Abstract
Mindfulness-based treatments have received increasing interest and empirical support in the clinical psychology literature. There are, however, no studies to date that have systematically examined treatment enactment, which is the amount and type of home practice participants incorporate into their daily lives. Because treatment enactment has been cited as a key aspect of treatment fidelity (Bellg et al., 2004), this study aimed to fill this important research gap by documenting treatment enactment (i.e., home practice) in the context of a larger study of mindfulness-based relapse prevention (MBRP; Bowen et al., 2009). Participants (N = 93) in this secondary analysis had been randomized in the parent study to receive MBRP. Alcohol and other drug (AOD) use, craving, and home practice were assessed at baseline, post-treatment, 2-month and 4-month follow-up time points. Findings indicated that MBRP participants significantly increased the amount of time spent in home practice over the course of the study. Further, greater time spent in home practice was associated with less craving and AOD use at the 2- and 4-month follow-ups. Unfortunately, the significant treatment gains in home practice faded somewhat at the 2- and 4-month follow-ups. These findings suggest that MBRP clinicians should target this post-intervention decline in home practice to maximize the benefits of mindfulness meditation in decreasing AOD use and craving.
Keywords: Substance use, Alcohol and drug use, Mindfulness, Mindfulness-Based Relapse Prevention, Treatment enactment, Substance abuse treatment
1. Introduction
Recent decades have seen an explosion of interest in clinical treatment programs based on mindfulness meditation, particularly those modeled after the Mindfulness-Based Stress Reduction (MBSR) program of Jon Kabat-Zinn and colleagues (Kabat-Zinn, 1990). As taught in these programs, mindfulness refers to the development of a mental state characterized by nonjudgmental awareness of present moment experience. This awareness includes physical sensations, thoughts, emotions, and the environment, and is characterized by an attitude of openness and curiosity. Recent meta-analyses (Hofmann, et al., 2010; Grossman, 2004) found that MBSR was being successfully applied to a broad range of chronic disorders, and there are now hundreds of such programs around the world. Evidence-based adaptations of MBSR include Mindfulness-based cognitive therapy (MBCT) for depression (Teasdale, et al., 2000), MBSR-T for stress reduction for adolescents (Biegel, et al., 2009), and MB-EAT for eating disorders (Kristeller, Baer, & Quillian-Wolever, 2006).
Recently, Bowen and colleagues (2010) developed Mindfulness-Based Relapse Prevention (MBRP) as a manualized, structured aftercare program for individuals who have completed intensive inpatient or outpatient treatment for substance use disorders. MBRP integrates mindfulness practices with cognitive-behavioral Relapse Prevention (Marlatt & Gordon, 1985) therapy and aims to help participants increase awareness and acceptance of difficult thoughts, feelings, and sensations to create changes in patterns of reactive behavior that commonly lead to relapse. Mindfulness training in MBRP provides clients with a new way of processing situational cues and monitoring internal reactions to contingencies, and this awareness supports proactive behavioral choices in the face of high-risk relapse situations (Witkiewitz, Marlatt, & Walker, 2005). In a recent, randomized pilot study of MBRP, Bowen and colleagues (2009) found that MBRP participants experienced fewer and shorter relapses compared to control participants.
1.1. Treatment Enactment
Despite the growing body of research supporting the use of mindfulness techniques in the treatment of various physical and psychological disorders, Ospina and colleagues (2007) noted that research on mindfulness practices and their therapeutic applications is still in an early stage of development. One important aspect of treatment development research in this stage is the evaluation of treatment integrity, also known as treatment fidelity. Studies have shown that strengthening treatment integrity can improve treatment outcomes (e.g., Henggeler, et al., 1997). The establishment and assessment of treatment integrity has been grouped into three broad areas (Bellg et al, 2004): treatment delivery (i.e., whether the treatment was delivered as intended), treatment receipt (i.e., whether the client comprehended and used the treatment skills during the session), and treatment enactment (i.e., whether the client applied skills learned in treatment to his or her daily life).
