating keratoplasty depends on diagnosis: a regression analysis. Graefe's Archive for Clinical and Experimental Ophthalmology 2002;240(5):387‐92. [DOI] [PubMed] [Google Scholar]
Langenbucher 2003 {published data only}
- Langenbucher A, Nguyen NX, Seitz B. Predictive donor factors for chronic endothelial cell loss after nonmechanical penetrating keratoplasty in a regression model. Graefe's Archive for Clinical and Experimental Ophthalmology 2003;241(12):975‐81. [DOI] [PubMed] [Google Scholar]
Lee JS 2009 {published data only}
- Lee JS, Desai NR, Schmidt GW, Jun AS, Schein OD, Stark WJ, et al. Secondary angle closure caused by air migrating behind the pupil in descemet stripping endothelial keratoplasty. Cornea 2009;28(6):652‐6. [DOI] [PubMed] [Google Scholar]
Nguyen 2002 {published data only}
- Nguyen NX, Langenbucher A, Seitz B, Kuchle M, Naumann GO. Impact of increased intraocular pressure on long‐term corneal endothelial cell density after penetrating keratoplasty. Ophthalmologica 2002;216(1):40‐4. [DOI] [PubMed] [Google Scholar]
Nguyen 2004 {published data only}
- Nguyen NX, Seitz B, Langenbucher A, Wenkel H, Cursiefen C. Clinical aspects and treatment of immunological endothelial graft rejection following penetrating normal‐risk keratoplasty [Klinik und therapie der immunreaktionen nach perforierender normalrisiko‐keratoplastik]. Klinische Monatsblatter fur Augenheilkunde 2004;221(6):467‐72. [DOI] [PubMed] [Google Scholar]
Nguyen 2009 {published data only}
- Nguyen DQ, Mumford LL, Jones MN, Armitage WJ, Cook SD, Kaye SB, et al. The visual and refractive outcomes of combined and sequential penetrating keratoplasty, cataract extraction, and intraocular lens insertion. Eye 2009;23(6):1295‐301. [DOI] [PubMed] [Google Scholar]
Pineros 1996b {published data only}
- Pineros OE, Cohen EJ, Rapuano CJ, Laibson PR. Triple vs nonsimultaneous procedures in Fuchs' dystrophy and cataract. Archives of Ophthalmology 1996;114(5):525‐8. [DOI] [PubMed] [Google Scholar]
Polack 1988 {published data only}
- Polack FM. Glaucoma in keratoplasty. Cornea 1985;7(1):67‐70. [PubMed] [Google Scholar]
Price FW August 1991 {published data only}
- Price FW Jr, Whitson WE, Marks RG. Progression of visual acuity after penetrating keratoplasty. Ophthalmology 1991;98(8):1177‐85. [DOI] [PubMed] [Google Scholar]
Price FW March 1991 {published data only}
- Price FW Jr, Whitson WE, Marks RG. Graft survival in four common groups of patients undergoing penetrating keratoplasty. Ophthalmology 1991;98(3):322‐8. [DOI] [PubMed] [Google Scholar]
Price MO 2011 {published data only}
- Price MO, Fairchild KM, Price DA, Price FW Jr. Descemet's stripping endothelial keratoplasty five‐year graft survival and endothelial cell loss. Ophthalmology 2011;118(4):725‐9. [DOI] [PubMed] [Google Scholar]
Price MO December 2009 {published data only}
- Price MO, Giebel AW, Fairchild KM, Price FW Jr. Descemet's membrane endothelial keratoplasty: prospective multicenter study of visual and refractive outcomes and endothelial survival. Ophthalmology 2009;116(12):2361‐8. [DOI] [PubMed] [Google Scholar]
Price MO March 2009 {published data only}
- Price MO, Jordan CS, Moore G, Price FW. Graft rejection episodes after Descemet stripping with endothelial keratoplasty: part two: the statistical analysis of probability and risk factors. British Journal of Ophthalmology 2009;93(3):391‐5. [DOI] [PubMed] [Google Scholar]
Price MO March 2010 {published data only}
- Price MO, Gorovoy M, Benetz BA, Price FW, Menegay HJ, Debanne SM, et al. Descemet's stripping automated endothelial keratoplasty outcomes compared with penetrating keratoplasty from the Cornea Donor Study. Ophthalmology 2010;117(3):438‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Price MO May 2010 {published data only}
