Abstract
In the companion papers this issue we presented the value of research on comorbidity, particularly in complex developmental disorders where the identification of etiology is challenging. As we will document below, Language Impairment (SLI) and Attention Deficit Hyperactivity Disorder (ADHD) have been shown to co-occur in a number of studies, and this phenomenon is commonplace in the experience of many clinicians. Given this, we must ask whether the overlap between SLI and ADHD can aid our understanding of these disorders, particularly with regard to the basis for comorbidity. As we review the literature, we will consider the models of comorbidity that were outlined in the Introduction to this issue. Finally, we present original data on SLI and ADHD from a population-based sample of children that have studied over the last two decades in the State of Iowa.
Attention Deficit Hyperactivity Disorder (ADHD) and poor spoken language ability in the form of language impairment (LI) are both common developmental disorders with important consequences in the lives of the affected children. Within clinical settings, many children present with both conditions and there has been a substantial literature that has supported this perspective. Research on the comorbidity of LI and ADHD can be divided between studies that are population based and those that are clinically ascertained. The majority of data has been derived from samples that are clinically ascertained. As we noted in the Tomblin and Mueller paper (see Mueller & Tomblin, this issue), research conducted in this way is subject to Berkson’s Bias and related problems because they can oversample comorbid cases and often have poor estimates of the rate of fully unaffected individuals, To date, there has only been one large population-based study on the comorbidity of LI and ADHD: Beitchman and colleagues (Beitchman et al., 1996; Beitchman, Hood, Rochon, & Peterson, 1989; Beitchman, Hood, Rochon, Peterson, et al., 1989; Beitchman, Nair, Clegg, Ferguson, & Patel, 1986; Beitchman et al., 2001) ascertained 142 children with speech and/or language impairments in kindergarten and matched them with controls on age, gender, and classroom/school. Teacher report at this time showed elevated rates of hyperactivity among the speech/language impaired group compared to controls (Beitchman et al., 1986). Psychiatric evaluation of a subset of the sample indicated that 30.4% of children in the speech-language impaired (SD/LI) group had ADD based on the DSM-III (1980) definition, compared to 4.5% of controls. If we treat speech –language impairment as a risk condition for ADD then we can represent the association between these conditions as a relative risk-ratio (RR) in which the rate of ADD in children positive for SD/LI is divided by the rate in children who do not present with SD/LI. We will be using RR as type of indicator for comorbidity in this paper; however, it should not be treated as a rate of comorbidity which is the rate of comorbid cases in the total population. Thus, at kindergarten, Beitchman et al. found a RR of 6.75 for ADD given SD/LI. Thus exposure to SD/LI raised the risk for ADD by more than a factor of 6 in these children. These cases and controls were then followed longitudinally to the age of 12. At age 12, no significant difference in the rates of ADHD was found between the SD/LI group and the controls (Beitchman et al., 1996). However, as noted by Lewis et al. in their accompanying article, when the speech/language-impaired group was broken apart by disorder, the RR of ADHD in the LI group was 3.7. Rates for the speech only group were not reported, but we may surmise that LI alone was related to ADHD but not in the SD in this sample. We can therefore conclude from this that the overlap beteen ADHD and at least LI exceeds the rate expected by chance. These findings are particularly useful because the LI and SD status of these children was determined after these children were sampled. Thus, these data are not based on a clinically served sample that, as pointed out in the Tomblin and Mueller (see this issue) can have an excess of comorbid cases. Due to the fact that the Beitchman et al studies were based on a population sample they could have examined their data in some additional ways. It should have been possible to derive an estimate of the actual rate of comorbidity in the population and it would also be possible to compute relative risks of LI and SD given ADHD.
The remaining studies concerned with comorbidity have mostly used a method in which the rate of LI was examined in children sampled because their ADHD status (+/−) or in small number the rate of ADHD was determined in children sampled on the basis of their LI status.
ADHD in Children with LI
As just noted, a small number of studies sampled children who were receiving clinical services for SD/LI and examined the rate of psychiatric disorders including ADHD. The largest study, by Baker and Cantwell, performed a prospective follow-up on the psychiatric status of 600 children ascertained on the basis of receiving speech and language services (Baker & Cantwell, 1987; Cantwell & Baker, 1987). They reported the rate of ADHD in children with LI to be 16% at the time of the initial study. When this sample was reviewed five years later this figure had more than doubled, rising to 37%. Language, but not speech, status in the initial study was predictive of psychiatric status at follow-up. Because there is no control group in these studies, it is not possible to compute the magnitude of association between LI and ADHD.
Benaisch et al. (1993) reported the rate of psychopathology in children who were SLI versus a typically developing control group. The most prominent psychopathology was ADHD which occurred in 18% of the SLI children and was not observed in the controls. Since the base rate in the controls was 0 we cannot determine the RR.
LI in Children with ADHD
As can be seen in Table 1, most of the studies on comorbidity of LI and ADHD employed the method wherein children were sampled for ADHD and then LI was determined. In most of these studies, no control group was employed and thus we only have rates of LI in children with ADHD which does not allow us to test whether these rates exceed chance levels (see Table 1). Even in studies that have included a control group, cases and controls are not necessarily ascertained in the same way, which again opens up the possibility of sample bias. For example, controls may in fact be patients with another diagnosis. This is often the case when studies are carried out via hospital or in-patient clinics. In the absence of a randomized control group, it is not possible to know the background prevalence rates or to computed RR at which the disorders under study occur. We can see in Table 1 that the rates of LI in children with ADHD often exceed 50% and as many as 90% of children with ADHD have co-existing language problems (Camarata, Hughes, & Ruhl, 1988; Gualtieri, Koriath, van Bourgondien, & Saleeby, 1983; Love & Tompson, 1988; Tirosh & Cohen, 1998; Trautman, Giddan, & Jurs, 1990). Many of these cases remained clinically unidentified until a (standardized) language assessment was carried out (i.e. as part of a comprehensive psychiatric evaluation or as part of a research study) (Cohen, Barwick, Horodezky, Vallance, & Im, 1998; Cohen, Davine, & Meloche-Kelly, 1989; Cohen, Davine, Horodezky, Lipsett, & Isaacson, 1993). In explaining this, Tannock and Schachar (1996) have suggested that children with unidentified language problems likely exhibit fewer difficulties with the expressive and social aspects of language, which is why a diagnosis of language impairment is overlooked. In addition, poor comprehension abilities may be misattributed by parents and teachers as inattention and and/or oppositional behavior (Howlin & Rutter, 1987).
Table 1.
