Abstract
Depression presents a serious condition for the individual and a major challenge to health care and society. Internet-based cognitive behavior therapy (ICBT) is a treatment option supported in several trials, but there is as yet a lack of effective studies of ICBT in “real world” primary care settings. We examined whether ICBT differed from treatment-as-usual (TAU) in reducing depressive symptoms after 3 months. TAU comprised of visits to general practitioner, registered nurse, antidepressant drugs, waiting list for, or psychotherapy, or combinations of these alternatives. Patients, aged ≥ 18 years, who tentatively met criteria for mild to moderate depression at 16 primary care centers in the south-western region of Sweden were recruited and then assessed in a diagnostic interview. A total of 90 patients were randomized to either TAU or ICBT. The ICBT treatment included interactive elements online, a workbook, a CD with mindfulness and acceptance exercises, and minimal therapist contact. The treatment period lasted for 12 weeks after which both groups were assessed. The main outcome measure was Beck Depression Inventory-II (BDI-II). Additional measures were Montgomery Åsberg Depression Rating Scale – self rating version (MADRS-S) and Beck Anxiety Inventory (BAI). The analyses revealed no significant difference between the two groups at post treatment, neither on BDI-II, MADRS-S, nor BAI. Twenty patients (56%) in the ICBT treatment completed all seven modules. Our findings suggest that ICBT may be successfully delivered in primary care and that the effectiveness, after 3 months, is at par with TAU.
Keywords: depression, Internet-based treatment, ICBT, primary care, effectiveness, randomized controlled trial
Introduction
Depression presents a major challenge for society worldwide. In 2030, it is estimated that depression will contribute the highest disease burden in high-income countries (Mathers & Loncar, 2006). According to the Swedish Council on Health Technology Assessment (SBU), about every fifth person in Sweden will experience at least one severe depression episode during their lifetime (SBU, 2004). In a survey distributed to randomly selected adults in Sweden, 17.2% were experiencing clinically significant depression (Johansson, Carlbring, Heedman, Paxling, & Andersson, 2013) and the prevalence of depression among Swedish primary care patients has been estimated to about 4% (Bodlund, Andersson, & Mallon, 1999) which seems to reflect the fact that many suffering from depression are hesitant to seek help (Priest, Vize, Roberts, Roberts, & Tylee, 1996).
Several treatment options for the disorder are available, mostly by antidepressant medication and less frequently by psychotherapy. The national guidelines of depression treatment issued by the Swedish National Board of Health and Welfare (2010) suggests psychotherapy and in particular cognitive behavioral therapy (CBT) as the prioritized treatment for mild to moderate states of depression in adults. At the same time, according to a Swedish national survey conducted by the National Board of Health and Welfare, the availability of evidence-based psychotherapy and CBT in primary care is low (Swedish National Board of Health and Welfare, 2013), often due to shortage of therapists resulting in limited access and unacceptably long waiting times.
Internet-based CBT (ICBT) for depression has been evaluated in several studies and ICBT typically has at least as good an effect as more traditional psychological treatments (Andersson, Hesser, Hummerdal, Bergman-Nordgren, & Carlbring, 2013; Andersson et al., 2013). Nevertheless, so far, few studies have been conducted within primary care. Most studies are also based on volunteers recruited via advertising. (Andersson & Cuijpers, 2009; Cuijpers, Donker, van Straten, Li, & Andersson, 2010; Richards & Richardson, 2012). Internet-based treatments provide a way of circumventing the therapist shortage (Johansson & Andersson, 2012), and the Swedish National Board of Health and Welfare (2010) also suggests ICBT as the treatment of first choice concerning mild depression in adults.
Research performed within the regular medical services on effectiveness, is likely to differ from efficacy studies performed under more controlled conditions. This situation renders it difficult to translate efficacy into effectiveness in real life settings (Roy-Byrne et al., 2003). Studies of ICBT delivered at primary care centers versus treatment-as-usual (TAU) have largely been absent. The expectation that ICBT may prove effective for depression in primary care also has been increased however by efficacy studies suggesting that the effect of ICBT could be comparable to “face-to-face” therapy (Cuijpers et al., 2010). In a British primary care trial (Proudfoot et al., 2003, 2004), effectiveness was examined comparing computer delivered CBT (where the computers and treatment are stationary at the primary care centers) for depression and/or anxiety with TAU. They found significantly greater improvement in patients receiving the computerized treatment and also greater patient satisfaction with this type of treatment.
The general aim of the PRIM-NET study – implementation of ICBT in Swedish primary care – was to examine (1). whether or not ICBT could be delivered as routine treatment option for mild to moderate depression at primary care centers and if so, (2). whether the effect of ICBT, including minimal therapist contact, differed from TAU. Our expectation was that ICBT would perform better than TAU.
