Abstract
Background
Gagging is a behavioral response that interferes with oral health care and has been suggested to relate to dental care-related fear. Little is known, however, about the epidemiology of gagging during dental treatment.
Methods
To explore this phenomenon, 478 participants were recruited from the waiting area of an oral diagnosis clinic. Participants completed the Dental Fear Survey, the Short Form-Fear of Pain Questionnaire, Dental Beliefs Scale, and a demographics questionnaire that included items about problems with gagging.
Results
Over half of the participants reported gagging on at least one occasion during dental visits, with 7.5% almost always, or always gagging. With higher frequency of problems with gagging, patients were more likely to have greater levels of dental care-related fear, fear of pain, and more negative beliefs of dental professionals and dental treatment. Further, participants who gagged more readily had greater dental care-related fear than other gaggers.
Conclusion
Gagging in the dental clinic is a prevalent problem, and dental care-related fear and fear of pain are associated with more frequent gagging.
Clinical Implications
Given the prevalence of patients reporting problem gagging, it may be helpful for providers to assess for this barrier to treatment. By targeting dental care-related fear, fear of pain, and negative beliefs about dental care in patients who often gag in the clinic, gagging may be reduced in frequency or intensity, potentially making treatment more comfortable for patients and easier for dental care providers.
Keywords: Pharyngeal reflex, gagging, dental care-related fear and anxiety, pain, behavioral sciences
Introduction
Gagging is thought to be a relatively common oral health issue.1 A behavioral response, gagging nevertheless is based on an innate biological mechanism (i.e, the pharyngeal reflex) that prevents choking.2 If stimulation is prolonged or severe, gagging may lead to vomiting.1 Although the response may be provoked in virtually all humans, the level and type of stimulation necessary to evoke gagging behavior varies across individuals.3 In addition to tactile stimulation in the mouth, gagging also may be induced by visual, auditory, or olfactory stimuli.4 This behavioral response may be induced only by stimulating anterior parts of the oral cavity, suggesting that conditioning (i.e., behavioral learning) and other psychological factors, are an important part of the etiology of frequent or “overactive” gagging.5 Indeed, though it may be elicited reflexively, the type of gagging that often is encountered by dental professionals probably is most accurately viewed as a behavioral response (i.e., an action that is the product, at least in part, of psychological variables).6,7 Gagging, especially when occurring frequently, can be particularly problematic in the context of dental care for some individuals; however, there is limited literature that specifically addresses the extent to which it interferes with treatment.
For the oral health care professional and his or her patient, gagging episodes may interrupt dental procedures, and, if severe or frequent, may even postpone dental care.1 Patients who frequently gag can be difficult to treat, and may require special care from the oral healthcare professional and/or extra time for procedures. Though it remains unknown why some patients gag while others do not, there are plausible explanations for the variation across patients. While many patients will gag with sufficient stimulation of the posterior pharynx (and glossopharyngeal nerve), which is uncommon in routine dental care, patients with gagging difficulties will gag due to sights, sounds, and odors that do not involve stimulation of any of the classic anatomic areas commonly associated with triggering a gag reflex. As mentioned above, it is likely that variation in the frequency of gagging during dental care is the result of individual differences in psychological variables. Dental care-related fear is one of those variables and warrants special consideration.
Many individuals experience some level of dental care-related fear; in fact, 45% of adult dental patients in the United States of America (USA) report at least moderate fears about dental work.8 Thus, dental care-related fear and anxiety are common problems that most dental professionals frequently encounter. A body of literature suggests that many fearful patients seek dental care only when orofacial pain is unbearable, instead of seeking preventive dental care.9 Fears about pain and negative beliefs about dental treatment and dental professionals, both of which are associated with dental care-related fear and anxiety, also contribute to the underutilization of dental care.10,11 Importantly, between 5 and 10% of citizens of the USA avoid the dentist altogether because of their anxiety and fear alone.12 This behavior has crucial public health significance reflected in the results of the first-ever Surgeon General’s report on oral health, which emphasizes that it is impossible to have good overall health without good oral health.13 Individuals who avoid dental treatment may be at greater risk for associated problems such as cardiovascular disease and diabetes, among other oral and systemic health conditions.14
Gagging is of relevance to all aspects of dental treatment, though little research exists on the etiology and epidemiology of the phenomenon. The purpose of this study was to examine the frequency and severity of gagging related to oral health care; additionally and specifically, the primary research question was whether there is a relation between gagging and dental care-related fears and beliefs. Given the possible relation between fear of the dental situation and gagging, it was hypothesized that dental patients who have problems with gagging during treatment would report: (1) higher dental care-related fear, (2) greater fears about pain, and (3) more negative beliefs about dental professionals and dental treatment, than individuals who do not gag or who gag less frequently.
