Abstract
Purpose
To identify which patients and canines are involved in dog bites of the head and neck, and how they impact health systems.
Materials and Methods
This is a single center, retrospective cohort study conducted from January 2012 to June 2013 from an academic, tertiary care center situated between multiple suburban and urban communities. Patients were identified by queried search for all bite-related diagnoses codes.
Results
334 unique dog bites were identified, of which 101 involved the head and neck. The mean patient age was 15.1 years ± 18.1. Of the more than 8 different breeds identified, one-third were caused by pit bull terriers and resulted in the highest rate of consultation (94%) and had 5 times the relative rate of surgical intervention. Unlike all other breeds, pit bull terriers were relatively more likely to attack an unknown individual (+31%), and without provocation (+48%). Injuries of the head and neck had an average follow-up of 1.26 ± 2.4 visits, and average specialty follow-up of 3.1 ± 3.5 visits.
Conclusions
The patients most likely to suffer dog bite injuries of the head and neck are children. Although a number of dog breeds were identified, the largest group were pit bull terriers, whose resultant injuries were more severe and resulted from unprovoked, unknown dogs. More severe injuries required a greater number of interventions, a greater number of inpatient physicians, and more outpatient follow-up encounters. Healthcare utilization and costs associated with dog bites warrant further investigation.
Introduction
Animal bites are a preventable public health issue, and yet these injuries have been on the rise. Canine bites became a national concern with the 1985 CDC release that reported as many as 4.7 million Americans are annually bitten by dogs.[1] Of these 4.7 million people, approximately 800,000 dog bite victims seek medical care.[1] At the time of this report, dog bites were not a new issue, this CDC report was one of the first times this type of injury shifted from a local or regional concern to the national stage.[2] Despite this national attention, the rate of dog ownership has continued to increase. In 2001, Shuler and her colleagues estimated that nearly 70 million dogs are owned in the United States, and that over 112 million people, or 40% of the population, have at least one dog in their home.[3] With this increase in ownership, it is now estimated that lifetime risk of being bitten by a dog approaches 50%.[4]
Dog bites account for over 80% of mammalian bites.[5] Dog bites, unlike the bites of cats, rats or human are crush injuries.[2, 6] At first glance, these injuries can appear less severe than wounds from these other bite because the superficial tissue may remain intact. While the dermis may not be broken, the underlying tissue may still be devitalized by crushing, tearing, and/or avulsing the supporting blood supply.[6] The force applied by a dog's jaw is often estimated to be between 300-450 pounds per square inch (PSI).[5, 7] There are reports of some canine bites having forces of upwards of 1,800 PSI, but the primary sources for this claim cannot be verified. [8-11] The force generated from some dog bites can fracture bone, dependent on the patient, dog breed and site of bite. [12, 13]
Dog bites injuries found in the head and neck disproportionately affect children, and have been previously reported to account for 3-4% of all pediatric emergency visits, and up to 40% of all pediatric traumas. [14-18] These injuries can lead to disfiguring scars and lengthy treatments. The need for facial plastic and reconstructive surgery and scar revisions for these injuries has been previously reported to be as high as 77% for these patients.[7] The treatment of dog bite injuries has been reported as the 5th most common ICD-9 code used by plastic surgeons.[19] Primary closure of open dog bite injuries of the head and neck is an accepted treatment due to the significant morbidity associated with scarring from healing from secondary intention. [20-25]
Due to the significant morbidity and controversy surrounding dog bite injuries, this investigation was initiated to identify which patients and canines are involved in these injuries of the head and neck, and how these injuries are currently treated. The objectives of this study include the following: 1) describe the patient population that suffer dog bites in the head and neck, 2) determine the dog breeds and circumstances responsible for these head and neck injuries, and 3) evaluate the current treatment and follow-up care associated with dog bite injuries of the head and neck. We sought to test the following hypotheses: 1) The patients who present with dog bite injuries of the head and neck will be significantly younger, than those bitten in other anatomical locations. 2) The dogs responsible for these injuries will be known to the patient and will be more likely to bite these patients after they are provoked. 3) We further hypothesized that the most severely injured patients would require significantly more resources, measured by consultation, operations, and follow-up. .
Materials and Methods
This is a single center retrospective cohort study conducted using patient data from January 2012 through June 2013. The study was performed at the University of California Davis Health System, a public, academic, tertiary care center, which is situated between multiple suburban and urban communities in Sacramento, California. UC Davis is one of three trauma centers in the greater Sacramento area, and is the sole Level 1 Trauma Center for a catchment area of over two-million people. Prior to the initiation of this study it was approved under the supervision of the UC Davis Institutional Review Board.
