Abstract
A method was developed for the measurement of 19 parent PAHs (PAHs) and 34 hydroxylated PAHs (OH-PAHs) in urine and personal air samples of particulate matter less than 2.5 um in diameter (PM2.5) using GC-MS and validated using NIST SRM 3672 (Organic Contaminants in Smoker’s Urine) and SRM 3673 (Organic Contaminants in Nonsmoker’s Urine). The method was used to measure PAHs and OH-PAHs in urine and personal PM2.5 samples collected from the operators of two different fish smoking facilities (tipi and smoke shed) burning two different wood types (alder and apple) on the Confederated Tribes of Umatilla Indian Reservation (CTUIR) while they smoked salmon. Urine samples were spiked with β-glucuronidase/arylsulfatase to hydrolyze the conjugates of OH-PAHs and the PAHs and OH-PAHs were extracted using Plexa and C18 solid phases, in series. The 34OH-PAHs were derivatized using MTBSTFA, and the mixture was measured by GC-MS. The personal PM2.5samples were extracted using pressurized liquid extraction, derivatized with MTBSTFA and analyzed by GC-MS for PAHs and OH-PAHs. Fourteen isotopically labeled surrogates were added to accurately quantify PAHs and OH-PAHs in the urine and PM2.5 samples and three isotopically labeled internal standards were used to calculate the recovery of the surrogates. Estimated detection limits in urine ranged from 6.0 to 181 pg/ml for OH-PAHs and from 3.0 to 90 pg/ml for PAHs, and, in PM2.5, they ranged from 5.2 to 155 pg/m3 for OH-PAHs and from 2.5 to 77 pg/m3 for PAHs. The results showed an increase in OH-PAH concentrations in urine after 6 hours offish smoking and an increase in PAH concentrations in air within each smoking facility. In general, the PAH exposure in the smoke shed was higher than in the tipi and the PAH exposure from burning apple wood was higher than burning alder.
Keywords: Polycyclic aromatic hydrocarbons (PAHs), OH-PAHs, Native Americans, Fish smoking
1. Introduction
Polycyclic aromatic hydrocarbons (PAHs) are ubiquitous environmental pollutants, found even in remote ecosystems (Landers et al., 2010; Primbs et al., 2008; Usenko et al., 2010). PAHs are emitted to the atmosphere during incomplete combustion of organic material (e.g. solid fuels, meat)(Tonne et al., 2004), including natural processes (e.g. forest fires, volcano eruptions)(Baek et al., 1991; Xu et al., 2006). Human exposure to PAHs occurs mainly through ingestion of food with high PAH concentrations, such as mollusks, crustaceans, oil, margarine (Veyrand et al., 2013), but also barbequed (Guillen et al., 1997), smoked (Essumang et al., 2012; Forsberg et al., 2012), or grilled meat (Alomirah et al., 2011). Additional sources of PAH exposure include inhalation of vehicular exhaust gases (Adetona et al., 2012), smoke from burning solid fuels (Li et al., 2011), and cigarette smoke (Zhong et al., 2011). Chronic exposure to PAHs has been linked to lung cancer (Motorykin et al., 2013) and peripheral arterial disease (Xu et al., 2013). The U.S. Environmental Protection Agency Integrated Risk Information System (1992) and the International Agency for Research on Cancer (IARC)(1983) identify some PAHs as probable human carcinogens. Additionally, some PAHs are known mutagens (Bostrom et al., 2002; Hainaut and Hollstein, 2000) and animal carcinogens (Neff, 1978; Tonne et al., 2004).
PAHs are metabolized in the human body via CYP-450 enzymes (Jerina et al., 1970). The most abundant PAH metabolites in the human body are hydroxylated PAHs (OH-PAHs)(Onyemauwa et al., 2009) and some OH-PAHs are more potent carcinogens than parent PAHs because they can bind to DNA(Wang et al., 2009; Wei et al., 2010) and cause cell mutations (Hainaut and Hollstein, 2000). 2-hydroxyphenanthrene has been shown to be linked to cardiovascular diseases (Xu et al., 2010) and 1-hydroxynaphthalene has a slight endocrine effect in adult males (Han et al., 2010). Diols, diol epoxides and tetraols are also formed by metabolism (Zhong et al., 2011). Hydroxy and dihydroxy-PAHs are excreted from the body with urine in the form of glucuronides and sulfates (Jacob and Seidel, 2002). Parent PAHs are not completely metabolized to OH-PAHs in the human body, therefore, urine contains a mixture of both PAHs and OH-PAHs (Becher and Bjorseth, 1983; Campo et al., 2006; Campo et al., 2007; Campo et al., 2010).
The most frequently measured OH-PAH biomarker for human exposure to PAHs is 1-hydroxypyrene (1-OH-Pyr)(Jongeneelen, 2001; Leroyer et al., 2010; Levin, 1995; Mucha et al., 2006). However, 1-OH-Pyr does not provide a complete assessment of human exposure to PAH mixtures because of the different molecular size, shape, and rates of metabolism of different PAHs (Barbeau et al., 2009; Li et al., 2008). Recently, several other OH-PAHs have been used as biomarkers of human exposure to PAHs, including 4-hydroxyphenanthrene (4-OH-Phe) (Rossbach et al., 2007) and 3-hydroxybenzo (a) pyrene (3-OH-BaP)(Barbeau et al., 2009; Leroyer et al., 2010) for total PAH exposure, 1,2-dihydroxynaphthalene (1,2-OH-Nap) for naphthalene exposure (Klotz et al., 2011), and 2-hydroxynaphthalene and the sum of hydroxyfluorenes for tobacco smoke exposure (St Helen et al., 2012). Ideally, multiple PAH metabolites, including parent PAHs, should be used as biomarkers to better understand the extent of human exposure to PAHs (Förster et al., 2008; Jacob and Seidel, 2002; Strickland and Kang, 1999).
The quantitative determination of multiple OH-PAH and PAH biomarkers in human urine is challenging due to difference in the polarity of these compounds and the potential for matrix interferrants (Campo et al., 2010; Li et al., 2010). The most common method for measuring OH-PAHs and PAHs in aqueous solutions, such as urine, is extraction using solid phase extraction (SPE), followed by either liquid chromatography coupled with mass spectrometry (LC-MS)(Chetiyanukornkul et al., 2006; Fan et al., 2012; Onyemauwa et al., 2009) or derivatization of OH-PAHs, followed by gas chromatography coupled with mass spectrometry (GC-MS)(Grova et al., 2011; Itoh et al., 2006; Klotz et al., 2011; Luan et al., 2007; Romanoff et al., 2006; Schummer et al., 2009; Smith et al., 2002; Usenko et al., 2010). Other methods include HPLC with fluorescence detection (Hagedorn et al., 2009; Kishikawa et al., 2004; Rossbach et al., 2007) and derivatization with pentafluorobenzyl bromide, followed by LC-MS/MS(Jacob et al., 2007).
Derivatization converts OH-PAHs into more volatile compounds and increases the selectivity and sensitivity of the GC/MS analysis. Several derivatization reagents that have been used for OH-PAHs include N-methyl-N-(trimethylsilyl) trifluoroacetamide (MSTFA)(Romanoff et al., 2006; Smith et al., 2002), N,O-bis (trimethylsilyl) trifluoroacetamide (BSTFA) (Itoh et al., 2006; Luan et al., 2007; Schummer et al., 2009), N,O-bis (trimethylsilyl) acetamide (BSA) with 5% trimethylchlorosilane (TMCS)(Klotz et al., 2011), N-(t-butyldimethylsilyl)-N-methyltrifluoroacetamide (MTBSTFA)(Grova et al., 2011; Schummer et al., 2009), and pentafluorobenzyl bromide (Jacob et al., 2007). The choice of derivatization reagent depends on the structure of the OH-PAH. While all of these derivatization reagents react with monohydroxylated PAHs, not all of them react with dihydroxy-PAHs, especially dihydroxy-PAHs with hindered OH groups (Luan et al., 2007). Schummer et al. (2009) compared BSTFA and MTBSTFA and concluded that MTBSTFA was the preferred derivatization reagent for OH-PAHs without sterically hindered OH groups because it gave higher analytical response and better chromatographic resolution of OH-PAH isomers. Another advantage of using MTBSTFA for the derivatization of OH-PAHs is that the products were more stable to hydrolysis in the presence of trace water (de Alda and Barcelo, 2001).
