Abstract
Depression is common among patients with breast cancer (BC) and their spouses. The diagnosis of BC often results in negative cognitive processes, such as appraisals of harm/loss, intrusive thoughts, and depressive rumination, all of which contribute to the occurrence of depression in both the patient and spouse. The present research is a cross-sectional exploration of the mediating role of depressive rumination in the relationships of intrusive thoughts and appraisal of harm/loss with depression, in a sample of 56 BC patients and their partners. We hypothesized that depressive rumination would mediate the relationships between cognitive processes and depression in both BC patient and their partners. Participants completed self-report measures of depressive symptoms, depressive rumination, cognitive appraisals, and intrusive thoughts. Path analyses using hierarchical linear regression were conducted to assess the relationships among variables. Results indicated that for BC patients, harm/loss appraisals and intrusive thoughts had direct effects on depression; only harm/loss appraisals had indirect effects through depressive rumination. For partners, both harm/loss appraisal and intrusive thoughts had direct effects on depression, and both had indirect effects through depressive rumination. Dyadic analysis showed no relation of partner cognitive variables with patient depression or patient cognitive variables with partner depression. Findings show that the perseverative practice of dwelling on these negative thoughts of loss and harm relates to depressive symptoms. Rumination may act as one possible mechanism by which intrusive thoughts and harm/loss appraisals lead to depressive symptoms.
Introduction
According to the National Cancer Institute, 15-25% of cancer patients experience depression (NCI, 2013). For patients with breast cancer, the rates of depression vary widely ranging from 15-30% depending on the method of assessment (Fann, Thomas-Rich, Katon, Cowley, Pepping, et al 2007). When lower levels of depression are included, estimates range from 25-65% (Reich, Lesur, & Perdrizet-Chevalier, 2008). Additionally, 32% of husbands/romantic partners of BC patients report depressive symptoms and mood disturbance (Milbury & Badr, 2012), and comparisons of husbands of BC patient to husbands of healthy women have yielded rates of 30% compared to 9 % respectively (Bigatti, Wagner, Lydon-Lam, Steiner, & Miller, 2011). Depression in BC has been associated with decreased efficacy of treatment and increased morbidity as well as poor quality of life (Fann et al, 2007; Reich et al, 2008). In the partners of patients, depression has been associated with distancing and avoidance behaviors (Bigatti, Brown, Steiner, & Miller, 2011), which could negatively impact the patient. Thus, it is important to examine the factors that contribute to the onset and maintenance of depressive symptoms in both the patient and the spouse.
Cognitive Correlates of Depression
The role of cognitions in the development and maintenance of depressive symptoms has been recognized for over 30 years, and cognitive based therapies (cognitive therapy and cognitive behavioral therapy) are considered to be the gold standards of evidence based treatment for depression (Butler, Chapman, Forman, & Beck, 2006; Wampold, Minami, Baskin, & Tierney, 2002). Negative intrusive thoughts, or negative thoughts that spontaneously come into one’s awareness, are one type of cognition that appears to be related to depression. Intrusive thoughts of past negative events are common in those with depression (Starr & Moulds, 2006). In the case of cancer, individuals may experience intrusive negative thoughts regarding what they may have done differently in order to prevent the disease or of what they have lost. Also common are intrusive thoughts about the damage that has been done in regard to both physical functioning and the emotional toll of coping with cancer. Whitaker and colleagues (2009) found that 48% of a sample of anxious cancer patient experienced frequent, uncontrollable intrusive thoughts. Furthermore, these researchers found that there was a significant relationship between a negative appraisal of these thoughts and depression severity (Whitacker, Watson, & Brewin, 2009). Both Starr and Moulds (2006) and Whitacker and colleagues (2009) explain the distinction between intrusive thoughts and the appraisals of the thought in question; intrusive thought can be related to numerous experiences and is not always negatively valenced; thus the interpretation or appraisal of the thought is separate from the appearance of the thought itself.
Breast cancer often elicits negative appraisals of threat (Gallagher, Parle, & Caims, 2002) or of harm/loss (Bjorck, Hopp, & Jones, 1999). Harm/loss appraisals in particular, which focus on the damage that has already been caused by the cancer, are predictive of depression in breast cancer patients (Bigatti, Steiner, & Miller, 2012). Intrusive negative thoughts in general, as well as the negative appraisal of loss, both contribute to the experience of depression in cancer patients; however, there appears to be a third less studied cognitive factor, depressive rumination, that may play an important role as well.
Depressive rumination is “the process of thinking perseveratively about one’s feelings and problems” (Nolen-Hoeksema, Wisco, & Lyubomirsky, 2008 p 400). It is possible that a thought may originate as an unwanted intrusive thought; however the process of attending to this thought repeatedly is what is defined as rumination. Rumination is predictive of the onset of depressive symptoms (Hong, 2007; Nolen-Hoeksema et al, 2008) even after controlling for other negative cognitive styles (Nolen-Hoeksema, Parker, & Larson, 1994; Spasojevic & Alloy, 2001). The link between rumination and depression has been noted in physically healthy populations (Gilbert, Cheung, Irons, & McEwan, 2005; Michl, McLaughlin, Shepard, & Nolen-Hoeksema, 2013). Within the realm of cancer, rumination on intrusive negative thoughts about cancer has been associated with greater distress (Morris & Shakespeare-Finch, 2011).
