Significance
Credit scoring is expanding into domains beyond lending. Today, credit scores are used by employers, utility companies, and automobile insurers to index high-risk behavior. Life insurance companies even incorporate credit scores into actuarial models. This expansion is controversial, as it is unclear what personal attributes credit scores capture. Following 1,000 individuals from birth to midlife, we show that low credit scores predict cardiovascular disease risk. We also show that the reason credit scores are broadly applicable as a risk stratification tool is because they capture enduring histories of human capital, beginning in childhood. These findings call attention to privacy concerns in a surveillance society, the value of financial literacy, and the importance of early childhood intervention to promote healthy aging.
Keywords: credit score, cardiovascular disease risk, human capital, consumer finance
Abstract
Credit scores are the most widely used instruments to assess whether or not a person is a financial risk. Credit scoring has been so successful that it has expanded beyond lending and into our everyday lives, even to inform how insurers evaluate our health. The pervasive application of credit scoring has outpaced knowledge about why credit scores are such useful indicators of individual behavior. Here we test if the same factors that lead to poor credit scores also lead to poor health. Following the Dunedin (New Zealand) Longitudinal Study cohort of 1,037 study members, we examined the association between credit scores and cardiovascular disease risk and the underlying factors that account for this association. We find that credit scores are negatively correlated with cardiovascular disease risk. Variation in household income was not sufficient to account for this association. Rather, individual differences in human capital factors—educational attainment, cognitive ability, and self-control—predicted both credit scores and cardiovascular disease risk and accounted for ∼45% of the correlation between credit scores and cardiovascular disease risk. Tracing human capital factors back to their childhood antecedents revealed that the characteristic attitudes, behaviors, and competencies children develop in their first decade of life account for a significant portion (∼22%) of the link between credit scores and cardiovascular disease risk at midlife. We discuss the implications of these findings for policy debates about data privacy, financial literacy, and early childhood interventions.
What can a person’s credit history tell you about their future health? The credit score—a computationally derived metric of a person’s financial history—was initially devised to stratify consumers based on the likelihood that they will pay back their debts. The use of credit scores as a screening tool has proven so successful that it has expanded well beyond consumer credit and into our everyday lives. Companies use credit scores to set interest rates for home mortgages and college loans, to tier premiums for car insurance, to price cell phone contracts and cable TV bills, and even to confer eligibility for employment (1). The expansion of credit scores into domains not directly related to creditworthiness raises questions about what personal characteristics underpin credit scores and whether these characteristics constitute legitimate grounds for screening individuals (2, 3). Nowhere is this concern more pronounced than in the application of credit scores to grade health risks. Life insurance companies have begun incorporating credit scores into predictive models of health and longevity (4, 5).
Despite the proven use of credit scoring techniques for facilitating risk assessment across industry, very little is known about the underlying factors that determine why credit scores are so broadly predictive. Some proponents of credit-scoring practices beyond lending argue that the same attributes that determine creditworthiness also guide behavior in other domains of life (6). Individuals who avoid risky and impulsive decisions, who plan and manage their finances, and who generally organize their lives are more likely to achieve better job performance, safer driving, and better health (7). The credit score, in this light, is a distillation of difficult-to-observe psychological traits and personal background into a prognostic index with high penetrance and wide application (7–9). In the current study we test this hypothesis by examining the association between credit scores and a seemingly distally related indicator: risk for cardiovascular disease. Established evidence that behavioral factors are central determinants of cardiovascular disease (10, 11) leads us to ask whether credit scores and cardiovascular disease risk are related because financial management and health management share a common constellation of contributory personal characteristics (12).
Individuals vary in their education, cognitive abilities, and noncognitive skills such as self-control, planfulness, and perseverance (13). Extensive social science research has documented that these three factors—collectively titled “human capital”—have stable and enduring effects on social and occupational attainment, earnings, and health (14–18). Here we test if the personal characteristics that make up human capital are the same characteristics that underpin credit scores and that account for covariation between credit scores and cardiovascular disease risk. To clarify whether the link between credit scores and cardiovascular disease risk can be attributed specifically to human capital factors, we also examine two alternative hypotheses: (i) credit scores may be linked to cardiovascular disease risk due to recent adverse shocks (such as job loss or illness) that undermine both credit scores and physical health and (ii) credit scores may be linked to cardiovascular disease risk due to a common association with income. We test these hypotheses in the context of the Dunedin (New Zealand) Study, a 1972–1973 birth cohort of 1,037 individuals followed from birth and repeatedly assessed, most recently in 2012, when study members were 38 y old. The cohort has suffered less than 5% attrition and spans the entire range of socioeconomic status so individuals with poor credit scores and/or high cardiovascular disease risk have not selectively dropped out of the study. As the cohort study members approach midlife, many are primed for major property purchases, starting a business, and taking out a life insurance policy. Amid these contingencies, their credit scores weigh heavily on their future life chances.
Results
Are Low Credit Scores Linked to Increased Risk for Cardiovascular Disease?