Limited amount of studies have been published on tribal exposure, including trace metals (Moon et al., 1986), polychlorinated biphenyls (PCBs)(Schaeffer et al., 2006) and methyl mercury from fish (Xue et al., 2012). This study was conducted in collaboration with the Confederated Tribes of the Umatilla Indian Reservation (CTUIR) in May 2011(Forsberg et al., 2012). Native Americans traditionally smoke fish for sustenance. During one of the fish smoking events, the fish was analyzed for PAHs before and after smoking (Forsberg et al., 2012). In addition, personal air samples of particulate matter with diameter less than 2.5 um (PM2.5) and urine samples were collected from the participants conducting the fish smoking activities in order to measure their exposure to PAHs due to inhalation resulting from their fish smoking activities. The objectives were to develop an analytical method for the determination of 19 PAHs and 34OH-PAHs in urine and PM2.5 and to use this method to better understand human exposure to OH-PAHs and PAHs via inhalation during traditional Native American fish smoking.
2. Material and methods
2.1 Reagents
All parent and hydroxy-PAHs standards, including 1-Hydroxynaphthalene (1-OH-Nap), 2-Hydroxynaphthalene (2-OH-Nap), 2,3-Dihydroxynaphthalene (2,3-OH-Nap), 1,3-Dihydroxynaphthalene (1,3-OH-Nap), 1,5-Dihydroxynaphthalene (1,5-OH-Nap), 1,6-Dihydroxynaphthalene (1,6-OH-Nap), 2,7-Dihydroxynaphthalene (2,7-OH-Nap), 2,6-Dihydroxynaphthalene (2,6-OH-Nap), 9-Hydroxyfluorene (9-OH-Flo), 3-Hydroxyfluorene (3-OH-Flo), 2-Hydroxyfluorene (2-OH-Flo), 1-Hydroxy-9-fluorenone (1-OH-Flon), 2-Hydroxy-9-fluorenone (2-OH-Flon), 2-Hydroxyanthraquinone (2-OH-AntQn), 4-Hydroxyphenanthrene (4-OH-Phen), 3-Hydroxyphenanthrene (3-OH-Phen), 2-Hydroxyphenanthrene (2-OH-Phen), 1-Hydroxyphenanthrene (1-OH-Phen), 3-Hydroxyfluoranthene (3-OH-Flt), 1-Hydroxypyrene (1-OH-Pyr), 2-Hydroxyenzo(a) anthracene (2-OH-BaA), 3-hydroxybenzo(c) pnenanthrene (3-OH-BcPhen), 10-Hydroxybenzo(a) pyrene (10-OH-BaP), 12-Hydroxybenzo(a) pyrene (12-OH-BaP), 7-Hydroxybenzo(a) pyrene (7-OH-BaP), 9-Hydroxybenzo(a) pyrene (9-OH-BaP), 3-Hydroxybenzo(a) pyrene (3-OH-BaP), 4-Hydroxychrysene (4-OH-Chr), 6-Hydroxychrysene (6-OH-Chr), 3-Hydroxychrysene (3-OH-Chr), 2-Hydroxychrysene (2-OH-Chr), 1-Hydroxychrysene (1-OH-Chr), 2,6-Hydroxyanthraquinone (2.6-OH-AntQn), 11-Hydroxybenzo(b) fluoranthene (11-OH-BbFlt), Naphthalene (Nap), Acenaphtylene (Acy), Acenaphthene (Ace), Fluorene (Flo), Phenanthrene (Phen), Anthracene (Ant), Fluoranthene (Flt), Pyrene (Pyr), Retene (Ret), Benzo(a) anthracene (BaA), Chrysene (Chr), Triphenylene (TriPh), Benzo(b) fluoranthene (BbFlt), Benzo(k) fluoranthene (BkFlt), Benzo(e) pyrene (BeP), Benzo(a) pyrene (BaP), Indeno(1,2,3-cd) pyrene (I(1,2,3-cd)Pyr), Dibenz(a,h) anthracene (BahA), Benzo(ghi) perylene (BghiPer)(Table S1) were purchased from AccuStandards, Inc. (New Haven, CT), Sigma-Aldrich (Milwaukee, WI), MRIGlobal (Kansas City, MO), VWR international, Inc (Radnor, PA), or TCI America (Portland, OR). The isotopically labeled standards, including1-Hydroxy[2H7]naphthalene, 2-Hydroxy[2H9]fluorene, 3-Hydroxy[13C6]phenanthrene, 1-Hydroxy[13C6]pyrene, 1-Hydroxy[13C6]benzo(a) anthracene, 3-Hydroxy[13C6]benzo(c) phenanthrene, 3-Hydroxy[13C6]chrysene, [2H10]-Fluorene, [2H10]-Phenanthrene, [2H10]-Pyrene, [2H12]-Triphenylene, [2H12]-Benzo(a) pyrene, [2H12]-Benzo(ghi) perylene (Table S1) were purchased from Cambridge Isotope Laboratories (Andover, MA), Santa Cruz Biotechnology Inc. (Santa Cruz, CA), MRI Global (Kansas City, MO), orC/D/N isotopes Inc. (Pointe-Claire, Quebec, Canada). The Bond Elute Plexa (30 mg and 60 mg, 3 mL), Bond Elute C18 (100 mg, 3 mL), and Bond Elute Si (500 mg, 3mL) cartridges were purchased from Agilent Technologies (New Castle, DE). The Focus (60mg, 3mL) cartridges were purchased from Varian, Inc (Lake Forest, CA), and the Isolute 101 (100mg, 3 mL) cartridges were purchased from Biotage LLC (Charlotte, NC). Optima grade solvents (methanol, hexane (Hex), ethyl acetate (EA), acetonitrile (ACN), and dichlromethane (DCM)) were purchased from Fisher Scientific (Santa Clara, CA), toluene (>=99.9%), MTBSTFA (>97%), BSTFA+TMCS (99:1) andBSA:TMC:TMSI (3:2:3)were purchased from Sigma-Aldrich (Milwaukee, WI). β-glucuronidase/arylsulfatase was purchased from Roche Diagnostics Corporation (Indianapolis, IN). Acetate buffer (pH=5.5, APHA) was purchased from Ricca Chemical Company (Arlington, TX). Certified drug free urine was purchased from UTAK laboratories, Inc (Valencia, CA). GC amber vials (1.5 mL) and inserts (300 μL) were purchased from VWR International (San Francisco, CA). Personal PM2.5samples were collected using a Leland Legacy Sample pump, Personal Environmental Monitor, and the quartz fiber filters were purchased from SKC Inc. (Eighty Four, PA). Standard Reference Materials (SRMs) were provided by National Institute for Standards and Technology (NIST) (Gaithersburg, MD).
2.2 Collection of urine and personal PM2.5 air samples
Urine and personal PM2.5 samples were collected from two male members of the Confederated Tribes of the Umatilla Indian Reservation (CTUIR) in May 2011 who smoked salmon (see Figure S1 for the sample collection timeline). The participants were asked not to eat foods containing PAHs, including fried, broiled, charcoaled, roasted or toasted foods, three days prior to the observation period when they smoked salmon. Both participants were non-smokers. Each participant operated one smoking structure – either a smoke shed (SS) and or a tipi (TP), shown in Figure S2. The participants smoked two batches of salmon in each structure. The first batch was smoked using apple wood and the second batch was smoked using alder wood producing a cross-over study design.
Freshly caught Spring Chinook Salmon from the Columbia River was purchased from a commercial Native American fisherman near Celilo, Oregon (Forsberg et al., 2012). In the smoke shed, fish fillets were placed on a shelf approximately 1.5 m feet above the fire, while in the tipi the fish fillets were hung on a string approximately 2 m above the fire. The smoke shed had a more confined space, with less ventilation, while the tipi had the open top, creating an updraft that carried the smoke over the fish. As needed, the operators periodically walked into each structure to add more wood to the fire. Depending on the structure and wood type, it took 22 to 35 hr to fully smoke the fish (Figure S1). Both operators wore a Leland Legacy Personal Environmental Monitor PM2.5 air sampler (PAS) to collect PM2.5 near their breathing zone. In order to capture total PM2.5 PAH exposure that only resulted from being inside the smoke structures, operators turned on their PAS before entering the smoking structures and turned off the PAS upon leaving the smoking structure. For each batch, the operators entered and left the smoking structures approximately 10–16 times during the 22 to 35 hr smoking period. The PM2.5was collected on quartz filters (34 mm in diameter) at a flow rate of 10 L/min. The filters were stored at −20°C until analysis.
Urine samples were collected in plastic urine collection cups using clean catch collection technique (U.S. Department of Health and Human Services. National Institutes of Health, 2012). When the apple wood was used for fish smoking, four urine samples were collected per participant, per structure: the first sample was collected just before starting to operate the smoking structure and then three samples were collected after 4–5 hr, 12–13 hr, and 22–23 hr of initiating the fish smoking activity (Figure S1). When alder wood was used for fish smoking, three urine samples were collected per participant, per structure: after 10 hr,22 hr and 33–34 hr of initiating activities to smoke the second batch of salmon (Figure S1). The sample that was collected prior to operating any smoke structure was also used as time zero for the second batch when alder wood was used in the smoking structures. The that elapsed between the end of smoking with apple wood and start of smoking with alder wood was 12.5 hr for the smoke shed operator and 10.9 hr for the tipi operator. Urine samples were stored at -25°C and analyzed within one week of collection. The study was approved by the Institutional Review Board of Oregon State University, the CTUIR Health Commission, and Portland Area Indian Health Board.