In this first study, we report results on depressive symptomatology measured at inclusion and at 12 weeks following the active treatment period. Using a randomized controlled design (RCT) and a protocol adapted to meet the actual conditions and requirements in the primary care system, we investigated depression outcomes measured at baseline and at post-treatment, 12 weeks from baseline.
Methods
Recruitment and treatments
Patients, aged ≥ 18 years, affected by mild to moderate depression, were recruited by general practitioners (GPs) and nurses at 16 participating Primary Care Centers in the southwestern region of Sweden (Västra Götaland). The GPs and nurses were instructed to invite all patients they met and suspected for mild to moderate depression. Patients received oral information about the study from the primary care center staff and were next asked to consider meeting a licensed psychologist or licensed psychotherapist for an approximately one hour assessment before acceptance of participation in the study. Patients, who agreed to participate, received an appointment for a structured interview within 2 weeks. Participants found to meet inclusion criteria in the psychologist/psychotherapist interview were then assigned to a contact with a registered nurse (RN) to fill out study protocols, including background data.
Eligible patients were randomized to either ICBT or TAU by an independent research unit at the University of Gothenburg. The randomization procedure occurred consecutively for all patients across primary care centers which made it impossible, at a specific primary care center, to predict the allocation of patients. All patients were introduced to and required to use a secure e-mail service (Mina Vårdkontakter) developed and used nationwide in Sweden for the purpose of secure contact between the health care provider and the patient.
Patients randomized to ICBT also received a personal login code, a printed workbook, and printed guidance on how to access the treatment from the RN.
Patients randomized to TAU received the treatment typically provided at the participating primary care center. The PRIM-NET project did not constrain the treatments offered to TAU patients except that they were not allowed participation in any Internet-based treatment during the study period. TAU therefore could consist of a diverse mix of antidepressants, scheduled contacts with personnel at the primary care center such as GPs or nurses, referral to regular psychotherapy (often preceded by a non-negligible waiting period), or combinations of these options depending on routines and available resources at each primary care center.
Depression inventories were administered via the secure e-mail system at Weeks 3 and 7 to both ICBT and TAU patients. Previous research has reported minor differences in scores for inventories answered on a paper format and via computer (Gwaltney, Shields, & Shiffman, 2008). The patients also met the RN for post-treatment measures 12 weeks after inclusion.
The regional medical ethics review board in Gothenburg, Sweden, approved the protocol. Written informed consent was obtained from all participants.
Interview procedure, assessment, inclusion criteria, and demographics
The assessment of prospective patients was performed by a licensed psychologist or licensed psychotherapist and was based on the Mini International Neuropsychiatric Interview Swedish version 6.0.0b (MINI) developed to determine the presence of Axis-I disorders using DSM-IV diagnostic criteria (Sheehan et al., 1998). Psychometric evaluations of the MINI indicate an excellent inter-rater reliability (k = 0.88–1.00; Lecrubier et al., 1997). The interview protocols were, after the patients had completed the study, reviewed by the project management to determine the validity of the initial assessment and diagnosis. The results of the randomization and the outcome after treatment were not known to the reviewers at this time.
Mild to moderate depression was diagnosed according to DSM-IV criteria and a Montgomery Åsberg Depression Rating Scale – self rating version (MADRS-S; Montgomery & Asberg, 1979) score less than 35, which is the cut off point for severe depression.
To be included in the study, patients had to meet the following criteria: (a) aged 18 or older, (b) access to a computer with speakers or headphones, (c) diagnosed with depression according to the MINI, and (d) a MADRS-S score < 35. If the patient was on antidepressant medication, the dosage had to be constant for the 4 weeks prior to inclusion. The exclusion criteria were (e) any prior suicide attempt (no boundary of time) or (f) currently found to be at a medium to high risk of suicide (operationalized by PRIM-NET as MADRS-S, Question 9>3 points and/or MINI Part B – Suicide>9), or were diagnosed according to the MINI with (g) substance dependence, (h) alcohol abuse, (i) bipolar disorder (manic and hypomanic episode), (j) psychotic disorders, or (k) any other severe psychiatric disorder, or during the interview demonstrated (l) cognitive disability or (m) insufficient knowledge of the Swedish language. Diagnosed anxiety disorders were allowed if deemed to be secondary to depression.