Patients in the UC Davis Electronic Medical Record (EMR) were identified by queried search for all bite-related chief complaints and bite-related diagnoses codes (Emergency Department (ED) and/or admit). Patients with non-dog bite injuries were excluded from the study. For each encounter, the following information was extracted from the EMR: date of service, medical record number, name, age, sex, length of stay, chief complaint, diagnosis code, location of incident, insurance provider, and discharge date and time. Further data was extracted from the primary encounter narrative and all subsequent follow-up visits. This extracted data included: time of incident, breed, bodily location of injury, dog's vaccination status, consultations, interventions, inpatient and outpatient antibiotics, relation of dog to patient, circumstances associated with the bite, tetanus and rabies vaccine administration, complications, and follow-up visit encounters. For clarity, the site of injury was dichotomized to general population (GP) of patients where bites affecting the body (including injuries of the head and neck) and those bites of only the head and neck region (H&N).
The Dog Bite Complication Index (DBCI, Table 1), a scale created a prior to this investigation, was developed for the purpose of evaluating dog bites on any anatomic portion of the body. We created the scale for the entire body because, to our knowledge, one had not previously developed and we intend to use this scale to compare dog bites and treatments in different anatomic locations. The scale was informed by the work of Lackmann et al., who previously developed a scale for categorizing facial dog bit injuries.[23] Lackmann's scale has previously been used by a number of authors to control for injury when comparing various treatment and surgical interventions for injuries of the head and neck.[5, 7, 13, 26] We also incorporated the efforts of Dire et al. and Cummings in order to determine anatomic locations at highest risk for complication following dog bite. [27, 28]
Table 1. Dog Bite Complication Index.
| Label | Description | Score |
|---|---|---|
| Minor |
|
1 |
| Mild |
|
2 |
| Moderate |
|
3 |
| Severe |
|
4 |
Statistical analysis was performed using RStudio Version 0.98 (RStudio IDE, Boston, Massachusetts). Means are reported with the standard deviation (SD). The data set was evaluated using the Student t-test, Chi-squared, two-tailed population proportionality test, and generalized linear regression. Significance was determined with P values less than 0.05.
Results
Excluding insect and human bites, 421 charts returned from the query of the UC Davis EMR. Of those charts, 62 were identified as non-dog bites and 26 were return visits to the ED, thus, yielding a total of 334 unique dog bites. Of these 334 bites, 101 involved the head and neck (Figure 1). The demographic data for these patients can be found in Table 2. The mean age of the patients with head and neck bites was 15.1 years ± 18.1 (range 11 months to 73 years, median of 6). This value is significantly less than the general dog bite population (t-test, p <0.0001) where the mean age was 28.6 years ± 21.5 (range 11 months to 95 years, median of 26). Of these patients with head and neck bite injuries, 57% of them were below the age of 10, and these bites to the head and neck accounted for 70% of all the dog bite injuries experienced by individuals under the age of 18. The gender distribution was equal in the bites of the head and neck group (male, n=47; female, n=53), while the general population of dog bites trended towards men (men, n=186; women, n=147) (Test of Equal Proportions, p<0.05).
Figure 1. Flow Chart of Enrolled Patients.
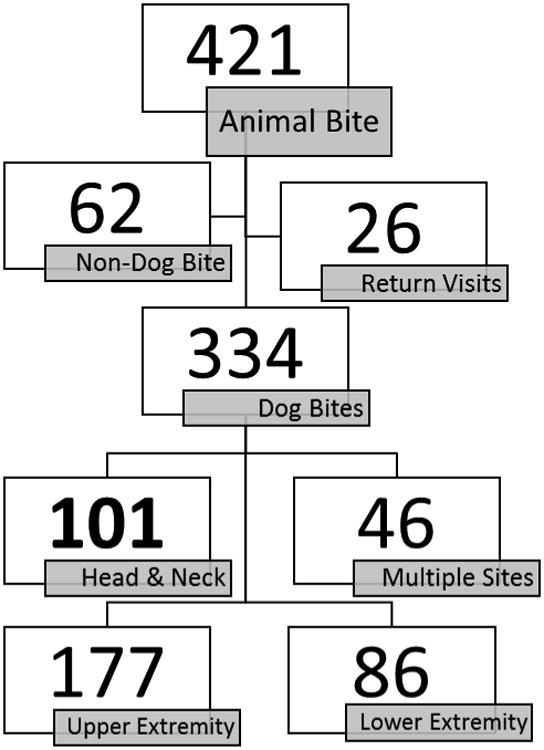
This flow chart graphically displays how select patients were removed for data collection and analysis.