2.3 Urine analytical method
The analytical method developed for the determination of PAH and OH-PAH in urine is shown in Figure 1. A3 ml aliquot of urine (blank UTAK urine was used for method development) was mixed with5mL of acetate buffer (pH=5.5). Six labeled PAH surrogates (10 μl, 1000 pg/μl) and 9labeled OH-PAH surrogates (20 μl, 500 pg/μl) were spiked into the mixture for quantitation, followed by the addition of β-glucuronidase/arylsulfatase (10 μl) and incubation overnight (37 °C, 15 hours) to hydrolyze OH-PAHs. Two SPE phases in series, Bond Elut Plexa (for OH-PAHs, top cartridge) and Bond Elut C18 (for PAHs, bottom cartridge), were used to extract the analytes from the urine matrix. The SPE cartridges were preconditioned with 3 mL of methanol, followed by 3 mL of deionized water. The urine was passed through the SPE cartridges and the analytes were retained on the two stationary phases. The analytes were then eluted with 3 ml of DCM, followed by 3 ml of EA and the two extracts were combined. The extract was then loaded onto a 500 mg silica column, previously conditioned with 3 mL of EA, 3 mL of DCM and 6 mL of Hex. The first silica fraction was eluted with 5 ml of 5% EA in Hex and contained parent PAHs. The second silica fraction was eluted with 5 ml of 20% of EA in Hex and contained OH-PAHs. The two fractions were concentrated separately to 300 μl using a TurboVap® evaporator (nitrogen gas, 30 °C water bath), transferred into amber GC vials with inserts and evaporated to ~20μl under a gentle stream of nitrogen. Internal standards were spiked into the extracts (10 μL, 1mg/L) to track surrogate recovery and 20 μl of toluene were added to both fractions. One hundred μl of acetonitrile (ACN) was added to OH-PAH fraction, the fraction was evaporated to 20 μl a second time, and 30 μl of MTBSTFA was added for derivitization and determination of 34 OH-PAHs. The OH-PAH fraction was incubated at 65 °C for 25 minutes and the PAH and OH-PAH fractions were analyzed separately by GC-MS (Table S1, OH-PAHs and LMW PAHs).
Figure 1.

Flow diagram of the entire analytical method for the measurement of 19 PAHs and 34 OH-PAH in urine and PM2.5 samples
2.4 PM2.5 analytical method
The analytical method for the determination of PAH and OH-PAH in PM2.5is also shown in Figure 1. The PM2.5 filters were spiked with PAH surrogates (10 μl, 1000 pg/μl) and OH-PAH surrogates (20 μl, 500 pg/μl) and extracted with Hex:Ace (3:1, v/v) using pressurized liquid extraction (PLE, 100°C, 1500 psi). The extract was loaded onto a silica column (20g), preconditioned with 50 ml of EA, 100 ml of DCM and 50 ml of Hex. The extract was eluted from the silica column using 100 ml of DCM. The eluent then was concentrated to 300 μL and a 40 μL aliquot was removed for PAH and OH-PAH analysis. The PM extract was then derivatized with MTBSTFA and analyzed for LMW PAHs, HMW PAHs, Oxy-PAHs, and OH-PAHs (Table S1).
2.5 PAH and OH-PAH analysis and detection limits
An Agilent 6890 GC chromatograph, equipped with 7683 series autosampler and 5973N mass selective detector with electron impact ionization was used for the analysis of 19 PAHs and 34 OH-PAHs. A DB-5 GC column (Agilent, 30 m x 25 m, 0.25 μm) was used and the carrier gas was helium with a flow rate of 1 ml/min. The GC oven temperature program for the analysis of PAH and OH-PAH was: 70 °C, hold for 1 min, then ramp 5 °C/min to 200 °C, hold for 5 min, ramp 5 °C/min to 250 °C, ramp 2 °C/min to 286 °C, and ramp 34 °C/min to 320 °C, hold for 5 min. The inlet and interface temperatures were 260 °C and 280°C, respectively. All analyses were done in selected ion monitoring (SIM) mode and Table S2 lists the m/z ions monitored. The total run time for the determination of19 PAHs and 34 OH-PAHs was 66 minutes. The method detection limits in urine and air were calculated based on response factors according to the US EPA method 8280A (U.S. EPA, 1996). Urinary PAH and OH-PAH concentrations were adjusted to creatinine concentration to account for dilution. The personal PM2.5 samples were also analyzed for high molecular weight PAHs (302 MW) and oxy-PAHs using previously published methods (Jia et al., 2011; Wang et al., 2012; Wang et al., 2011).
2.6 Creatinine measurements
Creatinine was measured using the method described in Chiaia et al. (Chiaia et al., 2008). Briefly, urine samples were brought to room temperature and 2 ml aliquot was centrifuged at 14 000 rpm. The supernatant was then transferred to HPLC vial and spiked with creatinine-D3(US Biological, Swampscott, MA) standard. Creatinine analyses were performed on the Agilent 1100 HPLC system equipped with WatersQuattro Micro tandem mass spectrometer (Milford, MA) operated in positive mode with an electrospray ionization interface. An injection volume of 100 μL was used. The 100 μL sample volume was directly injected into a 2.0 × 4.0 mm C18 security guard cartridge that was attached to a 150 × 4.6 mm 5 μm particle size Luna C18 column (Phenomenex, Torrance, CA). Isocratic conditions with a mobile phase of 10 mM ammonium acetate in 5% methanol were used at a column temperature of 35 °C and a flow rate of 500 μL/min.
3. Results and Discussion
3.1 Development and Validation of Analytical Method
Experiments were conducted to optimize and validate the analytical method (Figure 1) including: urine extraction recoveries, PM2.5 extraction recoveries, the storage stability of underivatized OH-PAHs in frozen urine, the storage stability of the derivatized OH-PAHs, the intra- and inter-day variability of analytical method, and the estimated detection limits (EDLs). In addition, we tested different SPE stationary phases for the urine extraction, the SPE elution solvent composition, the volume of β-glucuronidase/arylsulfatase needed for the enzymatic hydrolysis of OH-PAHs and the choice of derivatizing agent (see Supporting Information). As a part of the validation of the analytical method, two NIST Standard Reference Materials (SRMs), SRM 3672 (Organic Contaminants in Smoker’s Urine) and SRM 3673 (Organic Contaminants in Non-Smoker’s Urine), were analyzed and the results compared to NIST reported concentrations.
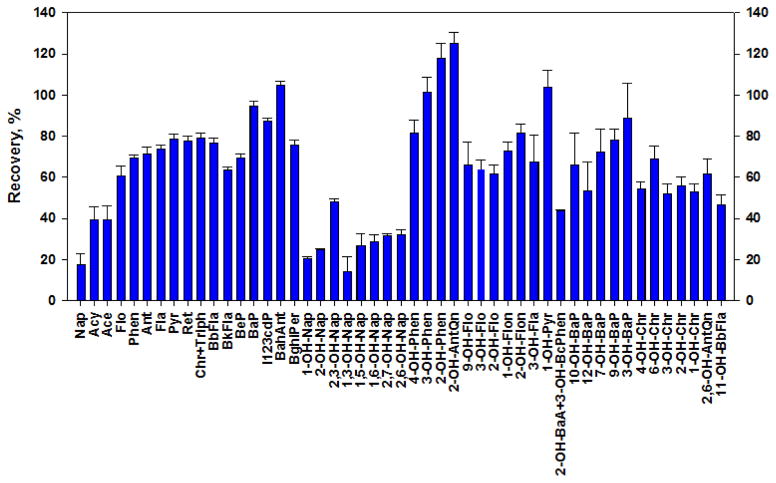
Urine Extraction Recoveries
The testing of different SPE stationary phases for the urine extraction, including Bond Elute Plexa (30 mg and 60 mg), Bond Elute C18 (100 mg), Focus cartridges (60mg), and the Isolute 101 cartridges (100 mg), is described in the Supporting Information (Figure S3). Based on the results of the PAH and OH-PAH recoveries from urine for the different SPE stationary phases, we chose to use the Bond Elute Plexa (60 mg) and Bond Elute C18 (50 mg), in series. A final recovery experiment was conducted for a PAH and OH-PAH mixture spiked in UTAK urine using the Bond Elute Plexa and Bond Elute C18, in series, with DCM and EA used as the elution solvents and the fractions combined (Figure 1). The recoveries for both PAHs and OH-PAHs for the entire analytical method are shown in Figure 2, and ranged from 14.3% to 125% (with a mean recovery of 64.2%). The OH-PAH recoveries were somewhat lower for the combination of SPE phases (61% ± 28%) (compared to Plexa alone, Figure 2 and S3), but were higher for PAHs (69%±21%) (Figure S4). Mono- and dihydroxynaphthalenes had the lowest recoveries of all OH-PAHs (28%±10%), this may be due to their increased polarity and volatility.