Methods
Participants
Participants (n = 478; 258 female) were outpatients reporting to the West Virginia University School of Dentistry oral diagnosis clinic. Participant demographics were consistent with those of the state of West Virginia (92.0% white, 4.7% African American, 0.9% Asian, 0.7% Hispanic, 0.7% Native American, and 0.6% “other”).15 The median age of participants was 33.0 years (Range: 18–90, M = 36.4, SD = 14.8), and the median level of education was 12 years (Range: 6–25, M = 12.6 years, SD = 2.5). Data were collected with the understanding and written consent of each participant in accordance with the Declaration of Helsinki (version 2008), and with approval from the West Virginia University Institutional Review Board. Participant anonymity was maintained during data collection and analysis.
Measures
Demographics and Gagging Behavior Questionnaire
Participants completed a self-report questionnaire, which assessed their gender, age, and race/ethnicity. In addition, participants were asked questions about gagging behavior using a Gagging Behavior Questionnaire, a measure designed by the authors for the purposes of this study. Items comprising that questionnaire are listed in Appendix A. Participants responded to appropriate items (i.e., items other than those prompting for specific examples of triggers) using a 5-point rating scale that included the following options: “never,” “rarely,” “sometimes,” “frequently,” and “almost always or always.” As described later, a single item from this questionnaire was used to assign participants to one of three gagging severity groups (i.e., “if you have ever had problems with gagging during dental visits, how often has gagging interrupted dental treatment?”); other items were used to assess additional aspects of gagging.
Dental Fear Survey
The Dental Fear Survey (DFS) is a 20-item self-report measure that assesses fear of specific dental-related stimuli.16 The DFS uses a 5-point rating scale ranging from “not at all” to “extreme.” Factor analysis has revealed three categories of dental care-related fear assessed using this instrument: Dental Avoidance and Anticipatory Anxiety (e.g., fear of dental work has caused putting off making an appointment), Fear of Specific Dental Stimuli or Procedures (e.g., feeling the needle injected, being seated in the dental chair), and Physiological Arousal associated with dental treatment (e.g., breathing rate increases, heart beats faster).13 A total score also can be calculated, with possible scores range from 20 – 100; higher scores indicate greater levels of dental care-related fear. The DFS has high internal consistency and test-retest reliability (r = .74), is highly correlated with another validated and widely-used measure of dental care-related fear (r = .92), and has been translated from English into numerous languages.17,18,19
Short-Form Fear of Pain Questionnaire
The Short Form of the Fear of Pain Questionnaire (SF-FPQ) is a 9-item self-report measure that assesses fear of potentially painful experiences across three subscales: Fear of Severe Pain, Minor Pain, and Medical/Dental Pain.20 Utilizing a 5-point rating scale, possible scores range from 3–15 per subscale with total scores ranging from 9–45; higher scores indicate greater levels of fear of pain. Versions of the FPQ have exhibited high internal consistency in the standardization sample, Cronbach’s α = .92, in addition to test-retest reliability, r = .72.20
Getz Dental Beliefs Scale
The Revised Dental Beliefs Scale (DBS) is a 28-item self-report measure that assesses participants’ perceptions of dentistry and dental care professionals.21 The DBS is comprised of three subscales: Professionalism, Communication, and Lack of Control. Items utilize a 5-point rating scale, and total possible scores range from 28–140; higher scores indicate negative views towards dentists and dental care in general. The DBS has high internal consistency (Cronbach’s α = .95) and test-retest reliability (r = .88).22,23
Procedure
Participants were recruited from the waiting area of the Oral Diagnosis Clinic at the West Virginia University School of Dentistry. A majority of these patients presented with a dental emergency (some of them in significant pain and others not), with a subset of patients presenting for new patient screenings. After being approached by a research assistant, volunteering, and providing informed consent, these patients completed the demographics questionnaire, DFS, SF-FPQ, and DBS prior to their dental examination, in that order. Upon completing the questionnaire battery, participants received $5.00 as compensation for their time.