Outcome measures
The primary outcome measure of depression was the Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 2006) administered at inclusion and post-treatment. A secondary outcome measure was the MADRS-S administered at inclusion, Weeks 3 and 7, and at post-treatment. MADRS-S was developed to be sensitive to changes in the degree of depression and was used to identify cases with worsened depression or elevated risk of suicide during treatment. The Beck Anxiety Inventory (BAI; Beck, Epstein, Brown, & Steer, 1988) for comorbid anxiety was used at inclusion and post-treatment. All inventories were administered in paper format, except the MADRS-S at Weeks 3 and 7 which for practical reasons had to be administered via the secure e-mail system.
Carlbring et al. (2007) identified significant effects between Internet- and paper administration of BDI-II and BAI. However, no significant version-, order- or interaction effects were found for MADRS-S.
Therapists
There were 12 therapists involved in the study, all licensed psychologists or licensed psychotherapists with qualified knowledge and previous experience of CBT treatment of depression. They were introduced to the aim, design, procedures, documents, and protocols of the project and continuously supervised by authors MK and ME.
The therapists performed the initial assessment of patients. Nine of them were also engaged in the support of patients they had assessed and who were randomized to the ICBT condition, i.e., all ICBT patients were supported by the therapist they had met during the initial assessment interview, with the exception of when their therapist was on vacation, etc.
Treatment conditions in ICBT
The ICBT treatment material used was a commercially available program in Swedish called Depressionshjälpen®. The program is based on CBT techniques, more specifically Behavioral activation (Martell, Dimidjian, & Herman-Dunn, 2010) with components from Acceptance and Commitment Therapy and Mindfulness. The material consists of Internet access to seven modules, each encompassing 8–10 slides of short texts, narrated explanatory models, and/or videos. The workbook consisted of fill-in diaries and exercises to be used in conjunction with the Internet modules. In the workbook, a CD with mindfulness and acceptance instructions were included (for further details see Carlbring et al., 2013, Table 2). Patients could access the Internet modules freely, but were advised to finish them in the predetermined order at a rate of about one module per week, which meant that a recommended treatment was finished in 8 weeks. They were also informed that access to the Internet modules was restricted to a maximum 12 weeks when the login code expired. The treatment period in PRIM-NET was thus defined as 12 weeks. Previous research has found indications that a strict deadline increases adherence (Andersson, Carlbring, Berger, Almlov, & Cuijpers, 2009). As previous research also has shown that the support of a therapist has a positive influence on outcome and drop-out rates compared to pure self-help treatment (Christensen, Griffiths, & Farrer, 2009; Richards & Richardson, 2012), minimal therapist contact was included. Patients were encouraged to have weekly contact via secure e-mail with their therapist. The patients also received three short telephone calls from the therapist, week 1, in the middle, and at the end of the treatment. Further contact via telephone or e-mail was provided if needed. The therapists were instructed to spend about 15 minutes by secure e-mail and/or telephone with each patient per week. The therapist could monitor the time and duration of each login to the Internet modules by each patient. Therapists were instructed to focus the feedback on validating the patient, reinforcing progress, and encouraging the patient to continue working with the program. Using the terms of Johnston, Titov, Andrews, Spence, and Dear (2011) all therapists were assumed to take the role of Coach.
Table 2 . Improvement of scores (ANCOVA) complete case analysis.
| TAU |
ICBT |
||||||
|---|---|---|---|---|---|---|---|
| M | SD | 95% CI | M | SD | 95% CI | Statistical significance | |
| BDI-II pre-post n = 65 | − 11.63 | 9.88 | − 8.24, − 15.02 | − 12.27 | 10.94 | − 8.18, − 16.35 | F(1,62) = .02, NS |
| MADRS-S week 0–3 n = 66 | − 2.12 | 5.56 | − 0.18, − 4.06 | − 0.91 | 6.12 | 1.30, − 3.11 | F(l,63) = .84, NS |
| MADRS-S week 0–7 n = 58 | − 6.24 | 8.16 | − 3.14, − 9.35 | − 4.31 | 7.96 | − 1.28, − 7.34 | F(1,55) = .85, NS |
| MADRS-S pre-post n = 65 | − 8.46 | 7.64 | − 5.83, − 11.08 | − 7.67 | 9.79 | − 4.01, − 11.32 | F(1,62) = .16, NS |
| BAI pre-post*n = 65 | − 6.71 | 9.03 | − 3.61, − 9.82 | − 5.93 | 9.17 | − 2.51, − 9.36 | F(l,62) = .22, NS |
Notes. Negative values indicate improvement. Covariat pre-treatment scores for the same scale except for *BAI where covariat is pre-treatment scores for BDI-II.