Figure 2.
Mean PAH and OH-PAH recoveries from urine over the entire method using Plexa+C18 SPE combined (three independent extractions, error bars represent standard deviation).
3.2 PM2.5 Extraction Recoveries
The PAH and OH-PAH extraction recoveries from quartz filters using pressurized liquid extraction (PLE) was determined. Blank and baked quartz filters were spiked with a mixture of 25 μl PAH (1 ng/μl), 25 μl of OH-PAH (1 ng/μl), 10 μl of PAH surrogates (1 ng/μl), and 20 μl of OH-PAH surrogates (500 ng/μl), and extracted with PLE using DCM and Hexane: Acetone (3:1, v/v) solution (100°C, 1500psi). Both fractions were evaporated to ~30 μl, followed by derivatization and GC-MS analysis. Figure S5 shows the PAH and OH-PAH PLE recoveries using these solvents. The mean recovery for PAHs was 67.5% using DCM (from 20.8% for Nap to 91.5% for B(ah)Ant) and 104.8% (from 46.7% for Acy to 189.6% for Phen) using Ace: Hex mixture. For OH-PAHs, the mean recoveries were 64.7% (range from 0% for 2,3-OH-Nap to 202.0% for 2-OH-AntQn) for DCM, and 91.5% (from 1.0% for 3-OH-BaP to 221.3% for 2-OH-Nap) for Hex:Ace. Overall, the mixture of Hexane and Acetone (3:1 v/v) had higher recoveries for both parent and hydroxy-PAHs and was chosen as the extraction solvent.
3.3 Storage stability of spiked OH-PAHs in frozen urine and derivatized OH-PAHs in extracts
The storage stability of OH-PAHs in frozen urine was investigated using six aliquots of UTAK urine (10 ml) that were spiked with 30 μl (1 ng/μl) of OH-PAHs from a standard mixture and frozen (-20 °C). Over a two week period (on days 1, 3, 6, and 13), one sample at a time was thawed, extracted, and analyzed using the method shown in Figure 1. Figure S6 shows the percent change in OH-PAH concentrations over 13 days. Most of the OH-PAHs (24 out of 34) were stable (% change from 0.80% to 17.8%) for up to 6 days, with the exception of dihydroxy-PAHs, 2-OH-AntQn, 9-OH-Flo, and 1-OH-Pyrwhich were stable for up to 3 days In contrast, Hagedorn et al. (2009) found that OH-PAHs were stable for at least seven months in frozen urine (-20 °C). However, in our study to determine stability of OH-PAHs in frozen urine we spiked UTAK urine with OH-PAHs that were unbound to sulfates and glucuronides, while the Hagedorn et al. study used urine samples that contained OH-PAHs which were bound to sulfates and glucuronides, making them more stable.
The stability of derivatized OH-PAH products in acetonitrile was also investigated. One hundred microliters of acetonitrile was spiked with OH-PAHs (50 μl, 1 ng/μl), the derivatization reaction was performed, the extracts were stored at (-20 °C) and the OH-PAH concentrations were measured in the acetonitrile extracts over a two week period (on days 1, 2, 7, and 14). Figure S7 shows the percent change in concentration of derivatized OH-PAH products in acetonitrile over a two week time period. The experiment showed that all of the derivatized OH-PAH products, except 9-OH-Flo and 1,3-OH-Nap, were stable at -20 °C for up to one week (% change from 0.09% to 10.2%), and up to two weeks at -20 °C, with the exception of 9-OH-Flo, 1,3-OH-Nap, 2-OH-AntQn, and 2,6-AntQn.
3.4 Intra- and inter-day variability of analytical method
Intra- and inter-day variability of the entire analytical method was determined by spiking three different concentrations of PAH and OH-PAH standards (1000, 100, and 10pg/μl) in UTAK urine, and analyzing each sample either three times during one day, or on three consecutive days, using the method shown in Figure 1.
Figure S8 and S9 show the mean and standard deviations for intra- and inter-day variability for the urine method. The mean intra-day variability of the analytical method was 1.1%, 1.0%, 1.6%, while the mean inter-day variability was 2.0%, 2.7%, and 5.2% for 1000 pg/μl, 100 pg/μl, and 10 pg/μl PAH and OH-PAH spikes, respectively.
3.5 Estimated detection limits (EDLs)
Table S1 shows the PAH and OH-PAH EDLs for the entire analytical method in urine and PM2.5. The PAH EDLs in urine ranged from 3.0 pg/ml for Phen to 89.7 pg/ml for BaP and were comparable to those reported by Campo et al. (2010) The OH-PAH EDLs in urine ranged from 6.0 pg/ml for 4-OH-Phen to 181.4 pg/ml for 2,3-OH-Nap. These detection limits were slightly higher than those reported by Onyemauwa et al. (2009), Itoh et al. (2006), Luan et al. (2007) and Romanoff et al. (2006), but lower than those reported by Campo et al. (2010) and Matarozzi et al. (2009). The benefits of the current method are the extensive number of analytes and the ability to quickly extract and analyze both PAHs and OH-PAHs. Additionally, silica cleanup significantly decrease the noise on the chromatogram, thus lowering estimated detection limits.
3.6 NIST urine SRM analysis for OH-PAH and PAH
Two NIST urine SRMs, SRM 3672 (Organic Contaminants in Smoker’s Urine) and SRM 3673 (Organic Contaminants in Non-Smoker’s Urine), were analyzed using the urine analytical method shown in Figure 1. The measured mean OH-PAH and PAH concentrations, and corresponding standard deviations, are presented in Table S3. In both SRM samples, the following compounds were measured above the EDL: 1-OH-Nap, 2-OH-Nap, 1,5-OH-Nap, 2-OH-Flu, 3-OH-Flu, 9-OH-Flu, 1-OH-Phen, 2-OH-Phen, 3-OH-Phen, 4-OH-Phen, 1-OH-Pyr, Phen, Flt, Pyr, and Ret. One compounds, 1,6-OH-Nap, was only measured in SRM 3672. With the exception of 1-OH-Nap, the OH-PAH concentrations were higher in the smoker’s urine compared to the non-smoker’s urine. Urinary PAH concentrations were not statistically different between the smoker’s and non-smoker’s urine. We measured 1,5-OH-Nap, 1,6-OH-Nap, Nap, Flu, and Pyr in the NIST urine SRMs that were not analyzed for by NIST.
The percent differences between our measured OH-PAH concentrations and the NIST OH-PAH concentrations ranged from 9% for 2-OH-Flu in SRM 3672(NIST, 2013a) to 1460% for 9-OH-Flu in SRM 3673(NIST, 2013b) (Table S3). The high percent differences for some of the measured OH-PAH concentrations between our measurement and NIST’s measurement of the NIST urine SRMs may be due to the absence of corresponding labeled surrogates for all of the OH-PAHs in our method. Because of cost limitations, only 5 out of 16 PAH and OH-PAH compounds detected above the EDL in our method had corresponding labeled surrogates (Table S3). However, the NIST method had corresponding labeled surrogates for all of the OH-PAH detected above the EDL.
3.7 PAH and OH-PAH Concentrations in Operators’ Urine from Fish Smoking Activities and Comparison to NHANES
Figure 3 shows the OH-PAH and PAH concentrations measured in the urine samples collected before and during the CTUIR fish smoking activities for the different types of wood (apple and alder), as well as the different smoking structures (tipi and smoke shed). The OH-PAH concentrations were normalized to the creatinine concentration of each urine sample to account for dilution (Viau et al., 2004).
Figure 3.
Mean OH- and PAH concentrations (three independent extractions, error bars represent standard deviation) in urine for A) Apple × Smoke Shed, B) Apple × Tipi, C) Alder × Smoke Shed, D) Alder × Tipi.