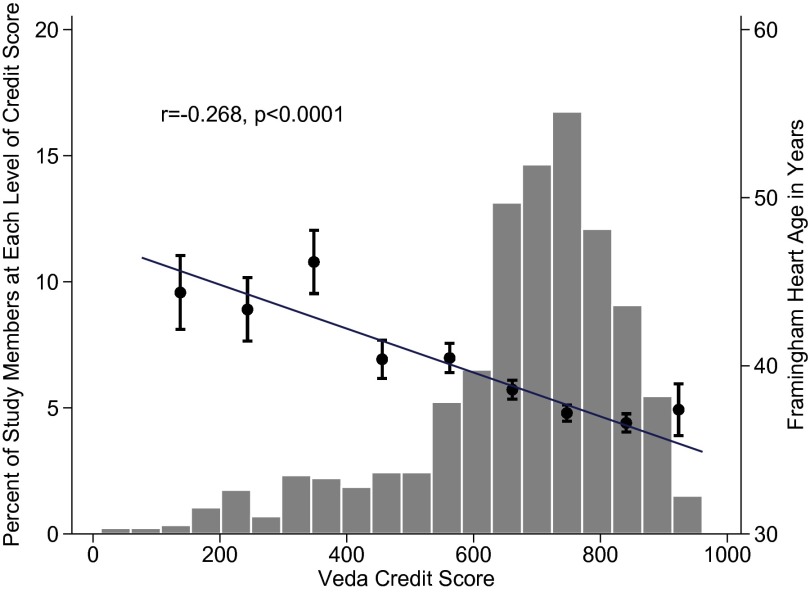
We assessed our study members’ credit scores by linking to administrative records acquired from the Veda Company, the largest credit reference agency in New Zealand and Australia (see Methods for more details). The credit scores of our study members ranged from 12 to 961 (mean = 675.2; SD = 168.6). We assessed our study members’ cardiovascular disease risk using the Framingham cardiovascular risk score, an omnibus measure of cardiovascular disease risk widely used by health care practitioners and insurance companies to predict future morbidity and mortality (19). Each study member’s cardiovascular disease risk was computed using risk factors collected during clinical assessments, including total cholesterol, HDL cholesterol, systolic blood pressure, diabetes status, and smoking status (see Methods for more details). Cardiovascular risk scores were then translated to a Framingham heart age for ease of communication and interpretation. Because cohort members were all born within a 12-mo period, their chronological age was fixed at 38 y; however, their heart age varied considerably, ranging from 22 to 85 y (mean = 38.5 SD = 8.0). Fig. 1 shows that study members with lower age 38 credit scores were at greater risk for age 38 cardiovascular disease; each 100-point difference in credit score was associated with a 13-mo difference in heart age.
Fig. 1.
Association between credit scores and Framingham heart age. The histogram shows the distribution of study members’ Veda credit scores (mean = 675.2). The dots and SE bars show average heart age for study members with credit scores <200, 201–300, 301–400, 401–500, 501–600, 601–700, 701–800, 801–900, and >900. All cohort members were aged 38 y at the time of credit reporting and heart age assessment. Heart age ranged from 22 to 85 y (mean = 38.5 y). The regression line shows the association between Veda credit score and Framingham heart age (r = −0.268). This association was similar for men (r = −0.236) and women (r = −0.259). The sex-adjusted association (r = −0.247) was used for all subsequent analyses examining the association between credit scores and heart age.
We next turned to test possible explanations for the observed association between study members’ credit scores and their heart age.
Do Recent Adverse Shocks Account for the Link Between Credit Scores and Cardiovascular Disease Risk?
The association we observed between credit scores and heart age could arise from recent adverse shocks that negatively affect financial and physical well-being. Three such examples are as follows: (i) physical illness impairing job productivity leading to financial distress; (ii) unemployment causing financial distress leading to impaired health; and (iii) extraordinary shocks leading to both financial distress and to impaired health. We tested the degree to which the association between credit scores and heart age was attributable to such adverse shocks. We acquired records from the New Zealand Ministry of Social Development relating to sickness and unemployment claims in the last 6 y and identified study members who were recently seriously ill (n = 81) or unemployed (n = 88). We also used self-reports to identify study members exposed to a set of exogenous shocks causing massive financial and physical distress (20, 21): the 2010–2011 Christchurch earthquakes (n = 93; see Methods for details).
On average, study members exposed to any of these recent events (n = 222) had credit scores that were 97 points lower (β = −0.25, P < 0.001) and heart ages that were 19 mo older (β = 0.08, P = 0.017), confirming the expected association of recent adverse shocks with impaired financial and physical well-being. A structural equation model (SEM) examining the residual correlation between credit scores and heart age revealed that adjustment for these adverse shocks reduced the correlation between credit scores and heart age by 6% (from r = −0.247 to r = −0.232; see Figs. S1 and S2 for sensitivity analyses). To test the significance of this reduction we replicated the SEM model just described, but constrained credit-score-to-heart-age covariance to its initial level absent adjustment for recent adverse shocks (covariance = −300.11; r = −0.247). This constrained model did not result in significantly poorer fit compared with the unconstrained model {[Δχ2(1), n = 817] = 0.42, P = 0.516}. This model comparison indicates that, although adverse shocks may have lowered credit scores or exacerbated cardiovascular disease risk, adverse shocks did not account for a significant portion of the cohort’s covariance between credit scores and cardiovascular disease risk.
Are Credit Scores and Cardiovascular Disease Risk Linked Because of Income?
The association we observe between credit scores and heart age could arise from a common association with income. Health inequalities are not equally distributed across income levels. Also, although income is not a direct input into credit-scoring models, income clearly affects the ability to pay back loans and bills. Under this hypothesis, credit scores may simply represent income differences grading individuals’ opportunity to invest in their health and avoid certain health risks. To address this possibility, we collected information about each study member’s age 38 household income and examined how adjustment for income affected the correlation between credit scores and heart age. As expected, study members with higher household incomes were more likely to have higher credit scores (β = 0.31, P < 0.001) and younger heart age (β = −0.14, P < 0.001); an NZ $10,000 rise in household income predicted a 12-point higher credit score and a 3-mo younger heart age. An SEM model examining the residual correlation between credit scores and heart age revealed that the credit-score-to-heart-age correlation was reduced by 15% (from r = −0.247 to r = −0.209) after adjusting for income (Fig. S2). We tested the significance of this reduction by replicating the aforementioned SEM model, but constraining credit-score-to-heart-age covariance to its initial level absent adjustment for household income. This constrained model did not result in significantly poorer fit compared with the unconstrained model {[Δχ2(1), n = 817] = 2.23, P = 0.135}, indicating that income did not account for a significant portion of the covariation between credit scores and cardiovascular disease risk. This model was also not significant after simultaneously accounting for both household income and adverse shocks (Fig. S3).