Power
In the planning of the PRIM-NET study and calculation of appropriate sample size, we assumed that to detect a significant improvement in the summation of scores employed in the completed instruments by approximately 10% in the ICBT group and almost no reclaim in the TAU group, we needed 71 patients in each group or study arm. The significance level was set at .05 and the beta error as .20 (power of the study; 1 − .20 = .80). The chosen effect size was estimated based on a rather similar study (Proudfoot et al., 2004) and the study group's empirical expectation from the study field.
Statistical analyses
To control for the randomization, we first analyzed baseline between-group differences in demographics and pre-treatment measures with independent t-tests and χ2 tests.
The assumption of “missingness” at random in clinical trials is typically unlikely and inferences about treatment effects are in principle valid only for those who actually accept or adhere to treatment. These considerations made us restrict the analyses to complete cases rather than employing available imputation methods.
Between-group changes in questionnaire scores were analyzed using univariate ANCOVAs, assigning pre-treatment depression scores as the covariate, which is recommended as the preferred method for analyzing the results of treatment trials (Vickers, 2005a, 2005b).
Within-group changes in questionnaires were analyzed using paired samples t-tests. Effect sizes (Cohen's d) were calculated for between- and within-group changes.
We also identified the proportion of patients that after the treatment reached a score of 13 or below on the BDI-II, which according to norms is the cut-off for defining recovery from depression (Beck et al., 2006). The difference in recovery rate between groups was evaluated by the χ2 test.
Results
Baseline comparisons
The post study assessment of interview protocols identified two patients who had, due to human error, been incorrectly included. They were consequently removed from the analyses (1 in ICBT and 1 in TAU).
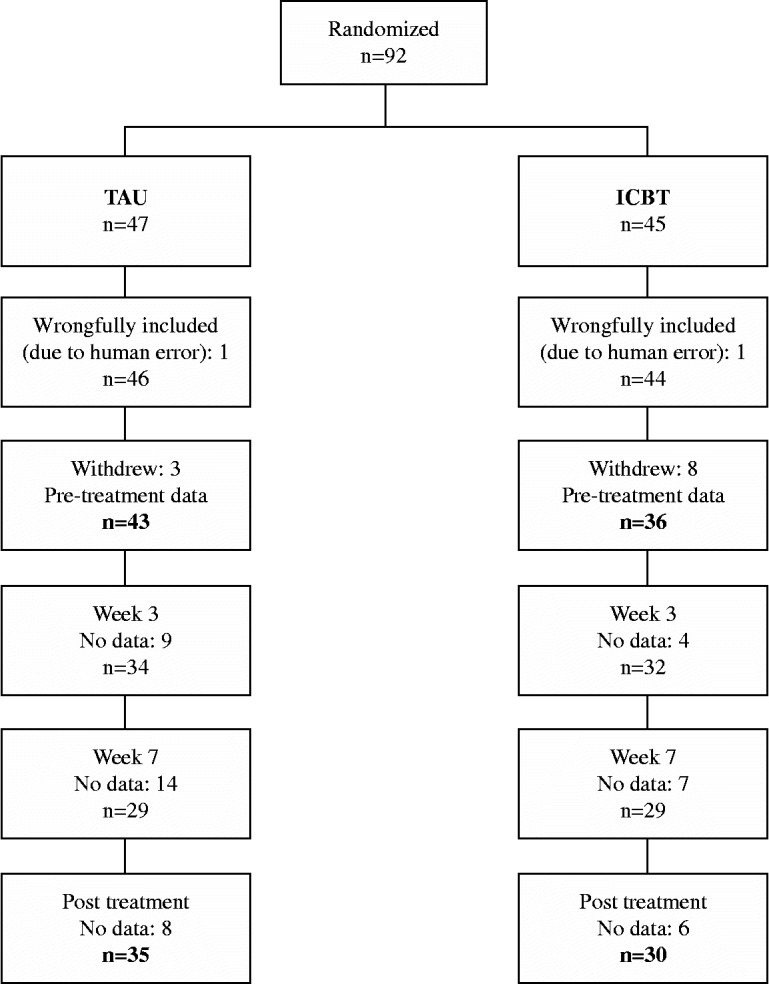
Of the remaining 90 patients, 11 later withdrew from their participation. Sixty-five of the 79 patients (82%) completed the post-treatment forms: 30 (83%) in the ICBT and 35 (81%), in the TAU condition (see Figure 1).
Figure 1 . Flowchart of study patients in each step of the study and analysis.
The mean age of participants was 36.6 years (SD = 11.3) and 52 (66%) were women. At inclusion, 5 (6%) patients suffered from minimal, 15 (19%) from mild, 27 (34%) from moderate, and 32 (41%) from severe depression according to BDI-II cut-off scores. A comparison of baseline scores revealed no significant difference between treatment groups and the randomization as expected produced a similar distribution across conditions (see Table 1). χ2 tests failed to reveal any significant between-group differences in demographic characteristics.