At the time zero the individual urinary OH-PAH concentrations ranged from 0.022 μg/g creatinine (4-OH-Phen) for the tipi (TP) operator to 11.2 μg/g creatinine (2-OH-Nap) for the TP operator. After the operating the smoking structures for 4 to 5 hours, urinary OH-PAHs concentrations increased 1.6 fold (4-OH-Phen, Apple-TP-U-4.3) to 25.4 fold (1-OH-Nap, Apple-TP-U-4.3), with a concentration range of 0.034 μg/g creatinine (4-OH-Phen, Apple-TP-U-4.3) to 18.5 μg/g creatinine (2-OH-Nap, Apple-TP-U-4.3). After twelve to thirteen hours of operating the smoking structures with apple wood, most OH-PAH concentrations in urine decreased by 2 to 95%, with the exception of 1-OH-Nap (Apple-SS-13.4), 1-OH-Phen (Apple-SS-13.4), 2-OH-Nap (Apple-TP-12.1), 4-OH-Phen (Apple-TP-12.1), 3-OH-Flu (Apple-TP-12.1), and 1-OH-Pyr (Apple-TP-12.1). These concentrations were higher than the time zero concentrations with exception of 4-OH-Phen (Apple-SS-13.4), and 9-OH-Flu (Apple-SS-13.4). This fluctuation in urinary OH-PAH over the first thirteen hours of operating a smoking structure likely reflects the need to spend more time in the smoking structures starting and maintaining the fires at the start of a smoking event, compared to the middle and end of the fish smoking activity when the fires are established. One metabolite, 4-OH-Phen, had time zero concentrations higher than at 13.4 hr or 23.2 hr after the start of smoking, indicating phenanthrene exposure prior to the start of the experiment for this operator. Figure 3 shows that,22 to 23 hours after the start of the fish smoking, the urinary OH-PAH concentrations continued to be higher than the pre-exposure concentrations (except 4-OH-Phen, Apple-SS-U-23.2 and 9-OH-Flu, Apple-TP-U-21.8).
For the second batch of salmon which was smoked using alder wood, urinary OH-PAH concentrations increased 1.1 fold (2-OH-Flu, Alder-TP-U-10.0) to 5.2 fold (1-OH-Phen, Alder-SS-U-10.0) after 10 hours of exposure and ranged from 0.066 μg/g creatinine (4-OH-Phen, Alder-TP-U-10.0) to 8.0 μg/g creatinine (2-OH-Nap, Alder-TP-U-10.0). After 21.8 hours of operating the smoking structures with alder wood, most urinary OH-PAHs concentrations increased even further from 1.2 (for 2-OH-Flu, Alder-TP-U-21.8) to 8.4 fold (3-OH-Phen, Alder-SS-U-21.8), with a concentration range from 0.165 μg/g creatinine (1-OH-Nap, Alder-TP-U-21.8) to 10.5 μg/g creatinine (2-OH-Nap, Alder-SS-U-21.8). Thirty-three of operating the smoking structures with alder wood, most urinary OH-PAH concentrations decreased, except for 4-OH-Phen (Alder-SS-33.3), 2-OH-Phen (Alder-SS-33.3), 1-OH-Phen (Alder-TP-33.8), 3-OH-Flu (Alder-TP-33.8), and 2-OH-Flu (Alder-TP-33.8). This pattern, which was also observed on the first day with apple wood, is likely due to decreased amount of time spent in the smoking structures once the fires have been established or because the fires are not as strong towards the end of the smoking process. Since the dihydroxynaphthalenes (1,3-; 2,3-; 2,7-; and 2,6-), hydroxyanthraquinones (2- and 2,6-), hydroxyfluorenones (1- and 2-), 3-hydroxyfluoranthene, 2-hycroxybenzo (a) anthracene, 3-hydroxybenzo (c) pnenanthrene, hydroxybenzo (a) pyrenes (3-, 7-, 9-, 10- and 12-), hydroxychrysenes (1-, 2-, 3-, 4-, and 6-), and 11-hydroxybenzo (b) fluoranthene were not detected above the EDL in the urine samples or in the NIST SRM urine samples, we conclude they are not predominant human metabolites of PAHs.
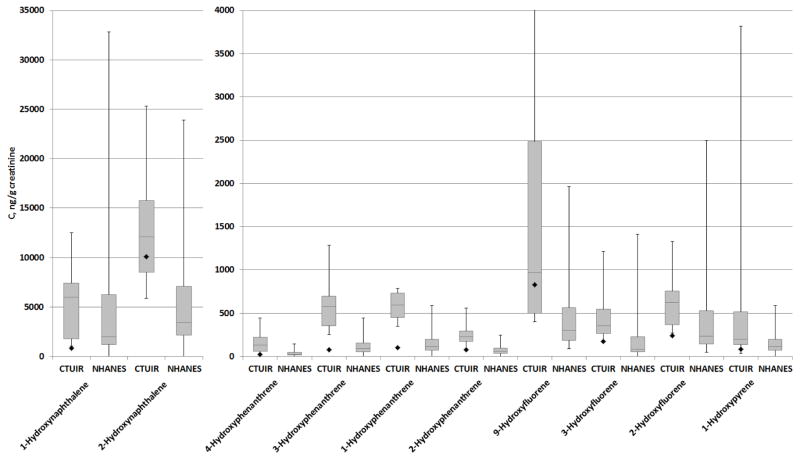
Creatinine-adjusted OH-PAH concentrations measured in the urine samples collected in this study were compared to creatinine-adjusted OH-PAH concentrations reported in the National Health and Nutrition Examination Survey (NHANES) for the U.S. population (Centers for Disease Control and Prevention (CDC)) (Figure 4). The average time zero concentrations for all measured OH-PAHs, except for 2-OH-Nap and 9-OH-Flu, were in the 25th-to-75th percentile of NHANES values (Figure 4, grey bars). The median urinary OH-PAH concentrations measured after time zero were higher than the NHANES median concentration. However, the highest urinary 1-OH-Nap, 3-OH-Flu, and 2-OH-Flu concentrations in the CTUIR urine samples were lower than the highest NHANES concentration. Both the median and the highest concentrations of 1-hydroxypyrene in the CTUIR urine samples collected after time zero were higher than the median and the highest NHANES values. On average, the mean CTUIR urinary OH-PAH concentrations were 4.4 times higher than the mean NHANES concentrations.
Figure 4.
The box plots of urinary OH-PAH concentrations for the CTUIR fish smoking activities and for NHANES values from 2007–2008 survey years (Crinnion, 2010). The grey rectangle represents the first and third quartile (25th and 75th percentile), the line inside is the median, and whiskers are minimum and maximum values. The black diamond is pre-exposure value for CTUIR samples.
Compared to time zero measurements, inhalation exposure that occurred as a result of smoking salmon led to elevated urinary PAH concentrations (Figure 3). After 5.5 hr from the start of fish smoking activities with apple wood, urinary phenanthrene concentrations increased from <EDL to 6.7 μg/g creatinine for the smoke shed operator and to 0.89 μg/g creatinine for the tipi operator. With apple wood, the urinary fluoranthene and retene concentrations also increased in the tipi operator after 4.3 hr from the start of fish smoking from 0.16 to 0.22 μg/g creatinine and from <EDL to 0.47 μg/g creatinine, respectively. In all of the urine samples collected after time zero when the operator was burning apple wood, the urinary PAH concentrations decreased over time after an initial spike in concentration after the initial exposure (Figure 3).
Compared to time zero, after 10 hr from the start of smoking salmon with alder wood, urinary PAHs increased for both operators (pyrene[from <EDL to 0.043 μg/g creatinine and from <EDL to 0.07 μg/g creatinine], retene[from 0.029 to 0.06 μg/g creatinine and from <EDL to 0.028 μg/g creatinine]), although fluoranthene concentrations only increased in the smoke shed operator’s urine (from <EDL to 0.032 μg/g creatinine, Figure 3). With alder wood, the retene concentrations were higher than the other PAH concentrations in operators’ urine (2.6 and 0.8 μg/g creatinine, respectively).
3.8 PAH Concentrations in Personal PM2.5 Air Samples Collected During Fish Smoking Activities
Figure 5 shows PAH, high molecular weight PAHs (MW>302), and oxy-PAH concentrations measured in personal PM2.5 samples. OH-PAHs were not detected in the personal PM2.5 samples above the EDLs. When apple wood was burned, personal PM2.5 PAH concentrations were, on average, 16.8 fold higher in the smoke shed than in the tipi (ranging from 5.0 fold for dibenzo[a,c]anthracene to 75.4 fold for 1-methylnaphthalene). The sum of the lower MW PAH concentrations in the personal PM2.5 samples when apple wood was burned was 9.1-fold higher in the smoke shed than in the tipi (6209 ng/m3vs 683 ng/m3, respectively). When alder wood was burned, the personal PM2.5 PAH concentrations were, on average, 4.6-fold higher in the smoke shed than in the tipi (ranging from 1.2 fold for phenanthrene to 8.0 fold for benzo[k]fluoranthene).
Figure 5.

Concentrations of low molecular weight (LMW) PAHs, high molecular weight (HMW) PAHs, and oxy-PAHs (OPAHs) in the tipi and the smoke shed personal PM2.5 samples.