Despite the relative newness of MBRP in the treatment literature, steps have already been taken to establish its integrity. For example, the treatment has been manualized (Bowen, Chawla, & Marlatt, 2010), and studies have begun to establish protocols in assessing both therapist competence and adherence in delivering MBRP (Chawla, et al., 2010). Thus far, however, the establishment of MBRP treatment integrity has been focused on therapist behavior, not participant behavior. To address this research gap, the present study therefore explores treatment enactment within a recent randomized controlled trial of MBRP.
1.2. Treatment Enactment in MBRP: The Role of Home Practice
Many mindfulness-based programs clearly state the importance of regular home practice of mindfulness meditation. For example, the manual for MBCT (Segal, 2002) recommends 45 minutes of daily home practice in order to obtain its therapeutic benefits. Although this expectation of daily home practice is well-established in the Buddhist meditation traditions on which these programs are based, there is mixed empirical evidence for the effects of home practice in clinical research studies (Carmody & Baer, 2008). Whereas several studies have shown an association between home practice and improved treatment outcomes for MBSR (Carlson, et al., 2001; Gross, 2004; Shapiro et al, 2003; Speca et al, 2000) and MB-EAT (Kristeller & Hallett, 1999), other researchers failed to find these significant associations (Astin, 1997; Davidson, et al., 2003). No research to date has examined the relationship between home practice and treatment outcomes for MBRP.
1.3. Current Study Aims and Hypotheses
The current study builds on previous MBRP research by examining treatment enactment (i.e., time spent in home practice of mindfulness meditation) during and following treatment delivery. A further aim of this study was to examine the association between home practice and key treatment outcomes: AOD use and craving. Since a goal of MBRP is to integrate mindfulness concepts into daily living, treatment enactment is believed to be critical to improved treatment outcomes. Thus, we hypothesized that participating in the MBRP program would lead to a pre- to posttest significant increase in home practice of mindfulness meditation. We also hypothesized that greater home practice would be associated with lower AOD use and craving following the intervention.
2. Methods
2.1. Participants
Participants in this secondary analysis (n = 93; 55.4% of the full 168 participants) were adults with substance-use disorders who were recruited from a community treatment agency to participate in the larger, parent MBRP efficacy trial (Bowen, et al., 2009). Clients at the agency complete 28-day inpatient (60.3%) or 90-day intensive outpatient (39.7%) treatment, and then attend approximately one year of aftercare. Eligible study participants were between the ages of 18 and 70; had completed the inpatient or intensive outpatient phase of treatment in the previous two weeks; demonstrated English fluency; and were medically cleared for participation. Exclusion criteria included presence of psychosis or dementia, imminent suicide risk, or significant withdrawal risk,.
2.2. MBRP Treatment
In the parent study, MBRP was delivered as an aftercare program (i.e., a relapse prevention program delivered after clients had successfully completed either inpatient or intensive outpatient treatment). MBRP comprised eight, weekly, two-hour, closed-group sessions that were delivered in a small group format. There were a total of 12 MBRP groups, ranging from 6–11 participants (average size was 8.1). Therapists facilitating MBRP groups held master’s degrees in psychology or social work and were experienced in delivery of cognitive-behavioral interventions. Therapists participated in intensive training and received weekly supervision throughout the trial. In addition, sessions were coded for therapist adherence and competence (Chawla, et al., 2010). Participants learned, practiced, and discussed relapse prevention and mindfulness meditation techniques. In addition to in-group instruction, participants received standardized meditation CDs and were expected to institute a regular mindfulness practice outside the group. They were also assigned mindfulness exercises for home practice (e.g., body scan, walking meditation, mindfulness of breath).
2.3. Measures
2.3.1. Demographic Questionnaire
This questionnaire assessed basic sociodemographics, such as gender, age, and racial/ethnic background. These data were used to describe the baseline sample.