Table 1 . Pre-treatment scores (t-test). Means (M) and standard deviation (SD) at pre-treatment.
| TAU |
ICBT |
||||||
|---|---|---|---|---|---|---|---|
| M | SD | Range | M | SD | Range | Statistical significance | |
| BDI-II | 26.09 | 9.39 | 8–43 | 25.50 | 7.87 | 11–45 | t(77) = − .30, ns |
| MADRS-S | 20.21 | 7.23 | 2–33 | 20.25 | 6.03 | 6–31 | t(77) = − .03, ns |
| BAI | 16.19 | 10.47 | 1–43 | 17.08 | 10.94 | 0–53 | t(77) = − .38, ns |
Comparisons between groups during the treatment period
A total of 22 patients, 11 in each group, were on pharmacological therapy when they were included in the study. At post-treatment, 18 in the TAU group and 8 in the ICBT group were on pharmacological therapy. Eight (19%) of the TAU patients received face-to-face treatment by a psychologist/psychotherapist during the study period; ergo, most patients in TAU (81%) did not receive psychological treatment.
Adherence to ICBT
Twenty (56%) of the ICBT participants completed the seven modules within the 12-week treatment period. The average number of completed modules was 5.1 (range 0–7, SD = 2.6, median = 7). The login time ranged from 0 to 868 minutes with a mean time of 249 minutes (median 188 minutes).
Post-treatment outcomes
Using univariate ANCOVAs controlling for pre-treatment scores, no significant differences were found between the reduction in scores for the ICBT and TAU groups, on MADRS-S scores during treatment, or on post-treatment BDI-II, MADRS-S and BAI scores (Table 2).
On the primary outcome measure (BDI-II), the mean between group effect size at post was d = 0 with within-group effect size for the ICBT group d = 1.09 (pre vs. post) and for the TAU group d = 1.27 (pre vs. post). There was no difference between treatment groups concerning the proportion of recovered patients, with a score of ≤ 13, on the BDI-II at post-treatment. In the TAU group, this was the case for 35% (15 out of 43) and in ICBT for 42% (15 out of 36), (χ2 (1), = .38, ns).
For the ICBT patients, the correlation of the reduction of depressive symptoms, measured by reduction of BDI-II, to the number of accessed modules was r = − .328, p = .072 (ns).
We also examined possible negative treatment effects as recommended by Rozental et al. (2014). Among the 65 patients who responded at follow up on BDI-II, we found that four patients (6%) deteriorated during treatment, one in TAU (3%) and three in ICBT (10%).
Discussion
Our main finding was that there was no significant difference between the ICBT and TAU in both BDI-II and MADRS-S scores. Furthermore, we found no difference between groups in the proportion of patients who recovered from depression according to the criterion of a BDI-II score of 13 or less. These findings accord well with previous efficacy studies showing ICBT to be at least as effective as other treatments for depression (Andersson & Cuijpers, 2009; Cuijpers et al., 2010; Richards & Richardson, 2012).
The mean number of completed modules in the ICBT treatment was 5.1 which implies that compared with live CBT in primary care and ICBT in previous efficacy studies (Cuijpers, Huibers, Ebert, Koole, & Andersson, 2013; Newby et al., 2013), we found a high adherence rate. In fact, 20 (56%), i.e., the majority of the patients receiving ICBT, completed all 7 modules. In Carlbring et al.'s (2013) trial of the same ICBT program on patients recruited by advertisement with a treatment period of 8 weeks, 11 of 40 patients (28 %) completed all 7 modules. One possible reason for the reversed findings in our study could be our prolonged treatment period that allowed patients 50% more time, 12 compared to 8 weeks. In PRIM-NET, 38 out of 179 (21%) first time access to any Internet modules were carried out after the initial 8-week period.
Among the strengths of our study is the comprehensive diagnostic interview of the patients performed by experienced psychologists/psychotherapists. This procedure ensured that the patient's needs were likely to be met by the treatment, a crucial aspect in achieving good effects for ICBT (Andersson et al., 2009). Furthermore, the recruitment of patients makes our study one of very few RCTs on ICBT accomplished in primary care and with results relevant to other primary care patients with mild to moderate depression.
Several limitations need to be addressed. First, despite an extended study period, we did not achieve our goal of recruiting 142 patients which left the study underpowered. Second, because the aim of the study was to assess the effectiveness in a real life primary care setting, our inclusion criteria allowed stable medication, which is common in similar studies (e.g., Carlbring et al., 2013; Vernmark et al., 2010) and our patients might have received other treatments for depression during the study period. Previous studies comparing treatments while allowing for stable medication find that medication status seem to be unrelated to change in depth of depression (Proudfoot et al., 2004; Vernmark et al., 2010). Third, PRIM-NET excluded patients with any suicidal ideation, a criterion probably not applied in regular care.