- Price MO, Bidros M, Gorovoy M, Price FW Jr, Benetz BA, Menegay HJ, et al. Effect of incision width on graft survival and endothelial cell loss after Descemet stripping automated endothelial keratoplasty. Cornea 2010;29(5):523‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Reinhard 2002 {published data only}
- Reinhard T, Bohringer D, Huschen D, Sundmacher R. Chronic endothelial cell loss of the graft after penetrating keratoplasty: influence of endothelial cell migration from graft to host [Chronischer endothelzellverlust des transplantats nach perforierender keratoplastik: einfluss der migration von endothelzellen vom transplantat zur wirtshornhaut]. Klinische Monatsblatter fur Augenheilkunde 2002;219(6):410‐6. [DOI] [PubMed] [Google Scholar]
Seitz 1999 {published data only}
- Seitz B, Langenbucher A, Kus MM, Kuchle M, Naumann GO. Nonmechanical corneal trephination with the excimer laser improves outcome after penetrating keratoplasty. Ophthalmology 1999;106(6):1156‐64. [DOI] [PubMed] [Google Scholar]
Seitz 2002 {published data only}
- Seitz B, Langenbucher A, Nguyen NX, Kuchle M, Naumann GO. Long‐term follow‐up of intraocular pressure after penetrating keratoplasty for keratoconus and Fuchs' dystrophy: comparison of mechanical and Excimer laser trephination. Cornea 2002;21(4):368‐73. [DOI] [PubMed] [Google Scholar]
Seitz 2003 {published data only}
- Seitz B, Langenbucher A, Kuchle M, Naumann GO. Impact of graft diameter on corneal power and the regularity of postkeratoplasty astigmatism before and after suture removal. Ophthalmology 2003;110(11):2162‐7. [DOI] [PubMed] [Google Scholar]
Seitz January 2001 {published data only}
- Seitz B, Langenbucher A, Nguyen NX, Kus MM, Kuchle M, Naumann GO. Graft endothelium and thickness after penetrating keratoplasty, comparing mechanical and excimer laser trephination: a prospective randomised study. Graefe's Archive for Clinical and Experimental Ophthalmology 2001;239(1):12‐7. [DOI] [PubMed] [Google Scholar]
Seitz November 2001 {published data only}
- Seitz B, Langenbucher A, Diamantis A, Cursiefen C, Küchle M, Naumann GO. Immunological graft reactions after penetrating keratoplasty ‐ A prospective randomized trial comparing corneal excimer laser and motor trephination [Immunreaktionen nach perforierender keratoplastik ‐ Eine prospektive randomisierte vergleichsstudie zwischen excimerlaser‐ und motortrepanation]. Klinische Monatsblatter fur Augenheilkunde 2001;218(11):710‐9. [DOI] [PubMed] [Google Scholar]
Terry 2005 {published data only}
- Terry MA, Ousley PJ. Deep lamellar endothelial keratoplasty: Visual acuity, astigmatism, and endothelial survival in a large prospective series. Ophthalmology 2005;112(9):1541‐8. [DOI] [PubMed] [Google Scholar]
Terry 2006 {published data only}
- Terry MA, Ousley PJ. Deep lamellar endothelial keratoplasty: Early complications and their management. Cornea 2006;25(1):37‐45. [DOI] [PubMed] [Google Scholar]
Terry 2009 {published data only}
- Terry MA, Shamie N, Chen ES, Phillips PM, Shah AK, Hoar KL, et al. Endothelial keratoplasty for Fuchs' dystrophy with cataract: complications and clinical results with the new triple procedure. Ophthalmology 2009;116(4):631‐9. [DOI] [PubMed] [Google Scholar]
Thompson 2003 {published data only}
- Thompson RW Jr, Price MO, Bowers PJ, Price FW Jr. Long‐term graft survival after penetrating keratoplasty. Ophthalmology 2003;110(7):1396‐402. [DOI] [PubMed] [Google Scholar]
Additional references
2012 Report ‐ Eye Bank Association of America
- Eye Bank Association of America. www.restoresight.org.
