Abstract
Background
CKD, an independent risk factor for CV disease, increases mortality in T2DM. Treating modifiable CV risk factors decreases mortality in diabetics with microalbuminuria, but the role of early CV prevention in diabetics with mild CKD by GFR criteria alone remains unclear. The purpose of this study was to probe whether T2DM patients with mild GFR impairment have atherogenic lipid profiles compared to diabetic counterparts with normal renal function.
Methods
In the Penn Diabetes Heart Study (PDHS), a single-center observational cohort of T2DM patients without clinical CVD, cross-sectional analyses were performed for directly measured lipid fractions in 1852 subjects with eGFR>60 mL/min/1.73 m2 determined by the CKD-EPI equation (n = 1852). Unadjusted and multivariable analyses of eGFR association with log-transformed lipid parameters in incremental linear and logistic regression models (with eGFR 90 mL/min/1.73 m2 as a cut-point) were performed.
Results
Mild GFR impairment (eGFR 60–90 mL/min/1.73 m2, median urinary ACR 5.25 mg/g) was associated with higher log-transformed Lp(a) values (OR 1.17, p = 0.005) and with clinically atherogenic Lp(a) levels above 30 mg/dL (OR 1.35, p = 0.013) even after full adjustment for demographics, medications, metabolic parameters, and albuminuria. Logistic regression demonstrated a trend towards significance between worse kidney function and apoB (p = 0.17) as well as apoC-III (p = 0.067) in the fully adjusted model.
Conclusions
Elevated Lp(a) levels have a robust association with mild GFR impairment in type 2 diabetics independent of race, insulin resistance, and albuminuria.
Introduction
Affecting over 20 million patients in the United States alone, chronic kidney disease (CKD) is an independent risk factor for cardiovascular (CV) disease and increased CV mortality [1]–[4]. Recently, CKD has been shown to be the predominant contributor to mortality among patients with type 2 diabetes mellitus (T2DM) [5], which still carries a high absolute risk of CV mortality despite more aggressive treatment of modifiable risk factors [1], [6]–[10]. This persistently elevated mortality risk may in part be due to unrecognized diabetic subpopulations at increased risk as well as unrecognized novel risk factors.
Prior studies examining mortality and CV outcomes in diabetics with CKD have focused on patients with microalbuminuria or with an estimated glomerular filtration rate (eGFR) less than 60 mL/min/1.73 m2. The role of early CV prevention for T2DM patients with mild GFR impairment (eGFR 60–90 mL/min/1.73 m2) in the absence of albuminuria remains unclear. Understudied, this group of diabetics without microalbuminuria does not meet current definitions of CKD and is not considered to be at increased CV risk [2]–[4], [11], [12]. However, mild GFR impairment may also be associated with modestly increased risk of both subclinical CV disease and adverse CV outcomes [5], [13], [14].
Furthermore, consensus guidelines for lipid management in T2DM patients with microalbuminuria or moderate to severe CKD focus on lowering low-density lipoprotein cholesterol (LDL-C) [11], [12], [15], which does not account for the full profile of lipid derangements seen in renal disease. Past studies have shown that CKD, even with microalbuminuria and eGFR>60 mL/min/1.73 m2 [16], is associated with elevated triglycerides (TG) and reduced high-density lipoprotein (HDL) but only minimal changes in LDL-C levels [17]–[20]. Dyslipidemia associated with renal impairment is also characterized by higher levels of triglyceride-rich lipoproteins (TGRL), which have recently garnered resurgent interest as causal biomarkers of CVD [21]–[23]. Measures of TGRLs include very-low-density lipoprotein (VLDL) cholesterol and triglycerides, apolipoprotein B (apoB), and apolipoprotein C-III (apoC-III), a protein that blocks lipoprotein lipase (LPL) and thus decreases VLDL metabolism and clearance. [17], [18], [23]–[30] In addition, lipoprotein(a) [Lp(a)], a lipoprotein consisting of an apo(B) moiety covalently linked to apolipoprotein(a) [apo(a)] and an independent genetic and causal risk factor for CVD [31]–[38], is significantly elevated in CKD patients compared to control populations [20], [38]–[41].
The purpose of this study was to probe whether T2DM patients with mild GFR impairment have atherogenic lipid profiles compared to their diabetic counterparts with normal renal function. We examined the association of mild GFR impairment, defined as eGFR between 60 and 90 mL/min/1.73 m2, with elevations in specific plasma lipid fractions in the Penn Diabetes Heart Study (PDHS), a cohort study of patients with T2DM but without overt CV disease or moderate to severe CKD. We hypothesized that mild renal impairment by eGFR criteria is already associated with atherogenic lipoprotein distribution characterized by elevated TG, VLDL-C, apoB, apoC-III, as well as increased circulating Lp(a).
Materials and Methods
Study Population
The Penn Diabetes Heart Study (PDHS), as previously described [42]–[46], is a single-center cross-sectional observational cohort of 2118 patients with T2DM, enrolled between 2001 and 2011. Participants were recruited from primary care and endocrinology clinics affiliated with the Hospital of the University of Pennsylvania (HUP). The University of Pennsylvania (Penn) Institutional Review Board approved the study protocol, and all subjects gave written informed consent. Inclusion criteria were: 1) a clinical diagnosis of T2DM (defined as fasting blood glucose >126 mg/dl, 2-hour post-prandial glucose >200 mg/dl, or use of oral hypoglycemic agents/insulin in a subject greater than age 40 years); 2) age of 35–75 years; and 3) a negative pregnancy test (if female and of child-bearing age). Exclusion criteria were: 1) history of clinical CV disease defined by myocardial infarction (MI), documented angiographic coronary artery disease, positive stress test, coronary or peripheral revascularization, stroke, or transient ischemic attack; 2) insulin use prior to age 35; 3) renal insufficiency defined at the time of recruitment as serum creatinine greater than 2.5 mg/dL; 4) active infection or malignancy; and 5) weight more than 300 pounds. For the current study, subjects were additionally excluded if their urinary albumin to creatinine ratio (ACR) was greater than 3000 mg/g or if their serum creatinine-based eGFR, calculated by the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [47], was determined to be below 60 mL/min/1.73 m2, leaving final sample size of 1852 subjects.
Data Collection
Study subjects were evaluated at the Clinical and Translational Research Center (CTRC) at HUP after a 12-hour fast. They completed a questionnaire regarding past medical, social, and family history as well as use of medications. Height, weight, waist and hip circumference, and bilateral resting systolic and diastolic blood pressures were measured. Samples of whole blood and urine were collected, processed, and stored (at −80 C). Complete blood count, basic metabolic panel, hemoglobin A1c, and microalbuminuria assays were performed at the clinical laboratories of HUP. Plasma insulin levels were measured at the core laboratory of the Penn Diabetes Center by radioimmunoassay (Linco Research, St. Charles, MO). Total cholesterol (TC), TG, HDL-C, and VLDL-C were measured enzymatically, while LDL-C was measured directly, after ultracentrifugation (β-centrifugation technique) in a Centers for Disease Control (CDC) certified lipid laboratory [42], [43], [45]. Lp(a) and apolipoproteins were measured by immunoturbidimetric assay (Wako Chemicals, U.S.A. Inc., Richmond, VA) on a Hitachi 912 autoanalyzer (Roche Diagnostics, Basel, Switzerland). Laboratory test results were generated by personnel blinded to the clinical characteristics of the study participants.