Previous studies have suggested that year-to-year fluctuations in earnings make past-year income a less reliable indicator than permanent income, which is based on a multiyear assessment (22). To account for this possibility, we conducted a sensitivity analysis replacing past-year income with 7-y income, assessed by averaging household income across age 32 and age 38 assessments. This analysis confirmed that income did not account for a significant portion of the covariation between credit scores and cardiovascular disease risk (Fig. S4).
Are Credit Scores and Cardiovascular Disease Risk Linked Due to Contemporaneous Human Capital Factors?
Alternatively, the association we observe between credit scores and heart age could arise from a common set of behaviors and competencies that either promote or mitigate prudent financial decision making and health management. Social science research has long recognized the contribution of human capital factors such as educational attainment, cognitive ability, and self-control as early predictors of health and successful aging. Although no similar program of research identifying the psychological underpinnings of credit scores has yet to develop, the industry-wide use of credit scoring models for stratifying population segments into risk tiers suggests that, in practice, credit scores may already be serving a similar function as a proxy for personal characteristics of prudent decision-making. To test the contribution of human capital factors in explaining the link between credit scores and cardiovascular disease risk, we assessed study members’ educational attainment, cognitive ability, and self-control, and then examined the extent to which these human capital factors accounted for covariation between credit scores and cardiovascular disease risk. Educational attainment was assessed based on study members’ highest level of education by age 38. Cognitive ability was assessed using IQ tests at the age 38 study assessment. Self-control at age 38 was assessed using personality ratings of conscientiousness, a trait indexing a propensity to be planful, organized, and perseverant (see Methods for details).
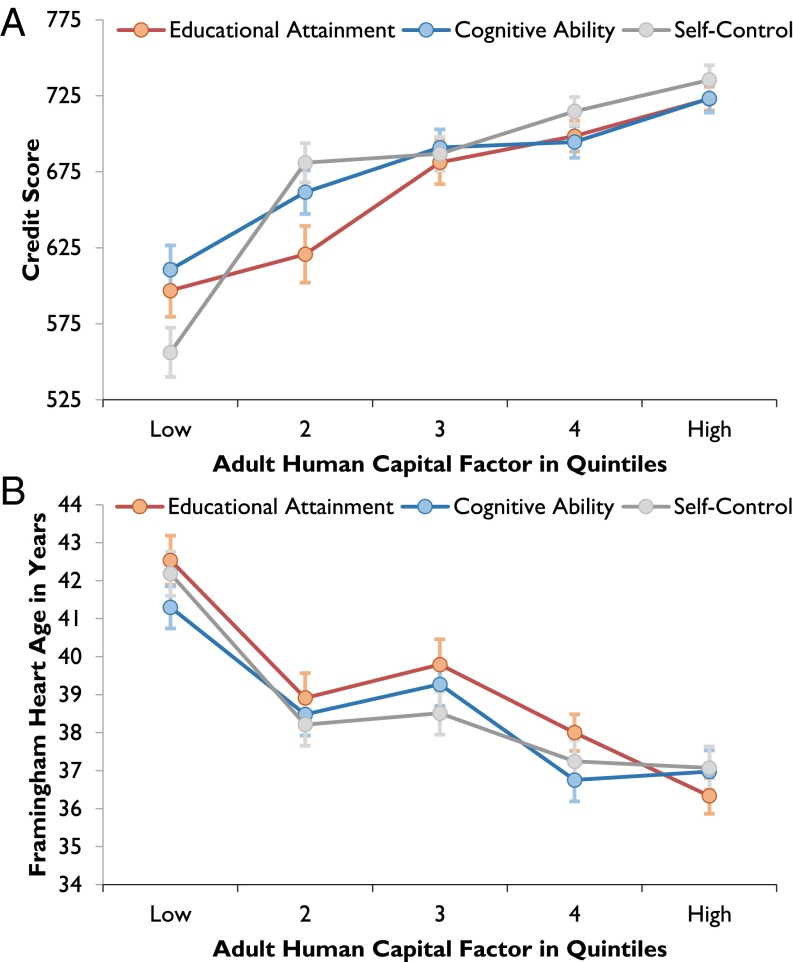
All three adult human capital factors—educational attainment, cognitive ability, and self-control—predicted both higher credit scores (Fig. 2A) and younger heart age (Fig. 2B). All three human capital factors were also positively associated with income (educational attainment: β = 0.39, P < 0.001; cognitive ability: β = 0.35, P < 0.001; self-control β = 0.38, P < 0.001); however, multivariate regression models revealed that all three human capital factors were associated with creditworthiness and heart age independent of income (Tables S1–S4).
Fig. 2.
Associations between adult human capital factors, credit scores, and heart age. Individual differences in study members’ educational attainment, adult cognitive ability, and self-control were associated with their (A) credit score (educational attainment: β = 0.28, P < 0.001; cognitive ability: β = 0.24, P < 0.001; self-control: β = 0.37, P < 0.001) and (B) heart age (educational attainment: β = −0.23, P < 0.001; cognitive ability: β = −0.20, P < 0.001; self-control: β = −0.23, P < 0.001). The dots and SE bars show the association between each quintile of a given adulthood human capital factor with credit score and heart age. Quintiles are shown for illustrative purposes; all statistical analyses were performed using continuous measures.