2.3.2. Substance Use
The Timeline Followback (TLFB; Sobell & Sobell, 1992) assessed daily use of alcohol (using a standard drink conversion chart) and drugs. At baseline, participants were asked to report for the 60 days prior to initial inpatient or outpatient treatment admission. For all other assessments, they reported on the 60 days immediately prior to assessment. The TLFB has demonstrated good reliability and validity with both online and in-person administration (Sobell, Brown, Gloria & Sobell, 1996). Because quantity measures are not equivalent across substances, days of any AOD use were summed and the resulting frequency score was used as one of the primary outcome variables in the current analyses.
2.3.3. Alcohol and Drug Craving
The Penn Alcohol Craving Scale (PACS; Flannery, Volpicelli & Pettinati, 1999) was adapted to include both alcohol and drug craving. The PACS is a 5-item, self-report measure assessing frequency, intensity, and duration of craving, and overall rating of craving for the previous week. It has shown excellent internal consistency and predictive validity for alcohol relapse. Its internal consistency in the current sample was .87. The total PACS score was used as an outcome variable in this study.
2.3.4. Home Mindfulness Practice
Home mindfulness practice was assessed by asking participants to report the type (i.e., formal or informal practices taught in the program), frequency (i.e., times per week), and duration (i.e., minutes per session) of their mindfulness practices outside of MBRP treatment (e.g., “What type of mindfulness do you currently practice? (check all that apply)” [with a list of formal and informal practices from the MBRP course to select from], and for each selected practice, prompts for, “On average, how many times per week do you practice?” and “How long, on average, is each of your sessions? (minutes)”). The mean number of hours spent in mindfulness meditation per week for a given timepoint was calculated from the participants’ raw data and was used as both an outcome and predictor variable in the main analyses.
2.4. Procedure
Procedures for the larger, parent study are detailed in Bowen et al. (2009) and are briefly summarized in this section. Participants (n=168) were recruited near the end of their inpatient or intensive outpatient treatment at the partnering community agency through flyers and referrals from agency or research staff. Interested individuals contacted research staff by telephone, were verbally consented for screening, and completed a 20- to 30-minute telephone eligibility screen. Eligible participants were invited and scheduled for an on-site information session. If they were interested in participation, they provided written, informed consent. Next, they completed the on-site, computerized baseline assessment. All assessments (including those at baseline and follow-up) were computerized and self-administered to maintain maximum privacy and confidentiality. Trained research staff were present at each assessment to assist and answer questions.
Participants were randomly assigned to either 8 weeks of MBRP group therapy or continuation of the agency’s standard aftercare group therapy (SA). Participants randomized to the MBRP group agreed to discontinue SA for the 8 weeks of the MBRP therapy. After completion of the MBRP program, those participants then returned to SA groups. Participants in the SA condition were given the opportunity to attend an MBRP therapy group free of charge upon completion of their final follow-up assessment.
At post-intervention, 2-month and 4-month follow-ups, participants again completed the computerized questionnaires listed in the Measures section. Participants who did not complete their scheduled follow-up assessments were contacted via telephone to document their substance use. All data obtained from participants about their substance use, whether via computer or telephone, were included in the main analyses. Participants who were not available at one time point were still included in the study when reached at another time point. All participants received local merchant gift cards in the amount of $40 for completion of each assessment. All participants were encouraged to continue attending 12-step or other self-help groups as recommended by their counselors at the treatment agency. Study procedures were reviewed and approved by the University of Washington Institutional Review Board.
