Abstract
Objectives
The utility of parametrial resection in women with early stage cervical cancer is controversial. In patients with favorable pathologic characteristics such as tumor size <2 cm and absence of lymphovascular space invasion, the rate of parametrial involvement is very low. More conservative surgical approaches have therefore been suggested. The objective of this report is to review the existing literature in this area and to describe an ongoing prospective study evaluating the safety and efficacy of conservative surgery in women with early stage cervical cancer.
Methods
We performed a search of PubMed for English language articles published between 1970 and 2010 using the MeSH terms “cervical cancer”, “conservative surgery”, and “cone biopsy”.
Results
Several retrospective studies have shown that <1% of patients with early stage cervical cancer with favorable pathologic characteristics have parametrial involvement. In addition, approximately 60% of patients undergoing radical trachelectomy have no residual disease in the final pathologic specimen. Recent studies have reported on the feasibility and safety of performing less radical surgery consisting of pelvic lymphadenectomy with cone biopsy, simple trachelectomy or simple hysterectomy in women with stage IA1 to IB1 cervical carcinoma. In addition, a prospective, multi-center, international trial is currently being performed to evaluate the outcomes of performing pelvic lymphadenectomy with conservative surgery (simple hysterectomy or cervical conization) in patients with favorable pathologic characteristics. Neoadjuvant chemotherapy followed by conservative surgery is also being explored as an option for patients with larger tumors and other pathologic characteristics that do not meet the criteria to perform conservative surgery alone.
Conclusions
The rate of parametrial involvement in women with early stage cervical cancer with favorable pathologic characteristics is low. Should the results of ongoing studies be favorable, conservative surgery could become the standard of care for certain women with early stage cervical cancer.
Keywords: cervical cancer, conservative surgery, parametrial involvement, cervical conization
Background
Cervical cancer is the most common cause of death from gynecologic cancer worldwide. For women with early stage disease undergoing surgical management, the standard treatment consists of a radical hysterectomy and pelvic lymph node dissection [1]. Although radical hysterectomy results in excellent local tumor control, it is also associated with significant morbidity [2-7]. Much of this morbidity is due to removal of the parametrium, which contains autonomic nerve fibers associated with bladder, bowel and sexual function.
Radical Trachelectomy
Radical trachelectomy offers a conservative approach for women with early stage disease who wish to retain fertility. Multiple studies have reported that radical trachelectomy is feasible, safe and has equivalent disease-free and overall survival rates when compared to radical hysterectomy [8-11]. However, like radical hysterectomy, radical trachelectomy involves removal of the parametrium and the associated complications. In addition, fertility cannot always be preserved in women undergoing radical trachelectomy. A recent study by Cibula et al. [12] reported that of 24 women referred for radical trachelectomy, fertility could not be preserved in 29%. This was primarily due to positive cranial margins or involved lymph nodes, and not due to parametrial involvement.
Parametrial Involvement in Early Cervical Cancer
The utility of parametrial resection in women with early stage cervical cancer is controversial. Several studies have shown that <1% of patients with early cervical cancer with favorable pathologic characteristics have parametrial involvement (Table 1) [13-19]. In addition, it has been shown that in approximately 60% of patients undergoing radical trachelectomy, the final pathologic specimen contains no residual disease [9].
Table 1.