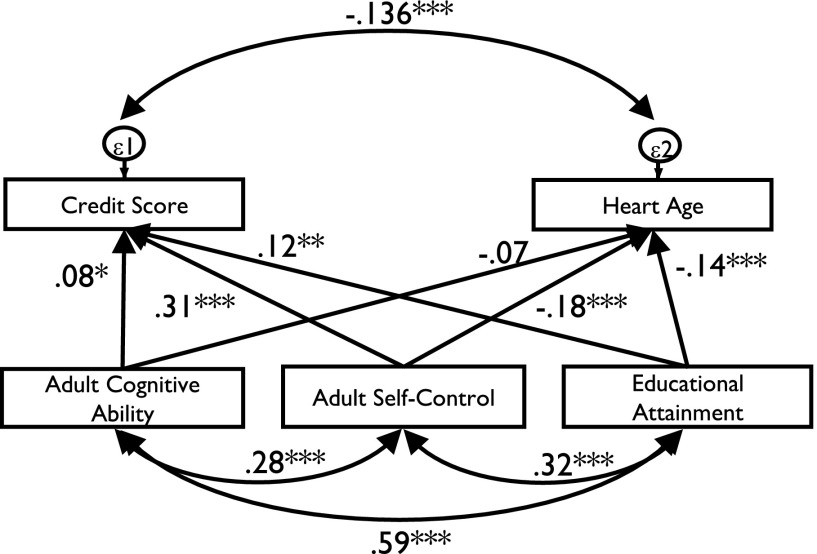
To examine the role of human capital factors in explaining covariation between credit scores and heart age, we used the same SEM framework we used for adverse shocks and for income, only this time substituting human capital factors (Fig. 3). In contrast to the modest changes in correlation between credit scores and heart age evidenced when adjusting for adverse events and income, adjusting for human capital factors reduced the correlation between credit scores and heart age by 45% (from r = −0.247 to r = −0.136). As before, we tested the significance of this reduction by constraining credit-score-to-heart-age covariance to initial levels absent adjustment for adult human capital factors. This constrained model resulted in a significantly poorer fit compared with the model wherein this constraint was not imposed {[Δχ2(1), n = 817] = 15.98, P < 0.001}. Thus, in contrast to adverse shocks and income, adult human capital factors not only were linked to credit scores and heart age, but also significantly accounted for why credit scores and heart age covary.
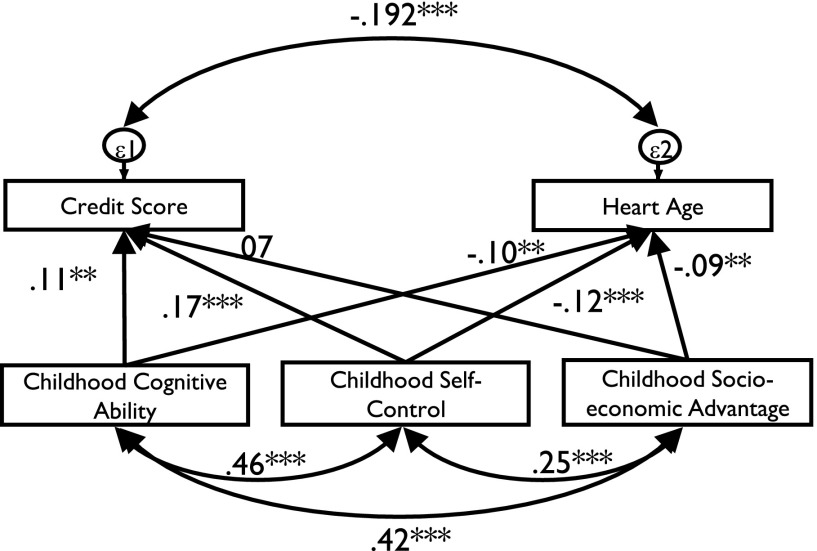
Fig. 3.
Effect of adult human capital factors on the covariation between credit scores and heart age. This structural equation model illustrates the role of human capital factors in the correlation between credit scores and heart age. Values associated with the paths represent standardized parameter estimates. Single headed arrows represent causal paths and double-headed arrows represent covariances. Sex (not presented) is included as a covariate with paths to all variables. Comparison with a model where the covariance between credit scores and heart age is constrained to initial levels showed that human capital factors accounted for a significant source of the link between credit scores and heart age. *P < 0.05, **P < 0.01, ***P < 0.001.
Can Covariation in Midlife Credit Scores and Cardiovascular Disease Risk Be Traced Back to Childhood Human Capital?
Our analyses provide initial evidence that credit scores and cardiovascular disease risk are linked due to shared human capital factors. However, because credit scores, heart age, and human capital were assessed cross-sectionally at age 38, the capacity of these analyses to establish causal inference is limited. For example, it is possible that poor credit scores or poor cardiovascular health lead to reduced human capital investment (23, 24), which could result in a similar pattern of association as seen here. To rule out the possibility of reverse causation and to assess the early-life contribution of human capital factors, we traced adult human capital factors to their childhood antecedents and then examined if childhood human capital could presage credit scores, heart age, and their covariation. Childhood human capital measures were derived as previously reported (18, 25) and represent foundational competencies of successful development. Three measures—childhood socioeconomic advantage, childhood cognitive ability, and childhood self-control—formed our measures of childhood human capital (see Methods for details). We measured the family socioeconomic status of study members when they were children to capture the social advantages in childhood that give rise to educational attainment. We measured childhood cognitive ability, the direct antecedent of adult cognitive ability. We also measured childhood self-control, the direct antecedent of adult self-control. Childhood human capital factors were all assessed in the first decade of life and, despite the passage of nearly three decades, childhood factors were all significantly correlated with their corresponding adult measures (r = 0.40 for family socioeconomic status to educational attainment, r = 0.81 for childhood cognitive ability to adult cognitive ability, and r = 0.36 for childhood self-control to adult self-control; all P < 0.001). We make no assumptions about the etiology of these measures of childhood human capital, which may derive from a wide variety of biological, psychological, and sociocultural factors.