Hypertension was defined as meeting one of the following criteria: 1) self-reported history of hypertension; 2) use of anti-hypertensive medications; 3) documented systolic blood pressure measurement greater than 140 mmHg; or 4) documented diastolic blood pressure measurement greater than 90 mmHg. Fasting homeostasis model assessment-estimated insulin resistance (HOMA-IR) was calculated using the following equation: (glucose [mg/dL] × insulin [µIU/mL]/405) [48]. eGFR was calculated based on the CKD-EPI equation [47]. Urinary ACR for each subject, reported in mg/g, was calculated by dividing spot urine albumin by spot urine creatinine concentrations.
Statistical Analysis
For descriptive data and unadjusted analyses of lipid profiles, the study population was divided into two groups based on eGFR 60–90 vs. eGFR>90 ml/min/1.73 m2. Data distributions are reported as median and interquartile range (IQR) for continuous variables and as proportions for categorical variables. Unadjusted analyses compared data across the two different groups using the chi-squared test, Student's t-test, and the Wilcoxon rank sum test. Data for unadjusted analyses were also presented separately according to race, which has been shown to influence lipid profiles [49].
Lipid biomarkers with skewed distributions were log-transformed for multivariable analysis. Multivariable associations of lipid parameters with eGFR were analyzed separately as a continuous outcome and as a binary outcome for the groups 60 mL/min/1.73 m2 <eGFR <90 mL/min/1.73 m2 and eGFR>90 mL/min/1.73 m2. Associations were assessed in the following incremental logistic regression models: Model 1 was adjusted for age, race, and gender; Model 2 was also adjusted for body mass index (BMI), hypertension, and use of lipid-lowering medications; Model 3 was further adjusted for duration on insulin, hemoglobin A1c, and HOMA-IR; and Model 4 was additionally adjusted for urinary ACR. In addition, because Lp(a) values >30 mg/dL are associated with CV disease [36], logistic regression was performed on Lp(a) as a binary variable using 30 mg/dL as a cut-off value. Interactions between eGFR and race, gender, hypertension, and urinary ACR in association with Lp(a) were probed through interaction terms incorporated into the fully adjusted regression models. Correction for multiple testing was not performed given the clinical correlation among outcome variables and the complementary nature of the following multivariable models. Statistical analyses were performed using STATA version 13.0 software (Stata Corps, College Station, TX).
Results
Characteristics of Study Population by eGFR Profiles and Race
Baseline characteristics of this sample of PDHS subjects, divided according to eGFR groups of 60–90 and >90 mL/min/1.73 m2, are presented in Table 1. The majority of the 1852 participants were male (63.7%). The higher eGFR group had a larger proportion of black participants (39.8% vs. 27.5%, p<0.001), higher fasting glucose levels (121 vs. 112 mg/dL, p<0.001), and slightly lower urinary ACR values (4.9 vs. 5.3 mg/g, p = 0.04).
Table 1. Baseline Characteristics by eGFR Category.
| eGFR>90 mL/min/1.73 m2 | eGFR 60–90 mL/min/1.73 m2 | P Value | |
| Number | 998 | 854 | |
| Age | 56 (50–62) | 63 (56–68) | <0.001 |
| Gender | 0.027 | ||
| Men | 61.4% | 66.4% | |
| Women | 38.6% | 33.6% | |
| Race | <0.001 | ||
| White | 54.1% | 67.1% | |
| Black | 39.8% | 27.5% | |
| Other | 6.1% | 5.4% | |
| Hypertension | 73% | 81% | <0.001 |
| Systolic BP (mmHg) | 130 (121–140) | 131 (121–143) | 0.12 |
| Diastolic BP (mmHg) | 77 (72–83) | 75 (71–81) | 0.001 |
| Waist Circumference (in) | 106 (97–117) | 107 (97–116) | 0.95 |
| BMI (kg/m2) | 32 (28–37) | 32 (28–36) | 0.20 |
| Glucose (mg/dL) | 121 (96–155) | 112 (94–138) | <0.001 |
| Hemoglobin A1c (%) | 6.8 (6.2–8) | 6.7 (6.1–7.4) | <0.001 |
| HOMA-IR | 4.68 (3.04–7.87) | 4.29 (2.77–6.68) | 0.10 |
| Serum Creatinine (mg/dL) | 0.8 (0.7–0.89) | 1.0 (0.9–1.1) | <0.001 |
| BUN (mg/dL) | 13 (11–16) | 17 (14–19) | <0.001 |
| eGFR (CKD-EPI) | 101.2 (95.48–109.45) | 78.82 (72.09–84.69) | <0.001 |
| Urinary ACR (mg/g) | 4.9 (3–18.2) | 5.3 (3–17.5) | 0.04 |
| Anti-Hypertensive Medications | |||
| ACE Inhibitor or ARB | 56.1% | 65.1% | <0.001 |
| Diuretic | 24.6% | 33.7% | <0.001 |
| CCB | 14.6% | 20.5% | 0.001 |
| Beta Blocker | 12.0% | 16.1% | 0.01 |
| Lipid-Lowering Medications | |||
| Statin | 51.4% | 59.4% | <0.001 |
| Fibrate | 4.3% | 7.5% | 0.003 |
| Niacin | 5.6% | 5.7% | 0.77 |
Categorical variables are shown as proportions; continuous variables as median values (IQR). Abbreviations: BP blood pressure, BMI body mass index, HOMA-IR homeostatic model assessment of insulin resistance, BUN blood urea nitrogen, eGFR estimated glomerular filtration rate, CKD-EPI Chronic Kidney Disease Epidemiology Collaboration, ACR albumin to creatinine ratio, CCB calcium channel blocker.
Lipid profiles by unadjusted analysis, reported as median values for each lipid parameter in Table 2, also differed between the eGFR groups. Because race may influence lipid profiles, unadjusted analyses for each lipid fraction are also presented by race. Compared to the higher eGFR group, the group with reduced eGFR had lower median LDL-C (93 vs. 98, p = 0.02), lower median apoA-II (33 vs. 34, p = 0.02), lower median apoB (79 vs. 82, p = 0.004), and higher median apoC-III (11.6 vs. 10.8, p = 0.04). Across all subjects, median Lp(a) did not differ between eGFR groups (20 vs. 20, p = 0.5), but median plasma Lp(a) levels were higher among black participants in the lower eGFR group compared to black participants in the higher eGFR group (49 vs. 42, p = 0.02).