Statistical Analyses
Following assignment of participants to one of three gagging frequency groups, demographic variables across the groups were analyzed by one-way analyses of variance (ANOVA). Multivariate analyses of covariance (MANCOVA) was utilized to address the primary research question and three specific hypotheses, that frequency of gagging during dental procedures is associated with: (1) greater levels of dental care-related fear, (2) more fear of pain, and (3) more negative beliefs about dentistry. Follow-up ANOVAs and Sheffe’s post hoc tests were employed to determine where there were significant between-group differences.
Results
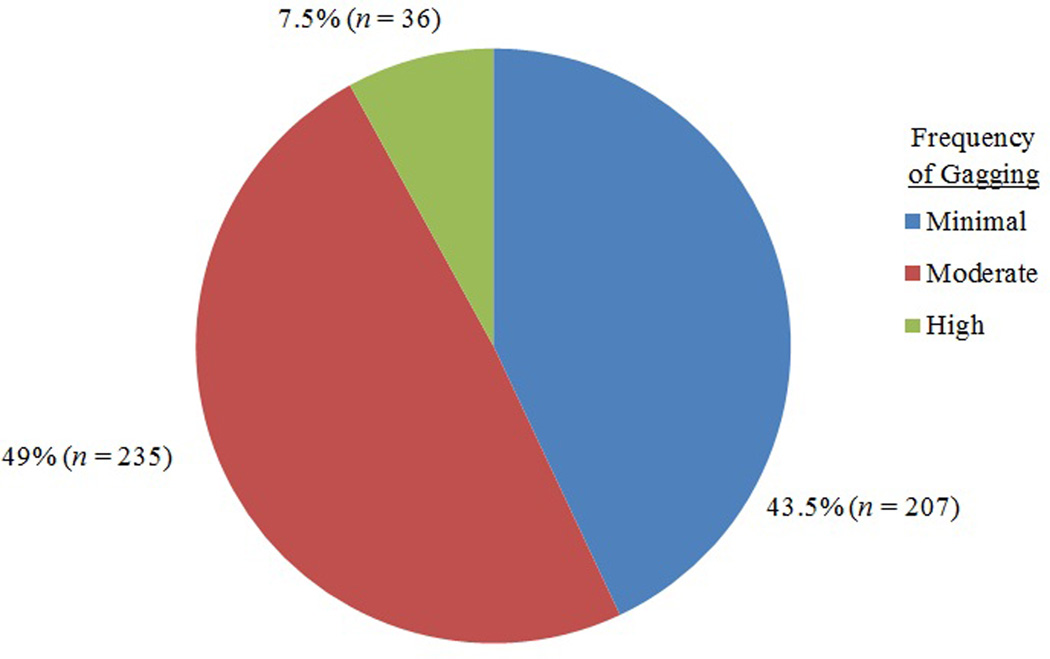
Initially, participants were assigned to one of three groups based on their response to the gagging questionnaire item related to frequency of gagging during dental treatment. Individuals who indicated almost always or always gagging during dental treatment were classified as having a high frequency of gagging in the clinic. Those who indicated sometimes or frequently gagging during dental treatment were classified as having a moderate frequency of gagging in the clinic. Finally, individuals who indicated never or rarely gagging during dental treatment were classified as having a minimal frequency of gagging in the clinic. The distribution of participants among these groups is presented in Figure 1. Notably, and unlike for dental care-related fear, no gender, age, or education differences for prevalence of gagging in the dental clinic were found.
Figure 1.
Percentage of sample with minimal, moderate, and high frequency of gagging.
Note. Total sample size: N = 478.