Table 2. Patient Demographic Data+.
| GP Bites | H&N Bites | P value | |
|---|---|---|---|
| N | 334 | 101 | |
| Sex | |||
| Male | 47 | 186 | <0.05a |
| Female | 53 | 147 | |
| Age (Years) | |||
| Mean | 28.6 ± 18.1 | 15.1 ± 18.1 | < 0.0001b |
| Range | 0.92 – 95 | 0.92 – 73 | |
| Median | 26 | 6 | |
| Breed | |||
| Pit Bull | 114 (34%) | 32 (32%) | |
| Police Dog* | 21 (6%) | 0 (0%) | |
| German Shepard | 14 (4%) | 5 (5%) | |
| Chihuahua | 10 (3%) | 3 (3%) | |
| Retriever | 8 (2%) | 6 (6%) | |
| Boxer | 8 (2%) | 4 (4%) | |
| Rottweiler | 8 (2%) | 3 (3%) | |
| All Other | 28 (8%) | 14 (14%) | |
| Not Reported | 123 (37%) | 34 (34%) | |
| Circumstance | |||
| Provoked | 84 (25%) | 40 (40%) | |
| Unprovoked | 134 (7%) | 27 (27%) | |
| Police Animal* | 22 (40%) | 0 (0%) | |
| Not Reported | 94 (28%) | 33 (33%) | |
| Relationship | |||
| Known | 197 (59%) | 73 (72%) | |
| Unknown | 87 (26%) | 16 (16%) | |
| Police Dog* | 28 (8%) | 4 (4%) | |
| Not Reported | 22 (7%) | 7 (7%) | |
| DBCI | |||
| Mean | 1.83 ± 1.22 | 2.63 ± 1.04 | <0.0001c |
| Median | 2.0 | 3.0 |
Results are listed with standard deviation
Police Dog induced injuries were extracted from reporting because they do not represent normal daily experiences
Test of Equal proportions
t-Test
χ2 test
More than 10 different breeds were identified in the chart. In patients with dog bites to the head and neck, pit bull terriers composed the largest portion of the plurality (32%), with the next most common breed being retrievers (6%). When the population of head and neck dog bites were taken as a whole, there was no relationship between these bites and whether or not they occurred provoked or unprovoked. In the population of patients bitten by pit bulls; however, pit bull terriers were significantly more likely to bite a patient without provocations (χ2, p <0.05). In the population of head and neck dog bites, the patient was more likely to be bitten by a dog they owned, or knew rather than a strange dog (χ2, p <0.0001). In the patients bitten by pit bull terriers however, there was no significance difference between known or unknown individuals in terms of bite rate.
Dog bite treatments were evaluated on the rate of consultation required, intervention required, and antibiotic used. All patients with dog bites were grouped by severity and likelihood of complications using the DBCI. By convention, all injuries that involve the head and neck fell into the mild, moderate, or severe categories. The results of the general dog bite population, and the head and neck bite population can be seen in Table 3. The only significant relationship in Table 3 is found in the general dog bite population between inpatient antibiotics and total number of follow-up visits in the Minor Severity category (Linear Regression Model, p<0.005). The most common complications seen were pain control, infection and wound breakdown. The complication rates for injuries found in the head and neck were similar across intervention type: not requiring closure (6%), repaired in the ED (8%), and repaired in the operative suite (10%). The results failed to reject the null hypothesis that use of antibiotics had an effect on the observed complication rate.
Table 3. Intervention Rate, Antibiotics, and Follow-up Care for Dog Bites+.