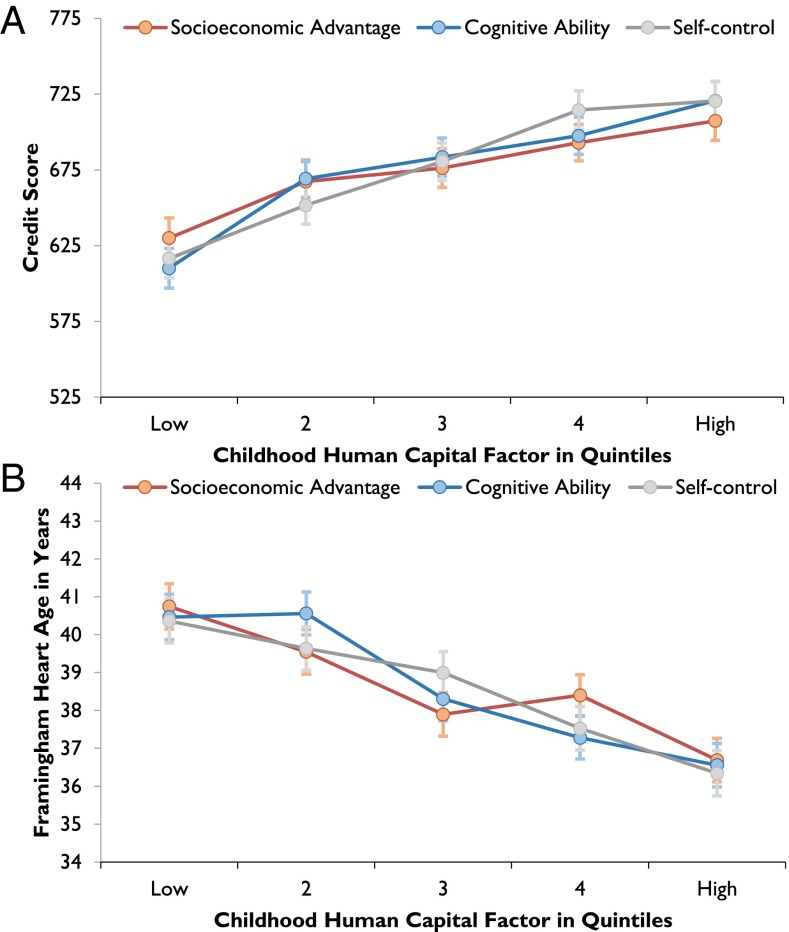
Fig. 4 shows that childhood socioeconomic advantage, cognitive ability, and self-control each predicted study members’ adult credit scores (Fig. 4A) and heart age (Fig. 4B). The associations between childhood human capital factors, credit scores, and heart age were significantly mediated by adult human capital. Adult human capital factors mediated between 64% and 82% of childhood effects on credit scores and between 75% and 87% of childhood effects on heart age (Table S5).
Fig. 4.
Associations between childhood human capital factors, credit scores, and heart age. Individual differences in study members’ childhood socioeconomic advantage, cognitive ability, and self-control forecast their (A) adult creditworthiness (socioeconomic advantage: β = 0.16, P < 0.001; cognitive ability: β = 0.21, P < 0.001; self-control: β = 0.23, P < 0.001) and (B) cardiovascular health risk (socioeconomic advantage: β = −0.17, P < 0.001; cognitive ability: β = −0.19, P < 0.001; self-control: β = −0.18, P < 0.001). The dots and SE bars show the association between each quintile of a given childhood human capital factor with credit score and heart age. Quintiles are shown for illustrative purposes; all statistical analyses were performed using continuous measures.
To test whether childhood human capital also accounted for covariation between credit scores and heart age, we replicated our previous SEM model, but substituted adult human capital factors with their childhood antecedents (Fig. 5). This model showed that adjusting for childhood human capital factors reduced the correlation between credit scores and heart age by 22% (from r = −0.247 to r = −0.192). Constraining the covariance between credit scores and heart age to its initial level, absent adjustment for childhood factors, resulted in significantly poorer fit {[Δχ2(1), n = 817] = 3.97, P = 0.046}, indicating that a significant portion of credit-score-to-heart-age covariance in adulthood was accounted for by the characteristic behaviors, skills, and attitudes study members developed in their first decade of life.
Fig. 5.
Effect of childhood human capital factors on credit scores, heart age, and their covariation. This structural equation model is the same as Fig. 3, except adult human capital factors have been replaced with their childhood antecedents. The values associated with the paths represent standardized parameter estimates. Controlling for childhood human capital reduces the standardized covariation between credit score and heart age from r = −0.247 to r = −0.192, a reduction of 22%. Sex (not presented) is included as a covariate with paths to all variables. *P < 0.05, **P < 0.01, ***P < 0.001.