2.5. Data Analysis Plan
Population-averaged generalized estimating equations (GEE; Zeger & Liang, 1986) were used to longitudinally test the proposed hypotheses. First, we tested whether home practice increased over the course of the study. Thus, the predictors were linear and quadratic time, and the outcome variable was hours of self-reported home practice at baseline, posttest, and 2- and 4-month follow-ups. Second, we tested whether home practice predicted improved outcomes for AOD use and craving. The reduced model included 3 predictor variables: linear and quadratic time and hours of self-reported home practice (varying across the 4 time points - baseline, posttest, 2-and 4-month follow-up). The full model additionally included two interaction variables of time x home practice as predictors: linear time x home practice and quadratic time x home practice. We compared the relative fit of the two models using the Quasi-likelihood Information Criterion (QIC) (Hardin & Hilbe, 2003).
Variables were examined for univariate outliers and deviation from expected distributions. Because AOD use and hours of home practice were positively skewed, overdispersed counts (Neal & Simons, 2007), we specified a negative binomial distribution and a log link. Because craving scores were positively skewed, interval variables that were greater than or equal to zero, we specified a gamma distribution with a log link. Repeated measures on one case served as the sole clustering variable. Because the data were clustered, unbalanced and evinced gaps for some participants, we used an exchangeable correlation structure to ensure model convergence (Hardin & Hilbe, 2003). To enhance model interpretability, exponentiated coefficients were used. Alpha was set to p = .05, and confidence intervals were set to 95%.
3. Results
3.1 Sample description
Participants (N = 93) were predominantly male (64.5%), and reported a mean age of 40.84 (SD = 1.07) years. Regarding racial background, 63.4% described themselves as White, 22.6% as Black/African American, 9.7% as American Indian/Alaska Native, 3.2% as Hawaiian/Pacific Islander, 1.1% as Asian, and 1.1% as “Other.” An additional 6.5% indicated a Hispanic/Latino/a ethnicity. Primary substances of abuse were alcohol (45.2%), cocaine/crack (36.2%), methamphetamines (13.7%), opiates/heroin (7.1%), marijuana (5.4%), and other (1.9%). Approximately 19.1% reported polysubstance use. Approximately 83%, 80%, and 74% of the sample completed post-intervention, 2-month, and 4-month follow-up assessments, respectively.
3.2. Development of Home Practice Over the Course of the Study
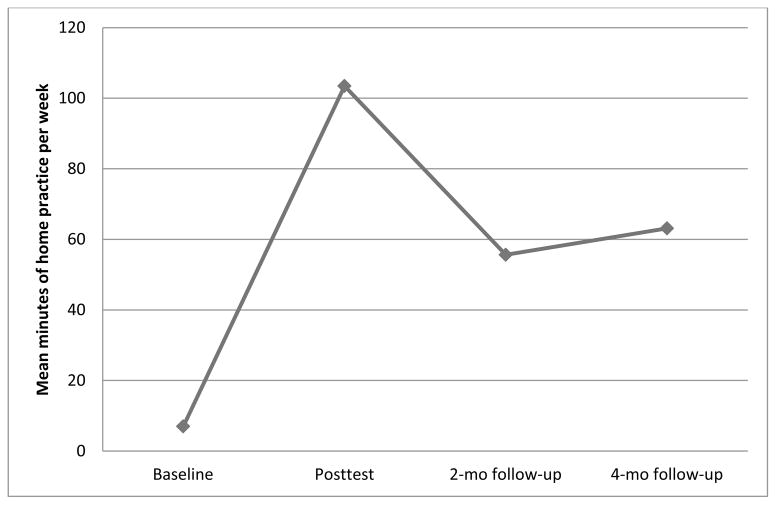
The GEE model for home practice was significant, χ2(2, N = 93) = 58.95, p < .001. As shown in Figure 1, participants engaged in significantly more mindfulness meditation over the course of the study; however the curvilinear relationship indicated these positive treatment effects dropped off at the 2- and 4-month follow-ups. This relationship is reflected in the linear time effects in Table 1, which indicated that between each time point, participants home practice increased by about 11-fold on average. On the other hand, the inverse quadratic time effect reflects the downturn seen in Figure 1 after the treatment course was completed (see Table 1 for model parameters).