| Consultation | No Intervention | ED Wound Closure | Operative Closure | Inpatient Antibiotics* | Outpatient Total Pills | Outpatient Follow-Up [Number of Encounters) | |
|---|---|---|---|---|---|---|---|
| GP Bites | |||||||
| Minor | 18% | 92% | 5% | 0% | 0.56 ± 0.71 | 11.85 ± 11.55 | 0.44 ± 1.12 |
| Mild | 27% | 66% | 28 % | 2% | 0.767 ± 0.61 | 13.79 ± 7.93 | 0.67 ± 2.32 |
| Moderate | 79% | 19% | 56% | 21% | 1.19 ± 1.00 | 15.29 ± 9.76 | 1.08 ± 1.51 |
| Severe | 100% | 11% | 33% | 53% | 1.72 ± 1.34 | 13.0 ± 10.81 | 2.61 ± 3.67 |
| H&N Bites | |||||||
| Minor | -------------- | -------------- | -------------- | -------------- | -------------- | -------------- | -------------- |
| Mild | 16% | 47% | 47% | 3% | 0.47 ± 0.614 | 11.06 ± 8.13 | 0.5 ± 0.75 |
| Moderate | 79% | 11% | 66% | 21% | 1.11 ± 1.1 | 14.58 ± 9.56 | 1.1 ± 1.56 |
| Severe | 100% | 15% | 35% | 50% | 1.45 ± 1.19 | 12.85 ± 10.90 | 3.30 ± 4.53 |
GP = General Population, patients who presented with bite injuries to all anatomic areas, including head and neck H&N = Head and Neck, patients who present with dog bit injuries in the head and neck only
This table list standard deviations
This is a list of the different types of antibiotics. The current data set did not have total number of doses.
Not included in Table 3 are the subgroup of injuries caused by pit bull terriers. Bites from pit bull terriers were more severe than those of other dogs, with a mean DBCI of 3.2 compared to 2.3 (t-test, p<0.0001). Bites from pit bull terriers had a significantly higher rate of consultation (χ2, p< 0.0001) when compared to other breeds, receiving specialty care in 94% of the cases and in 50% of the cases, respectively. Injuries from pit bull terrier bites were significantly more like to require surgical repair (χ2, p< 0.05), and had five times the rate of operative repair when compared to other breeds.
Dog bite injuries in the head and neck returned to the medical center for a mean number of 1.26 ± 2.5 follow-up encounters. The percentage of patients returning for follow-up care was commensurate to the injury severity as categorized by the DBCI, increasing progressively from minor (GP 16%; H&N Not Applicable), to mild (GP 31%; H&N 38%), to moderate (GP 48%; H&N 53%), to severe (GP 67%; H&N 70%). As would be expected, the average number of follow-up appointments also followed this progression (Table 3). Not included in Table 3, is the follow-up by practice type. Individuals who sought primary care follow-up returned for a mean of 1.29 ± 0.76 visits. Those who received there follow-up care from the emergency department received 1.57 ± 0.53 follow up encounters. Individuals who followed up with specialty care, defined as otolaryngology-head and neck surgery, facial plastic and reconstructive surgery, plastic surgery, or ophthalmology, returned for an average of 3.11 ± 3.51 encounters. The average severity of the injuries, as measured using the DCBI, were 1.86±0.90, 2.9±0.90, and 3.2±0.69 for primary care, emergency medicine care, and specialty care respectively. When controlling for injury severity, there was not a significant relationship between length of follow-up and encounter specialty (ANOVA, p = 0.0701).
Discussion
Our first objective was to better characterize the patient population that suffers dog bites of the head and neck due to the paucity of recent studies. In this investigation the patients who were bitten by dogs in the head or neck were more likely to be children under the age of ten, with an equal to slight disposition towards girls than boys. These results agree with previous studies evaluating canine bites at tertiary medical centers.[7, 13, 21, 22]
The key finding from our second objective, determining the dogs responsible for bites, is the importance of pit bull terriers in patients with dog bites of the head and neck. The findings of this study are consistent with and extend from previous publications.[5, 7, 11-13, 16, 21, 22, 29] Dog bites from pit bull terriers, compared to bites from all other dogs are more common, more severe, and not related to the dog being provoked. Taken as a whole all other breeds are more likely to bite their owners or other known individuals, either provoked or unprovoked. Pit bull terriers, to the contrary, were found to be more likely to bite a stranger without provocation. Also of note, of the dog bites reported to the Sacramento City Clerk, 204 of the 622 were perpetrated by pit bull terriers.[30] We recognize that the observations of the dog breed and circumstances of dog bites are likely influenced by confounding factors other than just dog breed. Some of these factors may include: 1) treatment or training of dog by owners as protective guard dogs, 2) relative distribution of certain dog breeds in urban, suburban, and rural areas, and 3) the various typical social constructs related to dog ownership.
The third objective of this investigation was to assess the resource used during the treatment of dog bite injuries, with the hypothesis that the most severely injured patients would have a significantly higher requirement for care. With the introduction of the DCBI, this is the first time that the resource utilization of dog bite injuries in the head and neck has been evaluated and compared to the dog bite injuries in other anatomical areas. The results of this investigation show that the more severe injuries did indeed require increased care, as measured by consultation, surgical intervention, and total number of follow-up visits and that this was consistent between anatomic locations.