Finally, difficulties in recruiting patients is a well-known problem in clinical trials (Clarke et al., 2005; De Graaf et al., 2009; Mead et al., 2005) and long recruitment periods seem to be a common problem. During the PRIM-NET study period, 3603 patients were diagnosed with depression but only 90, i.e., 2.5% of the diagnosed, were included. Recruitment of mild to moderately depressed individuals from the general population or in primary health care is a challenge and often attracts interest by more severely depressed patients. One reason why interventions aimed at mild to moderate depression attract fewer patients than expected based on prevalence rates could be that those with mild to moderate depression are less likely to actively seek treatment (Kessler et al., 2003). One of the key symptoms of depression is a lack of motivation and the depression may have to become severe before it leads to actively seeking treatment. Sweden is one of the countries in the world with the highest Internet usage: 84.7% of the population. The young are more Internet literate with 94% of 16–24-year-olds using it daily, compared to only 50% of 65–74-year-old (Statistics Sweden, 2013). The mean age among all patients diagnosed with depression at participating primary care centers during PRIM-NET was roughly 53 years while the mean age of our included patients was 36.6 years. This is also considerably younger than the mean age of 44 years in the study by Carlbring et al. (2013). Our younger sample might reflect a more positive attitude to ICBT among younger primary care patients, but there is also a possibility that the primary care center staff selected patients who were believed to be Internet literate and for whom they also, for various reasons, thought the ICBT would be an accurate treatment rather than invite all with suspected depression. Both Clarke et al. (2005) and Mead et al. (2005) found that those accepting participation were older than those declining, the opposite of what seems to be the case for PRIM-NET, and thus supporting this notion. The generalizability of our results to primary care patients might be limited, but time suggests the opposite. As the population grows older, internet literacy and usage follows individuals into old age and the trend is therefore increased use of computers/Internet in everyday life for a growing proportion of the population. Although our sample was younger and more Internet literate than the average primary care patient, a post hoc analysis revealed that the effectiveness was in fact similar across age groups. There is also a high probability that when ICBT is introduced into primary care, the same type of patients that were recruited to this study will be attracted to this type of treatment.
For those suffering from mild to moderate depression, primary care is and should be their first point for help. Future research needs to address questions concerning (a) how a growing part of depressed patients can be identified and offered ICBT, (b) how individuals with mild depression can be identified and offered psychological treatment, and (c) whether the long-term effects differ between ICBT and TAU.
In conclusion, the implementation of ICBT in primary care offers a convenient and effective psychological therapy in patients affected by mild to moderate depression. From a patient perspective, ICBT might be seen as a new appealing treatment even if our first PRIM-NET Study report, based on short-term follow-up data provides no clear support for a superior effectiveness than TAU.
Acknowledgements
This study was sponsored by grants from the Region of Västra Götaland and REHSAM.
Declaration of interest
Kristofer Vernmark is employed by Psykologpartners W&W AB, which is a company developing and selling products related to the research described in this paper. The other six authors report no conflict of interest.
References
- Andersson G., Carlbring P., Berger T., Almlov J. Cuijpers P. What makes internet therapy work? Cognitive Behaviour Therapy. 2009;1:55–60. doi: 10.1080/16506070903116935. [DOI] [PubMed] [Google Scholar]
- Andersson G. Cuijpers P. Internet-based and other computerized psychological treatments for adult depression: A meta-analysis. Cognitive Behaviour Therapy. 2009;38:196–205. doi: 10.1080/16506070903318960. [DOI] [PubMed] [Google Scholar]
- Andersson G., Hesser H., Hummerdal D., Bergman-Nordgren L. Carlbring P. A 3.5-year follow-up of Internet-delivered cognitive behaviour therapy for major depression. Journal of Mental Health. 2013;22:155–164. doi: 10.3109/09638237.2011.608747. [DOI] [PubMed] [Google Scholar]