Summary of clinical studies on comorbidity
| Study | Sample: size, source, comparison group | Age (years) | Findings |
|---|---|---|---|
| Alloway (2010) | 964 children from community sample, UK | 10 | 8% community sample had ADHD symptoms; ~50% of these were receiving additional classroom support for learning difficulties |
| Benaisch et al. (1993) | 56 children with LI and 43 controls followed longitudinally from age 4 to 8, USA | 4–8 | 18% of children with LI scored in the clinical range on the CBCL hyperactivity subscale versus 0% controls |
| Cantwell and Baker (1987) | 600 children from community speech and hearing clinics, USA | 2–16 | 23% of children in the S/L group had ADD; 33% of children in the language group had ADD |
| Baker and Cantwell (1987) | Subset of 300 children from Cantwell and Baker (1987) sample | Ascertained ages 2–16, followed for 5 years: 6–20 at follow-up | 16% of children with S/L had ADD at the time of the initial study; 37% of children with S/L had ADD at follow-up |
| Baker and Cantwell (1992) | Subset of 65 children from the Cantwell and Baker (1987), all comorbid for ADD | 6–15 | 62% of children with ADD had S/LI impairment; 22% had language only |
| Berry et al. (1985) | 134 ADD from clinic; 94 school based controls, USA | 6–13 | 26% of ADD had expressive language problems; 8% had receptive problems |
| Camarata, Hughes & Ruhl (1988) | 38 mild to moderately behavior-disorder children from public schools, USA | 8–12 | 37 children (97%) fell at least 1SD below the normative mean on one of more of the TOLD-I subtests |
| Chess & Rosenberg (1974) | 563 referrals from psychiatric outpatient clinic, USA | Preschool | 24% had LI, most of which ADD symptoms |
| Cohen et al. (1989, 1993, 1996, 1998, 2000) | 399 consecutive referrals to psychiatric outpatient clinic, Canada | 4–12 | Children with SLI were more likely to have ADD symptoms |
| Gualtieri et al. (1983) | 26 consecutive admissions to psychiatric inpatient care, USA | 5–13 | 90% of children with ADD had SLI |
| Love & Thompson (1988) | 200 referrals to child psychiatric outpatient clinic, Canada | Preschool | 66% of children with ADD had SLI |
| Tannock et al. (1995) | 20 ADHD referred for medication trial, Canada | 7–11 | 60% children with ADHD had S/LI. All but one previously undiagnosed |
| Tirosch & Cohen (1998) | 120 children ascertained by teacher report | 6–11 | 45% of children with ADHD were impaired in at least one language domain |
| Trautman et al. (1990) | 67 psychiatric referrals to day treatment program, USA | 6–13 | 63% of S/L had ADD; 27% of ADD had S/L impairment |
Summary
We can see that most of the evidence concerning the comorbidty of ADHD with LI comes from studies of children with ADHD. In these studies we find very high rates of LI and certainly much more than would be expected in a group of children without ADHD. We also see was seems to be elevated rates of ADHD in the small number of studies where the sampling began with children who were LI. Tannock and Schachar have described the overlap between LI and ADHD as slightly asymmetrical in that more children with ADHD have co-occurring speech and/or language impairments (average 50%) than children with S/LI have ADHD (average 20%) (Tannock & Schachar, 1996, p. 133). The data presented here would also support this conclusion. If this asymmetry is valid, it might be consistent with a model of comorbidity (Model 3) described in Tomblin and Mueller wherein ADHD increases the risk for LI which also has a separate etiological source distinct from ADHD. We can also conclude that the literature is surprisingly limited with respect to what would be viewed as well-designed studies that use a population sample and provide for a control group.
Is there a Direct Causal Link between LI and ADHD?
As just noted, the asymmetry of the rates of ADHD given LI or LI given ADHD suggest that ADHD could influence LI. This issue with respect to a direct influence of the symptoms of ADHD on LI or vice versa has been the subject of several papers. In other words, to what degree does ADHD confer risk for LI? And, to what degree does LI confer risk for ADHD? Knowing this can inform thinking about models of comorbidity. Some authors have proposed a causal relationship between LI and ADHD (Figure 1 (a)) (Rice, 1993) or, conversely, ADHD and LI (Figure 1 (b)) (Lynam, Moffitt, & Stouthamer-Loeber, 1993).
Figure 1.
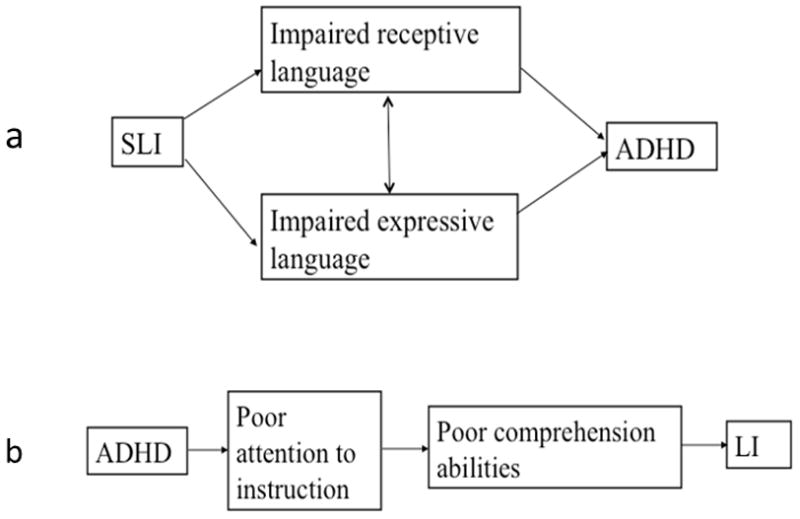
Two models of influence between ADHD and LI.
As outlined in Chapter 2, attention is the process of selectively concentrating on one aspect of information to the exclusion of other information. The early language learner must be able to selectively focus on relevant linguistic input and ignore irrelevant input. S/he must sustain this focus in order to form an association between an object and a label in the process of word learning. When the source of language input shifts, the language learner must also be able to shift his or her attention to avoid missing relevant input. As language develops, s/he must be able to attend to linguistic sequences and social routines for the development of grammatical and pragmatic skills. If the s/he is unable to do this, either because of attentional deficits (Figure 1(a)), or because of language problems (Figure 1 (b)), the process of language learning will be disrupted. Children who do not comprehend or remember language are prone to be inattentive (Figure 1 (a)). Empirical evidence suggests that children with LI may have deficits in selective (Stevens, Fanning, Coch, Sanders, & Neville, 2008) and sustained attention (Finneran, Francis, & Leonard, 2009; Spaulding, Plante, & Vance, 2008). Attentional shifting, on the other hand, is believed to be intact (Ebert & Kohnert, 2011; Schul, Stiles, Wulfeck, & Townsend, 2004).
