Abstract
Objectives:
To evaluate subjective sleep quality, day-time sleepiness, prevalence of substance use, satisfaction with life among residents at our institute. To evaluate association of sleep qualitywith satisfaction with life and day-time sleepiness. To compare the findings between residents in clinical and para-clinical departments.
Materials and Methods:
Eighty-four residents filled questionnaires to obtain socio-demographic information and use of substance (s). Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and Satisfaction With Life scale (SWLS) were also used. Association between sleep quality and sleepiness and satisfaction with life was evaluated. From the data collected, comparisons were made between the clinical and para-clinical department residents.
Results:
A significant number of residents belonging to the clinical faculty were poorsleepers; reported high levels of abnormal day-time sleepiness and less satisfaction with life compared to residents in para-clinical faculties. The differences in correlation between sleepiness and satisfaction with life with sleep quality among the two groups were not found to be significant. A larger percentage of clinical residents reported use of at least one substance during the residency period compared to the para-clinical residents.
Conclusions:
Poor sleep quality is perceived greatly by the resident doctors in our public hospital, especially among clinical faculties. Interventions are thus necessary in order to ensure adequate sleep among them.
Keywords: Quality, residents, satisfaction, sleep, sleepiness
Sleep–an outcome of the circadian rhythm–is a reversible state of reduced consciousness, characterized by slowing of brain electrical activity, altered muscle tone, and autonomic changes. Disturbed quantity or quality of sleep interferes with the normal mental and bodily functioning. In a highly skilled and stressful occupation like the practice of medicine, sleep-deprivation can have disastrous outcomes for doctors and patients alike.
Sleep has far-reaching physiological and psychological benefits. Over the recent years, there has been a debate on how much sleep is needed for humans to function normally. Most of the research has found that those who sleep at least 7 hours daily at night maintain a satisfactory level of functioning.[1] This is essential for various types of cognitive processes. For example, memory formation and learning involve three major steps–acquisition, consolidation, and recall, the first and last of which occur in wakeful states and consolidation occurs in sleep. In wakefulness, memory codes are thought to be stored in the hippocampus; and in slow-wave sleep, there is a re-iteration of these codes from the hippocampus to the neo-cortex. This cycle repeats with each slow-wave sleep cycle resulting in consolidation of the memory code or trace.[2,3,4]
Neuronal plasticity is the ability of neurons to take up the function of other neurons and establish new synaptic connections when the need arises, for example, if a part of the brain has suffered traumatic or ischemic damage, the unaffected neurons may begin to perform the work initially assigned to the now-damaged areas. This plastic ability of the neurons also has been shown to be affected by sleep disturbances.[5,6]
The effect of sleep restriction/deprivation on cognitive functioning has been amply recorded. For example in a study, truck drivers were subjected to sleep restriction of 3, 5, 7, or 9 hours of total time in bed (TIB) daily for a week, followed by a “sleep recovery” phase of 3 days of 8-hours sleep in laboratory conditions. They were evaluated using Psychomotor Vigilance Tasks (PVT) for speed and reaction times daily. Those who had <9 hours of TIB were found to have lower speed and more reaction time compared to those with 9-hours TIB. Also the improvement with recovery after a week of restriction was more prominent for those with 3- or 5-hours TIB but remained at lower levels indicating a failure to recover on PVT completely at end of study period. Those with 9-hours TIB in the first week did not show any change in their PVT performance after the recovery phase. This highlights the fact that even if sleep compensation is allowed, the functioning of the individuals who are chronically sleep-deprived remains below optimal.[7,8,9,10] This shows why sleep-deprived drivers are more likely to be involved in accidents.[11]
Findings of a study also include that the cumulative neuro-behavioral impairments resulting from restricted sleep for 14 days (4 or 6 hours per night) was almost as high as those seen after 48-72 hours of total sleep deprivation. This indicates that it is not enough to get just a “little sleep” daily, and that our brain requires a daily dose of atleast 7 hours of it's “beauty sleep” to work normally.[8]
Sleep disturbances also affect the emotional state or mood of the subject.[12] Irritability, argumentativeness, hallucinations and in extremes, even disorientation can be the outcomes. Sleep restriction/deprivation is also shown to alter endocrine and metabolic profiles, cause immunological disturbances, increase cardio-vascular morbidities, and even induce gene transcription alterations.[10,13,14,15,16,17,18,19]
The current sleep trends make these and many other worrisome effects a very real public health risk. A poll conducted by telephonic interviews of 1,506 adults in the US in 2004-2005 found a decreasing trend in the number of persons sleeping >/= 7 hours on weekends and weeknights when compared with findings in a similar 1998 survey.[20] Thus, the average American is sleeping much less now than he used to earlier. There are not sufficient studies documenting sleep trends specifically in India, even though current employment profiles may be related with reduced or irregular sleep.[21] In view of major role of sleep in human functioning, we undertook the following cross-sectional study at our institute. We evaluated the subjective sleep quality, day-time sleepiness, satisfaction with life, and use of substances among the residents. This would enable us to identify if there is a potential problem which may need to be scrutinized in detail at the institute in order to provide appropriate remediation.