Depressive rumination may mediate the relationship between the cognition and depression. Although previous research has addressed the role of rumination in the development of depressive symptoms (Nolen-Hoeksema et al, 2008; Papageorgiou & Wells, 2003 Papageorgiou & Siegle, 2003), few if any have looked at its relationship to intrusive thoughts or negative appraisals among those facing cancer. It may be that intrusive thoughts and harm/loss appraisals exert their influence on mood either completely, or more strongly, through ruminative thinking. It is worth noting that although all three of these cognitive constructs are thought to be related to one another, the current literature views them as related but distinct cognitive experiences (Smith & Alloy, 2009). The present study explored the relationships among depression, depressive rumination, intrusive thoughts, and appraisal of harm/loss in a sample of breast cancer patients and their partners. We hypothesized that both intrusive thought and appraisals of harm/loss would have direct and indirect effects, through depressive rumination, on the experience of depressive symptoms in both BC patient and their partners.
Method
Participants
Participants were 56 women diagnosed with BC and their partners who were participating in a study examining the ways in which couples cope with BC. Participants were recruited from a sample of BC patients undergoing treatment at a tertiary Midwestern Cancer Center. Criteria for eligibility included a) a breast cancer diagnosis, b) current chemotherapy or biological treatment, c) married or in living together in a romantic relationship, based on patient report, d) the romantic partner willing to participate in the study, and e) patient and partner able to read and write in English.
Procedures
The present research was conducted with approval from the Indiana University Institutional Review Board in accordance with the university’s requirements for appropriate human subjects research. Patients were approached by research assistants while attending an oncology appointment for BC treatment. Patients who met study criteria were provided with detailed information about the study. The spouse was often present during the appointment and consented along with the patient. Otherwise, the patient was encouraged to consult with her partner about joint participation and the research assistant obtained the couple’s contact information for follow-up regarding participation interest. Following initial expression of interest, the oncologist confirmed that the patient was medically appropriate for study participation. Once approval was received from the oncologist, the couple was contacted to confirm the interest and couples were mailed survey packets. Each assessment took approximately 60 minutes to complete. Participants were asked to complete the measures individually and to refrain from discussing the surveys until both had separately returned the packets. Participants who failed to return their packets within 2 weeks received reminder phone calls.
Of 112 couples approached, 21 refused to participate (18.75%). Health concerns, other time commitments/responsibilities, and lack of interest were the most common reasons for refusal. Assessment packets were mailed to 91 couples who were eligible and consented to participate. Of these, 26 couples (28.57%) did not return packets. There were 8 dyads where either the patient or the partner did not return the packets, and these were excluded from analyses as well. Following this, the dyad participation rate was 62.64% (n = 57 of the 91 who initially agreed to participate). Participants with complete data did not differ from those with missing data on any clinical or demographic variables. These procedures for recruiting family members of cancer patients are regularly used in psycho-oncology research and typically yield similar or lower percentages of participation (Manne, 1999; Manne & Glassman, 2000).
Measures
All measures were administered to both patients and partners. Scales were adapted to refer to “your cancer” or “your partner’s cancer” depending on the individual assessed.
Participant characteristics
A demographic questionnaire was created specifically for this study. This measure assessed participants’ characteristics including age, income, education, employment status, duration of partnership, and view of current health (1 = “poor” to 5 “excellent”). Disease status (i.e. stage and recurrent or original diagnosis) and treatment variables were obtained via medical chart review conducted after the receipt of both of the assessment packets and the signed informed consent.
Depressive symptoms
Depressive symptoms were measured with the Center for Epidemiologic Studies Depression Scale (CES-D, Radloff, 1977). This 20-item self-report instrument has reliability at α = .88 (Radloff, 1977). Importantly, the CES-D has proven reliable when administered to a breast cancer populations, with α = .89 (Hann, Winter, & Jacobsen, 1999). Validity has been established in breast cancer patients also, with breast cancer patients reporting significantly more depressive symptomology than healthy controls as well as increasing symptomology over time compared to no changes for controls (Hann et al., 1999).
Depressive rumination
The Ruminative Responses Scale (Nolen-Hoeksema, 1991) was used to assess depressive rumination. The scale was preceded by the statement It is normal to feel down or sad to a certain degree in response to the diagnosis and treatment of breast cancer in you or someone close to you to encourage participants to reflect upon depressive experiences related to cancer. The scale begins with instructions that ask respondents to “…read each of the items below and indicate whether you never, sometimes, often or always think or do each one when you feel down, sad, or depressed. Please indicate what you generally do, not what you think you should do” followed by 22 items such as “think about a recent situation, wishing it had gone better”, which are rated on a Likert scale from 0-3. Scores are calculated by summing the responses on all 22 items, and higher scores indicate greater degrees of rumination. The scale has strong psychometric properties, with Chronbach alpha scores at or around .90 suggesting good reliability, and significant correlations between ruminative responses and depressed mood suggesting adequate validity (Nolen-Hoeksema et al, 1994).