As expected, the requirement of care gradually rose as the severity of injury increased, but the difference in health care utilization observed between moderate and severe injuries was striking. This observed difference may be due to a fundamental difference between the moderate and severe injury classifications. Intrinsic to the DCBI, severe injuries were characterized by tissue loss (Table 1) which may have required increased follow-up as the injury healed by secondary intention. Regardless of the severity of the presenting injury, we observed that patients who were seen by specialists, tended to have more follow-up encounters than patients who sought care from their primary care physician or emergency physician. While this observation is not statistically significant, the trend speaks to increased system utilization and health care costs. To our knowledge, our preliminary findings on dog bite severity and health system utilization has not been previously studied, and warrants further investigation.
In our evaluation of dog bite follow-up and management patterns, we found that the use of antibiotics did not appear to correlate with either the severity of the injury, or likelihood of complication. The length of treatment was not standardized in any group, and, based upon the literature, the utility of prophylactic antibiotics is unclear.[24, 31, 32] In the primary analysis of the data there was a strong correlation between the number of follow-up encounters and inpatient antibiotic usage. This relationship appears to be a surrogate for injury severity, as those who had more severe injuries, and increased interventions received more and varied types of antibiotics.
This retrospective chart review has a number of key limitations. Breed, relationship to the offending dog, and circumstances surrounding the presenting injury are self-reported, and as such it is likely that some of the dog breeds have been incorrectly assigned due to either information or recall bias. While these concerns are common to this study design, the impact of these biases on the reported results is unknown. Other limitations of this study include that the datasets we used were not built for research purposes, and at times lack either relevant patient or animal information. In order to mitigate these concerns we are expanding to not only other area health systems, but have also obtained county records for comparison. These records include dog licensure information, and the animal care service records of Sacramento County for the past three years. While none of these data sets are complete, the combination should give an indication of local trends in ownership and breed.
At this time, neither the local, state nor national burden of head neck dog bite injuries is known. The most recent study undertaken to assess the communal burden of this injury type was conducted in 1979, and had significant flaws as detailed in Appendix A. Furthermore, registries of these injuries, such as the Sacramento County Clerk's record of Dog Bites and Animal Registration, are incomplete at best.[30] Although the catchment area for dog bites in this study includes a broad range of socioeconomic and geographic areas, there are likely contextual factors that are unmeasured in this or any retrospective study. Certain areas may contain more of one type of popular dog breeds, which may undergo dog training (protective guard dog) that would affect the geographic distribution of dogs and the dog bites that occur. In future studies, we hope to better control for these confounding variables when evaluating the characteristics of the patients, the attacking dog, and the circumstances of the injury. Overall, this expanded data set will inform efforts to improve dog bite classification, management, and preventive measures.
Conclusion
Dog bites are a significant public health concern, and may account for 40% of all pediatric traumas.[16] In this investigation, we found that dog bites of the head and neck disproportionately affected pediatric patients. Among the dog breeds responsible for these head and neck injuries, one-third involved pit bull terriers, whose resulting injuries were more severe, had nearly twice the requirement for specialty consultation, and had higher rate of surgical exploration and repair. Severe injuries required significantly more resources, including specialty consultation, surgical intervention, and follow-up. The impact and costs of dog bites to communities and health systems are relatively unknown. In future investigations we hope to measure the resource utilization in an effort to improve the characterization of the patient-specific and dog related factors that contribute to the dog bites. Ultimately, we intend to improve standardized early treatment and develop preventive measures for these resource intense injuries.
Appendix A
One of the unexpected findings in reviewing the available literature is that the true current burden of head and neck dog bites is unknown. In the literature on dog bites of the head and neck, a single study by Karlson is often cited for the burden of this injury.[5, 11-13, 33] In this investigation, the totality of pediatric head and neck dog bites was reported for the county surrounding Madison, Wisconsin (Dane County). In their analysis they extrapolated their findings, of 133 dog bites per 100,000 children under the age of 10, to the general United States population. At the time of the study, 1979, there were 33 million children under 10 years old, leading to the statistic of 44,000 children who suffer dog bites of the head and neck. A serious flaw of this oftquoted study is the assumption that Dane County is representative of the entirety of the United States.