Discussion
The current study elucidates a human capital perspective on the meaning of the credit score. Amid growing public concern over extending the use of credit scores to domains beyond lending (2, 3), we find that credit scores modestly but significantly predict risk for cardiovascular disease in a cohort of adults entering midlife. Interestingly, credit scores did not simply act as a proxy for income; instead, the link between credit scores and cardiovascular disease risk was largely explained by study members’ level of human capital: their educational attainment, cognitive ability, and self-control. The temporal precedence of human capital in this relationship was supported by our observation that childhood human capital factors assessed in the first decade of life partially explained the covariation between credit scores and heart age. Although childhood human capital did not explain the credit score–heart age connection completely, its contribution was notable, given that 30 y elapsed between predictor and outcome measurements. These findings raise several considerations for policy and future research.
The first consideration relates to the social welfare climate of our New Zealand-based study. Our finding that adverse life events did not significantly attenuate the association between credit scores and heart age should be interpreted within the context of New Zealand’s social service programs and universal health care policy. A recent analysis of New Zealand census data indicated that 5% of bankruptcies could be attributed to ill health or the absence of health insurance (26). This figure stands in stark contrast to the United States, where it has been reported that >60% of bankruptcies are due to medical-related expenses (27). The issue of uncollected medical debt damaging credit scores, a growing concern in the United States (28, 29), should be less influential in our New Zealand-based study. Our empirical findings are largely consistent with this assumption. Linking to administrative records of study members’ social welfare benefits, we find that the general association between credit scores and heart age could not be explained by study members’ recent illness lowering their credit score or recent unemployment raising their cardiovascular disease risk. Furthermore, exposure to the Christchurch earthquakes, examples of extraordinary exogenous shocks, did not materially affect the link between credit scores and cardiovascular disease risk. Nevertheless, our finding that ∼45% of the correlation between credit scores and heart age could be accounted for by human capital factors raises the question of what unobserved sources may be contributing to the remaining heterogeneity. Previous research has noted the practical challenges inherent in identifying the myriad situational circumstances (e.g., local market conditions, inaccuracies in credit history reporting, and adverse personal events) that may affect the predictive validity of credit scores (30). International replications of our study are needed.
A second consideration relates to the extension of credit scoring practices to domains beyond lending. Our finding that credit scores predict risk for cardiovascular disease provides empirical support for credit-based scoring techniques in the life insurance industry. Our integration of psychometric assessment to explain the nature of this relationship is a first step in understanding why credit scores and cardiovascular disease risk are linked. Our findings suggest that life insurance companies that acquire an applicant’s credit score are also indirectly acquiring information about that applicant’s educational attainment, intelligence, and personality, right back to childhood. We suspect that citizens are unaware of the degree to which credit scores provide insight into such private and sensitive domains. Individuals who may never consent to a personality test or an IQ test before applying for insurance are unwittingly consenting to reveal this information when granting access to their credit scores. Credit scoring is an unobtrusive measure that reveals quite a bit about a person. Future debate on the extended use of credit scoring techniques should consider threats to privacy and confidentially. Interestingly, in developing countries where credit scores are either unobtainable or unreliable, measurement of an individual’s conscientious personality is successfully being used as a substitute for credit scores (31).
A third consideration relates to the timing of interventions to promote financial and physical well-being. We found that a portion of the link between credit scores and cardiovascular disease risk was explained by personal characteristics already present in the first decade of life. Compared with children in the top quintile of self-control, children in the bottom quintile went on to develop heart ages that were on average 4 y older and credit scores that were on average 103 points lower. Other childhood human capital factors had similar effects. Childhood self-control is of particular interest because of evidence that self-control is amenable to intervention early in life, and because economic models suggest that early investment may be more cost-effective than later remediation (32, 33). Our findings suggest that interventions successful at improving children’s self-control may benefit their financial and physical well-being decades later in life.
Our life chances often depend on how we are evaluated by others. Today more than ever, many of these evaluations—obtaining a college loan, getting a job interview, and securing a mortgage—are conducted by people we will never meet, using proprietary algorithms to which we are not privy. In these impersonal contexts, credit scores have replaced personal reputational relationships as rationalized gauges of character and competence. Although policy debate about the consequences of expanded credit scoring jumps ahead, our understanding of the psychological factors that lead credit scores to be useful lags behind. In this study, we present evidence that the reason credit scores predict distally related domains such as cardiovascular disease risk is because credit scores capture enduring histories of human capital.
Methods
A more detailed report of the study design and analyses is available in the SI Text.
Dunedin Study Sample.
Participants are members of the Dunedin Multidisciplinary Health and Development Study, which tracks the development of 1,037 individuals born in 1972–1973 in Dunedin, New Zealand.
Age 38 Outcomes.
Credit scores.
Credit scores were acquired at the age 38 assessment phase from the Veda Company. The Veda credit score algorithm is proprietary. Scores are based on 5-y histories of consumer credit activity and include the following factors: the number and types of credit applications and inquiries, age of credit file, residential stability, adverse information such as payment defaults and judgments, and the existence of any current or prior insolvency information. Factors such as race, national origin, marital status, occupation, salary, employment history, medical or academic records are not included in Veda scoring. Of the 961 study members who participated in the age 38 assessment, 11 did not consent to a credit rating search and 82 were not credit active in the last 5 y (the majority of whom resided overseas) and consequently had reports with no credit history, resulting in 868 valid observations. Eight study members were flagged by Veda as insolvent and were not given a credit score by Veda. We repeated all analyses with these individuals coded to the lowest credit score and with these individuals excluded from analyses. The results were unchanged. Here we report analyses based on the 860 study members with a credit score.
Heart age.