Summary
As outlined in Tomblin and Mueller (this issue), many possible models have been proposed to explain the phenomenon of co-occurring disorders. Some of these can be rejected as explanations for the co-occurrence of ADHD and LI on the basis of existing evidence. Firstly, comorbidity is not likely due to the chance co-occurrence of two unrelated disorders: (1) the Beitchman study actually demonstrated statistically significant association. (2) the high degree of overlap between LI and ADHD seems well above the rate expected in the population at large. Thus, it is unlikely that the overlap is due to chance (Model 1). Neither is the degree of overlap so great that LI and ADHD can be assumed to be the same disorder (i.e. there is no 1:1 correlation) (Model 8). Evidence that comorbidity is common to both community (Beitchman et al., 1996; Beitchman, Hood, Rochon, & Peterson, 1989; Beitchman et al., 1986; Camarata et al., 1988) and clinical samples (Baker & Cantwell, 1987; Cantwell & Baker, 1987; Cohen et al., 1998; Cohen et al., 1989; Cohen et al., 1993; Cohen et al., 2000; Gualtieri et al., 1983; Love & Tompson, 1988) indicates this is not an artifact of referral bias (Model 2). Nor is it simply an artifact of measurement because high rates of comorbidity are found with a range of diagnostic methods, including symptom checklists, rating scales, and diagnostic interviews (Model 3). Although many symptoms of ADHD described in the DSM-IV are characteristic of pragmatic language dysfunction (e.g. talking excessively, blurting out answers before questions have been completed, interrupting others), we would not expect that eliminating these overlapping symptoms from the diagnostic criteria for ADHD would result in a significant decrease in the rate of the disorder, or in the rate of comorbidity. Executive dysfunction accounts for the core behavioral deficits in ADHD and some of pragmatic problems in LI (Model 4), but it doesn’t explain the entire range of linguistic deficits or the behavioral problems seen in the disorders.
Although we can begin to eliminate some models of comorbidty, we have also seen that the evidence base in this literature is limited by the fact that so few studies were well designed to examine comorbidty. In the current study, we will examine data obtained in a large study of children who were sampled from a population and then examined with regard to LI and ADHD status. In so doing we will ask what the prevalence of ADHD is in children with LI and likewise what the prevalence of LI is with in children with ADHD. Additionally, we will ask what the RR is for LI given ADHD and vice versa and further whether this level of risk is much different. These data will allow us to address some of the issues raised in this review with greater confidence given the design of the study.
We will also extend the inquiry into the possible models of comorbidity by examining whether there is evidence of shared liability for these disorders arising from familial sources –either cultural or genetic. In this regard, we will ask a question that is similar to that posed in the Lewis et al. study (this issue). Specifically we will as whether a history in the parents of speech, language or reading disorder increase the risk for ADHD in the children and does this history in the parents also associated with the rate of comorbidity of ADHD and LI.
COMORBIDITY OF LI AND ADHD IN A POPULATION SAMPLE: THE IOWA COHORT
The children in this study were all participants in a cross-sectional epidemiological study of SLI in children who were between 5 and 6 and just entering school. As we will describe this study involved a population sample of children. A subsample of these children were then enrolled in a 10 year longitudinal study. The data used in this study will be based on the children when they were around 10 years of age and typically attending fourth grade.
Method
Cross-sectional Study
Sample and participant selection
Participants and their families were recruited in Iowa and Illinois from a longitudinal study of children with and without language impairment (Tomblin, Records, et al., 1997; J. B. Tomblin, N. L. Records, & X. Zhang, 1996b; Tomblin, Smith, & Zhang, 1997). In the longitudinal study, children were ascertained in kindergarten and followed throughout their school years into adulthood.
Screening Phase
The original pool of participants (n=7,218) were screened in kindergarten as part of a cross-sectional epidemiological study of language impairment (Tomblin, Records, et al., 1997). The screening tool, which comprised 40 items from the Picture Vocabulary, Sentence Imitation, and Grammatic Completion subtests of the Test of Language Development-2: Primary (TOLD-2: P; Newcomer & Hammill, 1988), was developed especially for this purpose and had very high predictive accuracy for diagnostic outcome. Methods are described in detail elsewhere (Tomblin, 2010; Tomblin, Records, et al., 1997; Tomblin et al., 1996b; Tomblin, Smith, et al., 1997).
Diagnostic Phase
Following the screening phase, a stratified-cluster sampling method was used to invite schools and individuals to participate in the diagnostic phase of the epidemiological study (Tomblin, Records, et al., 1997). Children who failed the language screening test, plus a random sample who passed (approximately 33%), were administered a more comprehensive set of language and cognitive assessments as a diagnostic battery for SLI (n=2,009). These are described in detail elsewhere (Tomblin, Records, et al., 1997; Tomblin et al., 1996b). The Block Design and Picture Completion subtests of the Wechsler Preschool and Primary Scale of Intelligence–Revised (WPPSI-R; Wechsler, 1989) were used to obtain an estimate of performance IQ. SLI is based on definition by exclusion. All children who participated in the study were required to have a performance IQ greater than 85 and normal hearing. To avoid potential confounds, children who did not have English as their primary language were excluded from the study.
Language testing
Children completed five language subtests from the TOLD-2: P: Picture Vocabulary, Oral Vocabulary, Grammatic Understanding, Sentence Imitation, and Grammatic Completion, as well as the test of Word Articulation (Newcomer & Hammill, 1988). The results of these assessments were used to estimate the prevalence of language impairments in kindergarten (Tomblin, Records, et al., 1997). Scores were converted into composite language ability scores and language diagnoses for the present study.
Longitudinal Follow-up Wave 3
After participation in the cross-sectional study a sample of 604 children were enrolled as participants in a longitudinal study. This sample contained an over representation of children with LI status in kindergarten along with a random sample of children without LI.
Table 3 provides a description of the sample in kindergarten with regard to gender, language status, nonverbal IQ, and parental education.
Table 3.
Characteristics of the children with language impairment and normal language status at Wave 3 (4th grade) by gender, kindergarten language ability, performance IQ, and mother’s education.
| Group | # | % Males | Composite Language Score (z-score) | Perf. IQ | Mother’s Education (years) |
|---|---|---|---|---|---|
| Normal Language (NL) | 385 | 57.7 | 0.03 | 98.0 | 13 |
| Language Impairment (LI) | 187 | 53.81 | −1.67 | 88.1 | 12 |
Normal Language Status (NL): No more than 1 language composite score out of 5 possible below −1.25 SD for age.