In the years since this study, the risk of dog bites has been theorized to be related to population density, in addition to poverty status.[2-5, 34-36] While the population density is not available for Dane County in 1980, it is possible to calculate the density for Madison, the county's largest and most population dense city. Using the 1980 census data, the urban population density of Madison Wisconsin would have been 78 people per square mile.[37, 38] At the same time, nationally, 74% of the country lived in urban areas with a population density of 182 people per square mile. Furthermore, the poverty level of Dane county and Wisconsin as a state were 9.68 and 7.54, respectively, lower than the nationally reported poverty rate of 12.40.[39] Since Karlson's investigation, there has not been an assessment of the communal burden of head and neck dog bites. Since 1980, the United States Population has grown by nearly 100 million people and the average population density of urban areas is now 283 people per mile.[38] Due to this gap in knowledge, we are currently developing a collaboration with other Northern California health systems for the purpose of creating a complete data set of these injuries. We hope, with the benefit of this data, to be able to assess the true burden of these injuries and to develop community initiatives directed towards dog bite prevention.
Footnotes
- Study concept and design: O'Brien, Andre, Squires, and Robinson.
- Acquisition of data: O'Brien, and Andre.
- Analysis and interpretation of data: O'Brien and Andre.
- Drafting of the manuscript: O'Brien and Andre.
- Critical revision of the manuscript: O'Brien, Andre, Squires, Robinson, and Tollefson.
- Statistical analysis and graphic design: O'Brien and Andre.
- Administrative, technical, and material support: O'Brien, Andre, and Tollefson.
- Study supervision: O'Brien, Andre, and Tollefson.
Conflict of Interest Disclosures: O'Brien was funded by NIH 5TL1TR000133-08 T32 grant during the course of this study. No other conflicts of interest.
Previous Presentation: Portions of this data set were presented as posters at the UC Davis Medical Student Research Poster Day, UC Davis. March 6, 2014 and the Association for Clinical and Translational Science Annual Meeting, April 10, 2014. In both instances the poster were not published or made available online.
Additional Contributions: Beth Morris MPH, UC Davis department of Emergency Medicine, retrieved medical records for the study. Brian Andre, Andre & Associates of Orange County, assisted with typesetting and preparation of the figures used in this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Daniel C. O'Brien, Email: daniel.obrien@ucdmc.ucdavis.edu, Department of Medical Education, University of California – Davis Medical Center, Sacramento, CA, U.S.A. Contribution: Project design, data acquisition and analysis, statistical evaluation, and manuscript development. Conflict of Interest: funded in full by T32 Institutional Grant from July 2013 – June 2014.
Tyler B Andre, Email: tylerbandre@gmail.com, Department of Emergency Medicine, Western Michigan University, Kalamazoo, MI, U.S.A, Department of Medical Education, University of California – Davis Medical Center, Sacramento, CA, U.S.A. Contribution: Project design, data acquisition and analysis, graphic design, and manuscript development. Conflict of Interest: None.
Aaron D. Robinson, Email: aaron.robinson@ucdmc.ucdavis.edu, Department of Otolaryngology Head and Neck Surgery, University of California – Davis Medical Center, Sacramento, CA, U.S.A. Contribution: Project design and critical review of the manuscript Conflict of Interest: None.
Lane D. Squires, Email: lane.squires@ucdmc.ucdavis.edu, Department of Otolaryngology Head and Neck Surgery, University of California – Davis Medical Center, Sacramento, CA, U.S.A. Contribution: Project design and critical review of the manuscript Conflict of Interest: None.