Table 2. Lipid and Lipoprotein Measurements by eGFR Category.
| eGFR (mL/min/1.73 m2), All Races | P Value | eGFR (mL/min/1.73 m2), White Subjects | P Value | eGFR (mL/min/1.73 m2), Black Subjects | P Value | ||||
| >90 | 60–90 | >90 | 60–90 | >90 | 60–90 | ||||
| TC* | 173 (149–198) | 169 (146–196) | 0.07 | 169 (148–195) | 167 (145–194) | 0.25 | 176 (153–200) | 170 (151–197) | 0.22 |
| HDL-C* | 46 (37–55) | 45 (38–55) | 0.82 | 44 (36–52) | 44 (37–52) | 0.65 | 48 (41–58) | 49 (40–61) | .39 |
| LDL-C* | 98 (79–120) | 93 (77–115) | 0.02 | 94.5 (78–116) | 92 (76–113) | 0.25 | 104 (82–125) | 96 (82–116) | 0.08 |
| VLDL-C* | 24 (17–35) | 25 (17–37) | 0.44 | 26 (19–38) | 27 (18–39) | 0.61 | 20 (14–29) | 22 (15–29) | 0.71 |
| TG* | 113 (80–170) | 116 (85–170) | 0.20 | 129 (94–194) | 132 (92–187) | 0.53 | 92 (70–127) | 99 (74–128) | 0.49 |
| ApoA-I§ | 130 (116–147) | 129 (116–144) | 0.40 | 129 (114–146) | 129 (116–142) | 0.62 | 134 (120–149) | 135 (118–155) | 0.62 |
| ApoA-II§ | 34 (31–38) | 33 (30–37) | 0.02 | 34 (30–37) | 33 (30–37) | 0.22 | 34 (31–39) | 34 (30–38) | 0.15 |
| ApoB§ | 82 (70–96) | 79 (68–92) | 0.004 | 82 (72–96) | 80 (69–92) | 0.03 | 83 (70–96) | 78 (68–91) | 0.06 |
| ApoC-III§ | 10.8 (7.5–15.4) | 11.6 (8.3–15.6) | 0.04 | 12.1 (9–16.2) | 12.2 (9.2–16.2) | 0.71 | 8.75 (6.1–12.6) | 10.2 (6.8–14.2) | 0.06 |
| ApoE§ | 3.9 (3.2–4.7) | 3.8 (3.2–4.5) | 0.24 | 3.8 (3.1–4.5) | 3.7 (3.1–4.4) | 0.38 | 4.1 (3.4–4.9) | 4 (3.4–4.8) | 0.62 |
| Lp(a)* | 20 (8–51) | 20 (7–50) | 0.5 | 11 (6–28) | 12 (6–31) | 0.51 | 42 (20–76) | 49 (25–89) | 0.02 |
| FFA§ | 0.61 (0.47–0.77) | 0.62 (0.49–0.79) | 0.41 | 0.63 (0.48–0.79) | 0.63 (0.49–0.79) | 0.74 | 0.59 (0.45–0.74) | 0.62 (0.5–0.76) | 0.18 |
Data represent bivariate associations between eGFR category and each denoted lipid parameter. eGFR categories were further stratified by white and black race. Data reported as median values (IQR). P values analyzed by Wilcoxon Rank Sum test. Abbreviations: TC total cholesterol, HDL-C high density lipoprotein cholesterol, LDL-C low density lipoprotein cholesterol, VLDL-C very low density lipoprotein cholesterol, TG trigylcerides, Lp(a) lipoprotein(a), apoA-I apolipoprotein A-I, apoA-II apolipoprotein A-II, apoB apolipoprotein B, apoC-III apolipoprotein C-III, apoE apolipoprotein E, FFA free fatty acids. *N = 1852, §N = 1439
Associations of Lipid Fractions with eGFR in Multivariable Models
Lp(a) analyses are discussed separately below. Linear regression with eGFR (all values >60 mL/min/1.73 m2) and log-transformed values of lipid fractions demonstrated that eGFR was significantly associated with levels of LDL-C and apoC-III after adjusting for demographic factors (Table 3). Although the association of eGFR with LDL-C lost significance after further adjustment, the associations of eGFR with apoC-III remained highly significant in the fully adjusted model that also accounts for urinary ACR (p = 0.001). The associations between eGFR and TG as well as eGFR and VLDL-C was significant after adjusting for hemoglobin A1c, HOMA-IR, and duration on insulin, in addition to demographic factors, BMI, hypertension, and use of lipid-lowering medications (Table 3) and remained significant in fully adjusted models (TG p = 0.01, VLDL-C p = 0.02). No statistically significant relationship between apoB and eGFR was seen.
Table 3. Multivariable Associations Between eGFR Values and Lipid Parameters.
| Lipid Parameter | Model 1 | Model 2 | Model 3 | Model 4 | ||||
| Beta Coefficient | P Value | Beta Coefficient | P Value | Beta Coefficient | P Value | Beta Coefficient | P Value | |
| TC | 0.029 | 0.28 | 0.010 | 0.70 | −0.024 | 0.34 | −0.020 | 0.42 |
| HDL-C | 0.012 | 0.64 | −0.004 | 0.869 | 0.012 | 0.61 | 0.016 | 0.52 |
| LDL-C | 0.065 | 0.016 | 0.044 | 0.083 | 0.015 | 0.556 | 0.015 | 0.56 |
| VLDL-C | −0.037 | 0.16 | −0.034 | 0.206 | −0.062 | 0.02 | −0.061 | 0.02 |
| TG | −0.036 | 0.17 | −0.024 | 0.342 | −0.068 | 0.009 | −0.066 | 0.01 |
| ApoA-I | 0.026 | 0.36 | 0.016 | 0.569 | 0.039 | 0.18 | 0.047 | 0.11 |
| ApoA-II | 0.012 | 0.70 | 0.028 | 0.359 | 0.035 | 0.27 | 0.040 | 0.21 |
| ApoB | 0.053 | 0.09 | 0.039 | 0.182 | −0.007 | 0.81 | −0.006 | 0.85 |
| ApoC-III | −0.075 | 0.02 | −0.070 | 0.02 | −0.111 | 0.001 | −0.109 | 0.001 |
| ApoE | −0.001 | 0.97 | −0.008 | 0.801 | −0.023 | 0.48 | −0.014 | 0.67 |
| Lp(a) | −0.085 | <0.001 | −0.089 | <0.001 | −0.089 | <0.001 | −0.087 | 0.001 |
| FFA | 0.031 | 0.30 | 0.027 | 0.361 | 0.024 | 0.44 | 0.022 | 0.47 |
Data represent standardized coefficients of change in log-transformed values of listed lipid fractions for every 10 ml/min/1.73 m2 higher eGFR. Linear regression was performed in incremental models with the following co-variates.
Model 1: Age, gender, race.
Model 2: Age, gender, race, BMI, hypertension, lipid-lowering medications (statin, fibrate, niacin).
Model 3: Age, gender, race, BMI, hypertension, lipid-lowering medications, hemoglobin A1c, HOMA-IR, duration on insulin.
Model 4: Age, gender, race, BMI, hypertension, lipid-lowering medications, hemoglobin A1c, HOMA-IR, duration on insulin, urinary ACR.
*Definition of hypertension includes the use of anti-hypertensive medications.
