Abstract
Reflection is an important learning technique for surgeons during their training and is a valuable tool for life-long learning and maintenance of certification to assure competency. Reflection helps individuals to evaluate their performance in the interest of improving their ability to deal with similar experiences in the future. Additionally, reflection can be helpful for established surgeons to continue to improve upon their performance and hone their craft. This article outlines the theoretical role of reflection in the learning process. We will discuss methods for incorporating reflection into training programs, and review the evidence for implementing reflection in surgical training.
Keywords: Surgery training, reflection, adult learning theory
Introduction
Given the busy nature of medical practice, it can be difficult for surgeons to find time to stop and reflect on activities and achievements. This is especially true during residency, when the pace of daily activities interspersed with several conferences a week often does not give the trainee time to pause and reflect on the materials they are expected to learn. However, the process of reflection is an integral part of development as a trainee and continued growth as a practicing surgeon. In the field of Surgery, every operation requires the coordination of many different activities, including setting up the operating room, obtaining the right equipment, planning for the surgical procedure, and orchestrating the surgical team to make sure the patient has a safe procedure. At the same time, the surgeon must be able to perform the technical aspects of the operation flawlessly, and if a particular surgical plan does not seem to work because of anatomic variation and unexpected findings during the operation, the surgeon may need to improvise swiftly using alternate methods of reconstruction. Given the multitude of factors that contribute to the outcome of the procedure, reflection is helpful for one to learn what went wrong and what went well during the procedure to improve the quality of care for future patients.
The methods of reflection described in this article are not simply for trainees, but are also important components of continued and lifelong learning. Because of the exponential increase in knowledge and surgical skills required, surgeons cannot rely merely on what they learned during training to subsist their growth as a surgeon throughout their career. Therefore, application of reflection, in the form of self-evaluation of events during the day, is even more important for one’s intellectual growth to improve one’s professional practices. Although a surgeon may have performed countless breast reconstructions, even a routine breast reconstruction procedure is cause for reflection at the end of the day to assess what went well and what could have been done differently to achieve optimal outcomes in future cases.
Theoretical models of reflection
In order to discuss reflection in surgical training, it is important to precisely define this term. Colloquially, reflection implies thinking something over in one’s head. In relation to education and learning, reflection is more complex. John Dewey, a renowned philosopher and educational reformer in the early 1900s often spoke of the importance of reflection in education.1,2 In his works, Dewey emphasizes four major criteria that can be used to help define reflection. First, he explains that reflection is a process to help a learner move from one experience to the next, while developing knowledge that will help them with the new experience. This aspect of Dewey’s definition of reflection also applies to surgical training. In Surgery, trainees often learn to conduct the procedure by first watching the procedure being performed, then performing a procedure, and finally showing the procedure to another individual. This is often referred to as the “See one, do one, teach one” method.3 During this process, it is important for the trainee to reflect upon what went well and what went poorly during these experiences to improve their performance in the future.
Dewey’s second criterion for reflection explains that reflection is strengthened when it is shared with others. For a surgical trainee, this may involve discussion with a mentor or peer. During this practice of sharing reflections, peers and mentors can help to reaffirm the ideas that they agree with. Moreover, they may offer new perspectives or their own experiences in certain instances. Sharing reflective thoughts with others can reinforce reflective practice, because trainees feel accountable to the group, which can promotes participation and engagement in reflection.4
Third, reflection involves knowledge of one’s attitudes and emotions, and the effect of those feelings on one’s actions and thoughts.4,5 Dewey notes that humans are both emotional and intellectual beings, and that both of these factors affect our decision-making process. For example, while determining care for a patient, a surgeon who is passionate about performing a certain procedure may be more likely to prescribe this treatment, without considering the benefits of alternative methods. According to Dewey, upon reflecting on this treatment recommendation, the surgeon should realize his/her preference for the treatment, and prescribe alternative treatments in the future that may be more effective for particular patients.