Afshari 2006
- Afshari NA, Pittard AB, Siddiqui A, Klintworth GK. Clinical study of Fuchs corneal endothelial dystrophy leading to penetrating keratoplasty: a 30‐year experience. Archives of Ophthalmology 2006;124(6):777‐80. [DOI] [PubMed] [Google Scholar]
Akova 1999
- Akova YA, Onat M, Koc F, Nurozler A, Duman S. Microbial keratitis following penetrating keratoplasty. Ophthalmic Surgery and Lasers 1999;30(6):449‐55. [PubMed] [Google Scholar]
Al‐Yousuf 2004
- Al‐Yousuf N, Mavrikakis I, Mavrikakis E, Daya SM. Penetrating keratoplasty: indications over a 10 year period. British Journal of Ophthalmology 2004;88(8):998‐1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Australian Graft registry data
- Australian Graft registry data. http://hdl.handle.net/2328/25859.
Ayres 2006
- Ayres BD, Rapuano CJ. Refractive power of the cornea. Comprehensive Ophthalmology Update 2006;7(5):243‐51. [PubMed] [Google Scholar]
Borboli 2002
- Borboli S, Colby K. Mechanisms of disease: Fuchs' endothelial dystrophy. Ophthalmology Clinics of North America 2002;15(1):17‐25. [DOI] [PubMed] [Google Scholar]
Claesson 2002
- Claesson M, Armitage WJ, Fagerholm P, Stenevi U. Visual outcome in corneal grafts: a preliminary analysis of the Swedish Corneal Transplant Register. British Journal of Ophthalmology 2002;86(2):174‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cross 1971
- Cross HE, Maumenee AE, Cantolino SJ. Inheritance of Fuchs' endothelial dystrophy. Archives of Ophthalmology 1971;85(3):268‐72. [DOI] [PubMed] [Google Scholar]
Dandona 1997
- Dandona L, Naduvilath TJ, Janarthanan M, Ragu K, Rao GN. Survival analysis and visual outcome in a large series of corneal transplants in India. British Journal of Ophthalmology 1997;81(9):726‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Davis 1998
- Davis EA, Azar DT, Jakobs FM, Stark WJ. Refractive and keratometric results after the triple procedure: experience with early and late suture removal. Ophthalmology 1998;105(4):624‐30. [DOI] [PubMed] [Google Scholar]
Heinzelmann 2013
- Heinzelmann S, Maier P, Böhringer D, Auw‐Hädrich C, Reinhard T. Visual outcome and histological findings following femtosecond laser‐assisted versus microkeratome‐assisted DSAEK. Graefe's Archive for Clinical and Experimental Ophthalmology 2013;251(8):1979‐85. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 16: Special topics in statistics. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. [Google Scholar]
Ing 1998
- Ing JJ, Ing HH, Nelson LR, Hodge DO, Bourne WM. Ten‐year postoperative results of penetrating keratoplasty. Ophthalmology 1998;105(10):1855‐65. [DOI] [PubMed] [Google Scholar]
Lam 2007
- Lam FC, Rahman MQ, Ramaesh K. Traumatic wound dehiscence after penetrating keratoplasty‐a cause for concern. Eye 2007;21(9):1146‐50. [DOI] [PubMed] [Google Scholar]
Lee WB 2009
- Lee WB, Jacobs DS, Musch DC, Kaufman SC, Reinhart WJ, Shtein RM. Descemet's stripping endothelial keratoplasty: safety and outcomes: a report by the American Academy of Ophthalmology. Ophthalmology 2009;116(9):1818‐30. [DOI] [PubMed] [Google Scholar]