Heart age is an estimate of vascular age based on the Framingham cardiovascular disease (CVD) risk score, a single multivariable function that predicts risk of developing all-CVD and its constituents (19). The 10-y CVD risk for each study member was computed using sex-specific factors collected at the age 38 assessment phase including: total cholesterol, HDL cholesterol, systolic blood pressure, diabetes status, and smoking status. Framingham CVD risk was then translated to heart age using the heart age calculators made available by the Framingham group (19). We excluded pregnant study members and study members who did not consent to phlebotomy, resulting in 900 valid observations.
Age 38 Covariates.
Social welfare benefits.
We conducted record linkage with the New Zealand Ministry of Social Development to identify study members who drew on government benefits. Because by New Zealand law, credit scores may only refer back a maximum of 5 y for consumer credit activity, study members who received either unemployment (n = 88) or sickness (n = 81) related benefits in the prior 6 y were counted as having received a benefit. Only one benefit can be received at any given time.
Exposure to the Christchurch earthquakes.
Christchurch, New Zealand, suffered two major earthquakes during the age 38 assessment, which took place in 2010–2011. We used self-reports of study members’ residential histories to identify study members living in the Christchurch area at the time of the earthquakes (n = 93). Credit scores were retrieved in 2012; thus, the impact of these natural disasters on the financial status of our Christchurch study members would have been captured.
Household income.
Following the census (34), study members were asked to list their sources of income and given the choice of 13 different income categories to report their total pretax annual income from all sources. Study members also reported pretax annual income for cohabitating partners/spouses (if relevant). Age 38 household income was the total annual income for the study member and their partner/spouse. The median household income for our New Zealand-based study members was NZ $82,500 (SD = 41,274). Seven-year household income was assessed by averaging annual household incomes at ages 32 and 38 (median, NZ $72,500; SD, 31,720).
Age 38 Human Capital Factors.
Educational attainment.
Education level was measured on a five-point scale relevant to the New Zealand educational system: 1 = no secondary school qualifications (14.7%), 2 = school certificate (14.9%), 3 = high school graduate or equivalent (14.2%), 4 = postsecondary diploma or certificate (27.3%), 5 = bachelor’s degree or higher (28.8%).
Adult cognitive ability.
IQ at age 38 was assessed using the Wechsler Adult Intelligence Scale–Fourth Edition (35) (mean = 100, SD = 15).
Adult self-control.
Adult self-control was assessed via multiple informant reports of the personality trait of conscientiousness, as previously described (36).
Childhood Human Capital Factors.
Childhood socioeconomic status.
Children’s socioeconomic status (SES) was measured with a six-point scale assessing the occupational status of study members’ parents when study members were children. The scale places each occupation into one of six categories (from 1, unskilled laborer; to 6, professional) on the basis of educational levels and income associated with that occupation in data from the New Zealand census. Childhood SES was the average of the highest SES level of either parent from birth through age 15. This variable reflects the socioeconomic conditions experienced by the participants while they were growing up.
Childhood cognitive ability.
IQ was assessed in childhood at ages 7, 9, 11, and 13 using the Wechsler Intelligence Scale for Children–Revised (37) and was averaged across the four childhood assessment phases (mean = 100, SD = 15).
Childhood self-control.
Children’s self-control during their first decade of life was measured using a multioccasion/multi-informant strategy, as previously described (18). Briefly, the composite score includes nine measures: observational ratings of children’s lack of control (3 and 5 y of age) and parent, teacher, and self-reports of impulsive aggression, hyperactivity, lack of persistence, inattention, and impulsivity (5, 7, 9, and 11 y of age).
Supplementary Material
Acknowledgments
We thank the Dunedin Study members, their peer informants, the Unit research staff, and Study founder Phil Silva. We also thank Veda for access to the New Zealand credit check data and the New Zealand Ministry of Social Development for access to the social welfare benefit data. The Dunedin Multidisciplinary Health and Development Research Unit is supported by the New Zealand Health Research Council. This research was supported by National Institute on Aging (NIA) Grant AG032282 and UK Medical Research Council Grant MR/K00381X. Additional support was provided by the Jacobs Foundation. S.I. was supported by a Rothschild Fellowship from the Yad Hanadiv Rothschild Foundation. D.W.B. was supported by NIA Grants T32-AG000029 and P30 AG028716-08.
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1409794111/-/DCSupplemental.
References
- 1.consumer.gov 2014. Your credit history. Available at: www.consumer.gov/articles/1009-your-credit-history#!what-to-know. Accessed April 7, 2014.
- 2. (2010) Use of credit information beyond lending: Issues and reform proposals. Hearing before the Subcommittee on Financial Institutions and Consumer Credit of the Committee on Financial Services, US House of Representatives, 111th Congress, second session, May 12, 2010. Available at www.gpo.gov/fdsys/pkg/CHRG-111hhrg58044/html/CHRG-111hhrg58044.htm. Accessed April 7, 2014.
- 3. (2010) Keeping score on credit scores: An overview of credit scores, credit reports, and their impact on consumers. Hearing before the Subcommittee on Financial Institutions and Consumer Credit of the Committee on Financial Services, US House of Representatives, 111th Congress, second session, March 24, 2010. Available at www.gpo.gov/fdsys/pkg/CHRG-111hhrg56781/html/CHRG-111hhrg56781.htm. Accessed April 7, 2014.