Language Impairment (LI): 2 or more language composite scores below −1.25 SD for age, normal hearing, absence of other developmental disorders such as autism, cerebral palsy, or mental retardation.
As these children were followed longitudinally, we employed several parent and teacher rating scales to assess psychosocial development. In Wave 3 of the study we asked teachers to complete a questionnaire with items from the DSM-IV checklist for ADHD (see Mueller & Tomblin, this issue). This provided an overall severity rating for ADHD on a scale of 0–18, as well as information on the ADHD subtypes. Teachers also completed the Teacher’s Report Form 4/16(Achenbach, 1991b). Parents were asked to complete the companion to the TRF, the Child Behavior Checklist 4/16 (Achenbach, 1991a). Both the TRF and the CBCL have a quantitative Attention subscale. This is commensurate with the DSM-III definition of ADD and includes questions on both inattentive and hyperactive behaviors. Additionally, parents were asked whether their child had ever received a clinical diagnosis or medication treatment for ADHD (See Table 4).
Table 4.
Questions Concerning History of ADHD diagnosis and treatment.
| Has doctor ever told you that your child has ADD? |
| Has a doctor ever told you that your child has ADHD? |
We did not include data from the TRF in the present analysis because many teachers failed to complete this form and doing so would have severely limited the size of the sample. It should be noted that here the CBCL and the DSM-IV checklist are not intended in place of a clinical diagnosis; as listed in Table 6, there were questions in the study that asked specifically about this. However, they are frequently used as part of the clinical diagnostic process, and have been used extensively in research of ADHD. In this study we used them to assign a risk likelihood for ADHD, as described below.
Table 6.
Prevalence rates (proportion of total sample) of the joint occurrence of ADHD and LI.
| LI Status | ADHD Status | ||
|---|---|---|---|
| High Risk | Medium Risk | Low Risk | |
| LI | .0352 | .0522 | .0526 |
| TD | .0766 | .1839 | .5995 |
Establishment of Risk for ADHD
In accordance with DSM-IV diagnostic standards on the cross-situational nature of ADHD, our analyses only included children for whom both parent CBCL and teacher DSM-IV data were available. This resulted in a loss of 42 children from the study (n=530). A risk for ADHD was calculated on the basis of: (1) teacher endorsement of six or more symptoms of Inattention or Hyperactivity/Impulsivity on the subscales of the DSM-IV checklist, or (2) a T-score greater than 60 (<−1 SD) on the CBCL Inattention subscale. Children were then divided then into the following groups: (1) children endorsed as ADHD by both parent and teacher report (High Risk for ADHD; HR-ADHD), (2) children endorsed as ADHD by teacher report but not by parent or vice versa (moderate ris for ADHD; MR-ADHD), (3) children endorsed as ADHD by neither parent nor teacher (Low Risk for ADHD; LR-ADHD).
As noted above, the CBCL does not differentiate between ADHD subtypes. Teacher report on the DSM-IV checklist was therefore used to further subdivide children in the HR-ADHD and MR-ADHD groups into ADHD-I, ADHD-H/I, and ADHD-C subtypes.
Determination of Family History of Language Impairment
As a part of a questionnaire regarding the child’s developmental history, parents were asked to indicate whether either biological parent had a history of speech, language, or reading problems. Previously, we have shown that although a family history of speech and/or language impairment does not in itself predict whether a child is at risk for developing these disorders, a family history of reading impairment does. This is likely because speech and language problems are less well recognized than reading problems. Given that reading impairment is often grounded in language impairment, a family history in which either biological parent was speech and/or language and/or reading impaired was considered a positive family history for the purposes of this study.
Results
As already described, risk for ADHD in this sample is attributed on the basis of parent and teacher report of ADHD symptoms. Although the CBCL and DSM-IV checklist have been independently validated in the study of ADHD, further validation was made possible in this study by examining the extent to which these correlate with formal diagnoses of ADD or ADHD, This is shown in Table 5. As noted in the Methods section, this sample contained an excess of children with LI (35.85%) due to an intentional over sampling of children with the disorder as part of the longitudinal study. We therefore weighted this sample so that it was representative of the population prevalence before performing further analyses (see Tomblin, Records, et al., 1997, p. for a description).. A Chi Square test confirmed that parental and teacher report were significantly associated with a clinical diagnosis of ADHD, χ2(2, N=517.6)=68.02, p<0.0001. If a clinical diagnosis is considered to be the gold standard, our data show that the CBCL and DSM-IV rating scales are fairly sensitive as measures. Most children with a formal diagnosis of ADHD were assigned to one of the two ADHD risk groups (MR-ADHD or HR-ADHD) based on parent and teacher report (81.2%). These tests are also moderately specific: that is, most of the children without a history of ADHD were correctly assigned to the LR-ADHD group (70.8%). The majority of classification errors were in the direction of children being classed as at risk for ADHD based upon parent and teacher report, but without a formal diagnosis. Intuitively this makes sense: it is likely that not all children with ADHD are diagnosed with the disorder because not all will have access to clinical services, etc.
Table 5.
Correspondence between parent and teacher assignment of risk for ADHD and formal diagnosis
| HR-ADHD | MR-ADHD | LR-ADHD | |
|---|---|---|---|
| Positive History | 3.9 | 4.5 | 1.95 |
| Negative History | 7.3 | 18.9 | 63.46 |
Prevalence of ADHD and LI
The weighted rate of LI in this sample was 14%. Importantly, we have computed the theoretical rate of LI based on the diagnostic scheme used and it should be 14% (J. B. Tomblin, N. Records, & X. Zhang, 1996a). From this we can see that weighting this sample provides a good approximation of population prevalence. The rate of ADHD, before weighting, was 30% for MR-ADHD and 16% for HR-ADHD (45% total). After weighting this fell to 24% for MR-ADHD and 11% for HR-ADHD (35% total). The prevalence of ADHD in the general population is estimated to be in the range of 8–12%. This is very similar to the rate for HR-ADHD group, which is our most conservative estimate of risk likelihood.
Prevalence of ADHD subtypes
Using items from the DSM-IV checklist, we computed prevalence rates for each of the three ADHD subtypes. After weighting, the prevalence of ADHD-I was 13%, ADHD-H was 2%, and ADHD-C was 6.1%. There were only 10 children with ADHD-H in this sample, so the confidence interval for this prevalence estimate is quite high.. Nevertheless, this pattern is consistent with prior literature. These combine to give an overall prevalence of 21%, which is similar to the rate for MR-ADHD group. This is as expected, given that information for subtyping comes from the DSM-IV checklist, which was only completed by teachers but not parents.