Intrusive thoughts
The Impact of Events Scale (Horowitz, Wilner, & Alvarez, 1979) was used to measure intrusive thoughts and avoidance using 15 items; 7 of the 15 items are specific to intrusive events. Responses are rated on a 4-point Likert scale which ranges from 0-5. Higher scores are indicative of greater distress. Thus scores for intrusive thinking can range from 0-35. The present study only examined the intrusive thoughts subscale due to its theoretical relevance. Horowitz et al. (1979) found good internal consistency (α = .78) and test-retests reliability (r = .89) for this subscale. A review of 23 studies that evaluated the psychometric properties of the IES reported a mean α = .86 on the Intrusion scale and strong support for content, construct, convergent and clinical validity of the IES (Sundin & Horowitz, 2002). A study of the psychometric properties of the IES in a cancer population further supports reliability (α = .77 for Intrusion). Validity was demonstrated by significant correlations between intrusion and anxiety (r = .64) as well as depression (r = .49) (Mystakidou, Tsilika, Parpa, Galanos, & Vlahos, 2007).
Appraisals
The Cognitive Appraisal of Health Scale (CAHS; Kessler, 1998) was used to assess the primary appraisals of threat, harm/loss, challenge, and benign/irrelevant with regards to the participants’ cancer (patient’s cancer for the partners). The scale consists of 28 items which are rated on a 5-point Likert scale ranging from 1-5 according to their agreement with each item; 8 items comprise the harm/loss subscale. Reliability estimates range from α = .76 to α = .88 (Kessler, 1998). Concurrent validity was demonstrated through clinically relevant differences in appraisals over time, with time since diagnosis positively correlating with benign and challenge appraisals and negatively correlating with harm/loss and threat appraisals (Kessler, 1998). In the present study only Harm/Loss appraisals were examined because they are the ones theoretically relevant to rumination. Items for this subscale were summed. Higher scores mean higher belief that the cancer has resulted in harm or loss to the individual.
Results
Data Analysis
Correlations were run to assess the relationships between variables. A path analysis using hierarchical linear regression was used to determine the direct and indirect effects, through depressive rumination, of intrusive thoughts and harm/loss appraisals on reported depressive symptoms. Separate analyses were conducted for patients and partners. Additional exploratory path analyses were conducted to examine the role of partner variables on patient outcomes and vice versa.
Participant Characteristics
The mean age for patients in this sample was 51.9 years (SD = 12.19). The majority of patients self-identified as non-Hispanic white (98.2%), the remaining 1.8% identified as “other”. Most patients had completed college (54.4%), and 61.4% were not currently employed. The mean age for partners was 52.96 years (SD = 12.15), and all partners identified as non-Hispanic white. The majority of partners were college educated (57.9%) and employed full time (63.2%). Of note, one dyad consisted of a same-sex couple. Information regarding the illness characteristics and breast cancer experience of the patients are available in Table 1.
Table 1.
Health Characteristics of Patients and Partners
| Patient Frequency (%) |
Partner Frequency (%) |
|
|---|---|---|
| Stage | ||
| 1 | 1.8 | --- |
| 2 | 5.3 | --- |
| 3 | 21.1 | --- |
| 4 | 71.9 | --- |
| Occurrence | ||
| First | 31.6 | --- |
| Recurrence | 68.4 | --- |
| Treatment(s) | ||
| Lumpectomy | 19.3 | --- |
| Radiation therapy | 24.6 | --- |
| Chemotherapy | 31.6 | --- |
| Hormone therapy | 3.5 | --- |
| Mastectomy | 21.1 | --- |
| Health Status | ||
| Poor | 3.4 | 1.7 |
| Fair | 15.8 | 8.8 |
| Good | 49.2 | 43.9 |
| Very Good | 21.1 | 29.8 |
| Excellent | 10.5 | 15.8 |
In terms of psychological variables, as a group the patients’ mean score for depressive symptoms was 10.15 (SD =6.85); 19.2% of the sample scored above the recommended cutoff for “significant depressive symptomology” (Radloff, 1977). For the spouses, the mean score for depressive symptoms was 12.21 (SD = 8.97); 35% scored above the recommended cutoff. Among the patient group, the mean for depressive rumination was 12.21 (SD = 8.19), and the mean for the spouses was 11.39 (SD = 8.28). The mean scores on the measure of harm/loss appraisals were 21.95 (SD = 8.19) for patients and 20.79 (SD = 5.59) for spouses. The mean score on the measure of intrusive thoughts for patients was 12.15 (SD = 8.46) and 11.35 (SD = 8.11) for spouses.