The last criterion of Dewey’s definition is that reflection is not a casual process, but rather a rigorous and deliberate activity that distinguishes reflection from other types of thought such as “stream of consciousness” and “beliefs.” In surgical training, this rigor could equate to thinking critically about specific steps of a procedure, and how well they were performed. This rigorous process could also include reflecting upon whether the correct procedure was chosen in order to achieve the optimal outcome. Despite Dewey’s description of reflection as a deliberate process, he does not describe a specific structure that explains the role reflection plays in learning.
David Kolb expanded upon Dewey’s definition of reflection with an experiential learning theory that incorporated reflection as part of the learning process. Kolb articulated that reflection is one of the four cornerstones of experiential learning. Specifically, Kolb’s theory explains that learning involves: concrete experience, reflective observation, abstract conceptualization, and active experimentation (Figure 1).6 This learning cycle begins with concrete experiences, which the learner reflects upon and forms observations. Next, the learner forms abstract concepts and generalizations from the experience, and uses these to guide actions in future similar experiences.6
Fig. 1.
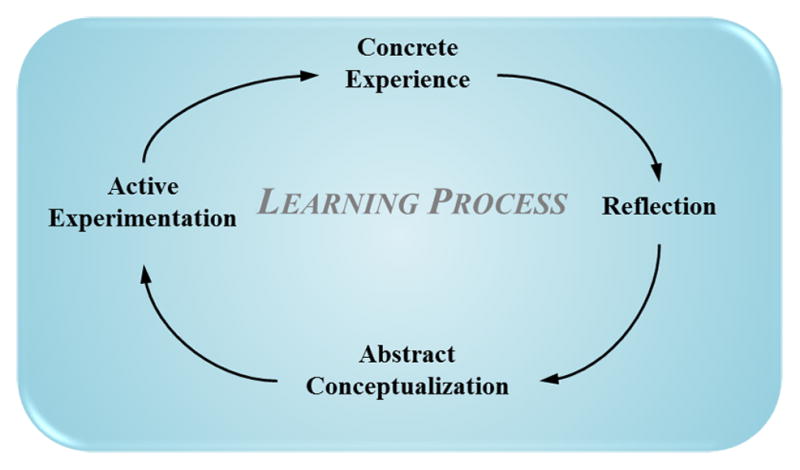
Diagram of the learning cycle as described by Kolb. Learning begins with concrete experiences. The learner then reflects upon these experiences, leading to the formation of abstract concepts and generalizations. These concepts and generalizations are then used to guide future action through active experimentation.
Kolb’s model is well suited to describe the learning process of a surgeon. During breast reconstruction, a surgeon must consider a number of technical and aesthetic factors to optimize the satisfaction of the patient. In Kolb’s model, concrete experience would be described by the surgeon conducting the procedure, or watching the procedure being conducted by another surgeon. Reflective observation would then occur after the procedure, as the surgeon thinks about what aspects of the procedure went well, and what aspects could use improvement. Some questions that may be considered are: Did I use the best procedure? Was the skin flap viable? Was the breast shaped to match the contralateral breast? Abstract conceptualization then involves the surgeon thinking about what techniques or treatments options could improve treatment for similar patients in the future. Finally, active experimentation occurs when the surgeon provides alternative methods of treatment for the next patient with a similar problem and looks to increase the patient’s satisfaction.
Donald Schon applied Kolb’s concepts of reflection to professional development in his book The Reflective Practitioner.7 In this book, Schon introduced the concepts of “reflection-on-action” and “reflection-in-action”. He describes that reflection-on-action occurs after the fact and involves determining what was done and what can be done in the future to improve the result, such as the previous example regarding breast reconstruction. This type of reflection leads to what Schon calls “reflection-in-action”, which is the practitioner’s ability to “think on their feet.” This ability involves self-monitoring by the practitioner and internally asking oneself whether they are dealing with the situation effectively. Schon’s theory adds to Kolb’s learning styles because it helps describe intuition, and the ability to improvise that is a result of the developed wisdom of senior surgeons over years of experience. In this way, active reflection-inaction can occur only after a surgeon continues to engage reflection-on-action to build fragments of knowledge that add over time to form experiential wisdom.