Comorbidity of ADHD and LI
Using the three possible risk categories for ADHD (High, Medium, Low) and the two possible categories of language status (LI and typically developing, TD) we computed estimates of prevalence for each joint condition. These are shown in Table 6. A Chi Square test showed a significant association between language status and risk for ADHD, χ2(2, N=519.6)=31.42, p<0.0001. When HR-ADHD is tested separately from MR-ADHD and then tested with LR-ADHD both were significantly associated with LI (χ2(1, N=396.93)=26.80, p<0.0001 and χ2(1, N=461.5)=17.06, p<0.0001 respectively). As shown in Table 6, the comorbidity of LI and HR-ADHD is 3.5% compared to the rate of 5.2% for the LI and MR-ADHD.. We can estimate the rate at which we expect two disorders to co-occur, by chance, by multiplying the prevalence rates of each of the separate disorders. We have calculated these as follows: LI=0.14; MR-ADHD=0.23; HR-ADHD=0.16. We then tested whether rates of comorbidity in this sample was significantly different to that expected by chance alone, and found that both LI with HR-ADHD, z (N=532)=6.59, p<0.0001, and LI with MR-ADHD, z (N=532)=6.59, p<0.0001 exceeded chance expectations. Thus, we can conclude that risk for ADHD and LI are significantly associated in this sample.
Relative Risk for LI and ADHD
In order to test whether there is a greater level of risk for ADHD given LI or vice versa we can compute relative risks As has been noted earlier, RR reflects the degree to which the rate of an outcome increases or decrease given an exposure where a RR of 1 represents no influence.. Thus, it treats one variable as influential on the other.
RR where LI is the risk factor
First we looked at the risk for ADHD as a function of language status. Here, LI is the risk factor or exposure for ADHD. Figure 2 shows that the rates of MR-ADHD and HR-ADHD in children with LI are greater than for TD controls (49% in the MR-ADHD and 40% HR-ADHD contrasted with 23% and 8% respectively in the TD group) These rates result in RR values of 3.52 for the HR-ADHD group which was significantly greater than a value of 1 ( z=5.34, p<0.0001) which is the value if LI did not influence ADHD. Likewise the RR value was 2.77 for the MR-ADHD (z=4.07, p<0.0001) given an exposure to LI. Thus we can see that there is a greater risk for HR-ADHD given LI than for MR-ADHD, even though the rate of MR-ADHD is higher in the LI exposed group.
Figure 2.
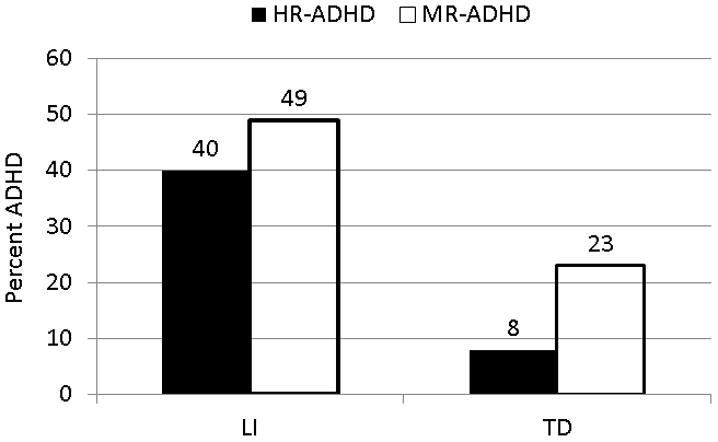
Rates of High Risk for ADHD (HR-ADHD) and Moderate Risk for ADHD (MR-ADHD) in children with language impairment (LI) and without (TD).
RR where ADHD is the risk factor
The RR of LI given exposure to ADHD was computed using the weighted rate of LI for the three risk groups. Results are shown in Figure 3. From this we can see that the risk for LI varies as a function of ADHD status: the base rate of LI is 8% in the LR-ADHD group; this rises to 22% for children with MR-ADHD; and is highest (31%) for the HR-ADHD group. The RR for LI in the HR-ADHD group was 3.9 which is significantly different from 1 ( z=5.05, p<0.0001). The risk of LI in the HR-ADHD group was 2.8 which also was significantly greater than 1 (z=4.07, p<0.0001).
Figure 3.
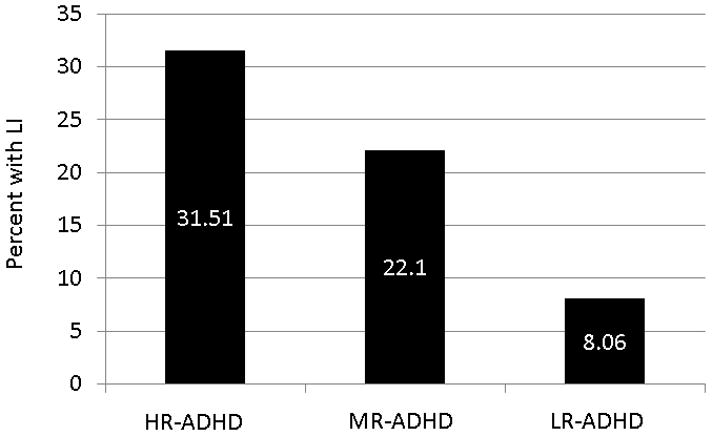
Rates of LI in children with High Risk for ADHD (HR-ADHD), Moderate Risk for ADHD (MR-ADHD) and Low Risk for ADHD (LR-ADHD).
These data further supports that there is a very likely association between LI and ADHD. Although the rate of ADHD in children with LI is higher than the rate of LI in children with ADHD, this is quite likely due largely to differences in the base rates for the two disorders. When relative risks are compared, the relative risk for ADHD given LI and the relative risk for LI given ADHD are quite similar: LI|HR-ADHD=3.9; HR-ADHD|LI=3.5; LI|MR-ADHD=2.8; MR-ADHD|LI=2.8. The symmetry of this relationship indicates we cannot assume that either disorder is nested within the other, or that one is driving the other.
Comorbidity of Subtypes of ADHD
Previous literature suggests that comorbidity of LI is highest in ADHD-I, followed by ADHD-C, and is relatively low in ADHD-H. Table 7 shows prevalence rates for the co-occurrence of LI by ADHD subtype in the current sample. There were not enough children in the ADHD-H group to examine comorbidity in this group. A Chi-Square test for the overall association of LI by ADHD subtype was, however, significant, χ2(3, N=568.9)=20.34, p<0.0001. Breaking this down by subtype, we see that, as expected, LI occurs most frequently with the ADHD-I subtype (3.6%). When we test the strength of association between LI by ADHD subtype, LI is significantly associated with ADHD-I χ2(1, N=522.8)=13.34, p<0.0001 and ADHD-C χ2(1, N=481.9)=9.8, p<0.002. It is not associated with ADHD-H χ2(1, N=458.5)=0.39, p=0.53.