Differences in Depressive Rumination Based on Health Variables
Exploratory analyses were conducted to examine patterns in depressive rumination in both patients and partners based on health variables (recurrence, cancer-stage, and self-rated health status). For patients, there were no significant differences in rumination based on cancer recurrence, F(1, 56) = 0.06, p = 0.81, cancer stage, F(2, 55) = 1.79, p = 0.18, or self-rated health status, F(4, 56) = 1.00, p = 0.42. Of note, only one patient identified as having stage 1 cancer, and thus she was not included in the group comparisons for stage. For partners, there were no significant differences in rumination based on their wives’ cancer recurrence, F(1, 55) = 0.39, p = 0.54, or cancer stage, F(2, 54) = 2.46, p = 0.10.
Descriptive Analyses
Correlations were conducted to examine the relationships between depression, depressive rumination, intrusive thoughts, and appraisal of harm/loss. Both patients and partners exhibited the same pattern of relationships between variables. Specifically, moderate positive relationships were observed between all cognitive variables (please refer to Table 2). Interestingly, none of the patient variables were associated with the partner variables.
Table 2.
Correlations between Variables of Interest
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1. Patient Depression | 1.00 | |||||||
| 2. Patient Depressive Rumination | .613** | 1.00 | ||||||
| 3. Patient Intrusive Thoughts | .557** | .334* | 1.00 | |||||
| 4. Patient Harm/loss Appraisal | .601** | .509** | .440** | 1.00 | ||||
| 5. Spouse Depression | .026 | −.042 | .103 | .111 | 1.00 | |||
| 6. Spouse Depressive Rumination | .081 | .012 | .091 | .155 | .657** | 1.00 | ||
| 7. Spouse Intrusive Thoughts | −.35 | −.223 | .137 | −.046 | .597** | .539** | 1.00 | |
| 8. Spouse Harm/loss Appraisal | .117 | .046 | −.032 | .212 | .557** | .543** | .374** | 1.00 |
Correlation is significant at the 0.01 level (2-tailed).
Correlation is significant at the 0.05 level (2-tailed).
Main Analyses
Path analysis for patients
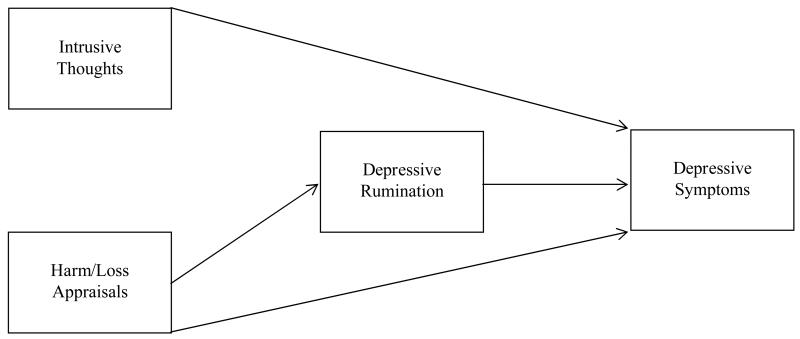
In a first regression, patient depressive rumination was regressed on patient intrusive thoughts and patient harm/loss appraisal. The regression was significant, F(2,54) = 10.197, p < .001, with 27.4% of the variance accounted for. Only harm/loss appraisal entered the regression equation (β = .449, p = .001). In a second regression, patient depression was regressed on patient intrusive thoughts and patient harm/loss in a first step, and patient depressive rumination in a second step. The first step was significant, F(2,54) = 23.732, p < .001, with 46.8% of the variance accounted for. Both harm/loss appraisal (β = .442, p < .001), and intrusive thoughts (β = .363, p = .002) entered the regression equation. The second step was also significant, F(1,53) = 11.946, p = .001, with 54.1% of the variance accounted for. Harm/loss appraisal (β = .277, p = .016), intrusive thoughts (β = .313, p = .003), and depressive rumination (β = .367, p = .001) entered the regression equation. Figure 1 shows these relationships and the effect coefficients. Intrusive thoughts, with only direct effects, has a coefficient of β = .313; harm/loss appraisals, with direct and indirect effects, has a total coefficient of β = .442.
Figure 1.
Path Analysis for Patient Variables
Path analysis for partners
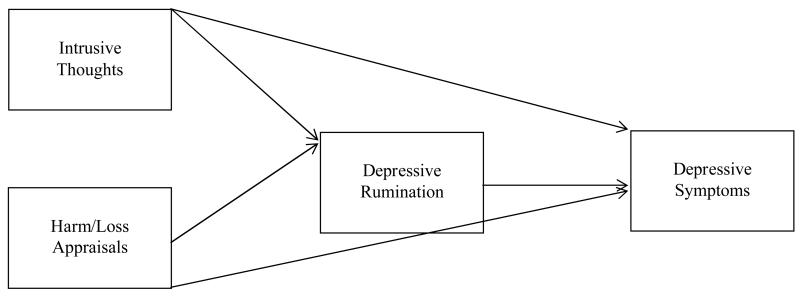
In a first regression, partner depressive rumination was regressed on partner intrusive thoughts and partner harm/loss appraisal. The regression was significant, F(2,53) = 19.277, p < .001, with 42.1% of the variance accounted for. Both harm/loss appraisal (β = .392, p = .001) and intrusive thoughts (β = .386, p = .001) entered the regression equation. In a second regression, partner depression was regressed on partner intrusive thoughts and partner harm/loss in a first step, and partner depressive rumination in a second step. The first step was significant, F(2,53) = 25.993, p < .001, with 47.6% of the variance accounted for. Both harm/loss appraisal (β = .404, p < .001), and intrusive thoughts (β = .439, p < .001) entered the regression equation. The second step was also significant, F(1,52) = 8.306, p = .006, with 54.0% of the variance accounted for. Harm/loss appraisal (β = .268, p = .018), intrusive thoughts (β = .306, p = .007), and depressive rumination (β = .347, p = .006) entered the regression equation. Figure 2 shows these relationships and the effect coefficients. With direct and indirect effects, intrusive thoughts has a total coefficient of β = .440 and harm/loss appraisals has a coefficient of β = .404.