**Statistically significant results are presented in bold.
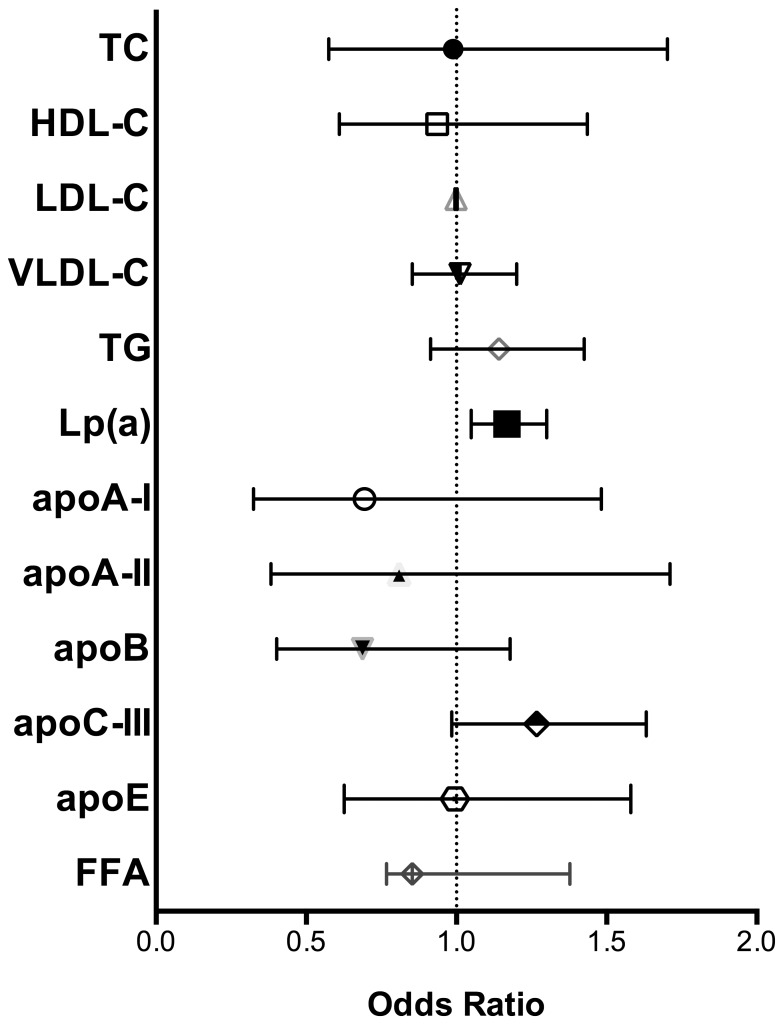
When eGFR as a binary outcome (eGFR>90 vs. 60–90 mL/min/1.73 m2) underwent logistic regression with the log-transformed lipid fractions, associations between eGFR categories and apoB reached significance controlling for demographic factors, metabolic parameters, and use of lipid-lowering medications (Table 4). The association with apoB, however, weakened after further adjustment for glycemic measures and urinary ACR but maintained a trend towards significance (p = 0.17). The trends seen with VLDL-C, TG, and apoC-III when eGFR was treated as a continuous outcome were not observed when eGFR was analyzed by logistic regression using a binary outcome (eGFR>90 vs. 60–90 mL/min/1.73 m2) (Fig. 1).
Table 4. Multivariable Associations Between Lower eGFR Category and Lipid Parameters.
| Lipid Parameter | Model 1 | Model 2 | Model 3 | Model 4 | ||||
| OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | |
| TC | 0.80 (0.50–1.29) | 0.36 | 0.82 (0.49–1.36) | 0.44 | 1.03 (0.60–1.77) | 0.92 | 0.99 (0.58–1.70) | 0.97 |
| HDL-C | 0.86 (0.58–1.28) | 0.47 | 1.01 (0.67–1.52) | 0.97 | 0.96 (0.63–1.48) | 0.87 | 0.94 (0.61–1.44) | 0.76 |
| LDL-C | 1.00 (0.99–1.00) | 0.15 | 1.00 (0.99–1.00) | 0.18 | 1.00 (0.99–1.00) | 0.50 | 1.00 (0.99–1.00) | 0.53 |
| VLDL-C | 1.01 (0.87–1.19) | 0.87 | 0.98 (0.84–1.15) | 0.83 | 1.02 (0.86–1.21) | 0.84 | 1.14 (0.91–1.43) | 0.24 |
| TG | 1.10 (0.90–1.34) | 0.37 | 1.03 (0.84–1.23) | 0.79 | 1.15 (0.92–1.44) | 0.84 | 1.01 (0.85–1.20) | 0.89 |
| ApoA-I | 0.79 (0.39–1.59) | 0.50 | 0.88 (0.43–1.81) | 0.73 | 0.76 (0.36–1.62) | 0.48 | 0.69 (0.32–1.48) | 0.35 |
| ApoA-II | 1.00 (0.50–2.00)0 | 0.99 | 0.88 (0.44–1.78) | 0.73 | 0.85 (0.40–1.79) | 0.67 | 0.81 (0.38–1.71) | 0.58 |
| ApoB | 0.58 (0.36–0.93) | 0.02 | 0.55 (0.33–0.91) | 0.021 | 0.70 (0.41–1.19) | 0.19 | 0.69 (0.40–1.18) | 0.17 |
| ApoC-III | 1.15 (0.91–1.46) | 0.24 | 1.13 (0.89–1.43) | 0.33 | 1.28 (0.99–1.65) | 0.06 | 1.27 (0.98–1.63) | 0.07 |
| ApoE | 0.93 (0.61–1.42) | 0.73 | 0.93 (0.60–1.44) | 0.74 | 1.06 (0.67–1.68) | 0.82 | 0.99 (–.63–1.58) | 0.98 |
| Lp(a) | 1.16 (1.05–1.28) | 0.004 | 1.17 (1.06–1.30) | 0.002 | 1.17 (1.05–1.31) | 0.004 | 1.17 (1.04–1.30) | 0.005 |
| FFA | 1.00 (0.76–1.31) | 0.98 | 0.99 (0.75–1.31) | 0.94 | 1,02 (0.76–1.37) | 0.88 | 1.03 (0.77–1.38) | 0.85 |
Data represent odds of lower eGFR category (mild renal impairment) with log-transformed values of lipid fractions. Logistic regression was performed in incremental models with the following co-variates.
Model 1: Age, gender, race.
Model 2: Age, gender, race, BMI, hypertension, lipid-lowering medications (statin, fibrate, niacin).
Model 3: Age, gender, race, BMI, hypertension, lipid-lowering medications, hemoglobin A1c, HOMA-IR, duration on insulin.
Model 4: Age, gender, race, BMI, hypertension, lipid-lowering medications, hemoglobin A1c, HOMA-IR, duration on insulin, urinary ACR.
*Definition of hypertension includes the use of anti-hypertensive medications.
**Statistically significant results are presented in bold.
Figure 1. Odds of Lower eGFR Category by Lipid Parameters.