Parametrial involvement rates in women with early cervical cancer with favorable pathologic characteristics
| Author | Year | Low-Risk Criteria | N | Parametrial Involvement in Low-Risk Group (%) |
|---|---|---|---|---|
| Kinney [13] | 1995 | Squamous histology only, tumor < 2 cm, no LVSI* | 83 | 0.0% |
| Covens [14] | 2002 | All histologies, tumor < 2 cm, DOI** < 10 mm, negative pelvic lymph nodes | 536 | 0.6% |
| Stegeman [15] | 2007 | Squamous, adenocarcinoma, adenosquamous or clear cell histology, tumor < 2 cm, DOI** < 10 mm, no LVSI*, negative pelvic lymph nodes | 103 | 0.0% |
| Wright [16] | 2008 | All histologies, tumor < 2 cm, no LVSI*, negative pelvic lymph nodes | 270 | 0.4% |
| Frumovitz [19] | 2009 | Squamous, adenocarcinoma or adenosquamous histology, tumor < 2 cm, no LVSI* | 125 | 0.0% |
LVSI: lymphvascular space involvement
DOI: depth of invasion
An early study by Kinney et al. [13] evaluated 83 patients with stage IB1 squamous cell carcinoma of the cervix with tumor size <2 cm and no lymphovascular space involvement (LVSI). None of the patients in that study were found to have parametrial involvement. A subsequent report by Covens and colleagues [14] evaluated 842 patients with stage IA1 to IB1 cervical cancer who underwent radical hysterectomy. They noted that 33 patients (4%) had parametrial involvement. Parametrial involvement was associated with larger tumor size, LVSI, greater depth of invasion and positive pelvic lymph nodes. They performed a subset analysis of 536 patients with tumor size ≤2 cm, negative lymph nodes and <10 mm of cervical stromal invasion. In this subgroup of patients, the incidence of parametrial involvement was only 0.6% (90% CI 0-1.1%). At a median of follow-up of 51 months, the 2 and 5-year recurrence free survival rates in this subgroup were 98% and 96%, respectively [14].
A follow-up study by Stegeman et al. [15] evaluated 103 premenopausal patients with stage IA1 to IB1 cervical cancer. All patients had tumors measuring <2 cm in diameter, <10 mm of stromal invasion, and negative pelvic lymph nodes. Only two of the 103 patients (1.9%) had parametrial involvement. Of note, both of these patients had LVSI present. Wright and colleagues [16] subsequently reported on 594 patients who underwent radical hysterectomy. Parametrial involvement was noted in 64 patients (10.8%) and was associated with advanced grade, deep cervical stromal invasion, LVSI, large tumor size and lymph node metastases. In a subgroup of 270 patients with negative lymph nodes, no LVSI, and tumors <2 cm, the incidence of parametrial involvement was only 0.4%. Among these 270 patients, two recurrences (0.7%) were noted after a median follow-up of 59 months. Frumovitz et al. [19] recently reported similar findings in 350 women who underwent radical hysterectomy at MD Anderson Cancer Center between 1990 and 2006. Parametrial involvement was noted in 7.7% of patients. However, in a subset of 125 patients with favorable pathologic characteristics (squamous, adenocarcinoma or adenosquamous histology; no LVSI; and tumors <2 cm), there were no cases of parametrial involvement.
Conservative Surgery
Given the low rate of parametrial involvement in cervical cancer patients with favorable pathologic characteristics undergoing radical hysterectomy or radical trachelectomy, a more conservative surgical approach has been suggested for these patients. Recent studies by Rob et al. [20, 21] reported on the feasibility and safety of performing less radical, fertility-sparing surgery in women with stage IA1 to IB1 cervical carcinoma. All patients underwent laparoscopic sentinel lymph node identification with frozen section. Of the 40 patients enrolled, 6 (15%) had positive sentinel lymph nodes on frozen section, and radical hysterectomy with pelvic lymphadenectomy was immediately performed. In the remaining patients, only a pelvic lymphadenectomy was performed. Following a 7-day interval to allow pathologic confirmation of negative lymph nodes, a large cone or simple vaginal trachelectomy was performed. With a mean follow-up of 47 months, one recurrence has been reported in a patient with a stage IB1 tumor with 8 mm of cervical stromal invasion and LVSI present. The patient was treated with chemoradiation and was reported to be without evidence of disease 62 months post-treatment. Of the 24 women who tried to conceive, 17 (71%) became pregnant and 11 delivered infants. The authors concluded that large cone or simple trachelectomy with laparoscopic pelvic lymph node dissection is safe and feasible with a high pregnancy rate in women with early stage cervical cancer [20, 21].
Smith et al. [22] recently performed a retrospective review of women with early stage cervical cancer to determine how many women treated with radical hysterectomy may have been eligible for fertility-sparing surgery consisting of cervical conization with pelvic lymph node dissection. The study included women ≤40 years of age who had not undergone previous sterilization, and who had tumors with favorable pathologic characteristics (tumor size <2 cm, no LVSI, and low-risk histologic subtypes). Of the 507 patients who underwent radical hysterectomy during the study period, 202 (39.8%) were 40 years of age or younger and had not had a previous tubal ligation. Of these 202 patients potentially interested in fertility preserving surgery, 53 (26.2%) met the above criteria and could have been eligible for conservative, fertility-sparing surgery with cervical conization and pelvic lymph node dissection. Of these 53 patients, none were found to have parametrial involvement or positive lymph nodes [22].