Table 7.
Prevalence rates (proportion of total sample) of the joint occurrence of ADHD and LI.
| LI Status | ADHD Subtype | |
|---|---|---|
| Inattentive | Combined | |
| LI | .036 | .018 |
| TD | .096 | .043 |
Relative risks for LI and ADHD Subtypes
We also examined the relative risk for LI by ADHD subtype. Again, we were interested in asymmetry between this and the risk for ADHD conditioned on LI, which might suggest that one condition is antecedent to the other. The RR for LI conditioned on ADHD-I was 2.34 (z=3.65, p=0.0084). When this was reversed and ADHD-I was conditioned on LI, the RR was 2.36 (z=3.68, p=0.008). These rates are very similr. The RR for LI conditioned on ADHD-C was 2.60 (z=3.19, p=0.0001), while the RR for ADHD-C conditioned on LI was 2.91 (z=3.06, p=0026). The RR for ADHD-H and LI were not significant due to the low small number of children in the ADHD-H group. Again, we conclude that RR for ADHD given LI is quite simlar to the RR for LI given ADHD.
Family History of Speech, Language, or Reading Problems and ADHD Comorbidity
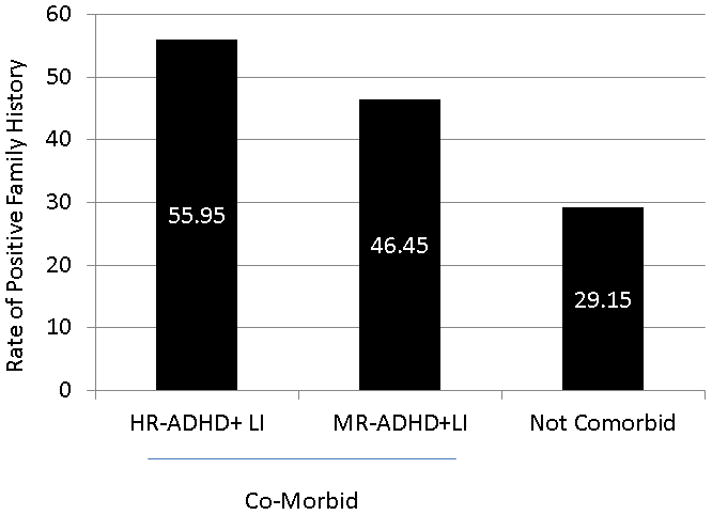
Under the hypothesis that children in families where there is a higher load of familial risk for speech, language and reading problems may be at greater risk for ADHD. We examined the data to determine whether the rate of ADHD was associated with parental report of positive family history. Figure 4 shows the rate of positive family history of speech, language and reading problems in children with high, medium and low levels of risk for ADHD. There is a clear trend for declining rates of positive history with declines in the level of ADHD risk and this association was significant Mantel Hansel χ2(, N=488)= 10.48, p=0.0.0012.
Figure 4.
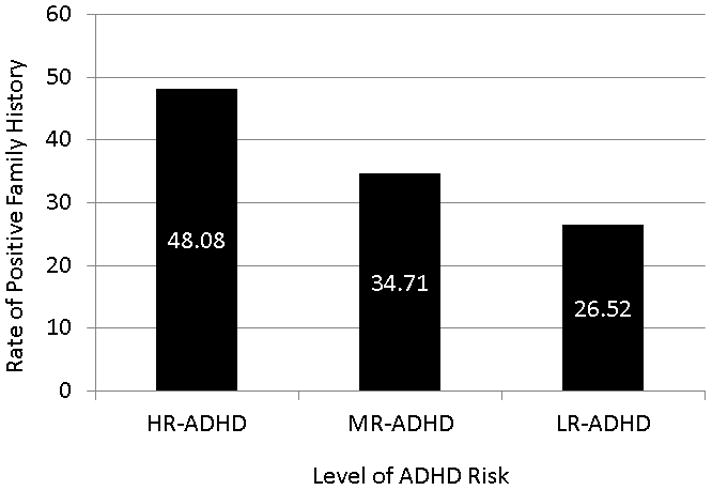
Rates of positive family history of speech, language and/or reading disorder in children with HR-ADHD, MR-ADHD and LR-ADHD.
Then we computed RR values for ADHD given an exposure to a positive family history.. The RR for HR-ADHD (given a positive family history of speech, language, or reading problems) was 1.81, which was significant z=2.5, p=0.01. By comparison, the RR for the MR-ADHD was 1.30, which was not significant z=1.64, p=0.10. It therefore appears that a family history of speech, language, or reading impairments only increases the risk for ADHD in the HR-ADHD. We might expect this. If ADHD and LI share a common etiology, and this is familial, we would expect to see that children who are comorbid for these disorders would also show elevated rates of positive family history. To varify this we compared rates of positive family history in children comorbid for ADHD and LI ( HR-ADHD and LI or MR-ADHD and LI) to children without ADHD (LR-ADHD), irrespective of language ability. These data are shown in Figure 5. Again, we see the rate of a positive family history of speech, language, or reading impairment increases as a function of the comorbidity of LI and ADHD. This overall relationship was significant, Mantel Hansel χ2(1, N=522)= 6.55, p=0.009. The relative risk for HR-ADHD given a positive family history was 1.97, which is was significant χ2(1, N=522)= 5.05, p=0.02. It is not, however, significant in the MR-ADHD group.
Figure 5.
Rates of positive family history of speech, language and/or reading disorder in children who are comorbid with LI and either HR-ADHD or MR-ADHD as well as the rate of positive family history in children who were only affected with LI, ADHD or neither.
Overall, we can conclude that family history is a risk factor for ADHD, as well as for the comorbidity of ADHD and LI.
Discussion
A review of the literature shows that ADHD and LI often overlap and are therefore considered comorbid. Much of this research has been carried out in clinical populations ascertained on the basis on one or other of the disorders, which have then estimated the rate at which the co-occuring disorder occurs. Studies designed in this way are influenced by Berkson’s bias, which artifically increases the observed rate of comorbidy, and so the high rates they report should be taken with some reservation. This is only the second study to examine the comorbidity between LI and ADHD in a sample that is population based. Children in this study were drawn from a larger cross-sectional study on the prevalence of language impairment in kindergarten. Although subsequent sampling of this cohort, which formed the basis of a longitudinal study on outcomes in children with and without language impairment, was biased toward children with LI, a large random sample of typically developing children was also maintained. To the extent this sampling bias was known, observations were weighted to counter this. We can, therefore, say that the the pattern of comorbidity we see between LI and ADHD in this study is an unnbiased estimate that represents the general population from which these children were drawn.