Figure 2.
Path Analysis for Partner Variables
Dyadic analyses
The path analyses were rerun including the partner variables in the patient model and the patient variables in the partner model. Specifically, in the first regressions, in a second step, the intrusive thoughts and harm/loss appraisals of the other were included as predictors of depressive rumination. In the second regression, the harm/loss appraisal, intrusive thoughts, and depressive rumination of the other were included in the first step. None of the partner variables entered the patient regressions and none of the patient variables entered the partner regressions (p > .05).
Discussion
The present study sought to evaluate intrusive thoughts and harm/loss appraisals as cognitive factors associated with the development and maintenance of depressive symptoms in women with breast cancer and their spouses, and to determine whether these cognitive factors exert their influence on depression through depressive rumination. Specifically, we hypothesized that depressive rumination would act as a mediator in the relationships between intrusive thoughts and harm/loss appraisals as predictors and depression as the outcome.
As a whole, our findings support these hypotheses. The results of the path analysis for patients suggested direct effects of harm/loss appraisal on both depressive rumination and depression, as well as indirect effects on depression through depressive rumination (see Figure 1). However, intrusive thought appeared to only have direct, independent effects on depression. The pattern of relationships for spouses fully supported our hypothesis; intrusive thinking and harm/loss appraisals had both direct effects on depression and depressive rumination, as well as indirect effects on depression via depressive rumination (see Figure 2).
Rumination may act as one possible mechanism by which intrusive thoughts and harm/loss appraisals lead to depressive symptoms. Breast cancer patients and their partners may engage in rumination when they are confronted with harm/loss appraisal or intrusive thoughts regarding the breast cancer experience. Given the cross-sectional nature of our study, it is also possible individuals who are depressed engaged in depressive rumination which leads them to recall intrusive thoughts and appraisals of harm and loss. In one study, participants with PTSD reported that rumination served both as a trigger for intrusive thoughts and a way to cope with intrusive thoughts (Michael, Halligan, Clark & Ehlers, 2007), highlighting the complicated interaction between these two forms of repetitive thought. More than likely, given the extant literature, this is a cyclical process and no matter where it started, the rumination perpetuates the relationships observed. Nolen-Hoeksema and colleagues (2008) referred to rumination as a perpetuating factor of depressive symptoms; they asserted that although rumination is a strong independent predictor of depression onset, rumination also has an effect on cognitive styles (such as harm/loss appraisals) to predict the duration and course of depression, This highlights rumination as a valid target of interventions to reduce depressive symptoms in breast cancer patients and spouses.
Because intrusive thoughts, harm/loss appraisals and rumination are all cognitive processes, they may be amenable to similar cognitive interventions. Several studies document beneficial effects of cognitive trainings to reduce these types of thinking and depressive symptoms in dysphoric and depressed patients. Patient interventions in these studies teach memory-specificity (Raes, Williams & Hermans, 2009), active suppression (Joormann, Hertel, LeMoult, & Gotlieb, 2009), positive reappraisal (Troy, Shallcross, Davis & Mauss, 2013), cognitive control (Siegle, Ghinassi, & Thase, 2007), and to be less generalized in their thinking (Watkins, Baeyens, & Read, 2009).
It is important for health care providers to assess and monitor the strategies that breast cancer patients and their partners use to manage the negative emotions and stress associated with cancer. Breast cancer patients and spouses who engage in negative intrusive thinking and appraisals of harm/loss, and allow them to become ruminative processes, may ultimately experience greater stress and depression, which has been linked to worse cancer related outcomes (Fann et al, 2007; Reich et al, 2008), and is related to poorer marital relationships (Bigatti et al, 2011).
Additionally, there is a growing body of literature supporting the use of acceptance and mindfulness based interventions to address various cognitive processes associated with increased depression and various other forms of emotional suffering (Hofmann, Sawyer, Witt, & Oh, 2010). One such study conducted among female, post-treatment cancer survivors found that Mindfulness-Based Stress Reduction Therapy increased attentiveness and reduced ruminative thinking (Campbell, Labelle, Bacon, Faris, & Carlson, 2012). Mindfulness-Based Cognitive Therapy, a combination of mindfulness and cognitive behavioral therapy techniques, may lead to increased cognitive reappraisal ability than cognitive therapies alone (Troy et al., 2013). Further research is needed to identify effective interventions for effectively coping with negative and ruminative thoughts and depression in a cancer-specific context, however, as the literature is very limited.