Figure 1.
This figure shows the mean minutes of home practice per week reported by participants prior to, during and following MBRP delivery.
Table 1.
Parameter Estimates from the GEE Model of Home Practice (in Hours)
| Variable | IRR | SE | z | p |
|---|---|---|---|---|
| Centered linear time | 10.62 | 3.30 | 7.61 | <.001 |
| Centered quadratic time | .53 | .05 | −6.51 | <.001 |
Notes. IRR = incident rate ratio. SE = Semi-robust standard error. z = z-score for the parameter.
3.3. Associations Between Home Practice and AOD and Craving Outcomes
The first GEE model for AOD outcomes was significant, χ2(3, N = 93) = 64.89, p < .001, QIC = 1419. Similar to the parent study findings (Bowen et al, 2009), AOD frequency significantly decreased over the course of the study; however, these decreases plateaued over time (see parameters in Table 2). After controlling for the time effects, home practice was inversely correlated with AOD use. Thus, averaged over the study, each additional hour of home practice was associated with 53% lower AOD use rates (see Table 2). The second model, which included the time x home practice interactions was significant, χ2(5, N = 93) = 57.25, p < .001, QIC = 1401, and the QIC indicated this model was slightly better-fitting. However, neither interaction was significant (ps > .45), which indicated that increasing home practice over time did not precipitate significant decreases in AOD use above and beyond the main effect.
Table 2.
Parameter Estimates from the GEE Model of Alcohol and Other Drug Outcomes
| Variable | IRR | SE | z | P |
|---|---|---|---|---|
| Reduced Model | ||||
| Centered linear time | .01 | .01 | −3.94 | <.001 |
| Centered quadratic time | 3.83 | 1.40 | 3.68 | <.001 |
| Mindfulness hours | .47 | .13 | −2.82 | .005 |
| Full Model | ||||
| Linear time | .01 | .01 | −3.76 | <.001 |
| Quadratic time | 3.42 | 1.13 | 3.72 | <.001 |
| Mindfulness hours | .30 | .10 | −3.74 | <.001 |
| Linear time x Mindfulness hours | .90 | .68 | −.14 | .89 |
| Quadratic time x Mindfulness hours | .84 | .20 | −.74 | .46 |
Notes. IRR = incident rate ratio. SE = Semi-robust standard error. z = z-score for the parameter.
The first GEE model for craving was significant, χ2(3, N = 92) = 19.20, p < .001, QIC = 1238. Craving significantly decreased over the course of the study (see Table 3 for model parameters). After controlling for the time effects, home practice was inversely correlated with craving. Thus, averaged over the study, home practice was associated with decreased cravings. The second model, which included the time x home practice interactions was also significant, χ2(5, N = 92) = 86.92, p < .001, QIC = 1236, and the QIC indicated this model was slightly better-fitting. Both the linear and quadratic time x home practice interactions were significant, which indicated that increasing home practice over time precipitated significant, longitudinal curvilinear decreases in craving (see Table 3 for log-rate effect sizes).
Table 3.
Parameter Estimates from the GEE Model of Craving Outcomes
| Variable | Exp(b) | SE | z | P |
|---|---|---|---|---|
| Reduced Model | ||||
| Centered linear time | .77 | .09 | −2.16 | .03 |
| Centered quadratic time | 1.06 | .04 | 1.60 | .11 |
| Mindfulness hours | .92 | .03 | −2.36 | .02 |
| Full Model | ||||
| Linear time | .62 | .08 | −3.90 | <.001 |
| Quadratic time | 1.12 | .04 | 2.93 | .003 |
| Mindfulness hours | .97 | .04 | −.90 | .37 |
| Linear time x Mindfulness hours | .63 | .05 | −5.49 | <.001 |
| Quadratic time x Mindfulness hours | 1.10 | .02 | 4.46 | <.001 |
Notes. Exp(b) = exponentiated coefficient. SE = Semi-robust standard error. z = z-score for the parameter.