The sum of the higher MW PAH (MW>302) concentrations were 424 ng/m3 for the smoke shed vs 55 ng/m3 for the tipi when apple wood was burned and 259 ng/m3 for the smoke shed vs 12 ng/m3 for the tipi when alder wood was burned (Figure 5). The higher MW PAH concentrations in the personal PM2.5 samples were 2.5% to 12% of the lower MW PAH concentrations in the samples. The average concentration of higher MW PAH in the personal PM2.5 samples was higher for apple wood compared to alder wood (7.7-fold vs21.2-fold, respectively).
Figure S10 shows the concentration profile of the lower MW PAHs, oxy-PAHs and higher MW PAHs in the personal PM2.5 samples across the four combinations of wood and smoking structure types. The lower MW PAHs with the in highest concentration were phenanthrene, fluoranthene and pyrene. Although the concentration of fluoranthene was the highest in all personal PM2.5 samples, a metabolite of fluoranthene (3-OH-Flt) was not identified in any urine samples, suggesting that 3-OH-Flt is not a major metabolite of fluoranthene. This is in agreement with Chetiyanukornkul et al. (2006) who did not detect urinary 3-OH-fluoranthene in an exposed population in Taiwan. Four urinary metabolites of phenanthrene (4-, 3-, 2-, and 1-OH-hydroxyphenanthrene) and one urinary metabolite of pyrene (1-hydroxypyrene) were identified (Figure 3). Although the highest urinary metabolite concentrations were for the hydroxynaphthalenes, the naphthalene concentrations in the personal PM2.5 samples were below the EDL. This discrepancy is likely due to the partitioning of naphthalene primarily to the gas phase and exposure to naphthalene via the gas phase rather than PM2.5(Radonic et al., 2011). The sum of all urinary OH-PAH concentrations followed the pattern Apple × SS Apple × TP>Alder × SS>Alder × TP, while the sum of PAHs in the personal PM2.5 samples followed the pattern Apple × SS>Alder x SS>Apple × TP>Alder × TP. These findings suggest that smoking fish in the tipi with alder wood had the lowest PAH exposure during smoking activities.
Smoking of fish and meats to preserve them is a cultural tradition among the CTUIR, as is eating large amounts of fish. While this activity cannot, therefore, be reduced, the information provided in this manuscript will allow the CTUIR to craft health advice for those engaged in this activity. The partnership between the university and Tribe benefits both the scientific community (advances in analytical methodology) and the Tribe (provides useful health-related information).
Supplementary Material
Acknowledgments
Funding Sources
This publication was made possible in part by grant number P30ES00210 from the National Institute of Environmental Health Sciences (NIEHS), NIH and NIEHS Grant P42 ES016465.
We thank Alex Brewer and Dr. Jennifer Field for conducting creatinine measurements. We thank Steven Wise from NIST for providing urine SRM samples.
Footnotes
Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the NIEHS, NIH.
References
- Adetona O, Sjodin A, Zheng L, Romanoff LC, Aguilar-Villalobos M, Needham LL, et al. Personal Exposure to PM2.5 and Urinary Hydroxy-PAH Levels in Bus Drivers Exposed to Traffic Exhaust, in Trujillo, Peru. Journal of Occupational and Environmental Hygiene. 2012;9:217–229. doi: 10.1080/15459624.2012.666142. [DOI] [PubMed] [Google Scholar]
- Alomirah H, Al-Zenki S, Al-Hooti S, Zaghloul S, Sawaya W, Ahmed N, et al. Concentrations and dietary exposure to polycyclic aromatic hydrocarbons (PAHs) from grilled and smoked foods. Food Control. 2011;22:2028–2035. [Google Scholar]
- Baek SO, Field RA, Goldstone ME, Kirk PW, Lester JN, Perry R. A REVIEW OF ATMOSPHERIC POLYCYCLIC AROMATIC-HYDROCARBONS - SOURCES, FATE AND BEHAVIOR. Water Air and Soil Pollution. 1991;60:279–300. [Google Scholar]
- Barbeau D, Marques M, Maitre A. 3-hydroxybenzo[a]pyrene as a new biomarker of exposure to carcinogenic polycyclic aromatic hydrocarbons. Toxicology Letters. 2009;189:S160–S160. [Google Scholar]
- Becher G, Bjorseth A. DETERMINATION OF EXPOSURE TO POLYCYCLIC AROMATIC-HYDROCARBONS BY ANALYSIS OF HUMAN-URINE. Cancer Letters. 1983;17:301–311. doi: 10.1016/0304-3835(83)90168-4. [DOI] [PubMed] [Google Scholar]
- Bostrom CE, Gerde P, Hanberg A, Jernstrom B, Johansson C, Kyrklund T, et al. Cancer risk assessment, indicators, and guidelines for polycyclic aromatic hydrocarbons in the ambient air. Environmental Health Perspectives. 2002;110:451–488. doi: 10.1289/ehp.110-1241197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campo L, Addario L, Buratti M, Scibetta L, Longhi O, Valla C, et al. Biological monitoring of exposure to polycyclic aromatic hydrocarbons by determination of unmetabolized compounds in urine. Toxicology Letters. 2006;162:132–138. doi: 10.1016/j.toxlet.2005.09.024. [DOI] [PubMed] [Google Scholar]
- Campo L, Fustinoni S, Buratti M, Cirla PE, Martinotti I, Foa V. Unmetabolized polycyclic aromatic hydrocarbons in urine as biomarkers of low exposure in asphalt workers. Journal of Occupational and Environmental Hygiene. 2007;4:100–110. [Google Scholar]
- Campo L, Rossella F, Pavanello S, Mielzynska D, Siwinska E, Kapka L, et al. Urinary profiles to assess polycyclic aromatic hydrocarbons exposure in coke-oven workers. Toxicology Letters. 2010;192:72–78. doi: 10.1016/j.toxlet.2008.12.018. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Updated Tables. Mar, 2013. Fourth National Report on Human Exposure to Environmental Chemicals. [Google Scholar]
- Chetiyanukornkul T, Toriba A, Kameda T, Tang N, Hayakawa K. Simultaneous determination of urinary hydroxylated metabolites of naphthalene, fluorene, phenanthrene, fluoranthene and pyrene as multiple biomarkers of exposure to polycyclic aromatic hydrocarbons. Analytical and Bioanalytical Chemistry. 2006;386:712–718. doi: 10.1007/s00216-006-0628-6. [DOI] [PubMed] [Google Scholar]
- Chiaia AC, Banta-Green C, Field J. Eliminating Solid Phase Extraction with Large-Volume Injection LC/MS/MS: Analysis of Illicit and Legal Drugs and Human Urine Indicators in US Wastewaters. Environmental Science & Technology. 2008;42:8841–8848. doi: 10.1021/es802309v. [DOI] [PubMed] [Google Scholar]
- Crinnion WJ. The CDC Fourth National Report on Human Exposure to Environmental Chemicals: What it Tells Us About our Toxic Burden and How it Assists Environmental Medicine Physicians. Alternative Medicine Review. 2010;15:101–108. [PubMed] [Google Scholar]
- de Alda MJL, Barcelo D. Review of analytical methods for the determination of estrogens and progestogens in waste waters. Fresenius Journal of Analytical Chemistry. 2001;371:437–447. doi: 10.1007/s002160101027. [DOI] [PubMed] [Google Scholar]
- Essumang DK, Dodoo DK, Adjei JK. Polycyclic aromatic hydrocarbon (PAH) contamination in smoke-cured fish products. Journal of Food Composition and Analysis. 2012;27:128–138. [Google Scholar]
- Fan RF, Wang DL, Ramage R, She JW. Fast and Simultaneous Determination of Urinary 8-Hydroxy-2′-deoxyguanosine and Ten Monohydroxylated Polycyclic Aromatic Hydrocarbons by Liquid Chromatography/Tandem Mass Spectrometry. Chemical Research in Toxicology. 2012;25:491–499. doi: 10.1021/tx200517h. [DOI] [PubMed] [Google Scholar]
- Forsberg ND, Stone D, Harding A, Harper B, Harris S, Matzke MM, et al. Effect of Native American Fish Smoking Methods on Dietary Exposure to Polycyclic Aromatic Hydrocarbons and Possible Risks to Human Health. Journal of Agricultural and Food Chemistry. 2012;60:6899–6906. doi: 10.1021/jf300978m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Förster K, Preuss R, Roßbach B, Brüning T, Angerer J, Simon P. 3-Hydroxybenzo[a]pyrene in the urine of workers with occupational exposure to polycyclic aromatic hydrocarbons in different industries. Occupational and Environmental Medicine. 2008;65:224–229. doi: 10.1136/oem.2006.030809. [DOI] [PubMed] [Google Scholar]