Consistent with prior literature, we found that ADHD and LI were significantly associated, regardless of whether this was conservatively estimated based on positive evidence from both parent and teacher (e.g. HR-ADHD), or less conservatively estimated (MR-ADHD). Our estimates of comorbidity were between 3 and 5%, depending on which ADHD risk group we considerm, which is rather high for a chronic health condition.
On the surface of things, it appeared that children with LI were at greater risk for ADHD than children with ADHD were for LI. This pattern can be seen in previous studies, and from this we might conclude that ADHD plays a causal role in the development of LI. This type of relationship was characterised in our accompanying paper (Tomblin & Mueller, this issue) as a “by-product” model of comorbidity. As we noted earlier, however, this pattern may simply be due to the fact that the base rate for ADHD is higher than that of LI. When the level of comorbidity was computed using RR, which control for differences in base rates, we did not see this asymetry. The risk for LI given ADHD, or the risk for ADHD given LI are very similar when compared in terms of relative values, which were all in the 2 to 3 range. These results do not, therefore, provide evidence for a “by-product” model of comobidity.
The “Alternate Forms”, “Correlated Liabilities” and “Causal model” accounts of comorbidity (see Tomblin & Mueller, this issue) rely on the notion of shared, or correlated, etiologies as the basis for comorbidity. These are compatiable with the symmetrical pattern of overlap between LI and ADHD observed in this sample, and so must be retained as possible explanations. The model of “Reciprocal Causation” must also be retained. We cannot distinguish further between these models, given the data in this study. In fact, we must be cautious in attempting to discern causality from these patterns of comorbidity, which are fundamentally correlational.
Relative risks can be used reflect the degree of association between two disorders, rather like an effect size. Using these, we can see that a child with LI is two to three times more likely to have ADHD than a child that is not LI. The same is true if LI is conditioned on ADHD. Additionally, we examined the comorbidity between LI and ADHD with regard to the principal subtypes. Within our sample most children were either ADHD-I or ADHD-C and very few were ADHD-H. This pattern is similar to what is generally seen in the literature. The number of children with ADHD-H was quite low and thus we are not able to draw conclusions regarding the pattern of comorbidity with this group; however, LI and the other two forms of ADHD were clearly comorbid with LI as has been show in previous literature.
Both LI and ADHD can be viewed as continuous traits. Thus, we might predict that children with LI who were in the LR-ADHD group would still exhibit more symptoms of ADHD than children without LI, even though they were classified in the unaffected ADHD group. The same might be said for the language skills of children in the MR-ADHD and HR-ADHD groups. We would expect to see more language problems among these groups, even among children not classified as LI. Given this, it might be that we have, in fact, underestimated the strength of the association between LI and ADHD, and this be more appropriately considered using quantiative phenotypes.
Family History of Speech, Language or Reading Disorder and ADHD
Although we cannot completely rule out the “by-product” model of comorbidity (ADHD is a by-product of LI, LI is a by-product of ADHD), our data suggest that ADHD and LI share a common etiology. As noted in an accompanying paper (Mueller & Tomblin, this issue), both disorders been shown to be familial and heritable, suggesting the possiblility of a genetic basis. At present, however, we are unable to say how much of phenotypic overlap between these disorders is due to shared genetic factors. The strongest method for testing this is a twin design, from which measures of genetic correlation can be calculated. Since this study comprised only unrelated probands, we we were limited in investigating famiality by asking, “to what extent does positive family history of speech, language, or reading problems confer risk for ADHD?”. We found that family history was positivley associated with both ADHD and comorbid ADHD and LI. Because the relationship between LI and ADHD appears to hold cross generations, this points to cross generational transmission of these disorder. This could be the result of shared environment, shared genes, or both.
Table 2.
Cohort characteristics and sample size across the waves of the study.
| Wave 1 | Wave 2 | Wave 3 | Wave 4 | Wave 5 | |
|---|---|---|---|---|---|
| Nominal Grade | Kindergarten | 2nd | 4th | 8th | 10th |
| Mean age | 5.9 | 8.0 | 9.9 | 13.9 | 15.9 |
| Range (yrs) | 5.3–6.7 | 7.1–9.0 | 9.1–10.9 | 13.1–15.4 | 14.9–16.4 |
| Total n | 604 | 604 | 570 | 527 | 504 |
Acknowledgments
This research was supported by grants DC00496 and DC02746 the National Institutes of Health, National Institute on Deafness and Other Communication Disorders, Grant
References
- Achenbach T, Edelbrock C. Manual for the Child Behavior Checklist. Burlington, VT: University of Vermont Press; 1983. [Google Scholar]
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991a. [Google Scholar]
- Achenbach TM. Manual for the Teacher’s Report Form and 1991 Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991b. [Google Scholar]
- Baker L, Cantwell DP. A prospective psychiatric follow-up of children with speech/language disorders. J Am Acad Child Adolesc Psychiatry. 1987;26(4):546–553. doi: 10.1097/00004583-198707000-00015. [DOI] [PubMed] [Google Scholar]
- Beitchman JH, Brownlie EB, Inglis A, Wild J, Ferguson B, Schachter D. Seven-year follow-up of speech/language impaired and control children: psychiatric outcome. J Child Psychol Psychiatry. 1996;37:961–970. doi: 10.1111/j.1469-7610.1996.tb01493.x. [DOI] [PubMed] [Google Scholar]
- Beitchman JH, Hood J, Rochon J, Peterson M. Empirical classification of speech/language impairment in children II. Behavioral characteristics. J Am Acad Child Adolesc Psychiatry. 1989;28:118–123. doi: 10.1097/00004583-198901000-00022. [DOI] [PubMed] [Google Scholar]
- Beitchman JH, Hood J, Rochon J, Peterson M, Mantini T, Majumdar S. Empirical classification of speech/language impairment in children I. Identification of speech/language categories. J Am Acad Child Adolesc Psychiatry. 1989;28(1):112–117. doi: 10.1097/00004583-198901000-00021. [DOI] [PubMed] [Google Scholar]