4. Discussion
4.1. Summary of Current Findings
The aims of this study were to assess the development of mindfulness meditation home practice during and subsequent to participation in MBRP and to examine the relationships between home practice and AOD use and craving. The current findings supported our hypotheses: participation in MBRP was associated with a significant increase in home practice, and increased involvement in home practice was associated with significantly lower AOD use and craving over the course of the study. This study’s findings, therefore, indicated that enactment, which entails building mindfulness practice into one’s daily life, plays a key role in ongoing recovery following MBRP treatment. The importance of home practice in the context of mindfulness-based treatments is fairly unique; not all treatments emphasize the importance of ongoing, daily “enactment” of key treatment components. The focus on teaching mindfulness skills for daily use versus only in high-risk situations has the potential to boost the longevity of MBRP treatment effects.
On the other hand, we found that home practice was not consistently maintained after the MBRP treatment ended. Similarly, the parent study showed that positive MBRP treatment effects plateaued at the 4-month follow-up (Bowen et al., 2009). These parallel findings may be related and may reflect the fact that most clients returned to standard aftercare, which did not involve mindfulness-based practice, after they completed the MBRP program. Considering this study’s findings of a significant association between home practice and decreased AOD use and craving, booster sessions may be clinically indicated to support participants’ fledgling practice and thereby extend the positive MBRP treatment effects. It may also be advisable to locate and recommend local mindfulness-meditation groups to provide people with a sense of community around their practice. Future studies are necessary to test the potential efficacy of these approaches in extending the positive effects of MBRP and home practice beyond the treatment setting.
4.2. Study Limitations
The current study has several limitations that deserve mention. First, the follow-up periods were relatively brief and may thereby not have captured either delayed or longer-term effects of home practice. Second, although research indicates up to two-thirds of individuals relapse within the first 3 months following treatment (Pickens, Hatsukami, Spicer & Svikis, 1985), rates of substance use remained low throughout the study, which limited variability in the AOD use data. Third, attrition in the current study may have led to self-selection bias. Future studies are needed to confirm these initial findings. Fourth, this study did not assess attendance at self-help groups, which may be a factor in level of substance use; any differences that remained after randomization could not be accounted for in the analyses. Despite these limitations, the current study established that MBRP is enacted during and following the treatment course and that enactment as measured by home practice is associated with positive treatment outcomes. Larger and particularly longer-term studies are necessary to judge whether these promising findings are replicable and generalizable (Baer, 2007).
4.3. Conclusions
The study findings showed that greater levels of home practice during and subsequent to MBRP treatment were associated with more favorable AOD treatment outcomes. These findings provide support for the utility of home practice in supporting behavior change in the context of mindfulness-based treatment. Although many mindfulness-based treatment programs emphasize regular home practice, empirical support has been mixed. This study replicates the findings of Carmody and Baer (2008), who found support for home practice in a clinical trial, and it extends the literature as the first study on the relationship between home practice and MBRP treatment outcomes. Additional studies are needed to determine the optimal amount of home practice needed to sustain therapeutic effects as well as ways to sustain home practice after treatment ends. Such research will fine-tune the development of these programs to ensure that clients obtain optimal benefits from mindfulness-based interventions.
Table 4.
Means (Standard Deviations) for Alcohol and Other Drug Use and Process Variable During the Study
| Variable | Baseline (n = 93) | Post-intervention (n = 77) | 2 months post-intervention (n = 74) | 4 months post-intervention (n = 69) |
|---|---|---|---|---|
| AOD Days | 27.0 (24.0) | .1 (.3) | 2.1 (7.2) | 5.1 (14.9) |
| PACS (craving) | 1.6 (1.1) | 1.1 (1.1) | 1.0 (1.0) | 1.1 (1.3) |
Acknowledgments
Role of Funding
The parent RCT was funded by National Institute on Drug Abuse Grant R21 DA010562. The National Institute on Drug Abuse had no role in the study design, data collection, data analysis, or manuscript writing.