How to implement reflection into surgical education
Reflection may be implemented in surgical training using a number of different methods. Portfolios have become a popular educational tool to promote reflection. For medical trainees, portfolios can provide a useful tool to organize and compile their work during the course of a program. The CanMEDS portfolio is one such portfolio developed at the University of Toronto. This resource prompts trainees to keep track of their achievements in research, education, teaching, clinical experiences, and leadership roles.8 In addition to traditional portfolios, electronic portfolios may be used to promote reflection. Some have even suggesting using online blogs, or social media including Twitter to promote reflection in medical trainees.9 These types of tools may promote participation in reflection by making the process more convenient and engaging. However, while using these methods, it is important to ensure that private health information is secure. In addition to these structured methods, reflection can also be done more informally such as though oral discussions with a mentor or peer.
Regardless of the form of reflection, there are a number of questions to consider while reflecting on an event or experience. Gibbs’ Structured Debriefing is a model that is commonly used to provide structure to the reflection process (Figure 2).10 This model begins with the individual describing the event, then evaluating their reaction and analyzing the situation. The individual then forms conclusions about the event and creates a personal action plan for dealing with similar events in the future. Table 1 details a surgeon going through a debriefing after an operation that went poorly.
Fig. 2.
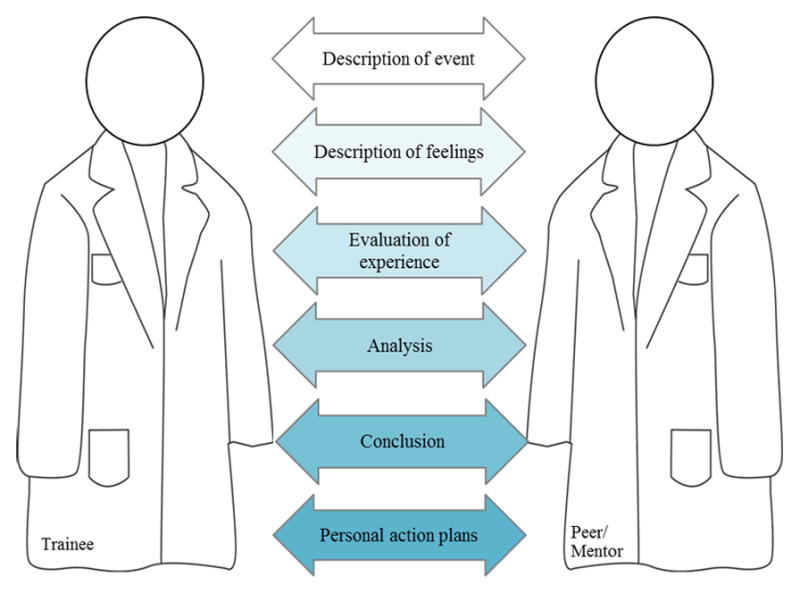
Gibb’s Structured Debriefing. This structured debriefing lists a number of ideas that a trainee can discuss with a peer or mentor while debriefing after a procedure. The process starts with a description of the event and ends with developing an action plan for similar future cases.
Table 1.