References
- 1.Sosin DM, Sacks JJ, Sattin RW. Causes of nonfatal injuries in the United States, 1986. Accident; analysis and prevention. 1992;24(6):685–7. doi: 10.1016/0001-4575(92)90022-b. Epub 1992/12/01. [DOI] [PubMed] [Google Scholar]
- 2.Harris D, Imperato PJ, Oken B. Dog bites--an unrecognized epidemic. Bulletin of the New York Academy of Medicine. 1974;50(9):981–1000. Epub 1974/10/01. [PMC free article] [PubMed] [Google Scholar]
- 3.Shuler CM, DeBess EE, Lapidus JA, Hedberg K. Canine and human factors related to dog bite injuries. Journal of the American Veterinary Medical Association. 2008;232(4):542–6. doi: 10.2460/javma.232.4.542. Epub 2008/02/19. [DOI] [PubMed] [Google Scholar]
- 4.Pfortmueller CA, Efeoglou A, Furrer H, Exadaktylos AK. Dog bite injuries: primary and secondary emergency department presentations--a retrospective cohort study. TheScientificWorldJournal. 2013;2013:393176. doi: 10.1155/2013/393176. Epub 2013/11/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morgan JP, 3rd, Haug RH, Murphy MT. Management of facial dog bite injuries. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 1995;53(4):435–41. doi: 10.1016/0278-2391(95)90720-3. Epub 1995/04/01. [DOI] [PubMed] [Google Scholar]
- 6.Galloway RE. Mammalian bites. The Journal of emergency medicine. 1988;6(4):325–31. doi: 10.1016/0736-4679(88)90370-8. Epub 1988/07/01. [DOI] [PubMed] [Google Scholar]
- 7.Eppley BL, Schleich AR. Facial dog bite injuries in children: treatment and outcome assessment. The Journal of craniofacial surgery. 2013;24(2):384–6. doi: 10.1097/SCS.0b013e31827fee33. Epub 2013/03/26. [DOI] [PubMed] [Google Scholar]
- 8.Baack BR, Kucan JO, Demarest G, Smoot EC. Mauling by pit bull terriers: case report. The Journal of trauma. 1989;29(4):517–20. doi: 10.1097/00005373-198904000-00019. Epub 1989/04/01. [DOI] [PubMed] [Google Scholar]
- 9.Tuggle DW, Taylor DV, Stevens RJ. Dog bites in children. Journal of pediatric surgery. 1993;28(7):912–4. doi: 10.1016/0022-3468(93)90695-h. Epub 1993/07/01. [DOI] [PubMed] [Google Scholar]
- 10.Sullivan SK. Banning the Pit Bull: Why Breed-Specific Legislation Is Constitutional. U Dayton L Rev. 1987;13:279. [Google Scholar]
- 11.Monroy A, Behar P, Nagy M, Poje C, Pizzuto M, Brodsky L. Head and neck dog bites in children. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2009;140(3):354–7. doi: 10.1016/j.otohns.2008.11.026. Epub 2009/03/03. [DOI] [PubMed] [Google Scholar]
- 12.Tu AH, Girotto JA, Singh N, Dufresne CR, Robertson BC, Seyfer AE, et al. Facial fractures from dog bite injuries. Plastic and reconstructive surgery. 2002;109(4):1259–65. doi: 10.1097/00006534-200204010-00008. Epub 2002/04/20. [DOI] [PubMed] [Google Scholar]
- 13.Wei LA, Chen HH, Hink EM, Durairaj VD. Pediatric facial fractures from dog bites. Ophthalmic plastic and reconstructive surgery. 2013;29(3):179–82. doi: 10.1097/IOP.0b013e3182880114. Epub 2013/03/21. [DOI] [PubMed] [Google Scholar]
- 14.Sibert JR, Maddocks GB, Brown BM. Childhood accidents--an endemic of epidemic proportion. Archives of disease in childhood. 1981;56(3):225–7. doi: 10.1136/adc.56.3.225. Epub 1981/03/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Feldman KA, Trent R, Jay MT. Epidemiology of hospitalizations resulting from dog bites in California, 1991-1998. American journal of public health. 2004;94(11):1940–1. doi: 10.2105/ajph.94.11.1940. Epub 2004/10/30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Islam S, Ansell M, Mellor TK, Hoffman GR. A prospective study into the demographics and treatment of paediatric facial lacerations. Pediatric surgery international. 2006;22(10):797–802. doi: 10.1007/s00383-006-1768-7. Epub 2006/09/02. [DOI] [PubMed] [Google Scholar]
- 17.Rivara FP, Bergman AB, LoGerfo JP, Weiss NS. Epidemiology of childhood injuries. II. Sex differences in injury rates. American journal of diseases of children [1960] 1982;136(6):502–6. doi: 10.1001/archpedi.1982.03970420026004. Epub 1982/06/01. [DOI] [PubMed] [Google Scholar]
- 18.Liebelt EL. Current concepts in laceration repair. Current opinion in pediatrics. 1997;9(5):459–64. doi: 10.1097/00008480-199710000-00002. Epub 1997/11/14. [DOI] [PubMed] [Google Scholar]
- 19.Surgeons ASoP. American Society of Plastic Surgeons 2012 Plastic Surgery Statistics Report. 2012 [Google Scholar]