We wish to pay a special tribute to our mentor, Dr. Alan Marlatt, who passed away before the publication of this manuscript. Additionally, we thank the other researchers at the Addictive Behaviors Research Center who work diligently to further the research of mindfulness-based treatments.
This research was supported by National Institute of Drug Abuse grant R21 DA010562.
Footnotes
Contributors
Grow designed the study and conducted literature searches. Collins and Grow performed the statistical analyses, wrote the protocol, and drafted the manuscript. Harrop drafted sections of the manuscript and assisted in revision. Marlatt provided guidance with study protocol and assisted in revision of the document. All authors contributed to the final manuscript. Grow, Collins, and Harrop have approved the final manuscript; Marlatt approved the first draft of this manuscript prior to his passing in March 2011.
Conflict of Interest
There are no conflicts of interest declared by any author.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Joel C. Grow, Email: joelg@uw.edu.
Susan E. Collins, Email: collinss@uw.edu.
Erin N. Harrop, Email: erind2@u.washington.edu.
References
- Astin J. Stress reduction through mindfulness meditation: Effects on psychological symptomatology, sense of control, and spiritual experiences. Psychotherapy and Psychosomatics. 1997;66:97–106. doi: 10.1159/000289116. [DOI] [PubMed] [Google Scholar]
- Baer R. Mindfulness, assessment, and transdiagnostic processes. Psychological Inquiry. 2007;18(4):238–242. [Google Scholar]
- Bellg AJ, Borrelli B, Resnick B, Hecht J, Minicucci D, Ory M, Czajkowski S. Enhancing Treatment Fidelity in Health Behavior Change Studies: Best Practices and Recommendations. Health Psychology. 2004;23(5):443–451. doi: 10.1037/0278-6133.23.5.443. [DOI] [PubMed] [Google Scholar]
- Biegel GM, Brown K, Shapiro S, Schubert C. Mindfulness-based stress reduction for the treatment of adolescent psychiatric outpatients: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2009;77(5):855–866. doi: 10.1037/a0016241. [DOI] [PubMed] [Google Scholar]
- Bowen S, Chawla N, Collins S, Witkiewitz K, Hsu S, Grow J, Marlatt A. Mindfulness-based relapse prevention for substance-use disorders: A pilot efficacy trial. Substance Abuse. 2009;30(4):295–305. doi: 10.1080/08897070903250084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Chawla N, Marlatt GA. Mindfulness-Based Relapse Prevention for Addictive Behaviors: A Clinician’s Guide. Guilford Press; 2010. [Google Scholar]
- Carlson L, Ursuliak Z, Goodey E, Angen M, Speca M. The effects of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients: 6-month follow-up. Supportive Care in Cancer. 2001;9:112–123. doi: 10.1007/s005200000206. [DOI] [PubMed] [Google Scholar]
- Carmody J, Baer R. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. Journal of Behavioral Medicine. 2008;31:23–33. doi: 10.1007/s10865-007-9130-7. [DOI] [PubMed] [Google Scholar]
- Chawla N, Collins S, Hsu S, Grow J, Douglass A, Marlatt GA. The mindfulness-based relapse prevention adherence and competence scale: Scale development, inter-rater reliability and validity. Psychotherapy Research. 2010;4:1–10. doi: 10.1080/10503300903544257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson RJ. Alterations in brain and immune function produced by mindfulness meditation. Psychosomatic Medicine. 2003;65:564–570. doi: 10.1097/01.psy.0000077505.67574.e3. [DOI] [PubMed] [Google Scholar]
- Flannery BA, Volpicelli JR, Pettinati HM. Psychometric properties of the Penn Alcohol Craving Scale. Alcoholism: Clinical and Experimental Research. 1999;23(8):1289–1295. [PubMed] [Google Scholar]
- Gross CR. Mindfulness meditation to reduce symptoms after organ transplant: A pilot study. Advances in Mind-Body Medicine. 2004;20(2):20–29. [PubMed] [Google Scholar]