A MANCOVA then was performed on the three dependent variables: Dental care-related fear (DFS total score), fear of pain (SF-FPQ total score), and negative beliefs about dental treatment (DBS total score). The independent variable was gagging group (i.e., high, moderate, or minimal frequency of gagging). Given their well-established associations with dental care-related fear, gender and age were entered into the analysis as covariates.24 The dependent variables, in combination, were significantly affected by gagging group, Wilk’s λ = .87, F(6, 942) = 11.15, p < .001, η2p = .066.
Follow-up ANOVAs revealed that there were significant differences across the gagging groups in DFS, SF-FPQ, and DBS scores. The results of these tests are presented in Table 1. Scheffe’s post hoc tests revealed that significant differences in DFS and DBS scores exist between participants in all three gagging groups (p < .05 for all between-group comparisons). Patients who have minimal frequency of gagging reported less dental care-related fear and fewer negative beliefs about dentistry than did patients who have moderate or high frequency of gagging. Similarly, patients who have moderate frequency of gagging reported less dental care-related fear and fewer negative beliefs about dentistry than did patients who have high frequency of gagging in the dental clinic. Scheffe’s post hoc tests revealed that significant differences in SF-FPQ scores exist between participants who reported minimal frequency of gagging and those who reported high frequency of gagging (p < .001), and between participants who reported moderate frequency of gagging and participants who reported high frequency of gagging (p = .006). Patients who have minimal or moderate frequency of gagging reported lower levels of fear of pain than did those with a high frequency of gagging in the dental clinic. Patients with minimal frequency of gagging did not have significantly different SF-FPQ scores than those with moderate frequency of gagging (p = .37).
Table 1.
DFS, SF-FPQ, and DBS score means, standard deviations, and ANOVAs by gagging group.
| Frequency of Gagging | ||||
|---|---|---|---|---|
| Minimal | Moderate | High | ||
| DFS Score | 37.4 (17.1)a | 45.9 (18.5)b | 61.3 (22.8)c | F(2, 478) = 28.5, p < .001, η2p = .12 |
| SF-FPQ Score | 21.4 (7.4)a | 22.6 (7.3)a | 27.6 (7.5)b | F(2, 478) = 9.8, p < .001, η2p = .04 |
| DBS Score | 45.1 (18.5)a | 53.0 (21.6)b | 69.4 (28.5)c | F(2, 478) = 21.3, p < .001, η2p = .08 |
Note.Means in each row that do not share a common superscript differ significantly on Sheffe’s post hoc tests at the .05 level. DFS: Dental Fear Survey; SF-FPQ: Short Form Fear of Pain Questionnaire; DBS: Dental Beliefs Scale.
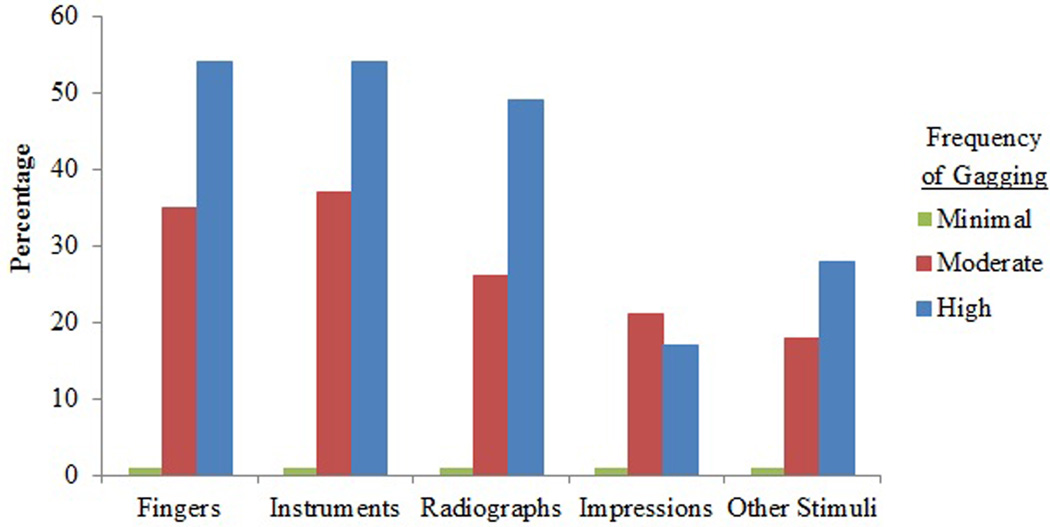
Figure 2 displays the triggers that were reported to induce gagging during previous dental visits, by gagging group. Interestingly, among individuals who indicated any problems with gagging, those who reported gagging during dental treatment resulting from less-intrusive stimuli (i.e., fingers in the mouth) reported greater levels of dental care-related fear, as measured by the DFS (M = 51.3, SD = 20.2) than did individuals who reported gagging from other stimuli, such as instruments or bitewing radiographs (M = 46.2, SD = 18.2; t(290) = 2.23, p < .05). Gagging in the dental clinic was positively associated with gagging in other contexts (r = 0.38, p < .001).