- 4.Dion MS. Predictive modeling: A life underwriter's primer. On the Risk. 2011;27(2):36–43. [Google Scholar]
- 5.Batty M, et al. Predictive Modeling for Life Insurance, Ways Life Insurers Can Participate in the Business Analytics Revolution. Deloitte Development LLP; New York: 2010. [Google Scholar]
- 6.Hartwig RP, Wilkinson C. The use of credit information in personal lines insurance underwriting. Insurance Issues Ser. 2003;1(2):1–10. [Google Scholar]
- 7.Brockett PL, Golden LL. Biological and psychobehavioral correlates of credit scores and automobile insurance losses: Toward an explication of why credit scoring works. J Risk Insur. 2007;74(1):23–63. [Google Scholar]
- 8.Meier S, Sprenger CD. Time discounting predicts creditworthiness. Psychol Sci. 2012;23(1):56–58. doi: 10.1177/0956797611425931. [DOI] [PubMed] [Google Scholar]
- 9.Bernerth JB, Taylor SG, Walker HJ, Whitman DS. An empirical investigation of dispositional antecedents and performance-related outcomes of credit scores. J Appl Psychol. 2012;97(2):469–478. doi: 10.1037/a0026055. [DOI] [PubMed] [Google Scholar]
- 10.Yusuf S, et al. INTERHEART Study Investigators Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet. 2004;364(9438):937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 11.Roger VL, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee Heart disease and stroke statistics—2012 update: A report from the American Heart Association. Circulation. 2012;125(1):e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gubler T, Pierce L. Healthy, wealthy, and wise: Retirement planning predicts employee health improvements. Psychol Sci. 2014;25(9):1822–1830. doi: 10.1177/0956797614540467. [DOI] [PubMed] [Google Scholar]
- 13.Almlund M, Duckworth AL, Heckman JJ, Kautz TD. 2011. Personality psychology and economics. NBER Working Paper (National Bureau of Economic Research, Cambridge, MA), No 16822.
- 14.Becker GS. Investment in human capital: A theoretical analysis. J Polit Econ. 1962;70(5):9–49. [Google Scholar]
- 15.Heckman JJ, Stixrud J, Urzua S. 2006. The effects of cognitive and noncognitive abilities on labor market outcomes and social behavior. NBER Working Paper (National Bureau of Economic Research, Cambridge, MA), No 12006.
- 16.Poulton R, et al. Association between children’s experience of socioeconomic disadvantage and adult health: A life-course study. Lancet. 2002;360(9346):1640–1645. doi: 10.1016/S0140-6736(02)11602-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burks SV, Carpenter JP, Goette L, Rustichini A. Cognitive skills affect economic preferences, strategic behavior, and job attachment. Proc Natl Acad Sci USA. 2009;106(19):7745–7750. doi: 10.1073/pnas.0812360106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moffitt TE, et al. A gradient of childhood self-control predicts health, wealth, and public safety. Proc Natl Acad Sci USA. 2011;108(7):2693–2698. doi: 10.1073/pnas.1010076108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.D’Agostino RB, Sr, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117(6):743–753. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 20.Dorahy MJ, Kannis-Dymand L. Psychological distress following the 2010 Christchurch earthquake: A community assessment of two differentially affected suburbs. J Loss Trauma. 2012;17(3):203–217. [Google Scholar]
- 21.Parker M, Steenkamp D. The economic impact of the Canterbury earthquakes. Reserve Bank New Zealand Bull. 2012;75(3):13–25. [Google Scholar]
- 22.Solon G. Intergenerational income mobility in the United States. Am Econ Rev. 1992;82(3):393–408. [Google Scholar]
- 23.Stoler A, Meltzer D. Mortality and morbidity risks and economic behavior. Health Econ. 2013;22(2):132–143. doi: 10.1002/hec.2797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jayachandran S, Lleras-Muney A. Life expectancy and human capital investments: Evidence from maternal mortality declines. Q J Econ. 2009;124(1):349–397. [Google Scholar]
- 25.Meier MH, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci USA. 2012;109(40):E2657–E2664. doi: 10.1073/pnas.1206820109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.New Zealand Ministry of Business Innovation and Employment 2014. Insolvency and Trustee Service Statistical Data Report 2012-2013. Available at: www.insolvency.govt.nz/cms/site-tools/about-us/statistics/statistical-data-reports. Accessed May 20, 2014.
- 27.Himmelstein DU, Thorne D, Warren E, Woolhandler S. Medical bankruptcy in the United States, 2007: Results of a national study. Am J Med. 2009;122(8):741–746. doi: 10.1016/j.amjmed.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 28.Rosenthal E. 2014. When health costs harm your credit. The New York Times, March 9, 2014, p. SR4.
- 29. (2013) Medical debt responsibility act of 2013. 113th Congress, 1st session, §160. Available at www.congress.gov/bill/113th-congress/senate-bill/160. Accessed May 20, 2014.
- 30.Avery RB, Calem PS, Canner GB. Consumer credit scoring: Do situational circumstances matter? J Bank Finance. 2004;28(4):835–856. [Google Scholar]
- 31.Klinger B, Khwaja AI, Del Carpio C. Enterprising Psychometrics and Poverty Reduction. Springer, New York; 2013. [Google Scholar]
- 32.Heckman JJ. Policies to foster human capital. Res Econ. 2000;54(1):3–56. [Google Scholar]
- 33.Cunha F, Heckman J, Schennach S. Estimating the technology of cognitive and noncognitive skill formation. Econometrica. 2010;78(3):883–931. doi: 10.3982/ECTA6551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anonymous . New Zealand Census of Population and Dwellings. Statistics NZ; Wellington, New Zealand: 2001. [Google Scholar]
- 35.Wechsler D. Wechsler Adult Intelligence Scale. 4th Ed Pearson Asessment; San Antonio, TX: 2008. [Google Scholar]
- 36.Israel S, et al. Translating personality psychology to help personalize preventive medicine for young adult patients. J Pers Soc Psychol. 2014;106(3):484–498. doi: 10.1037/a0035687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wechsler D. Manual for the Wechsler Intelligence Scale for Children: Revised. Psychological Corporation; New York: 1974. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.