- Andersson G., Hesser H., Veilord A., Svedling L., Andersson F., Sleman O., … Carlbring P. Randomized controlled non-inferiority trial with 3-year follow-up of internet-delivered versus face-to-face group cognitive behavioural therapy for depression. Journal of Affective Disorders. 2013;151:986–994. doi: 10.1016/j.jad.2013.08.022. [DOI] [PubMed] [Google Scholar]
- Beck A. T., Epstein N., Brown G. Steer R. A. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck A. T., Steer R. A. Brown G. K. Svensk version (Swedish version). Stockholm: Psykologiförlaget AB; 2006. BDI-II, Beck Depression Inventory – Second edition. Manual. [Google Scholar]
- Bodlund O., Andersson S. -O. Mallon L. Effects of consulting psychiatrist in primary care 1-year follow-up of diagnosing and treating anxiety and depression. Scandinavian Journal of Primary Health Care. 1999;17:153–157. doi: 10.1080/028134399750002566. [DOI] [PubMed] [Google Scholar]
- Carlbring P., Brunt S., Bohman S., Richards J. C., Öst L. -G. Andersson G. Internet vs. paper and pencil administration of questionnaires commonly used in panic/agoraphobia research. Computers in Human Behavior. 2007;23:1421–1434. [Google Scholar]
- Carlbring P., Hagglund M., Luthstrom A., Dahlin M., Kadowaki A., Vernmark K. Andersson G. Internet-based behavioral activation and acceptance-based treatment for depression: A randomized controlled trial. Journal of Affective Disorders. 2013;148:331–337. doi: 10.1016/j.jad.2012.12.020. [DOI] [PubMed] [Google Scholar]
- Christensen H., Griffiths K. M. Farrer L. Adherence in internet interventions for anxiety and depression. Journal of Medical Internet Research. 2009;11:e13. doi: 10.2196/jmir.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke G., Eubanks D., Reid E., Kelleher C., O'Connor E., DeBar L. L. Gullion C. Overcoming depression on the Internet (ODIN) (2): A randomized trial of a self-help depression skills program with reminders. Journal of Medical Internet Research. 2005;7:e16. doi: 10.2196/jmir.7.2.e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P., Donker T., van Straten A., Li J. Andersson G. Is guided self-help as effective as face-to-face psychotherapy for depression and anxiety disorders? A systematic review and meta-analysis of comparative outcome studies. Psychological Medicine. 2010;40:1943–1957. doi: 10.1017/S0033291710000772. [DOI] [PubMed] [Google Scholar]
- Cuijpers P., Huibers M., Ebert D., Koole S. L. Andersson G. How much psychotherapy is needed to treat depression? A metaregression analysis. Journal of Affective Disorders. 2013;149:1–13. doi: 10.1016/j.jad.2013.02.030. [DOI] [PubMed] [Google Scholar]
- De Graaf L. E., Gerhards S. A. H., Arntz A., Riper H., Metsemakers J. F. M., Evers S. M. A. A. Huibers M. J. H. Clinical effectiveness of online computerised cognitive-behavioural therapy without support for depression in primary care: Randomised trial. British Journal of Psychiatry. 2009;195:73–80. doi: 10.1192/bjp.bp.108.054429. [DOI] [PubMed] [Google Scholar]
- Gwaltney C. J., Shields A. L. Shiffman S. Equivalence of electronic and paper-and-pencil administration of patient-reported outcome measures: A meta-analytic review. Value Health. 2008;11:322–333. doi: 10.1111/j.1524-4733.2007.00231.x. [DOI] [PubMed] [Google Scholar]
- Johansson R. Andersson G. Internet-based psychological treatments for depression. Expert Review of Neurotherapeutics. 2012;12:861–870. doi: 10.1586/ERN.12.63. [DOI] [PubMed] [Google Scholar]
- Johansson R., Carlbring P., Heedman Å., Paxling B. Andersson G. Depression, anxiety and their comorbidity in the Swedish general population: Point prevalence and the effect on health-related quality of life. PeerJ. 2013;1:e98. doi: 10.7717/peerj.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston L., Titov N., Andrews G., Spence J. Dear B. F. A RCT of a transdiagnostic internet-delivered treatment for three anxiety disorders: Examination of support roles and disorder-specific outcomes. PLoS One. 2011;6:e28079. doi: 10.1371/journal.pone.0028079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R. C., Berglund P., Demler O., Jin R., Koretz D., Merikangas K. R. Wang P. S. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Lecrubier Y., Sheehan D. V., Weiller E., Amorim P., Bonora I., Harnett Sheehan K. Dunbar G. C. The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: Reliability and validity according to the CIDI. European Psychiatry. 1997;12:224–231. [Google Scholar]
- Martell C. R., Dimidjian S. Herman-Dunn R. New York: Guilford Press; 2010. Behavioural activation for depression. A clinicians's guide. [Google Scholar]