Magovern 1979
- Magovern M, Beauchamp GR, McTigue JW, Fine BS, Baumiller RC. Inheritance of Fuchs' combined dystrophy. Ophthalmology 1979;86(10):1897‐923. [DOI] [PubMed] [Google Scholar]
Melles 1998
- Melles GR, Eggink FA, Lander F, Pels E, Rietveld FJ, Beekhuis WH, et al. A surgical technique for posterior lamellar keratoplasty. Cornea 1998;17(6):618‐26. [DOI] [PubMed] [Google Scholar]
Muraine 2003
- Muraine M, Sanchez C, Watt L, Retout A, Brasseur G. Long‐term results of penetrating keratoplasty. A 10‐year‐plus retrospective study. Graefe's Archive for Clinical and Experimental Ophthalmology 2003;241(7):571‐6. [DOI] [PubMed] [Google Scholar]
Pineros 1996a
- Pineros O, Cohen EJ, Rapuano CJ, Laibson PR. Long‐term results after penetrating keratoplasty for Fuchs' endothelial dystrophy. Archives of Ophthalmology 1996;114(1):15‐8. [DOI] [PubMed] [Google Scholar]
Price MO February 2010
- Price MO, Price FW Jr. Endothelial keratoplasty ‐ a review. Clinical and Experimental Ophthalmology 2010;38(2):128–40. [DOI] [PubMed] [Google Scholar]
RevMan 2013 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.2. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2013.
Riddle 1998
- Riddle HK Jr, Parker DA, Price FW Jr. Management of postkeratoplasty astigmatism. Current Opinion in Ophthalmology 1998;9(4):15‐28. [DOI] [PubMed] [Google Scholar]
Rosenblum 1980
- Rosenblum P, Stark WJ, Maumenee IH, Hirst LW, Maumenee AE. Hereditary Fuchs' dystrophy. American Journal of Ophthalmology 1980;90(4):455‐62. [DOI] [PubMed] [Google Scholar]
Terry 2001
- Terry MA, Ousley PJ. Deep lamellar endothelial keratoplasty in the first United States patients: early clinical results. Cornea 2001;20(3):239‐43. [DOI] [PubMed] [Google Scholar]
Terry 2003
- Terry MA. Deep lamellar endothelial keratoplasty (DLEK): pursuing the ideal goals of endothelial replacement. Eye 2003;17(8):982‐8. [DOI] [PubMed] [Google Scholar]
Tuft 1995
- Tuft SJ, Gregory W. Long‐term refraction and keratometry after penetrating keratoplasty for keratoconus. Cornea 1995;14(6):614‐7. [PubMed] [Google Scholar]
Vetter 2013
- Vetter JM, Butsch C, Faust M, Schmidtmann I, Hoffmann EM, Sekundo W, et al. Irregularity of the posterior corneal surface after curved interface femtosecond laser‐assisted versus microkeratome‐assisted descemet stripping automated endothelial keratoplasty. Cornea 2013;32(2):118‐24. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Kashani 2010
- Kashani S, Shortt AJ. Endothelial keratoplasty versus penetrating keratoplasty for Fuchs endothelial dystrophy. Cochrane Database of Systematic Reviews 2010, Issue 3. [DOI: 10.1002/14651858.CD008420] [DOI] [PubMed] [Google Scholar]
Nanavaty 2011
- Nanavaty MA, Shortt AJ. Endothelial keratoplasty versus penetrating keratoplasty for Fuchs endothelial dystrophy. Cochrane Database of Systematic Reviews 2011, Issue 7. [DOI: 10.1002/14651858.CD008420.pub2] [DOI] [PubMed] [Google Scholar]