Figure 2.
Percentage of sample reporting gagging stimulated by common triggers, by gagging group.
Discussion
Gagging is a prevalent, intrusive concern in dental care; that there are no observed effects of gender, age, or level of education on problems with gagging suggests it is a generalized across socioeconomic and other demographic strata. It would be helpful, therefore, for dental professionals to monitor whether a patient has problems with gagging, as the experience could be a source of discomfort, and could lead to avoidance of care, especially for fearful patients. The present study demonstrates, as hypothesized, that gagging is associated with dental care-related fear, fear of pain, and negative perceptions of oral healthcare professionals and dental treatment. Other research that has focused exclusively on patients with problem gagging found a high degree of dental fear in such patients as a whole, but not differentiated across gagging severity levels.7
These results highlight an important problem in dental care, but are not able to elucidate the mechanisms involved. It may be that dental care-related fear causes more frequent gagging in the dental clinic, that frequent gagging causes apprehension and leads to the development of dental care-related fear, or, more likely, that a feedback cycle exists wherein fear results in more frequent gagging which reinforces and perpetuates the fear. The type of data collected for the purposes of the present study does not allow such a mechanistic model to be tested. Regardless of the true cause-and-effect relations between the phenomena, an association between fear and gagging likely exists as a result of operant, classical, and other conditioning.
Although reflexive, gagging is modifiable by chairside and other behavioral interventions that can be employed by dentists and the oral healthcare team.1 A number of these treatments may be of particular relevance to dental professionals who routinely utilize bitewing radiographs, impressions, and placement of appliances in their practice, as these procedures are associated with a greater prevalence of problems with gagging. One commonly used strategy for dealing with gagging in the dental clinic is to encourage patients to breathe through the nose before the behavioral response is triggered. Prior to procedures with patients who have problems with gagging, a clinician can teach and practice nose breathing, demonstrating that the technique works by encouraging the patient to put their own fingers or a dental instrument into the mouth during the practice. Reminding and encouraging patients to utilize nose breathing before and during the procedure may be critical. Encouraging pediatric patients with problems with gagging to wiggle their toes during procedures also can be effective; the method provides distraction and may also provide an outlet of physiological arousal that can serve to decrease gagging behavior. Patients who manage their own gagging and who can complete treatment subsequently may experience lower levels of fear during the procedure and may develop more positive beliefs about dentistry.