Less radical surgery has also been suggested for women who do not desire future fertility. Pluta et al. [23] reported on 60 women with stage IA1 to IB1 cervical cancer with favorable pathologic characteristics (tumor size <2 cm and <50% stromal invasion) who did not desire future fertility. All patients underwent laparoscopic sentinel lymph node identification with frozen section. Of the 60 patients enrolled, 5 had positive sentinel lymph nodes on frozen section and underwent radical hysterectomy with pelvic lymphadenectomy. In the remaining 55 patients, a complete pelvic lymphadenectomy and simple vaginal hysterectomy was performed. With a median follow-up of 47 months, no recurrences were reported. The authors concluded that simple hysterectomy with pelvic lymph node dissection is safe and feasible in select women with early stage cervical cancer who do not desire future fertility [23].
Neoadjuvant Chemotherapy and Conservative Surgery
The use of neoadjuvant chemotherapy followed by conservative surgery in women with early cervical cancer desiring future fertility has recently been described [21, 24, 25]. Plante and colleagues [25] reported on three patients with bulky stage IB1 disease treated with three cycles of neoadjuvant chemotherapy with cisplatin, paclitaxel and ifosfamide followed by radical vaginal trachelectomy and pelvic lymph node dissection. A complete pathologic response was noted in all three patients with no residual invasive carcinoma noted at surgery. Although follow-up was limited, there were no recurrences or pregnancies reported at the time of publication [25]. A subsequent study by Maneo et al. [24] reported on 21 patients with stage IB1 tumors (≤3 cm in size) who underwent three cycles of neoadjuvant chemotherapy with cisplatin, paclitaxel and ifosfamide followed by cervical conization and pelvic lymphadenectomy. A complete pathologic response with no residual carcinoma was noted in 5 patients (24%). With a median follow-up of 69 months, there have been no recurrences reported. Among the 9 patients who have attempted pregnancy, 6 patients have conceived with 9 live births.
A similar study by Rob and colleagues [21] reported on 9 patients with early stage cervical cancer who did not meet the favorable pathologic criteria for their previously described studies. These patients underwent three cycles of neoadjuvant chemotherapy with cisplatin and ifosfamide (squamous cell) or cisplatin and adriamycin (adenocarcinoma) followed by a cervical conization or simple vaginal trachelectomy and pelvic lymphadenectomy. To date, no recurrences have been reported, and reproductive ability has been maintained in 6 of the 9 patients [21]. These preliminary studies suggest that neoadjuvant chemotherapy followed by conservative surgery may be an option for patients with cervical cancer desiring future fertility.
Prospective Study
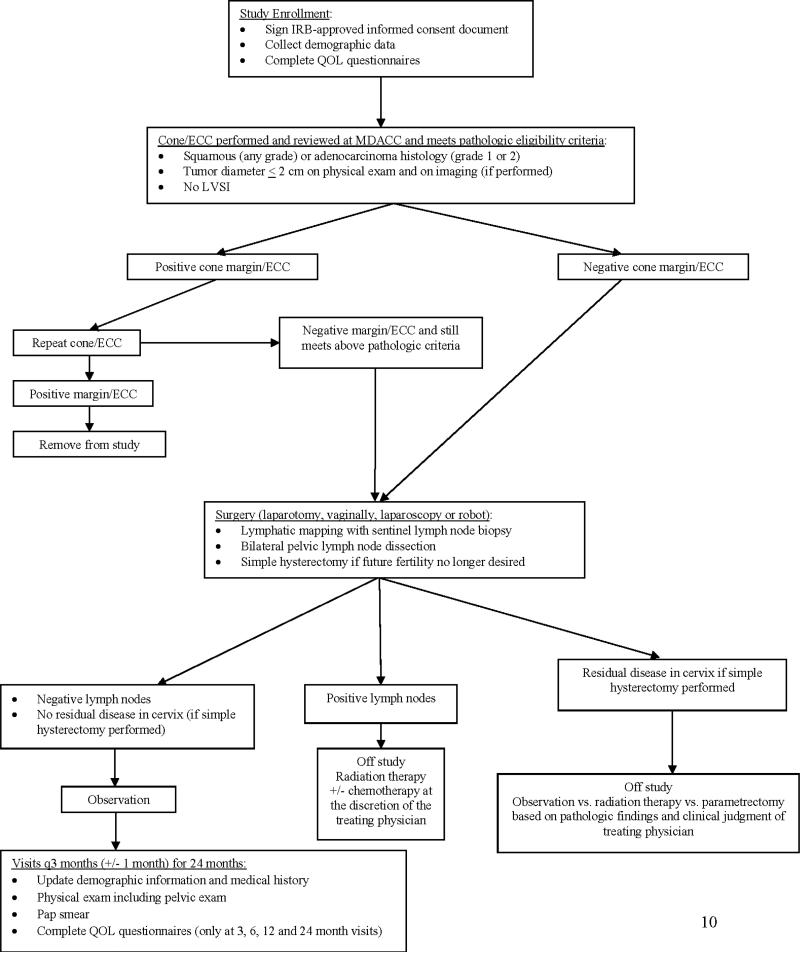