Our exploratory dyadic analyses examining the impact of partner cognitive factors on patient depressive symptoms, and the converse, yielded non-significant relationships among variables. Intrusive thinking, cognitive appraisals, and rumination are all private cognitive experiences that may not be explicitly shared with one’s partner. Thus, unless these cognitive processes were spoken aloud to the partner, patients and partners may not be aware of their presence in the other. Assisting patients and spouses in sharing their concerns may be particularly important in a population prone to protective buffering. Langer, Rudd, and Syrjala (2007) found that spouses modulate both their facial expressions and the positivity of their words when the patient is present versus not present and that buffering of this sort was negatively associated with the marital satisfaction reported by each. It may be this type of protective behavior that resulted in our findings of no relationships between patient and spouse variables. Research suggests that cognitive processing of stressful experiences is most beneficial when shared and that perceptions of social constraint related to open expression about cancer by one partner is associated with negative affect in the other partner (Manne, 1999; Pasipanodya, Parrish, Laurenceau, Cohen, Siegel et al, 2012). Particularly in late-stage cancers, where both partners likely have similar existential fears, an intervention for couples could be particularly effective to encourage more honest communication and thus facilitate cognitive and emotional processing. The research literature reveals a dearth of intervention studies targeted at couples; however, work by Manne and colleagues (2005) focused on early stage disease and couples’ communication, and a recent mindfulness-based stress reduction intervention also designed for couples, significantly reduced both patient and partner mood disturbance (Birnie, Garland, & Carlson, 2010).
Another direction for future research could focus on how content of thought relates to both negative and positive outcomes in cancer populations. In a mixed cancer population, Morris and Shakespeare-Finch (2011) reported varied psychological outcomes based on rumination content, finding that intrusive rumination and life purpose rumination was associated with distress, while deliberate rumination on benefits and social support was associated with post-traumatic growth. It is possible that this type of deliberate positive rumination may reduce harm/loss appraisals through positive reappraisal. Segerstrom, Stanton, Alden, and Shortridge (2003) also recommend considering both content valence and purpose of repetitive thought, highlighting the complicated relationship these variables can have. For example, Segerstom and colleagues (2003) report mixed findings with regard to searching for purpose, when they found it predicted better overall mental health as well as greater depression, while searching for meaning related to cancer predicted intrusive thought. Our measure of depressive rumination focused on negative feelings, but a study designed with this purpose in mind could develop a measure with a more diverse set of items to capture the diversity of ruminative thinking that may be occurring.
As with all studies, the conclusions drawn from the present study must be considered in light of its limitations. First, the generalizability of this study is limited to the characteristics of this sample, which include college educated, non-Hispanic women and their partners confronting mostly late stage breast cancer. Less educated and minority women and male cancer patients may report different experiences under similar circumstances. Cognitive processes may be different, o relate differently, in women with early stages of breast cancer. Additionally, the cross-sectional nature of this study’s research design limits the conclusions that can be drawn. A future longitudinal study, or experimental study with manipulation of the independent variables, would be necessary to make causal claims regarding the relationship between these cognitions and depression.
In conclusion, although intrusive thoughts and harm/loss appraisals show direct effects on depressive symptoms, rumination appears to play a significant role in partially modulating the relationship between intrusive thought and harm/loss appraisal in women with breast cancer and their spouses. Healthcare providers can assist these patients and spouses by connecting them to interventions which teach both to better cope with cognitive processes and ruminative thought by either changing or reducing these thoughts or encouraging present-moment focus rather than preoccupation with repetitive, negative thoughts about the causes, consequences and meaning of cancer.