- Grossman P. Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of Psychosomatic Research. 2004;57:35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- Hardin JW, Hilbe JM. Generalized estimating equations. Boca Raton, FL: Chapman & Hall/CRC; 2003. [Google Scholar]
- Henggeler SW, Melton GB, Brondino MJ, Scherer DG, Hanley JH. Multisystemic therapy with violent and chronic juvenile offenders and their families: The role of treatment fidelity in successful dissemination. Journal of Consulting and Clinical Psychology. 1997;65:821–833. doi: 10.1037//0022-006x.65.5.821. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full Catastrophe Living. New York, NY: Delacorte; 1990. [Google Scholar]
- Kristeller JL, Baer RA, Quillian-Wolever Ruth. Mindfulness-Based Approaches to Eating Disorders. In: Baer Ruth A., editor. Mindfulness-based treatment approaches: Clinician’s guide to evidence base and applications. San Diego, CA, US: Elsevier Academic Press; 2006. [Google Scholar]
- Kristeller JL, Hallett CB. An exploratory study of a meditation-based intervention for binge eating disorder. Journal of Health Psychology. 1999;4:357–363. doi: 10.1177/135910539900400305. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, Gordon JR. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. New York: Guilford Press; 1985. [Google Scholar]
- Neal D, Simons J. Inference in regression models of heavily skewed alcohol use data. Psychology of Addictive Behaviors. 2007;21(4):441–452. doi: 10.1037/0893-164X.21.4.441. [DOI] [PubMed] [Google Scholar]
- Ospina MB, Bond TK, Karkhaneh M, Tjosvold L, Vandermeer B, Liang Y, Klassen TP. Meditation practices for health: State of the research. Agency for Healthcare Research and Quality Publication; 2007. (No. 07-E010) [PMC free article] [PubMed] [Google Scholar]
- Pickens R, Hatsukami D, Spicer J, Svikis D. Relapse by alcohol abusers. Alcoholism: Clinical and Experimental Research. 1985;9:244–247. doi: 10.1111/j.1530-0277.1985.tb05744.x. [DOI] [PubMed] [Google Scholar]
- Ramel W, Goldin PR, Carmona PE, McQuaid JR. The Effects of mindfulness meditation on cognitive processes and affect in patients with past depression. Cognitive Therapy & Research. 2004;28:433–455. [Google Scholar]
- Segal Z, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. New York: Guilford; 2002. [Google Scholar]
- Shapiro SL, Bootzin R, Figueredo A, Lopez A, Schwartz G. The efficacy of mindfulness-based stress reduction in the treatment of sleep disturbance in women with breast cancer: An exploratory study. Journal of Psychosomatic Research. 2003;54(1):85–91. doi: 10.1016/s0022-3999(02)00546-9. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. A technique for assessing self-reported alcohol consumption. In: Litten, Allen, editors. Measuring Alcohol Consumption: Psychosocial and Biological Methods. New Jersey: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Sobell LC, Brown JL, Gloria I, Sobell MB. The reliability of the Alcohol Timeline Followback when administered by telephone and by computer. Drug Alcohol Depend. 1996;42(1):49–54. doi: 10.1016/0376-8716(96)01263-x. [DOI] [PubMed] [Google Scholar]
- Speca M, Carlson LE, Goodey E, Angen M. A randomized, wait-list controlled clinical trial: The effect of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Psychosomatic Medicine. 2000;62(5):613–622. doi: 10.1097/00006842-200009000-00004. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA, Walker D. Mindfulness-based relapse prevention for alcohol and substance use disorders. Journal of Cognitive Psychotherapy. 2005;19(3):211–228. [Google Scholar]
- Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. [PubMed] [Google Scholar]