Multivariable analysis adjusted for the following co-variates: age, race, gender, body mass index, hypertension (definition includes use of anti-hypertensive medications), use of lipid-lowering medication, hemoglobin A1c, HOMA-IR, duration on insulin, urinary albumin to creatinine ratio. Abbreviations: TC total cholesterol, HDL-C high density lipoprotein cholesterol, LDL-C low density lipoprotein cholesterol, VLDL-C very low density lipoprotein cholesterol, TG trigylcerides, Lp(a) lipoprotein(a), apoA-I apolipoprotein A-I, apoA-II apolipoprotein A-II, apoB apolipoprotein B, apoC-III apolipoprotein C-III, apoE apolipoprotein E, FFA free fatty acids.
Higher Lp(a) Levels Are Associated with Mild GFR Impairment
Across all incremental multivariable models, the lower eGFR group maintained a robust and consistent association with higher plasma Lp(a) levels (OR 1.17, 1.05–1.30, p = 0.005). Thus, the inverse association remained statistically significant even with adjustment for race, glycemic parameters, and urinary ACR (Table 4). Using a cut-point in circulating Lp(a) levels (at 30 mg/dL), values above which had previously been found to be associated with CV disease [36], logistic regression in incremental models again demonstrated a statistically significant and consistent association (e.g., in fully adjusted model OR 1.35, 1.06–1.71, p = 0.013) between mild GFR impairment (eGFR 60–90 mL/min/1.73 m2) and this clinical definition of elevated circulating Lp(a) levels (Table 5). Interaction terms between eGFR and race, gender, hypertension, and urinary ACR in association with Lp(a) were not statistically significant.
Table 5. Association Between Lower eGFR Category and Lp(a)>30 mg/dL.
| Multivariable Model | Odds Ratio (95% CI) | P Value |
| Model 1 | 1.33 (1.06–1.67) | 0.014 |
| Model 2 | 1.34 (1.07–1.69) | 0.012 |
| Model 3 | 1.36 (1.07–1.72) | 0.011 |
| Model 4 | 1.35 (1.06–1.71) | 0.013 |
Data represent odds of lower eGFR category with plasma Lp(a) greater than 30 mg/dL. Logistic regression performed in incremental models with the following co-variates.
Model 1: Age, gender, race.
Model 2: Age, gender, race, BMI, hypertension, lipid-lowering medications (statin, fibrate, niacin).
Model 3: Age, gender, race, BMI, hypertension, lipid-lowering medications, hemoglobin A1c, HOMA-IR, duration on insulin.
Model 4: Age, gender, race, BMI, hypertension, lipid-lowering medications, hemoglobin A1c, HOMA-IR, duration on insulin, urinary ACR.
*Definition of hypertension includes the use of anti-hypertensive medications.
Discussion
In this study of diabetic individuals, we demonstrate that mild GFR impairment is indeed associated with an atherogenic lipid profile, primarily through its strong association with elevated plasma Lp(a) levels. Previous studies with smaller cohorts have shown mixed results in evaluating the correlation between plasma Lp(a) and markers of renal disease, including reduced eGFR and albuminuria [39], [50]. Utilizing a large, well-characterized cohort of individuals with T2DM, our study is among the first to demonstrate a robust association between higher plasma Lp(a) levels and mildly reduced eGFR independent of race, glycemic control, and albuminuria. This significant association was also observed when Lp(a) levels were dichotomized at 30 mg/dL, a clinically relevant cutoff in Lp(a). Thus, Lp(a) levels greater than 30 mg/dL are associated with increased risk of CV disease [36] and in our study are associated with the lower eGFR.
Among diabetic individuals with an eGFR greater than 60 mL/min/1.73 m2, the association between higher plasma Lp(a) and reduced eGFR may have potential implications in the care of T2DM patients with mild GFR impairment. Lp(a) levels are well established to be elevated in moderate to severe CKD patients, [20], [38]–[41] and here we show that they are also elevated in the setting of mild GFR impairment regardless of albuminuria status. Recent studies have identified Lp(a) as an independent genetic and causal risk factor for CV disease[31]–[38] with several studies showing that higher plasma levels of Lp(a) and genetic variation in the LPA gene that raise Lp(a) levels increase the risk of myocardial infarction (MI) in patients with and without established coronary heart disease [31], [37], [38], [51]. Thus, specific therapeutic targeting of Lp(a) is under development for treatment of heart disease. Our findings suggest that elevated Lp(a) levels might contribute even from an early stage of CKD to the higher incidence of CV disease in patients with CKD [52]. Specifically, the association of elevated plasma Lp(a) with eGFR in the 60–90 ml/min/1.73 m2 range independent of albuminuria status suggests that diabetic patients with even mild renal impairment may have more cardiovascular risk than previously thought. This also raises the possibility of targeting of Lp(a) as a preventative strategy for lowering CVD in CKD patients.
Our findings for Lp(a) contradict a previous study that found Lp(a) to be positively associated with albuminuria [39] and separate work that found an association between Lp(a) and albuminuria but not with eGFR in a smaller cohort primarily of non-diabetic patients [50]. In the PDHS cohort, the association between Lp(a) and eGFR in both linear and logistic regression models was consistent and robust to adjustment for urinary ACR. In contrast, the association of Lp(a) with urinary ACR in the PDHS sample did not reach statistical significance in any models (data not shown). Overall, our results indicate that mildly reduced eGFR alone in T2DM patients is associated with higher levels of a this pro-atherogenic lipid moiety and that the sub-population of diabetics with eGFR between 60 and 90 mL/min/1.73 m2 but without albuminuria may warrant further study of their CV disease risk.
Although our study demonstrates an inverse relationship between eGFR and Lp(a), the mechanism behind this association remains unknown. Prior Mendelian randomization studies established causality between CV disease and genetic variations in the LPA gene [31], [37]. However, the causal direction between plasma Lp(a) and renal impairment is unclear. One study showed that plasma Lp(a) levels, which were not lowered by hemodialysis, decreased rapidly in CKD patients after renal transplantation, suggesting a role for the kidney in Lp(a) catabolism [52]. Another human study demonstrated a renovascular arteriovenous difference of −9% in Lp(a) concentrations as well as the presence of apo(a) fragments in urine, supporting the kidney's involvement in Lp(a) 's clearance from circulation [53]. Thus, renal disease per se may lead to increases in circulating Lp(a) and account for our observed association of Lp(a) levels with mild GFR impairment. However, it remains unclear whether Lp(a) also plays a role in the development and progression of renal disease. A prior study of 49 non-diabetic individuals with moderate to severe CKD did not find a statistically significant association between plasma Lp(a) levels and progression of renal disease [54]. However, it utilized a small study sample with a majority of subjects having already moderate renal impairment due to chronic glomerulonephritis; thus these subjects may have had stronger competing risks for CKD progression. A larger Chronic Renal Insufficiency Cohort (CRIC) study also did not find a statistically significant association between Lp(a) levels and CKD progression [55] but again had participants with more severe renal disease than the PDHS subjects. Because these studies focused on populations with different characteristics from the PDHS cohort, they do not necessarily counter the possibility that Lp(a) may play a causal role in early CKD in diabetics, although determination of causality is beyond the scope of our study.