- Beitchman JH, Nair R, Clegg M, Ferguson B, Patel PG. Prevalence of psychiatric disorders in children with speech and language disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1986;25(4):528–535. doi: 10.1016/s0002-7138(10)60013-1. [DOI] [PubMed] [Google Scholar]
- Beitchman JH, Wilson B, Johnson C, Atkinson L, Young AR, Adlaf E, Douglas L. Fourteen-year follow-up of speech/language-impaired and control children: psychiatric outcome. Journal of American Academy of Child and Adolescent Psychiatry. 2001;40(1):75–82. doi: 10.1097/00004583-200101000-00019. [DOI] [PubMed] [Google Scholar]
- Camarata SM, Hughes CA, Ruhl KL. Mild/moderate behaviorally disorder students: a population at risk for language disorders. Language, Speech, and Hearing Services in Schools. 1988;19:191–200. [Google Scholar]
- Cantwell DP, Baker L. Clinical significance of children with communication disorders: perspectives from a longitudinal study. Journal of Child Neurology. 1987;2:257–264. doi: 10.1177/088307388700200404. [DOI] [PubMed] [Google Scholar]
- Cohen NJ, Barwick MA, Horodezky MB, Vallance DD, Im N. Language, achievement, and cognitive processing psychiatrically disturbed children with previously unidentified and unsuspected language impairements. J Child Psychol Psychiatry. 1998;39(6):865–877. [PubMed] [Google Scholar]
- Cohen NJ, Davine M, Meloche-Kelly M. Prevlance of unsuspected language disorders in a child psychiatric population. J Am Acad Child Adolesc Psychiatry. 1989;28:107–111. doi: 10.1097/00004583-198901000-00020. [DOI] [PubMed] [Google Scholar]
- Cohen NJ, Davine N, Horodezky MB, Lipsett L, Isaacson L. Unsuspected language impairment in psychiatrically disturned children: Prevalence and language and behavioral characteristics. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:595–603. doi: 10.1097/00004583-199305000-00016. [DOI] [PubMed] [Google Scholar]
- Cohen NJ, Vallance DD, Barwick MA, Im N, Menna R, Horodezky MB, Isaacson L. The interface between ADHD and language impairment: An examination of language, achievement and cognitive processing. Journal of Child Psycholgy and Psychiatry. 2000;41(3):353–362. [PubMed] [Google Scholar]
- Ebert KD, Kohnert K. Sustained attenion in children with primary language impairment: A meta-analysis. Journal of Speech, Language, and Hearing Research. 2011;54:1372–1384. doi: 10.1044/1092-4388(2011/10-0231). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finneran DA, Francis AL, Leonard LB. Sustained attention in children wtih Specific Language Impairment (SLI) Journal of Speech, Language, and Hearing Research. 2009;52:915–929. doi: 10.1044/1092-4388(2009/07-0053). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gualtieri C, Koriath U, van Bourgondien M, Saleeby N. Language disorders in children referred for psychiatric services. J Am Acad Child Psychiatry. 1983;22:165–171. doi: 10.1016/s0002-7138(09)62330-x. [DOI] [PubMed] [Google Scholar]
- Howlin P, Rutter M. The consequences of language delay for other aspects of development. In: Yule W, Rutter M, editors. Language Development and Disorders. Oxford: Blackwell Publishers; 1987. pp. 271–294. [Google Scholar]
- Love AJ, Tompson MGG. Language disorders and attention deficit disorder in young children referred for psychiatric assessment. American Journal of Orthopsychiatry. 1988;58:52–63. doi: 10.1111/j.1939-0025.1988.tb01566.x. [DOI] [PubMed] [Google Scholar]
- Lynam D, Moffitt T, Stouthamer-Loeber M. Explaining the relation between IQ and delinquency: Class, race, test motivation, school failure, or self-control? Journal of Abnormal Child Psychology. 1993;102:187–196. doi: 10.1037//0021-843x.102.2.187. [DOI] [PubMed] [Google Scholar]
- Rice ML. “Don’t talk to him; he’s werid”: A social consequences account of language and social interactions. Baltimore, MD: Paul H. Brookes Publsihing; 1993. [Google Scholar]
- Schul R, Stiles J, Wulfeck B, Townsend J. How ‘generalised’ is the ‘slowed processing’ in SLI? The case of visuospatial attentional orienting. Neuropsychologia. 2004;42:661–671. doi: 10.1016/j.neuropsychologia.2003.10.010. [DOI] [PubMed] [Google Scholar]
- Spaulding TJ, Plante E, Vance R. Sustained selective attention skills of preschool children with specific language impairment: Evidence for separate attentional capacities. Journal of Speech, Language, and Hearing Research. 2008;51:16–34. doi: 10.1044/1092-4388(2008/002). [DOI] [PubMed] [Google Scholar]
- Stevens C, Fanning J, Coch D, Sanders L, Neville H. Neural mechanisms of selective auditory attention are enhanced by computerized training: Electrophysiological evidence from language-impaired and typically developing children. Brain Research. 2008;1205:55–69. doi: 10.1016/j.brainres.2007.10.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tirosh E, Cohen NJ. Language deficit with attention-deficit disorder: A prevalent comorbidity. Journal of Child Neurology. 1998;13(10):493–497. doi: 10.1177/088307389801301005. [DOI] [PubMed] [Google Scholar]
- Tomblin JB. The EpiSLI Database: A Publicly Available Database on Speech and Language. Language, Speech, and Hearing Services in Schools. 2010;41:108–117. doi: 10.1044/0161-1461(2009/08-0057). [DOI] [PubMed] [Google Scholar]
- Tomblin JB, Records N, Zhang X. A system for the diagnosis of specific language impairment in kindergarten children. Journal of Speech and Hearing Research. 1996a;39:1284–1294. doi: 10.1044/jshr.3906.1284. [DOI] [PubMed] [Google Scholar]
- Tomblin JB, Records NL, Buckwalter P, Zhang X, Smith E, O’Brien M. Prevalence of specific language impairment in kindergarten children. J Speech Lang Hear Res. 1997;40(6):1245–1260. doi: 10.1044/jslhr.4006.1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomblin JB, Records NL, Zhang X. A system for the diagnosis of specific language impairment in kindergarten children. J Speech Hear Res. 1996b;39(6):1284–1294. doi: 10.1044/jshr.3906.1284. [DOI] [PubMed] [Google Scholar]
- Tomblin JB, Smith E, Zhang X. Epidemiology of specific language impairment: prenatal and perinatal risk factors. J Commun Disord. 1997;30(4):325–343. doi: 10.1016/s0021-9924(97)00015-4. quiz 343–324. S0021-9924(97)00015-4 [pii] [DOI] [PubMed] [Google Scholar]
- Trautman RC, Giddan JJ, Jurs SG. Language risk factor in emotionally disturbed children within a school and day treatment program. Journal of Childhood Communication Disorders. 1990;13:123–133. [Google Scholar]