Not all patients, particularly highly fearful ones, may benefit from a nose breathing strategy to eliminate problematic gagging behavior; extremely high levels of fear may hinder a patient’s ability to attend to the task. Behavior therapies, such as relaxation training, distraction, and systematic desensitization, seek to replace the association, learned through conditioning, of dental contexts and fear with the gagging response via extinction learning.1 Additionally, by identifying and systematically confronting a hierarchy of fears and triggers of gagging, systematic desensitization “shapes” the patient’s response and helps him or her cope with stress, and remain relaxed while experiencing increasingly aversive stimuli.25 There are straightforward ways to desensitize patients who frequently experience gagging, utilizing a similar behavioral approach.9
Alternatively to behavior therapies, various techniques, such as the salt-on-the-tongue, acupuncture, and hypnosis have been used in the treatment of frequent gagging.26,27 Whether these strategies truly are efficacious is unknown; however, one of the mechanisms involved likely is distraction (which itself is a behavioral approach) of the patient, long enough to complete treatment. Such techniques do not eliminate the problem altogether.9 Other distraction methods include having the patient raise his/her legs, counting up or down from 100, and so on. Distraction techniques that include the use of audiovisual equipment have demonstrated success in reducing fear, anxiety, and pain in the dental clinic and may be useful for some, but not all, patients in addressing problems with gagging that are associated with dental care-related fear.28
To be certain, more comprehensive behavioral techniques, which seek to eliminate the association between two stimuli (e.g., dental care and gagging), may be more appropriate for patients who desire longer-lasting reduction of dental care-related fear and associated problems with frequent gagging. A psychologist, other behavioral specialist, or dentist with proper training could treat a problem with frequent gagging using these techniques. Behavioral therapies that target a gagging response are theoretically promising, even though not yet well-studied, and should be further explored in randomized clinical trials to assess their efficacy in reducing the gag response and improving dental treatment-seeking behavior. If gagging is an immediate problem that is delaying or preventing treatment, special care must be provided as a high level of dental care-related fear may be present. Reviews and recent empirical studies have been published on the myriad techniques available to manage gagging problems in dentistry.1,7,29 Future work should address which of these techniques are most effective for reducing problems with gagging and whether certain methods are most appropriate for different severities of gagging.
In assessing gagging, the retrospective design of the present study presents a unique limitation. Participants were asked to recall their experiences with gagging episodes; however, long-term memory becomes increasingly fallible as the time from the event increases.30 As a result, the participants may recall more or less gagging than what actually was experienced. It also may be the case that fearful individuals are more likely to report a greater predisposition to gagging without actually being more likely to gag in the dental setting. Thus, the self-report of gagging provides the patient’s unique vantage point, but the accuracy of the data may be limited. Measures of the severity of the pharyngeal reflex, such as the Classification of Gagging Problem index or the Gagging Problem Assessment, may be good tools to utilize for clinician-rated assessment.7,31 Such approaches also are valuable, in that they rely on observation of overt behavior. Still, the current study’s reliance on patient self-report of the frequency of problematic gagging is a strength – patients’ perception of their problems with gagging are important, as this understanding likely informs and perpetuates their fears and beliefs about dental care.
That study data were collected in a single emergency/screening school of dentistry clinic presents another limitation. Such individuals are not fully representative of the general population, particularly those who receive asymptomatic dental care. Future samples should include multiple dental offices that serve different populations in order to improve the generalizability of the research. Further research also should examine the relation between “overactive” gagging and cognitive vulnerabilities, as cognitions have been shown to affect dental care-related fear.24
Conclusion
Greater dental care-related fear and fear of pain are related to higher frequency of gagging problems during dental treatment across sociodemographic groups, an important finding that has broad implications for dental professionals working across specialty areas. This study is another step in determining critical correlates of and potential treatment targets for gagging, a behavioral response that is more than an “overactive” pharyngeal reflex. Given the prevalence of problematic frequent gagging, future studies should examine the mechanisms of how this barrier to treatment develops and is maintained, considering variables such as dental care-related fear, fear of pain, and negative beliefs about the dentist, as well as cognitive vulnerabilities and previous experiences with dental treatment.
Acknowledgements
The authors thank the West Virginia University School of Dentistry for assisting in data collection, and the patients of the West Virginia University School of Dentistry clinics for their time and participation. Partial support for this project was provided through the West Virginia University School of Dentistry Research Committee. Preparation of this manuscript was supported by the West Virginia University Research Challenge Fund and the National Institute for Dental and Craniofacial Research (2R01 DE014899). Comments and suggestions from anonymous reviewers on an earlier draft of this manuscript are acknowledged with appreciation.
This article is dedicated in memory of Elliot Shulman, DDS, a pediatric dentist, beloved father of the second author, and esteemed colleague of the three other authors.
Appendix A
Gagging Behavior Questionnaire
|
Contributor Information
Cameron L. Randall, Department of Psychology, Eberly College of Arts and Sciences, West Virginia University. He is affiliated with the Center for Oral Health Research in Appalachia.
Grant P. Shulman, Department of Psychology, College of Arts and Sciences, University of Nebraska-Lincoln.