Debriefing after a finger arthroplasty procedure using Gibbs’ structured debriefing.
| Stage of Debriefing | Reflections/observations |
|---|---|
| Description of events | When performing a finger arthroplasty procedure using a particular new type of implant, the operating surgeon did not check whether the implant was ready for the operation, and proceeded to make an incision. During surgery, when asking for the implant, it was found that the implant was not the implant that the surgeon wanted. |
| Description of feelings | The surgeon was uncomfortable that the essential material was not available for the procedure. |
| Evaluation | The surgeon felt confident with the technical aspects of the procedure, as he had performed similar procedures multiple times. However, the preparation for the procedure was poor, as there was no confirmation that the essential materials had been ordered and prepared for the procedure. |
| Analysis | The surgeon realized that he had requested the implant, but there was a miscommunication between him and the nursing staff regarding the exact type of implant required. |
| Conclusions | More care needs to be taken regarding ordering materials for procedures, and confirming that the correct materials are available in the operating room. |
| Personal action plan | In the future, the surgeon and the nurse lead will verify that the correct implant has been ordered and is available 24 hours before the surgical procedure. Furthermore, another verification stage is to confirm that the implant is in the operating room prior to bringing the patient back to the operating room. |
Debriefing, which is required in most operating rooms, is not necessarily restricted to negative experiences. These exercises should also focus on what went well. For example, a surgeon performing a facelift operation had a smooth conduct of the surgical procedure and in record time. At the end of the procedure, the surgeons should reflect and assess all of the processes that worked well. These factors may include the nurses setting up the equipment tray with all of the necessary equipment, appropriate preoperative planning to ensure sequential, meticulous elevation of the skin and fascia flaps, and prudence of the anesthesiologist in inducing the patient and waking the patient smoothly from anesthesia without significant changes in blood pressure. Sharing these reflections with co-workers not only highlights particularly effective methods, but also positively reinforces good habits in the operating room and boosts morale.
In addition to these methods of reflection, the senior author (KCC) has incorporated reflection into his practice by reviewing preoperative, intraoperative, postoperative pictures for every patient with his assistant weekly if possible. By viewing these pictures, one can reflect on whether the preoperative decision-making process is appropriate. These sessions require one to be introspective to promote self-guided assessment and reflection.
Evidence for Incorporating Reflection
Although there is limited empirical evidence in the literature regarding the impact of reflection on training, a few studies have investigated this area. Toy et al. conducted a study looking at the effect of incorporating reflection into an Obstetrics and Gynecology resident training program.11 Once a month, residents were given an hour to reflect on their past rotation and set goals for the upcoming rotation. This was done for six months. Clinical performance was measured using the number of procedures that each trainee logged in the ACGME website during the six-month period at the end of the program. All the residents reported that the reflection time was more valuable to them than the traditional didactic time it replaced. Moreover, all residents reported performing more clinical procedures during the six months that reflection was implemented than during the six months without the reflection time. The authors concluded that an increase of reflective practice correlated with an increase in clinical performance and efficiency.
Sobral et al. evaluated the effect of reflection on learning in a group of medical students. They measured reflection using a 14-item questionnaire called the Reflection-in-Learning Scale (RLS) to appraise the students’ use of reflective learning. One hundred and three medical students participated in a 30-hour course geared towards improving learning methods by developing self-appraisal and reflective thinking.12 This course separated the students into small groups that met two hours per week. The program specifically encouraged self-appraisal of current learning practices, discussion of learning strategies with peers, and setting and evaluating achievement of learning goals. At the end of the term, the authors found that 81% of the students reported higher scores on the Reflection-In-Learning Scale than at the beginning of the term. This indicated an increase in the students’ use of reflection. Moreover, they found that at the end of the term, the more reflective individuals, as determined by the Reflection-in-Learning Scale, had a higher average grade point average.
Lonka et al. studied the use of portfolios in an Obstetrics and Gynecology training course in Finland.13 They found that the degree of the students’ participation in the portfolio activity (measured by amount of written text in the portfolio) correlated with their performance in the course. Students had generally positive attitudes towards participating in the reflection exercises: 50% of the students reported the portfolio to be useful, 16% of the students reported negative comments on the portfolio, and 34% refrained from commenting on the portfolio. A similar study was conducted with medical educators. Beecher et al. studied reflection of medical educators using educational portfolios.14 They found that at the end of the study, all 10 participants indicated that the reflection during this exercise caused them to change their lesson plans in the future.