Given the low rates of parametrial involvement reported in multiple retrospective studies, M.D. Anderson Cancer Center is currently conducting a prospective, international, multi-institutional cohort study evaluating the safety and feasibility of performing conservative surgery in women with early stage cervical cancer with favorable pathologic characteristics. The inclusion criteria include stage IA2 or IB1 disease; tumor size ≤2 cm; and squamous cell carcinoma or adenocarcinoma histology. Patients with LVSI or high-risk histologic subtypes are excluded.
Patients desiring future fertility undergo cervical conization and pelvic lymph node dissection only (Figure 1). Patients not desiring future fertility undergo a simple hysterectomy and pelvic lymph node dissection. The primary objective of the study is to evaluate the safety and feasibility of performing conservative surgery in this group of patients. Secondary objectives include assessing treatment-associated morbidity and quality of life factors in patients undergoing conservative surgery compared with historical data from matched patients treated with radical hysterectomy. In addition, the sensitivity of lymphatic mapping and sentinel lymph node biopsy in the determination of pelvic lymph node metastases is being estimated.
Figure 1.
Treatment schema
The sample size for the study will be a total of 100 patients across all participating institutions. As the study treatment is significantly different from the current standard of care, two monitoring rules have been included in the protocol. The first monitoring rule states that if ≥2 patients who undergo simple hysterectomy have residual disease in the hysterectomy specimen, the treatment strategy will be considered unsafe and the study stopped. The second monitoring rule states that the study will be discontinued if ≥2 patients develop recurrent disease within the 24-month follow-up period. In addition, the MD Anderson Cancer Center Data Safety and Monitoring Committee is monitoring the overall conduct of the study.
Summary
Retrospective studies have shown that less than 1% of patients with early stage cervical cancer with favorable pathologic characteristics have parametrial involvement on radical hysterectomy specimens. In addition, approximately 60% of radical trachelectomy specimens contain no residual disease. Therefore, a prospective, international, multi-center trial is currently being performed to determine the safety and feasibility of performing pelvic lymphadenectomy with conservative surgery (simple hysterectomy or cervical conization) in patients with favorable pathologic characteristics. Should the results be favorable, this could alter the standard of care for this group of women. In addition, neoadjuvant chemotherapy followed by conservative surgery should be further explored as an option for patients with larger tumors and other pathologic characteristics that do not meet the criteria to perform conservative surgery alone.
Research Highlights.
<1% of patients with early stage cervical cancer with favorable pathologic characteristics have parametrial involvement.
Conservative surgery (lymphadenectomy with simple hysterectomy or cervical conization) may be an option for this group of patients.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement: The authors report no conflict of interest.