- 20.Baker MD, Lanuti M. The management and outcome of lacerations in urban children. Annals of emergency medicine. 1990;19(9):1001–5. doi: 10.1016/s0196-0644(05)82563-6. Epub 1990/09/01. [DOI] [PubMed] [Google Scholar]
- 21.Rui-feng C, Li-song H, Ji-bo Z, Li-qiu W. Emergency treatment on facial laceration of dog bite wounds with immediate primary closure: a prospective randomized trial study. BMC emergency medicine. 2013;13(Suppl 1):S2. doi: 10.1186/1471-227x-13-s1-s2. Epub 2013/08/09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu PS, Beres A, Tashjian DB, Moriarty KP. Primary repair of facial dog bite injuries in children. Pediatric emergency care. 2011;27(9):801–3. doi: 10.1097/PEC.0b013e31822c1112. Epub 2011/09/01. [DOI] [PubMed] [Google Scholar]
- 23.Lackmann GM, Draf W, Isselstein G, Tollner U. Surgical treatment of facial dog bite injuries in children. Journal of cranio-maxillo-facial surgery : official publication of the European Association for Cranio-Maxillo-Facial Surgery. 1992;20(2):81–6. doi: 10.1016/s1010-5182(05)80472-x. Epub 1992/02/01. [DOI] [PubMed] [Google Scholar]
- 24.Guy RJ, Zook EG. Successful treatment of acute head and neck dog bite wounds without antibiotics. Annals of plastic surgery. 1986;17(1):45–8. doi: 10.1097/00000637-198607000-00009. Epub 1986/07/01. [DOI] [PubMed] [Google Scholar]
- 25.Callaham M. Prophylactic antibiotics in common dog bite wounds: a controlled study. Annals of emergency medicine. 1980;9(8):410–4. doi: 10.1016/s0196-0644(80)80153-3. Epub 1980/08/01. [DOI] [PubMed] [Google Scholar]
- 26.Kuvat SV, Bozkurt M, Kapi E, Karakol P, Yaçsar Z, Güven E. Our treatment approaches in head-neck injuries caused by animal bites. Journal of Craniofacial Surgery. 2011;22(4):1507–10. doi: 10.1097/SCS.0b013e31821d4de0. [DOI] [PubMed] [Google Scholar]
- 27.Cummings P. Antibiotics to prevent infection in pateints with dog bite wounds: A meta-analysis of randomized trials. Annals of emergency medicine. 1994;23(3):535–40. doi: 10.1016/s0196-0644(94)70073-7. [DOI] [PubMed] [Google Scholar]
- 28.Dire DJ, Hogan DE, Riggs MW. A Prospective Evaluation of Risk Factors for Infections from Dog-bite Wounds. Academic Emergency Medicine. 1994;1(3):258–66. doi: 10.1111/j.1553-2712.1994.tb02442.x. [DOI] [PubMed] [Google Scholar]
- 29.Mitchell RB, Nanez G, Wagner JD, Kelly J. Dog bites of the scalp, face, and neck in children. The Laryngoscope. 2003;113(3):492–5. doi: 10.1097/00005537-200303000-00018. Epub 2003/03/05. [DOI] [PubMed] [Google Scholar]
- 30.Office SCCs. Three Year Summary of Statistics for Dogs: Registration, Reported Bites, and Pound Data. Excel. 2013 [Google Scholar]
- 31.Brakenbury PH, Muwanga C. A comparative double blind study of amoxycillin/clavulanate vs placebo in the prevention of infection after animal bites. Archives of emergency medicine. 1989;6(4):251–6. doi: 10.1136/emj.6.4.251. Epub 1989/12/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Quinn JV, McDermott D, Rossi J, Stein J, Kramer N. Randomized controlled trial of prophylactic antibiotics for dog bites with refined cost model. The western journal of emergency medicine. 2010;11(5):435–41. Epub 2011/02/05. [PMC free article] [PubMed] [Google Scholar]
- 33.Karlson TA. The incidence of facial injuries from dog bites. JAMA : the journal of the American Medical Association. 1984;251(24):3265–7. Epub 1984/06/22. [PubMed] [Google Scholar]
- 34.Berzon DR, Farber RE, Gordon J, Kelley EB. Animal bites in a large city--a report on Baltimore, Maryland. American journal of public health. 1972;62(3):422–6. doi: 10.2105/ajph.62.3.422. Epub 1972/03/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Beck AM, Jones BA. Unreported dog bites in children. Public health reports [Washington, DC : 1974] 1985;100(3):315–21. Epub 1985/05/01. [PMC free article] [PubMed] [Google Scholar]
- 36.Langley J. The incidence of dog bites in New Zealand. The New Zealand medical journal. 1992;105(927):33–5. Epub 1992/02/12. [PubMed] [Google Scholar]
- 37.Beaureu USA. 1980 Census of population: general population characteristics. 1983 [Google Scholar]
- 38.Beaureu USA. CBSA report chapter 3. 2012 [Google Scholar]
- 39.Beaureu USA. Population by poverty status in 1979:1980, all counties. 1983 [Google Scholar]