Acknowledgments
This project was funded by the National Cancer Institute (5R03CA115224)
References
- Bigatti SM, Brown LF, Steiner JL, Miller KD. Breast cancer in a wife: How husbands cope and how well it works. Cancer Nursing. 2011;34(3):193–201. doi: 10.1097/NCC.0b013e3181ef094c. DOI:10.1097/NCC.0b013e3181ef094c. [DOI] [PubMed] [Google Scholar]
- Bigatti SM, Steiner JL, Miller KD. The role of cognitive appraisals and coping in psychological distress in advanced breast cancer patients. Stress and Health. 2012;28(5):355–361. doi: 10.1002/smi.2444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bigatti SM, Wagner CD, Lydon JR, Steiner JL, Miller KD. Depression in husbands of breast cancer patients: Relations to coping and social support. Supportive Cancer Care. 2011;19(4):455–466. doi: 10.1007/s00520-010-0835-8. DOI 10.1007/s00520-010-0835-8. [DOI] [PubMed] [Google Scholar]
- Birnie K, Garland SN, Carlson LE. Psychological benefits for cancer patients and their partners participating in mindfulness-based stress reduction (MBSR) Psycho-Oncology. 2010;19:1004–1009. doi: 10.1002/pon.1651. [DOI] [PubMed] [Google Scholar]
- Bjorck JP, Hopp DP, Jones LW. Prostate cancer and emotional functioning: Effects of mental adjustment, optimism, and appraisal. Journal of Psychosocial Oncology. 1999;17:71–85. [Google Scholar]
- Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: A review of meta-analyses. Clinical Psychology Review. 2006;26:17–31. doi: 10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Campbell TS, Labelle LE, Bacon SL, Faris P, Carlson LE. Impact of mindfulness-based stress reduction (MBSR) on attention, rumination and resting blood pressure in women with cancer. Journal of Behavioral Medicine. 2012;35:262–271. doi: 10.1007/s10865-011-9357-1. [DOI] [PubMed] [Google Scholar]
- Fann JR, Thomas-Rich AM, Katon WJ, Cowley D, Pepping M, McGregor BA, Gralow Major depression after breast cancer: a review of epidemiology and treatment. General Hospital Psychiatry. 2008;30:112–126. doi: 10.1016/j.genhosppsych.2007.10.008. [DOI] [PubMed] [Google Scholar]
- Gallagher J, Parle M, Cairns D. Appraisal and psychological distress six months after diagnosis of breast cancer. British J Health Psyc. 2002;7(3):365–376(12). doi: 10.1348/135910702760213733. [DOI] [PubMed] [Google Scholar]
- Gilbert P, Cheung M, Irons C, McEwan K. An exploration into depression-focused and anger-fovused rumination in relation to depression in a student population. Behavioural and Cognitive Psychotherapy. 2005;33:273–283. doi: 10.1017/S1352465804002048. [Google Scholar]
- Hann D, Winter K, Jacobson P. Measurement of depressive symptoms in cancer patients: Evaluation of the center for epidemiological studies depression scale (ces-d) Journal of Psychosomatic Research. 1999;46(5):437–443. doi: 10.1016/s0022-3999(99)00004-5. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Witt A, Oh D. The effect of mindfulness-based theraoy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2010;78(2):169–183. doi: 10.1037/a0018555. doi:10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz M, Wilner N, Alvarez W. Impact of events scale: A measure of subjective stress. Psychsomatic Medicine. 1979;41(3):209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- Hong RY. Worry and rumination: Differential associations with anxious and depressive symptoms and coping behavior. Behaviour Research and Therapy. 2007;45:277–290. doi: 10.1016/j.brat.2006.03.006. [DOI] [PubMed] [Google Scholar]
- Joorman J, Hertel PT, LeMoult J, Gotlib IH. Training forgetting of negative material in depression. Journal of Abnormal Psychology. 2009;118:34–43. doi: 10.1037/a0013794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler TA. The cognitive appraisal of health scale: Development and psychometric evaluation. Research in Nursing & Health. 1998;21:73–82. doi: 10.1002/(sici)1098-240x(199802)21:1<73::aid-nur8>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- Langer SL, Rudd ME, Syrjala KL. Protective buffering and emotional dysynchrony among spousal caregivers of cancer patients. Health Psychology. 2007;26:635–643. doi: 10.1037/0278-6133.26.5.635. [DOI] [PubMed] [Google Scholar]
- Manne SL. Intrusive thoughts and psychological distress among cancer patients: The role of spouse avoidance and criticism. Journal of Consulting and Clinical Psychology. 1999;67:539–546. doi: 10.1037//0022-006x.67.4.539. [DOI] [PubMed] [Google Scholar]
- Manne SL, Glassman M. Perceived control, coping efficacy, and avoidance coping as mediators between spouses’ unsupportive behaviors and cancer patients’ psychological distress. Health Psychology. 2000;19:155–164. doi: 10.1037//0278-6133.19.2.155. [DOI] [PubMed] [Google Scholar]
- Manne SL, Ostroff JS, Winkel G, Fox K, Grana G, Miller E, Frazier T. Couple-focused group intervention for women with early stage breast cancer. Journal of consulting and clinical psychology. 2005;73(4):634. doi: 10.1037/0022-006X.73.4.634. [DOI] [PubMed] [Google Scholar]
- Micheal T, Halligan SL, Clark DM, Ehlers A. Rumination in posttraumatic stress disorder. Depression and Anxiety. 2007;24:307–317. doi: 10.1002/da.20228. [DOI] [PubMed] [Google Scholar]
- Michl LC, McLaughlin KA, Shepard K, Nolen-Hoeksema S. Rumination as a mechanism linking stressful life events to symptoms of depression and anxiety: Longitudinal evidence in early adolescents and adults. Journal of Abnormal Psychology. 2013;122(2):339–352. doi: 10.1037/a0031994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milbury K, Badr H. Sexual problems, communication patterns, and depressive symptoms in couples coping with metastatic breast cancer. Psycho-Oncology. 2012 doi: 10.1002/pon.3079. DOI: 10.1002/pon.3079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris BA, Shakespeare-Finch J. Rumination, post-traumatic growth, and distress: Structural equation modeling with cancer survivors. Psycho-Oncology. 2011;20:1176–1183. doi: 10.1002/pon.1827. [DOI] [PubMed] [Google Scholar]
- Mystakidou K, Tsilika E, Parpa E, Galanos A, Vlahos L. Caregivers of advanced cancer patients: Feelings of hopelessness and depression. Cancer Nursing. 2007;30(5):412–418. doi: 10.1097/01.NCC.0000290807.84076.73. Doi:10.1097/01.NCC.0000290807.84076.73. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute Depression PDR: Health Professional Version. 2013 Retrieved on August 5, 2013 from http://www.cancer.gov/cancertopics/pdq/supportivecare/depression/HealthProfessional.