References
- 1.Piver MS, Rutledge F, Smith JP. Five classes of extended hysterectomy for women with cervical cancer. Obstet Gynecol. 1974;44:265–72. [PubMed] [Google Scholar]
- 2.Landoni F, Maneo A, Colombo A, Placa F, Milani R, Perego P, Favini G, Ferri L, Mangioni C. Randomised study of radical surgery versus radiotherapy for stage Ib-IIa cervical cancer. Lancet. 1997;350:535–40. doi: 10.1016/S0140-6736(97)02250-2. [DOI] [PubMed] [Google Scholar]
- 3.Low JA, Mauger GM, Carmichael JA. The effect of Wertheim hysterectomy upon bladder and urethral function. Am J Obstet Gynecol. 1981;139:826–34. doi: 10.1016/0002-9378(81)90551-2. [DOI] [PubMed] [Google Scholar]
- 4.Kadar N, Saliba N, Nelson JH. The frequency, causes and prevention of severe urinary dysfunction after radical hysterectomy. Br J Obstet Gynaecol. 1983;90:858–63. doi: 10.1111/j.1471-0528.1983.tb09328.x. [DOI] [PubMed] [Google Scholar]
- 5.Bergmark K, Avall-Lundqvist E, Dickman PW, Henningsohn L, Steineck G. Vaginal changes and sexuality in women with a history of cervical cancer. N Engl J Med. 1999;340:1383–9. doi: 10.1056/NEJM199905063401802. [DOI] [PubMed] [Google Scholar]
- 6.Sood AK, Nygaard I, Shahin MS, Sorosky JI, Lutgendorf SK, Rao SS. Anorectal dysfunction after surgical treatment for cervical cancer. J Am Coll Surg. 2002;195:513–9. doi: 10.1016/s1072-7515(02)01311-x. [DOI] [PubMed] [Google Scholar]
- 7.Frumovitz M, Sun CC, Schover LR, Munsell MF, Jhingran A, Wharton JT, Eifel P, Bevers TB, Levenback CF, Gershenson DM, Bodurka DC. Quality of life and sexual functioning in cervical cancer survivors. J Clin Oncol. 2005;23:7428–36. doi: 10.1200/JCO.2004.00.3996. [DOI] [PubMed] [Google Scholar]
- 8.Hertel H, Kohler C, Grund D, Hillemanns P, Possover M, Michels W, Schneider A. Radical vaginal trachelectomy (RVT) combined with laparoscopic pelvic lymphadenectomy: prospective multicenter study of 100 patients with early cervical cancer. Gynecol Oncol. 2006;103:506–11. doi: 10.1016/j.ygyno.2006.03.040. [DOI] [PubMed] [Google Scholar]
- 9.Plante M, Renaud MC, Francois H, Roy M. Vaginal radical trachelectomy: an oncologically safe fertility-preserving surgery. An updated series of 72 cases and review of the literature. Gynecol Oncol. 2004;94:614–23. doi: 10.1016/j.ygyno.2004.05.032. [DOI] [PubMed] [Google Scholar]
- 10.Shepherd JH, Spencer C, Herod J, Ind TE. Radical vaginal trachelectomy as a fertility-sparing procedure in women with early-stage cervical cancer-cumulative pregnancy rate in a series of 123 women. Bjog. 2006;113:719–24. doi: 10.1111/j.1471-0528.2006.00936.x. [DOI] [PubMed] [Google Scholar]
- 11.Abu-Rustum NR, Sonoda Y. Fertility-sparing radical abdominal trachelectomy for cervical carcinoma. Gynecol Oncol. 2007;104:56–9. doi: 10.1016/j.ygyno.2006.10.036. [DOI] [PubMed] [Google Scholar]
- 12.Cibula D, Slama J, Svarovsky J, Fischerova D, Freitag P, Zikan M, Pinkavova I, Pavlista D, Dundr P, Hill M. Abdominal radical trachelectomy in fertility-sparing treatment of early-stage cervical cancer. Int J Gynecol Cancer. 2009;19:1407–11. doi: 10.1111/IGC.0b013e3181b9549a. [DOI] [PubMed] [Google Scholar]
- 13.Kinney WK, Hodge DO, Egorshin EV, Ballard DJ, Podratz KC. Identification of a low-risk subset of patients with stage IB invasive squamous cancer of the cervix possibly suited to less radical surgical treatment. Gynecol Oncol. 1995;57:3–6. doi: 10.1006/gyno.1995.1091. [DOI] [PubMed] [Google Scholar]