Unlike Lp(a), other lipid fractions we studied did not demonstrate a robust association with mild GFR impairment (eGFR <90 but >60 mL/min/1.73 m2). Although we had hypothesized that elevated plasma levels of TG, VLDL-C, apoB, and apoC-III would be associated with mild GFR impairment, the inverse relationship between eGFR and TG, VLDL, and apoC-III seen on linear regression did not remain statistically significant on logistic regression with mild GFR impairment as an outcome. This finding is consistent with greater power in modeling eGFR as a continuous outcome variable compared to examining eGFR outcomes as collapsed binary variables.
Prior studies have demonstrated that TGRLs and multiple apolipoprotein fractions were associated with CKD, but these studies generally examined populations with lower mean eGFR and higher urinary ACR values than the PDHS sample [20], [25], [26], [29], [30]. Also, their analyses were either not adjusted or did not adjust for hypertension, glycemic control, and insulin resistance. Here we show by linear regression analyses that TGRLs are associated with eGFR in the PDHS sample. This trend could be mediated by increased apoC-III as higher apoC-III levels in the setting of CKD is likely to impair LPL activity and decrease TG and VLDL metabolism. Currently, therapies targeting the apoC-III pathway are being developed [56], and further studies on apoC-III and outcomes in mild CKD are needed.
Our work has several strengths. This study, including a substantial proportion of women and minorities, is the largest with the unique focus on CV biomarkers in a population (mild GFR impairment) that may be under-recognized for increased CV risk. Other studies on Lp(a) in renal disease have primarily included patients on dialysis or with late-stage CKD who already have established increased CV risk and excess all-cause mortality. Our findings for Lp(a) in multivariable analyses were robust, with control for confounding variables of clinical relevance to CKD as well as CV disease. Our study also has some weaknesses. The cross-sectional nature of our study does not allow for the establishment of a causal direction in the associations we found between eGFR and the lipid parameters of interest. Other weaknesses include the use of eGFR rather than measured GFR or cystatin-C, recruitment of patients from a small geographical area, absence of a non-diabetic comparison group, absence of isoform and genotypic data for LPA.
In summary, our data show that in diabetic individuals mild renal impairment has a robust association with elevated Lp(a) levels and also appears to associate with increased apoC-III which ultimately leads to elevated atherogenic TGRLs. Both of these lipid mediators are causal in CV disease and also are promising therapeutic targets currently under development. Whether these lipid pathways represent specific targets for increased risk of CV disease in CKD population remains to be established. Future studies are warranted to assess potential benefit of early preventive interventions even in populations with mild CKD where these early lipid abnormalities may increase later risk of CV events. Finally, genomic studies are required to address whether LPA variants associated with CV disease are also associated with development and progression of CKD in order to establish whether Lp(a) is a causal risk factor for CKD and hence a potential future therapeutic target for reducing renal outcomes as well as CV event.
Supporting Information
Correlation Matrix of All Lipid Parameters. Spearman's correlation coefficient is reported for each lipid parameter with all other corresponding lipid parameters. Coefficients with p<0.05 are bolded. Abbreviations: TC total cholesterol, HDL-C high density lipoprotein cholesterol, LDL-C low density lipoprotein cholesterol, VLDL-C very low density lipoprotein cholesterol, TG trigylcerides, Lp(a) lipoprotein(a), apoA-I apolipoprotein A-I, apoA-II apolipoprotein A-II, apoB apolipoprotein B, apoC-III apolipoprotein C-III, apoE apolipoprotein E, FFA free fatty acids.
(DOCX)
Multivariable Associations Between eGFR Values and Lipid Parameters. Data represent standardized coefficients of change in log-transformed values of listed lipid fractions for every 10 ml/min/1.73 m2 higher eGFR. Linear regression was performed in incremental models with the following co-variates: age, gender, race, BMI, hypertension, lipid-lowering medications, hemoglobin A1c, HOMA-IR, duration on insulin, urinary ACR, and all other lipid parameters found to have significant associations with eGFR (those listed in this table).
(DOCX)
De-identified data from this dataset were used for the analysis presented in this manuscript. The second worksheet of the Excel file contains a key to the binary coding of variables.
(XLS)
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by National Institute of Diabetes and Digestive and Kidney Diseases: T32-DK00700640, JL. K23-DK097201, FPW; National Heart, Lung and Blood Institute: K24-HL107643, MPR; Clinical and Translational Science Award (UL1RR024134) from the National Center for Research Resources and a Diabetes and Endocrine Research Center award (P20-DK 019525) awarded to the University of Pennsylvania. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, et al. (2007) Prevalence of chronic kidney disease in the United States. JAMA 298:2038–2047 10.1001/jama.298.17.2038. [DOI] [PubMed] [Google Scholar]
- 2. Sarnak MJ (2003) Kidney Disease as a Risk Factor for Development of Cardiovascular Disease: A Statement From the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation 108:2154–2169 10.1161/01.CIR.0000095676.90936.80. [DOI] [PubMed] [Google Scholar]
- 3. Manjunath G, Tighiouart H, Ibrahim H, MacLeod B, Salem DN, et al. (2003) Level of kidney function as a risk factor for atherosclerotic cardiovascular outcomes in the community. J Am Coll Cardiol 41:47–55. [DOI] [PubMed] [Google Scholar]
- 4. Go AS, Chertow GM, Fan D, McCulloch CE, Hsu C-Y (2004) Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 351:1296–1305 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 5. Afkarian M, Sachs MC, Kestenbaum B, Hirsch IB, Tuttle KR, et al. (2013) Kidney Disease and Increased Mortality Risk in Type 2 Diabetes. Journal of the American Society of Nephrology 24:302–308 10.1681/ASN.2012070718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Haffner SM, Lehto S, Rönnemaa T, Pyörälä K, Laakso M (1998) Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med 339:229–234 10.1056/NEJM199807233390404. [DOI] [PubMed] [Google Scholar]
- 7. Huang ES, Laiteerapong N, Liu JY, John PM, Moffet HH, et al. (2013) Rates of Complications and Mortality in Older Patients With Diabetes Mellitus. JAMA Intern Med. 10.1001/jamainternmed.2013.12956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fox CS, Coady S, Sorlie PD, D'Agostino RB, Pencina MJ, et al. (2007) Increasing Cardiovascular Disease Burden Due to Diabetes Mellitus: The Framingham Heart Study. Circulation 115:1544–1550 10.1161/CIRCULATIONAHA.106.658948. [DOI] [PubMed] [Google Scholar]