Given the limited data on reflection and education, it is difficult to say that implementation of reflection necessarily correlates with higher test scores or improved performance. However, it is evident that reflection time is valued by medical trainees. More research should be conducted in the future to determine the effect of implementing reflection in a training program. Furthermore, different methods of incorporating reflection into surgical training should also be evaluated for effectiveness.
Conclusion
Reflection is an important learning tool for surgical training, and continued education of established surgeons. The conceptual basis of reflection is described by the theories of Dewey, Kolb, and Schon. Reflection may be incorporated into surgical training and practice by use of portfolios, electronic methods, and informal meetings with peers and mentors. Incorporating these methods will promote the value of self-evaluation, and will promote practices that ultimately can improve patient outcomes.
Acknowledgments
Supported in part by grants from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (2R01 AR047328-06) National Institute of Arthritis and Musculoskeletal and Skin Diseases and National Institute on Aging (R01 AR062066) and a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) (To Dr. Kevin C. Chung).
References
- 1.Dewey J. How we think. Boston: Heath & Co; 1933. [Google Scholar]
- 2.Dewey J. Democracy and education : an introduction to the philosophy of education. London, England: Free Press; 1944. [Google Scholar]
- 3.Kotsis SV, Chung KC. Application of the “see one, do one, teach one” concept in surgical training. Plast Recon Surg. 2013;131:1194–201. doi: 10.1097/PRS.0b013e318287a0b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rodgers C. Defining Reflection: Another Look at John Dewey and Reflective Thinking. Teach Coll Rec. 2002;104:842–66. [Google Scholar]
- 5.Dewey J. Experience and Education. United States: Kappa Delta Pi; 1938. [Google Scholar]
- 6.Kolb DA. Experience as the source of learning and development. Englewood Cliffs, N.J: Prentice-Hall; 1984. Experiential learning. [Google Scholar]
- 7.Schön DA. The reflective practitioner : how professionals think in action. New York: Basic Books; 1983. [Google Scholar]
- 8.Berger E, Shouldice M, Kuper A, Albert M. The CanMEDS portfolio: a tool for reflection in a fellowship programme. Clin Teach. 2011;8:151–5. doi: 10.1111/j.1743-498X.2011.00463.x. [DOI] [PubMed] [Google Scholar]
- 9.Forgie SE, Duff JP, Ross S. Twelve tips for using Twitter as a learning tool in medical education. Med Teach. 2013;35:8–14. doi: 10.3109/0142159X.2012.746448. [DOI] [PubMed] [Google Scholar]
- 10.Gibbs G. Learning by Doing: a Guide to Teaching and Learning. Cheltenham: Further Education Unit; 1988. [Google Scholar]
- 11.Toy EC, Harms KP, Morris RK, Jr, Simmons JR, Kaplan AL, Ownby AR. The effect of monthly resident reflection on achieving rotation goals. Teach Learn Med. 2009;21:15–9. doi: 10.1080/10401330802384276. [DOI] [PubMed] [Google Scholar]
- 12.Sobral DT. Medical students’ mindset for reflective learning: a revalidation study of the reflection-in-learning scale. Adv Health Sci Educ Theory Pract. 2005;10:303–14. doi: 10.1007/s10459-005-8239-0. [DOI] [PubMed] [Google Scholar]
- 13.Lonka K, Slotte V, Halttunen M, et al. Portfolios as a learning tool in obstetrics and gynaecology undergraduate training. Med Educ. 2001;35:1125–30. doi: 10.1046/j.1365-2923.2001.01054.x. [DOI] [PubMed] [Google Scholar]
- 14.Beecher ALJ, Morzinski A. Use of the educator’s portfolio to stimulate reflective practice among medical educators. Teaching and Learning in Medicine. 1997;9:56–9. [Google Scholar]