- Mathers C. D. Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Medicine. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mead N., MacDonald W., Bower P., Lovell K., Richards D., Roberts C., Bucknall A. The clinical effectiveness of guided self-help versus waiting-list control in the management of anxiety and depression: A randomized controlled trial. Psychological Medicine. 2005;35:1633–1643. doi: 10.1017/S003329170500560X. [DOI] [PubMed] [Google Scholar]
- Montgomery S. A. Asberg M. A new depression scale designed to be sensitive to change. British Journal of Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- Newby J. M., Mackenzie A., Williams A. D., McIntyre K., Watts S., Wong N., Andrews G. Internet cognitive behavioural therapy for mixed anxiety and depression: A randomized controlled trial and evidence of effectiveness in primary care. Psychological Medicine. 2013 doi: 10.1017/S0033291713000111. in press. doi:10.1017/S0033291713000111. [DOI] [PubMed] [Google Scholar]
- Priest R. G., Vize C., Roberts A., Roberts M. Tylee A. Lay people's attitudes to treatment of depression: Results of opinion poll for defeat depression campaign just before its launch. British Medical Journal. 1996;313(7061):858–859. doi: 10.1136/bmj.313.7061.858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proudfoot J., Goldberg D., Mann A., Everitt B., Marks I. Gray J. A. Computerized, interactive, mltimedia cognitive-behavioural program for anxiety and depression in general practice. Psychological Medicine. 2003;33:217–227. doi: 10.1017/S0033291702007225. [DOI] [PubMed] [Google Scholar]
- Proudfoot J., Ryden C., Everitt B., Shapiro D. A., Goldberg D., Mann A. Gray J. A. Clinical efficacy of computerised cognitive-behavioural therapy for anxiety and depression in primary care: Randomised controlled trial. British Journal of Psychiatry. 2004;185:46–54. doi: 10.1192/bjp.185.1.46. [DOI] [PubMed] [Google Scholar]
- Richards D. Richardson T. Computer-based psychological treatments for depression: A systematic review and meta-analysis. Clinical Psychology Review. 2012;32:329–342. doi: 10.1016/j.cpr.2012.02.004. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne P. P., Sherbourne C. D., Craske M. G., Stein M. B., Katon W., Sullivan G. Bystritsky A. Moving treatment research from clinical trials to the real world. Psychiatric Services. 2003;54:327–332. doi: 10.1176/appi.ps.54.3.327. [DOI] [PubMed] [Google Scholar]
- Rozental A., Andersson G., Boettcher J., Ebert D., Cuijpers P., Knaevelsrud C., … , Carlbring P. Internet Interventions. 2014. Consensus statement on defining and measuring negative effects of internet interventions. http://www.invent-journal.com/ [Google Scholar]
- SBU . Stockholm: Stockholm SBU; 2004. Behandling av depressionssjukdomar, En systematisk litteraturöversikt. SBU-rapport nr 166/1 [Treatment of depressive disorders, a systematic literature review. SBU report No. 166/1]. [PubMed] [Google Scholar]
- Sheehan D. V., Lecrubier Y., Sheehan K. H., Amorim P., Janavs J., Weiller E. Dunbar G. C. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal Clinical Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- Statistics Sweden . Stockholm: SCB; 2013. Use of computers and the internet by private persons in 2012. [Google Scholar]
- Swedish National Board of Health and Welfare . Stockholm: Socialstyrelsen; 2010. Nationella riktlinjer för vård vid depression och ångestsyndrom 2010 – stöd för styrning och ledning. [National guidelines for treatment of depression and anxiety 2010: Support for governance and management]. [Google Scholar]
- Swedish National Board of Health and Welfare . Stockholm: Socialstyrelsen; 2013. Nationell utvärdering 2013 – vård och insatser vid depression, ångest och schizofreni Rekommendationer, bedömningar och sammanfattning. [National evaluation, 2013 – care and interventions for depression, anxiety and schizophrenia, recommendations, estimates and summary]. [Google Scholar]
- Vernmark K., Lenndin J., Bjärehed J., Carlsson M., Karlsson J., Öberg J., Andersson G. Internet administered guided self-help versus individualized e-mail therapy: A randomized trial of two versions of CBT for major depression. Behaviour Research and Therapy. 2010;48:368–376. doi: 10.1016/j.brat.2010.01.005. [DOI] [PubMed] [Google Scholar]
- Vickers A. J. Analysis of variance is easily misapplied in the analysis of randomized trials: A critique and discussion of alternative statistical approaches. Psychosomatic Medicine. 2005a;67:652–655. doi: 10.1097/01.psy.0000172624.52957.a8. [DOI] [PubMed] [Google Scholar]
- Vickers A. J. Parametric versus non-parametric statistics in the analysis of randomized trials with non-normally distributed data. BMC Medical Research Methodology. 2005b;5:35. doi: 10.1186/1471-2288-5-35. [DOI] [PMC free article] [PubMed] [Google Scholar]