- Grova N, Salquebre G, Schroeder H, Appenzeller BMR. Determination of PAHs and OH-PAHs in Rat Brain by Gas Chromatography Tandem (Triple Quadrupole) Mass Spectrometry. Chemical Research in Toxicology. 2011;24:1653–1667. doi: 10.1021/tx2003596. [DOI] [PubMed] [Google Scholar]
- Guillen MD, Sopelana P, Partearroyo MA. Food as a source of polycyclic aromatic carcinogens. Rev Environ Health. 1997;12:133–46. doi: 10.1515/reveh.1997.12.3.133. [DOI] [PubMed] [Google Scholar]
- Hagedorn HW, Scherer G, Engl J, Riedel K, Cheung F, Errington G, et al. Urinary Excretion of Phenolic Polycyclic Aromatic Hydrocarbons (OH-PAH) in Nonsmokers and in Smokers of Cigarettes with Different ISO Tar Yields. Journal of Analytical Toxicology. 2009;33:301–309. doi: 10.1093/jat/33.6.301. [DOI] [PubMed] [Google Scholar]
- Hainaut P, Hollstein M. p53 and human cancer: The first ten thousand mutations. Advances in Cancer Research, Vol 77. 2000;77:81–137. doi: 10.1016/s0065-230x(08)60785-x. [DOI] [PubMed] [Google Scholar]
- Han Y, Xia Y, Zhu P, Qiao S, Zhao R, Jin N, et al. Reproductive hormones in relation to polycyclic aromatic hydrocarbon (PAH) metabolites among non-occupational exposure of males. Science of the Total Environment. 2010;408:768–773. doi: 10.1016/j.scitotenv.2009.11.021. [DOI] [PubMed] [Google Scholar]
- International Agency for Research on Cancer (IARC) Chemical, Environmental and Experimental Data. Vol. 32. World Health Organization; Lyon, France: 1983. Benzo[a]pyrene. In: IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Polynuclear Aromatic Compounds. Part 1; pp. 33–224. [Google Scholar]
- Itoh N, Tao H, Ibusuki T. In-tube silylation in combination with thermal desorption gas chromatography-mass spectrometry for the determination of hydroxy polycyclic aromatic hydrocarbons in water. Analytica Chimica Acta. 2006;555:201–209. [Google Scholar]
- Jacob J, Seidel A. Biomonitoring of polycyclic aromatic hydrocarbons in human urine. Journal of Chromatography B. 2002;778:31–47. doi: 10.1016/s0378-4347(01)00467-4. [DOI] [PubMed] [Google Scholar]
- Jacob P, Wilson M, Benowitz NL. Determination of phenolic metabolites of polycyclic aromatic hydrocarbons in human urine as their pentafluorobenzyl ether derivatives using liquid chromatography-tandem mass spectrometry. Analytical Chemistry. 2007;79:587–598. doi: 10.1021/ac060920l. [DOI] [PubMed] [Google Scholar]
- Jerina DM, Daly JW, Witkop B, Zaltzman P, Udenfrie S. 1,2-NAPHTHALENE OXIDE AS AN INTERMEDIATE IN MICROSOMAL HYDROXYLATION OF NAPHTHALENE. Biochemistry. 1970;9:147. doi: 10.1021/bi00803a019. [DOI] [PubMed] [Google Scholar]
- Jia YL, Stone D, Wang WT, Schrlau J, Tao S, Simonich SLM. Estimated Reduction in Cancer Risk due to PAH Exposures If Source Control Measures during the 2008 Beijing Olympics Were Sustained. Environmental Health Perspectives. 2011;119:815–820. doi: 10.1289/ehp.1003100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jongeneelen FJ. Benchmark guideline for urinary 1-hydroxypyrene as biomarker of occupational exposure to polycyclic aromatic hydrocarbons. Annals of Occupational Hygiene. 2001;45:3–13. [PubMed] [Google Scholar]
- Kishikawa N, Morita S, Wada M, Ohba Y, Nakashima K, Kuroda N. Determination of hydroxylated polycyclic aromatic hydrocarbons in airborne particulates by high-performance liquid chromatography with fluorescence detection. Analytical Sciences. 2004;20:129–132. doi: 10.2116/analsci.20.129. [DOI] [PubMed] [Google Scholar]
- Klotz K, Schindler BK, Angerer J. 1,2-Dihydroxynaphthalene as biomarker for a naphthalene exposure in humans. International Journal of Hygiene and Environmental Health. 2011;214:110–114. doi: 10.1016/j.ijheh.2010.11.003. [DOI] [PubMed] [Google Scholar]
- Landers DH, Simonich SM, Jaffe D, Geiser L, Campbell DH, Schwindt A, et al. The Western Airborne Contaminant Assessment Project (WACAP): An Interdisciplinary Evaluation of the Impacts of Airborne Contaminants in Western US National Parks. Environmental Science & Technology. 2010;44:855–859. doi: 10.1021/es901866e. [DOI] [PubMed] [Google Scholar]
- Leroyer A, Jeandel F, Maitre A, Howsam M, Deplanque D, Mazzuca M, et al. 1-Hydroxypyrene and 3-hydroxybenzo[a]pyrene as biomarkers of exposure to PAH in various environmental exposure situations. Science of the Total Environment. 2010;408:1166–1173. doi: 10.1016/j.scitotenv.2009.10.073. [DOI] [PubMed] [Google Scholar]
- Levin JO. FIRST INTERNATIONAL WORKSHOP ON HYDROXYPYRENE AS A BIOMARKER FOR PAH EXPOSURE IN MAN - SUMMARY AND CONCLUSIONS. Science of the Total Environment. 1995;163:165–168. [PubMed] [Google Scholar]
- Li Z, Mulholland JA, Romanoff LC, Pittman EN, Trinidad DA, Lewin MD, et al. Assessment of non-occupational exposure to polycyclic aromatic hydrocarbons through personal air sampling and urinary biomonitoring. Journal of Environmental Monitoring. 2010;12:1110–1118. doi: 10.1039/c000689k. [DOI] [PubMed] [Google Scholar]
- Li Z, Sandau CD, Romanoff LC, Caudill SP, Sjodin A, Needham LL, et al. Concentration and profile of 22 urinary polycyclic aromatic hydrocarbon metabolites in the US population. Environmental Research. 2008;107:320–331. doi: 10.1016/j.envres.2008.01.013. [DOI] [PubMed] [Google Scholar]
- Li Z, Sjoedin A, Romanoff LC, Horton K, Fitzgerald CL, Eppler A, et al. Evaluation of exposure reduction to indoor air pollution in stove intervention projects in Peru by urinary biomonitoring of polycyclic aromatic hydrocarbon metabolites. Environment International. 2011;37:1157–1163. doi: 10.1016/j.envint.2011.03.024. [DOI] [PubMed] [Google Scholar]
- Luan TG, Fang SH, Zhong Y, Lin L, Chan SMN, Lan CY, et al. Determination of hydroxy metabolites of polycyclic aromatic hydrocarbons by fully automated solid-phase microextraction derivatization and gas chromatography-mass spectrometry. Journal of Chromatography A. 2007;1173:37–43. doi: 10.1016/j.chroma.2007.10.038. [DOI] [PubMed] [Google Scholar]
- Mattarozzi M, Musci M, Careri M, Mangia A, Fustinoni S, Campo L, et al. A novel headspace solid-phase microextraction method using in situ derivatization and a diethoxydiphenylsilane fibre for the gas chromatography-mass spectrometry determination of urinary hydroxy polycyclic aromatic hydrocarbons. Journal of Chromatography A. 2009;1216:5634–5639. doi: 10.1016/j.chroma.2009.05.072. [DOI] [PubMed] [Google Scholar]
- Moon J, Smith TJ, Tamaro S, Enarson D, Fadl S, Davison AJ, et al. Trace metals in scalp hair of children and adults in three Alberta indian villages. Science of the Total Environment. 1986;54:107–125. doi: 10.1016/0048-9697(86)90259-7. [DOI] [PubMed] [Google Scholar]
- Motorykin O, Matzke MM, Waters KM, Simonich SLM. Association of Carcinogenic Polycyclic Aromatic Hydrocarbon Emissions and Smoking with Lung Cancer Mortality Rates on a Global Scale. Environmental Science & Technology. 2013;47:3410–3416. doi: 10.1021/es305295d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mucha AP, Hryhorczuk D, Serdyuk A, Nakonechny J, Zvinchuk A, Erdal S, et al. Urinary 1-hydroxypyrene as a biomarker of PAH exposure in 3-year-old Ukrainian children. Environmental Health Perspectives. 2006;114:603–609. doi: 10.1289/ehp.7898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neff JM. Polycyclic aromatic hydrocarbons in the aquatic environment and cancer risk to aquatic organisms and man. Symposium: Carcinogenic Polynuclear Aromatic Hydrocarbons in the Marine Environment. 1978:385–409. [Google Scholar]
- NIST. SRM 3672 - Organic Contaminants in Smokers’ Urine (Frozen) 2013a;2014 [Google Scholar]
- NIST. SRM 3673 - Organic Contaminants in Non-Smokers’ Urine (Frozen) 2013b;2014 [Google Scholar]