- 9. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, et al. (2014) Heart Disease and Stroke Statistics–2014 Update: A Report From the American Heart Association. Circulation 129:e28–e292 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gaede P, Lund-Andersen H, Parving H-H, Pedersen O (2008) Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med 358:580–591 10.1056/NEJMoa0706245. [DOI] [PubMed] [Google Scholar]
- 11. KDIGO (2014) KDIGO Clinical Practice Guideline for Lipid Management in CKD: summary of recommendation statements and clinical approach to the patient. Kidney Int. 10.1038/ki.2014.31. [DOI] [PubMed] [Google Scholar]
- 12. KDOQI (2007) KDOQI Clinical Practice Guidelines and Clinical Practice Recommendations for Diabetes and Chronic Kidney Disease. Am J Kidney Dis 49:S12–S154 10.1053/j.ajkd.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 13. Joosen IA, Schiphof F, Versteylen MO, Laufer EM, Winkens MH, et al. (2012) Relation between Mild to Moderate Chronic Kidney Disease and Coronary Artery Disease Determined with Coronary CT Angiography. PLoS ONE 7:e47267 10.1371/journal.pone.0047267.t004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dohi T, Miyauchi K, Okazaki S, Yokoyama T, Tamura H, et al. (2011) Long-term impact of mild chronic kidney disease in patients with acute coronary syndrome undergoing percutaneous coronary interventions. Nephrology Dialysis Transplantation 26:2906–2911 10.1093/ndt/gfq820. [DOI] [PubMed] [Google Scholar]
- 15. National Kidney Foundation (2012) KDOQI CLINICAL PRACTICE GUIDELINE FOR DIABETES AND CKD: 2012 UPDATE. YAJKD 60:850–886 10.1053/j.ajkd.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 16. de Boer IH, Astor BC, Kramer H, Palmas W, Rudser K, et al. (2008) Mild elevations of urine albumin excretion are associated with atherogenic lipoprotein abnormalities in the Multi-Ethnic Study of Atheroslcerosis (MESA). Atherosclerosis 197:407–414 10.1016/j.atherosclerosis.2007.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Vaziri ND (2006) Dyslipidemia of chronic renal failure: the nature, mechanisms, and potential consequences. Am J Physiol Renal Physiol 290:F262–F272 10.1152/ajprenal.00099.2005. [DOI] [PubMed] [Google Scholar]
- 18. Keane WF, Tomassini JE, Neff DR (2013) Lipid abnormalities in patients with chronic kidney disease: implications for the pathophysiology of atherosclerosis. J Atheroscler Thromb 20:123–133. [DOI] [PubMed] [Google Scholar]
- 19. Pennell P, Leclercq B, Delahunty MI, Walters BAJ (2006) The utility of non-HDL in managing dyslipidemia of stage 5 chronic kidney disease. Clin Nephrol 66:336–347. [DOI] [PubMed] [Google Scholar]
- 20. Attman PO, Samuelsson O, Alaupovic P (1993) Lipoprotein metabolism and renal failure. YAJKD 21:573–592. [DOI] [PubMed] [Google Scholar]
- 21. Global Lipids Genetics Consortium Willer CJ, Schmidt EM, Sengupta S, Peloso GM, et al. (2013) Discovery and refinement of loci associated with lipid levels. Nat Genet 45:1274–1283 10.1038/ng.2797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nakamura T, Obata J-E, Hirano M, Kitta Y, Fujioka D, et al. (2011) Atherosclerosis. Atherosclerosis 218:163–167 10.1016/j.atherosclerosis.2011.04.040. [DOI] [PubMed] [Google Scholar]
- 23. Lamprea-Montealegre JA, McClelland RL, Astor BC, Matsushita K, Shlipak M, et al. (2013) Chronic Kidney Disease, Plasma Lipoproteins, and Coronary Artery Calcium Incidence: The Multi-Ethnic Study of Atherosclerosis. Arteriosclerosis, Thrombosis, and Vascular Biology 33:652–658 10.1161/ATVBAHA.112.300624. [DOI] [PubMed] [Google Scholar]
- 24. Attman P-O, Samuelsson O (2009) Dyslipidemia of kidney disease. Current Opinion in Lipidology 20:293–299 10.1097/MOL.0b013e32832dd832. [DOI] [PubMed] [Google Scholar]
- 25. Ooi EMM, Chan DT, Watts GF, Chan DC, Ng TWK, et al. (2011) Plasma apolipoprotein C-III metabolism in patients with chronic kidney disease. The Journal of Lipid Research 52:794–800 10.1194/jlr.M011163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wang X, Belani S, Coyne DW, Fabbrini E, Reeds DN, et al. (2012) Very Low Density Lipoprotein Metabolism in Patients with Chronic Kidney Disease. Cardiorenal Med 2:57–65 10.1159/000335509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Chan DT, Dogra GK, Irish AB, Ooi EM, Barrett PH, et al. (2009) Chronic kidney disease delays VLDL-apoB-100 particle catabolism: potential role of apolipoprotein C-III. The Journal of Lipid Research 50:2524–2531 10.1194/jlr.P900003-JLR200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Holzmann MJ, Jungner I, Walldius G, Ivert T, Nordqvist T, et al. (2012) Dyslipidemia is a strong predictor of myocardial infarction in subjects with chronic kidney disease. Ann Med 44:262–270 10.3109/07853890.2010.532153 [DOI] [PubMed] [Google Scholar]
- 29. Attman PO, Knight-Gibson C, Tavella M, Samuelsson O, Alaupovic P (1998) The compositional abnormalities of lipoproteins in diabetic renal failure. Nephrol Dial Transplant 13:2833–2841. [DOI] [PubMed] [Google Scholar]
- 30. Attman PO, Samuelsson O, Alaupovic P (2011) The effect of decreasing renal function on lipoprotein profiles. Nephrology Dialysis Transplantation 26:2572–2575 10.1093/ndt/gfq762 [DOI] [PubMed] [Google Scholar]
- 31. Clarke R, Peden JF, Hopewell JC, Kyriakou T, Goel A, et al. (2009) Genetic variants associated with Lp(a) lipoprotein level and coronary disease. N Engl J Med 361:2518–2528 10.1056/NEJMoa0902604 [DOI] [PubMed] [Google Scholar]
- 32. Emerging Risk Factors Collaboration, Erqou S, Kaptoge S, Perry PL, Di Angelantonio E. (2009) Lipoprotein(a) concentration and the risk of coronary heart disease, stroke, and nonvascular mortality. JAMA 302:412–423 10.1001/jama.2009.1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Virani SS, Brautbar A, Davis BC, Nambi V, Hoogeveen RC, et al. (2012) Associations Between Lipoprotein(a) Levels and Cardiovascular Outcomes in Black and White Subjects: The Atherosclerosis Risk in Communities (ARIC) Study. Circulation 125:241–249 10.1161/CIRCULATIONAHA.111.045120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tsimikas S, Hall JL (2012) Lipoprotein(a) as a Potential CausalGenetic Risk Factor of Cardiovascular Disease. J Am Coll Cardiol 60:716–721 10.1016/j.jacc.2012.04.038. [DOI] [PubMed] [Google Scholar]
- 35. Anderson JL, Knight S, May HT, Home BD, Bair TL, et al. (2013) Validation and Quanti. The American Journal of Cardiology 112:799–804 10.1016/j.amjcard.2013.05.009. [DOI] [PubMed] [Google Scholar]
- 36. Jacobson TA (2013) Lipoprotein(a), Cardiovascular Disease, and Contemporary Management. Mayo Clinic Proceedings 88:1294–1311 10.1016/j.mayocp.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 37. Kamstrup PR, Tybjaerg-Hansen A, Steffensen R, Nordestgaard BG (2009) Genetically elevated lipoprotein(a) and increased risk of myocardial infarction. JAMA 301:2331–2339 10.1001/jama.2009.801. [DOI] [PubMed] [Google Scholar]
- 38. Kronenberg F, Utermann G (2012) Lipoprotein(a): resurrected by genetics. Journal of Internal Medicine 273:6–30 10.1111/j.1365-2796.2012.02592.x. [DOI] [PubMed] [Google Scholar]
- 39. Kronenberg F, Kuen E, Ritz E, Junker R, König P, et al. (2000) Lipoprotein(a) serum concentrations and apolipoprotein(a) phenotypes in mild and moderate renal failure. J Am Soc Nephrol 11:105–115. [DOI] [PubMed] [Google Scholar]
- 40.O'Donoghue ML, Morrow DA, Tsimikas S, Sloan S, Ren AF, et al. (2013) Accepted Manuscript. J Am Coll Cardiol: 1–43. doi:10.1016/j.jacc.2013.09.042.