- Nolen-Hoeksema S. Responses to depression and their effects on the duration of depressive episodes. Journal of Abnormal Psychology. 1991;100(4):569–582. doi: 10.1037//0021-843x.100.4.569. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Parker LE, Larson J. Ruminative coping with depressed mood following loss. Journal of Personality and Social Psychology. 1994;67:92–104. doi: 10.1037//0022-3514.67.1.92. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking Rumination. Perspectives on Psychological Science. 2008;3:400–424. doi: 10.1111/j.1745-6924.2008.00088.x. doi:10.1111/j.1745-6924.2008.00088.x. [DOI] [PubMed] [Google Scholar]
- Papageorgiou C, Siegle GJ. Rumination and depression: Advances in theory and research. Cognitive Therapy and Research. 2003;27(3):243–245. [Google Scholar]
- Papageorgiou C, Wells A. An empirical test of a clinical metacognitive model of rumination and depression. Cognitive Therapy and Research. 2003;27(3):261–273. [Google Scholar]
- Pasipanodya EC, Parrish BP, Laurenceau JP, Cohen LH, Siegel SC, Graber EC, Belcher A. Social constraints on disclosure predict daily well-being in couples coping with early-stage breast cancer. Journal of Family Psychology. 2012;26:661–667. doi: 10.1037/a0028655. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measures. 1977;1:385–401. [Google Scholar]
- Reich M, Lesur A, Perdrizet-Chevalier C. Depression, quality of life, and breast cancer: a review of the literature. Breast Cancer Research and Treatment. 2008;110:9–17. doi: 10.1007/s10549-007-9706-5. [DOI] [PubMed] [Google Scholar]
- Raes F, Willians J, Hermans D. Reducing cognitive vulnerability to depression: A preliminary investigation of Memory Specificity Training (MEST) in patients with depressive symptomology. Journal of Behavioral Therapy and Experimental Psychiatry. 2009;40:24–38. doi: 10.1016/j.jbtep.2008.03.001. [DOI] [PubMed] [Google Scholar]
- Segerstrom SC, Stanton AL, Alden LE, Shortridge BE. A multidimensional structure for repetitive thought: What’s on your mind, and how, and how much? Journal of Personality and Social Psychology. 2003;85:909–921. doi: 10.1037/0022-3514.85.5.909. [DOI] [PubMed] [Google Scholar]
- Siegle GJ, Ghinassi F, Thase M. Neurobehavioral therapies in the 21st century: Summary of an emerging field and an extended example of cognitive control for depression. Cognitive Therapy Research. 2007;31:235–262. [Google Scholar]
- Smith JM, Alloy LB. A roadmap to rumination: A review of the definition, assessment, and conceptualization of this multifaceted construct. Clinical Psychology Review. 2009;29(2):116–128. doi: 10.1016/j.cpr.2008.10.003. Dio:10.1016/j.cpr.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spasojevic J, Alloy LB. Rumination as a common mechanism relating depressive risk to depression. Emotion. 2001;1:25–37. doi: 10.1037/1528-3542.1.1.25. [DOI] [PubMed] [Google Scholar]
- Starr S, Moulds ML. The role of negative interpretations of intrusive memories in depression. Journal of Affective Disorders. 2006;93:125–132. doi: 10.1016/j.jad.2006.03.001. [DOI] [PubMed] [Google Scholar]
- Sundin E, Horowitz MJ. Impact of event scale: psychometric properties. British Journal of Psychiatry. 2002;180(3):205–209. doi: 10.1192/bjp.180.3.205. doi:10.1192/bjp.180.3.205. [DOI] [PubMed] [Google Scholar]
- Troy AS, Shallcross AJ, Davis TS, Mauss IB. History of mindfulness-based cognitive therapy is associated with increased cognitive reappraisal ability. Mindfulness. 2013;4(3):213–222. doi: 10.1007/s12671-012-0114-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wampold BE, Minami T, Baskin TW, Tierney SC. A meta-(re)analysis of the effects of cognitive therapy versus other therapies for depression. Journal of Affective Disorders. 2002;68:159–65. doi: 10.1016/s0165-0327(00)00287-1. [DOI] [PubMed] [Google Scholar]
- Watkins E, Baeyens C, Read R. Concreteness training reduces dysphoria: Proof-of-principle for repeated cognitive bias modification in depression. Journal of Abnormal Psychology. 2009;118:55–64. doi: 10.1037/a0013642. [DOI] [PubMed] [Google Scholar]
- Whitacker KL, Watson M, Brewin CR. Intrusive cognitions and their appraisal in anxious cancer patients. Psycho-Oncology. 2009;18:1147–1155. doi: 10.1002/pon.1512. [DOI] [PubMed] [Google Scholar]