Richard J. Crout, Department of Periodontics, West Virginia University School of Dentistry. He is affiliated with the Center for Oral Health Research in Appalachia.
Daniel W. McNeil, Department of Psychology, Eberly College of Arts and Sciences, West Virginia University, and a Clinical Professor, Department of Dental Practice and Rural Health, West Virginia University School of Dentistry. He is affiliated with the Center for Oral Health Research in Appalachia.
References
- 1.Bassi GS, Humphris GM, Longman LP. The etiology and management of gagging: A review of the literature. Journal of Prosthetic Dentistry. 2004;91(5):459–567. doi: 10.1016/S0022391304000939. [DOI] [PubMed] [Google Scholar]
- 2.Rothenberg MA, Chapman CF. Dictionary of medical terms. 5th ed. Hauppauge, NY: Barron’s Educational Series; 2006. Gag reflex; p. 239. [Google Scholar]
- 3.Eli I. Oral psychophysiology: Stress, pain, and behavior in dental care. Boca Raton, Florida: CRC Press; 1992. pp. 79–87. [Google Scholar]
- 4.Murphy WM. A clinical survey of gagging patients. Journal of Prosthetic Dentistry. 1979;42(2):145–147. doi: 10.1016/0022-3913(79)90163-x. [DOI] [PubMed] [Google Scholar]
- 5.Newton AV. The psychosomatic component in prosthodontics. Journal of Prosthetic Dentistry. 1984;52(6):871–874. doi: 10.1016/s0022-3913(84)80022-0. [DOI] [PubMed] [Google Scholar]
- 6.Ramsay DS, Weinstein P, Milgrom P, Getz Problematic gagging: Principles of treatment. Journal of the American Dental Association. 114:178–183. doi: 10.14219/jada.archive.1987.0023. [DOI] [PubMed] [Google Scholar]
- 7.Saita N, Fukuda K, Koukita Y, Ichinohe T, Yamashita S. Relationship between gagging severity and its management in dentistry. Journal of Oral Rehabilitation. 2013;40(2):106–111. doi: 10.1111/joor.12014. [DOI] [PubMed] [Google Scholar]
- 8.Dionne RA, Gordon SM, McCullagh LM, Phero JC. Assessing the need for anesthesia and sedation in the general population. Journal of the American Dental Association. 1998;129(2):167–173. doi: 10.14219/jada.archive.1998.0173. [DOI] [PubMed] [Google Scholar]
- 9.Armfield J, Stewart JF, Spencer JA. The vicious cycle of dental fear: Exploring the interplay between oral health, service utilization and dental fear. BMC Oral Health. 2007;7:1–15. doi: 10.1186/1472-6831-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McNeil DW, Berryman L. Components of dental fear in adults. Behaviour Research and Therapy. 1989;27:233–236. doi: 10.1016/0005-7967(89)90041-7. [DOI] [PubMed] [Google Scholar]
- 11.Doerr PA, Lang WP, Nyquist LV, Ronis DL. Factors associated with dental anxiety. Journal of the American Dental Association. 1998;129:1111–1119. doi: 10.14219/jada.archive.1998.0386. [DOI] [PubMed] [Google Scholar]
- 12.Milgrom P, Weinstein P, Heaton LJ. Treating fearful dental patients: A patient management handbook. 3rd ed. Seattle, WA: Dental Behavioral Resources; 2009. pp. 246–250. [Google Scholar]
- 13.U.S. Department of Health and Human Services. Rockville, MD: U.S. Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000. Oral health in America: A report of the Surgeon General. [Google Scholar]
- 14.Williams R, Barnett AH, Claffey N, et al. The potential impact of periodontal disease on general health: A consensus view. Current Medical Research and Opinion. 2008;24(6):1635–1643. doi: 10.1185/03007990802131215. [DOI] [PubMed] [Google Scholar]
- 15.Rural Policy Research Institute. West Virginia: 2009. State demographic and economic profiles. http://www.rupri.org/Profiles/WestVirginia2.pdf. [Google Scholar]