- 41. Sechi LA, Zingaro L, Catena C, Perin A, De Marchi S, et al. (1999) Lipoprotein(a) and apolipoprotein(a) isoforms and proteinuria in patients with moderate renal failure. Kidney Int 56:1049–1057 10.1046/j.1523-1755.1999.00621.x. [DOI] [PubMed] [Google Scholar]
- 42. Reilly MP, Iqbal N, Schutta M, Wolfe ML, Scally M, et al. (2004) Plasma leptin levels are associated with coronary atherosclerosis in type 2 diabetes. Journal of Clinical Endocrinology & Metabolism 89:3872–3878 10.1210/jc.2003-031676 [DOI] [PubMed] [Google Scholar]
- 43. Lilly SM, Qasim AN, Mulvey CK, Churchill TW, Reilly MP, et al. (2013) Non-compressible arterial disease and the risk of coronary calcification in type-2 diabetes. Atherosclerosis 230:17–22 10.1016/j.atherosclerosis.2013.06.004 [DOI] [PubMed] [Google Scholar]
- 44. Qasim AN, Rafeek H, Rasania SP, Churchill TW, Yang W, et al. (2013) Atherosclerosis. Atherosclerosis 226:419–424 10.1016/j.atherosclerosis.2012.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Martin SS, Qasim AN, Wolfe M, Clair CS, Schwartz S, et al. (2011) Comparison of High-Density Lipoprotein Cholesterol to Apolipoprotein A-I and A-II to Predict Coronary Calcium and the Effect of Insulin Resistance. The American Journal of Cardiology 107:393–398 10.1016/j.amjcard.2010.09.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Mulvey CK, McNeill AM, Girman CJ, Churchill TW, Terembula K, et al. (2014) Differential Associations of Oral Glucose Tolerance Test-Derived Measures of Insulin Sensitivity and Pancreatic β-Cell Function With Coronary Artery Calcification and Microalbuminuria in Type 2 Diabetes. Diabetes Care 37:124–133 10.2337/dc12-1880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, et al. (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, et al. (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419. [DOI] [PubMed] [Google Scholar]
- 49. Willey JZ, Rodriguez CJ, Carlino RF, Moon YP, Paik MC, et al. (2011) Race-ethnic differences in the association between lipid profile components and risk of myocardial infarction: The Northern Manhattan Study. American Heart Journal 161:886–892 10.1016/j.ahj.2011.01.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Uhlig K, Wang S-R, Beck GJ, Kusek JW, Marcovina SM, et al. (2005) Factors associated with lipoprotein(a) in chronic kidney disease. American Journal of Kidney Diseases 45:28–38 10.1053/j.ajkd.2004.08.043 [DOI] [PubMed] [Google Scholar]
- 51.Elosua R, Sayols-Baixeras S, Lluís-Ganella C, Lucas G (2014) Pathogenesis of coronary artery disease: focus on genetic risk factors and identification of genetic variants. TACG: 15. doi:10.2147/TACG.S35301. [DOI] [PMC free article] [PubMed]
- 52. Rosas S, Joffe M, Wolfe M, Brayman K, Rader DJ (2008) Effects of Renal Replacement Therapy on Plasma Lipoprotein(a) Levels. Am J Nephrol 28:361–365 10.1159/000112225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Kronenberg F, Trenkwalder E, Lingenhel A, Friedrich G, Lhotta K, et al. (1997) Renovascular arteriovenous differences in Lp[a] plasma concentrations suggest removal of Lp[a] from the renal circulation. The Journal of Lipid Research 38:1755–1763. [PubMed] [Google Scholar]
- 54. Samuelsson O, Attman PO, Knight-Gibson C, Larsson R, Mulec H, et al. (1996) Plasma levels of lipoprotein (a) do not predict progression of human chronic renal failure. Nephrol Dial Transplant 11:2237–2243. [DOI] [PubMed] [Google Scholar]
- 55.Rahman M, Yang W, Akkina S, Alper A, Anderson AH, et al. (2014) Relation of Serum Lipids and Lipoproteins with Progression of CKD: The CRIC Study. Clinical Journal of the American Society of Nephrology. doi:10.2215/CJN.09320913. [DOI] [PMC free article] [PubMed]
- 56. Chan DC, Pang J, Romic G, Watts GF (2013) Postprandial Hypertriglyceridemia and Cardiovascular Disease: Current and Future Therapies. Curr Atheroscler Rep 15:309 10.1007/s11883-013-0309-9 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Correlation Matrix of All Lipid Parameters. Spearman's correlation coefficient is reported for each lipid parameter with all other corresponding lipid parameters. Coefficients with p<0.05 are bolded. Abbreviations: TC total cholesterol, HDL-C high density lipoprotein cholesterol, LDL-C low density lipoprotein cholesterol, VLDL-C very low density lipoprotein cholesterol, TG trigylcerides, Lp(a) lipoprotein(a), apoA-I apolipoprotein A-I, apoA-II apolipoprotein A-II, apoB apolipoprotein B, apoC-III apolipoprotein C-III, apoE apolipoprotein E, FFA free fatty acids.
(DOCX)
Multivariable Associations Between eGFR Values and Lipid Parameters. Data represent standardized coefficients of change in log-transformed values of listed lipid fractions for every 10 ml/min/1.73 m2 higher eGFR. Linear regression was performed in incremental models with the following co-variates: age, gender, race, BMI, hypertension, lipid-lowering medications, hemoglobin A1c, HOMA-IR, duration on insulin, urinary ACR, and all other lipid parameters found to have significant associations with eGFR (those listed in this table).
(DOCX)
De-identified data from this dataset were used for the analysis presented in this manuscript. The second worksheet of the Excel file contains a key to the binary coding of variables.
(XLS)
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.