- 14.Covens A, Rosen B, Murphy J, Laframboise S, DePetrillo AD, Lickrish G, Colgan T, Chapman W, Shaw P. How important is removal of the parametrium at surgery for carcinoma of the cervix? Gynecol Oncol. 2002;84:145–9. doi: 10.1006/gyno.2001.6493. [DOI] [PubMed] [Google Scholar]
- 15.Stegeman M, Louwen M, van der Velden J, ten Kate FJ, den Bakker MA, Burger CW, Ansink AC. The incidence of parametrial tumor involvement in select patients with early cervix cancer is too low to justify parametrectomy. Gynecol Oncol. 2007;105:475–80. doi: 10.1016/j.ygyno.2007.01.016. [DOI] [PubMed] [Google Scholar]
- 16.Wright JD, Grigsby PW, Brooks R, Powell MA, Gibb RK, Gao F, Rader JS, Mutch DG. Utility of parametrectomy for early stage cervical cancer treated with radical hysterectomy. Cancer. 2007;110:1281–6. doi: 10.1002/cncr.22899. [DOI] [PubMed] [Google Scholar]
- 17.Steed H, Capstick V, Schepansky A, Honore L, Hiltz M, Faught W. Early cervical cancer and parametrial involvement: is it significant? Gynecol Oncol. 2006;103:53–7. doi: 10.1016/j.ygyno.2006.01.027. [DOI] [PubMed] [Google Scholar]
- 18.Strnad P, Robova H, Skapa P, Pluta M, Hrehorcak M, Halaska M, Rob L. A prospective study of sentinel lymph node status and parametrial involvement in patients with small tumour volume cervical cancer. Gynecol Oncol. 2008;109:280–4. doi: 10.1016/j.ygyno.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 19.Frumovitz M, Sun CC, Schmeler KM, Deavers MT, Dos Reis R, Levenback CF, Ramirez PT. Parametrial involvement in radical hysterectomy specimens for women with early-stage cervical cancer. Obstet Gynecol. 2009;114:93–9. doi: 10.1097/AOG.0b013e3181ab474d. [DOI] [PubMed] [Google Scholar]
- 20.Rob L, Charvat M, Robova H, Pluta M, Strnad P, Hrehorcak M, Skapa P. Less radical fertility-sparing surgery than radical trachelectomy in early cervical cancer. Int J Gynecol Cancer. 2007;17:304–10. doi: 10.1111/j.1525-1438.2007.00758.x. [DOI] [PubMed] [Google Scholar]
- 21.Rob L, Pluta M, Strnad P, Hrehorcak M, Chmel R, Skapa P, Robova H. A less radical treatment option to the fertility-sparing radical trachelectomy in patients with stage I cervical cancer. Gynecol Oncol. 2008;111:S116–20. doi: 10.1016/j.ygyno.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 22.Smith AL, Frumovitz M, Schmeler KM, Reis RD, Nick AM, Coleman RL, Ramirez PT. Conservative surgery in early-stage cervical cancer: What percentage of patients may be eligible for conization and lymphadenectomy? Gynecol Oncol. 2010 doi: 10.1016/j.ygyno.2010.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pluta M, Rob L, Charvat M, Chmel R, Halaska M, Jr., Skapa P, Robova H. Less radical surgery than radical hysterectomy in early stage cervical cancer: a pilot study. Gynecol Oncol. 2009;113:181–4. doi: 10.1016/j.ygyno.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 24.Maneo A, Chiari S, Bonazzi C, Mangioni C. Neoadjuvant chemotherapy and conservative surgery for stage IB1 cervical cancer. Gynecol Oncol. 2008;111:438–43. doi: 10.1016/j.ygyno.2008.08.023. [DOI] [PubMed] [Google Scholar]
- 25.Plante M, Lau S, Brydon L, Swenerton K, LeBlanc R, Roy M. Neoadjuvant chemotherapy followed by vaginal radical trachelectomy in bulky stage IB1 cervical cancer: case report. Gynecol Oncol. 2006;101:367–70. doi: 10.1016/j.ygyno.2006.02.001. [DOI] [PubMed] [Google Scholar]