- Onyemauwa F, Rappaport SM, Sobus JR, Gajdosova D, Wu RA, Waidyanatha S. Using liquid chromatography-tandem mass spectrometry to quantify mono hydroxylated metabolites of polycyclic aromatic hydrocarbons in urine. Journal of Chromatography B-Analytical Technologies in the Biomedical and Life Sciences. 2009;877:1117–1125. doi: 10.1016/j.jchromb.2009.02.067. [DOI] [PubMed] [Google Scholar]
- Primbs T, Piekarz A, Wilson G, Schmedding D, Higginbotham C, Field J, et al. Influence of Asian and Western United States urban areas and fires on the atmospheric transport of polycyclic aromatic hydrocarbons, polychlorinated biphenyls, and fluorotelomer alcohols in the Western United States. Environmental Science & Technology. 2008;42:6385–6391. doi: 10.1021/es702160d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radonic J, Miloradov MV, Sekulic MT, Kiurski J, Djogo M, Milovanovic D. The octanol-air partition coefficient, K-OA as a predictor of gas-particle partitioning of polycyclic aromatic hydrocarbons and polychlorinated biphenyls at industrial and urban sites. Journal of the Serbian Chemical Society. 2011;76:447–458. [Google Scholar]
- Romanoff LC, Li Z, Young KJ, Blakely NC, Patterson DG, Sandau CD. Automated solid-phase extraction method for measuring urinary polycyclic aromatic hydrocarbon metabolites in human biomonitoring using isotope-dilution gas chromatography high-resolution mass spectrometry. Journal of Chromatography B-Analytical Technologies in the Biomedical and Life Sciences. 2006;835:47–54. doi: 10.1016/j.jchromb.2006.03.004. [DOI] [PubMed] [Google Scholar]
- Rossbach B, Preuss R, Letzel S, Drexler H, Angerer J. Biological monitoring of occupational exposure to polycyclic aromatic hydrocarbons (PAH) by determination of monohydroxylated metabolites of phenanthrene and pyrene in urine. International Archives of Occupational and Environmental Health. 2007;81:221–229. doi: 10.1007/s00420-007-0209-9. [DOI] [PubMed] [Google Scholar]
- Schaeffer DJ, Dellinger JA, Needham LL, Hansen LG. Serum PCB profiles in Native Americans from Wisconsin based on region, diet, age, and gender: Implications for epidemiology studies. Science of the Total Environment. 2006;357:74–87. doi: 10.1016/j.scitotenv.2005.04.030. [DOI] [PubMed] [Google Scholar]
- Schummer C, Delhomme O, Appenzeller BMR, Wennig R, Millet M. Comparison of MTBSTFA and BSTFA in derivatization reactions of polar compounds prior to GC/MS analysis. Talanta. 2009;77:1473–1482. doi: 10.1016/j.talanta.2008.09.043. [DOI] [PubMed] [Google Scholar]
- Smith CJ, Huang WL, Walcott CJ, Turner W, Grainger J, Patterson DG. Quantification of monohydroxy-PAH metabolites in urine by solid-phase extraction with isotope dilution-GC-MS. Analytical and Bioanalytical Chemistry. 2002;372:216–220. doi: 10.1007/s00216-001-1123-8. [DOI] [PubMed] [Google Scholar]
- St Helen G, Goniewicz ML, Dempsey D, Wilson M, Jacob P, Benowitz NL. Exposure and Kinetics of Polycyclic Aromatic Hydrocarbons (PAHs) in Cigarette Smokers. Chemical Research in Toxicology. 2012;25:952–964. doi: 10.1021/tx300043k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strickland P, Kang DH. Urinary 1-hydroxypyrene and other PAH metabolites as biomarkers of exposure to environmental PAH in air particulate matter. Toxicology Letters. 1999;108:191–199. doi: 10.1016/s0378-4274(99)00089-2. [DOI] [PubMed] [Google Scholar]
- Tonne CC, Whyatt RM, Camann DE, Perera FP, Kinney PL. Predictors of personal polycyclic aromatic hydrocarbon exposures among pregnant minority women in New York City. Environmental Health Perspectives. 2004;112:754–759. doi: 10.1289/ehp.5955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. National Institutes of Health. Clean catch urine sample. Vol. 2012 U.S. National Library of Medicine; 2014. [Google Scholar]
- U.S. EPA. Integrated Risk Information System (IRIS) Vol. 1992 US Environmental Protection Agency; 2011. [Google Scholar]
- U.S. EPA; U.S. Environmental Protection Agency, editor. Method 8280A. Washington, DC: 1996. The analysis of polychlorinated dibenzo-p-dioxins and polychlorinated dibenzofurans by high-resolution gas chromatography/low resolution mass spectrometry (HRGC/LRMS) [Google Scholar]
- Usenko S, Smonich SLM, Hageman KJ, Schrlau JE, Geiser L, Campbell DH, et al. Sources and Deposition of Polycyclic Aromatic Hydrocarbons to Western US National Parks. Environmental Science & Technology. 2010;44:4512–4518. doi: 10.1021/es903844n. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veyrand B, Sirot V, Durand S, Pollono C, Matchand P, Dervilly-Pinel G, et al. Human dietary exposure to polycyclic aromatic hydrocarbons: Results of the second French Total Diet Study. Environment International. 2013;54:11–17. doi: 10.1016/j.envint.2012.12.011. [DOI] [PubMed] [Google Scholar]
- Viau C, Lafontaine M, Payan JP. Creatinine normalization in biological monitoring revisited: the case of 1-hydroxypyrene. International Archives of Occupational and Environmental Health. 2004;77:177–185. doi: 10.1007/s00420-003-0495-9. [DOI] [PubMed] [Google Scholar]
- Wang J, Chen S, Tian M, Zheng X, Gonzales L, Ohura T, et al. Inhalation Cancer Risk Associated with Exposure to Complex Polycyclic Aromatic Hydrocarbon Mixtures in an Electronic Waste and Urban Area in South China. Environmental Science & Technology. 2012;46:9745–9752. doi: 10.1021/es302272a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang LR, Wang Y, Chen JW, Guo LH. A structure-based investigation on the binding interaction of hydroxylated polycyclic aromatic hydrocarbons with DNA. Toxicology. 2009;262:250–257. doi: 10.1016/j.tox.2009.06.015. [DOI] [PubMed] [Google Scholar]
- Wang WT, Jariyasopit N, Schrlau J, Jia YL, Tao S, Yu TW, et al. Concentration and Photochemistry of PAHs, NPAHs, and OPAHs and Toxicity of PM2.5 during the Beijing Olympic Games. Environmental Science & Technology. 2011;45:6887–6895. doi: 10.1021/es201443z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei Y, Lin Y, Zhang A-Q, Guo L-H, Cao J. Evaluation of the noncovalent binding interactions between polycyclic aromatic hydrocarbon metabolites and human p53 cDNA. Science of the Total Environment. 2010;408:6285–6290. doi: 10.1016/j.scitotenv.2010.09.024. [DOI] [PubMed] [Google Scholar]
- Xu SS, Liu WX, Tao S. Emission of polycyclic aromatic hydrocarbons in China. Environmental Science & Technology. 2006;40:702–708. doi: 10.1021/es0517062. [DOI] [PubMed] [Google Scholar]
- Xu X, Cook RL, Ilacqua VA, Kan H, Talbott EO, Kearney G. Studying associations between urinary metabolites of polycyclic aromatic hydrocarbons (PAHs) and cardiovascular diseases in the United States. Science of the Total Environment. 2010;408:4943–4948. doi: 10.1016/j.scitotenv.2010.07.034. [DOI] [PubMed] [Google Scholar]
- Xu X, Hu H, Kearney GD, Kan H, Sheps DS. Studying the effects of polycyclic aromatic hydrocarbons on peripheral arterial disease in the United States. Science of the Total Environment. 2013;461–462:341–347. doi: 10.1016/j.scitotenv.2013.04.089. [DOI] [PubMed] [Google Scholar]
- Xue J, Zartarian VG, Liu SV, Geller AM. Methyl mercury exposure from fish consumption in vulnerable racial/ethnic populations: Probabilistic SHEDS-Dietary model analyses using 1999–2006 NHANES and 1990–2002 TDS data. Science of the Total Environment. 2012;414:373–379. doi: 10.1016/j.scitotenv.2011.10.010. [DOI] [PubMed] [Google Scholar]
- Zhong Y, Carmella SG, Upadhyaya P, Hochalter JB, Rauch D, Oliver A, et al. Immediate Consequences of Cigarette Smoking: Rapid Formation of Polycyclic Aromatic Hydrocarbon Diol Epoxides. Chemical Research in Toxicology. 2011;24:246–252. doi: 10.1021/tx100345x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.