- 16.Kleinknecht R, Klepac R, Alexander LD. Origins and characteristics of fear of dentistry. Journal of Dental Research. 1973;86(4):842–848. doi: 10.14219/jada.archive.1973.0165. [DOI] [PubMed] [Google Scholar]
- 17.Kleinknecht R, Thorndike RM, McGlynn FD, Harkavy J. Analysis of the Dental Fear Survey with cross-validation. Journal of the American Dental Association. 1984;108(1):59–61. doi: 10.14219/jada.archive.1984.0193. [DOI] [PubMed] [Google Scholar]
- 18.McGlynn FD, McNeil DW, Gallagher SL, Vrana S. Factor structure, stability, and internal consistency of the Dental Fear Survey. Behavioral Assessment. 1987;9(1):57–66. [Google Scholar]
- 19.Johansson P, Berggren U. Assessment of dental fear: A comparison of two psychometric instruments. Acta Odontologica Scandinavica. 1992;50(1):43–49. doi: 10.3109/00016359209012745. [DOI] [PubMed] [Google Scholar]
- 20.McNeil DW, Rainwater AJ. Development of the Fear of Pain Questionnaire-III. Journal of Behavioral Medicine. 1998;21(4):389–410. doi: 10.1023/a:1018782831217. [DOI] [PubMed] [Google Scholar]
- 21.Smith TA, Weinstein P, Milgrom P, Getz T. An evaluation of an institution-based dental fears clinic. Journal of Dental Research. 1984;63:272. [Google Scholar]
- 22.Kvale G, Milgrom P, Getz T, Weinstein P, Johnsen TB. Beliefs about professional ethics, dentist-patient communication, control and trust among fearful dental patients: The factor structure of the revised dental beliefs survey. Acta Odontologica Scandinavica. 2004;62(1):21–29. doi: 10.1080/00016350310005780. [DOI] [PubMed] [Google Scholar]
- 23.Coolidge T, Heima M, Coldwell S, Weinstein P, Milgrom P. Psychometric properties of the revised dental beliefs survey. Community Dentistry and Oral Epidemiology. 2005;33(4):289–297. doi: 10.1111/j.1600-0528.2005.00214.x. [DOI] [PubMed] [Google Scholar]
- 24.McNeil DW, Randall CL. Dental fear and anxiety associated with oral health care: Conceptual and clinical issues. In: Mostofsky D, Forgione A, Giddon D, editors. Behavioral dentistry. 2nd ed. 2013. Manuscript in press. [Google Scholar]
- 25.Head LS, Gross AM. Systematic desensitization. In: O’Donohue WT, Fisher JE, editors. Cognitive Behavior Therapy. Hoboken, NJ: John Wiley & Sons; 2008. pp. 542–549. [Google Scholar]
- 26.Chidiac JJ, Chamseddine L, Bellos G. Gagging prevention using nitrous oxide or table salt: A comparative pilot study. International Journal of Prosthodontics. 2001;14(4):364–366. [PubMed] [Google Scholar]
- 27.Eitner S, Wichmann M, Holst S. A long-term therapeutic treatment for patients with a severe gag reflex. International Journal of Clinical and Experimental Hypnosis. 2005;53(1):74–86. doi: 10.1080/00207140490914252. [DOI] [PubMed] [Google Scholar]
- 28.Frere CL, Crout R, Yorty J, McNeil DW. Effects of audiovisual distraction during dental prophylaxis. Journal of the American Dental Association. 2001;132:1031–1038. doi: 10.14219/jada.archive.2001.0309. [DOI] [PubMed] [Google Scholar]
- 29.Dickinson CM, Fiske J. A review of gagging problems in dentistry: Clinical assessment and management. SADJ. 2006;61(6):258–262. 266. [PubMed] [Google Scholar]
- 30.Goldstein EB. Cognitive psychology: Connecting mind, research, and everyday experience. 3rd ed. Belmont, CA: Wadsworth; 2011. pp. 542–550. [Google Scholar]
- 31.van Linden van den Heuvell CFEC, ter Pelkwijk BJ, Stegenga B. Development of the gagging problems assessment: A pilot study. Journal of Oral Rehabilitation. 2008;35(3):196–202. doi: 10.1111/j.1365-2842.2007.01774.x. [DOI] [PubMed] [Google Scholar]