MATERIALS AND METHODS
This was a cross-sectional study undertaken after obtaining clearance from the Ethics Committee of the Institute. Eighty-four residents who were working/studying at the various clinical and para-clinical faculties at the time of the study period (August 2010 to October 2010) were evaluated after taking their consent as per the declaration of Helsinki. The tools used for assessment were the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS); the Satisfaction With Life Scale (SWLS). Other relevant data was obtained using a semi-structured questionnaire. The PSQI is a validated scale which assesses sleep quality across seven domains (subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, use of sleep medications, and day-time dysfunction), and the composite scores obtained indicate “good” (score <5) and “poor” (score >/= 5) sleepers. SWLS is also a valid and reliable measure of satisfaction with life across all age-groups.
RESULTS
Of the 84 residents who participated, 44 were from the clinical faculties–departments of general medicine, general surgery, obstetrics-gynecology, psychiatry, orthopedics, and pediatrics (i.e. those with direct patient contact during work period), and 40 were from the para-clinical faculties–departments of biochemistry, physiology, pathology, and microbiology (i.e. those with minimal to no direct patient contact during work period).
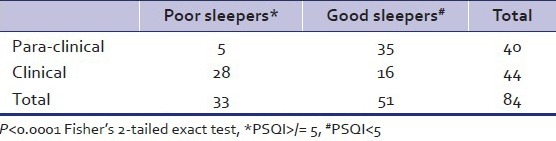
Among the para-clinical group, 12.5% were poor sleepers (PSQI >/= 5) compared to 63.6% of the clinical group. The difference between the clinical and non-clinical groups was also found to be statistically significant (P < 0.0001 by Fisher's exact test-2-tailed, Table 1).
Table 1.
Comparison of pittsburgh sleep quality index scores between clinical and para-clinical groups
Among the clinical faculties, subjective sleep quality and sleep duration were most affected, whereas sleep efficiency was most affected in the para-clinical group.
ESS helps to classify day-time sleepiness into “normal, borderline, and abnormal” (scores of 0–10, 10–12, 12–20, respectively). Abnormal daytime sleepiness was found in the clinical faculties only–20.45% (n = 9) of the sample of 44. The difference between the two groups was found to be significant (P = 0.00012 by Fisher's exact test-2 tailed, Table 2).
Table 2.
Comparison of epworth sleepiness scale scores between clinical and para-clinical groups
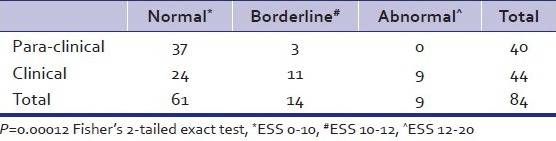
There was a positive correlation between scores of PSQI and ESS in both groups (r = 0.413 and 0.268 in clinical and para-clinical groups, respectively). The difference between the correlations was not significant (P = 0.465 by Fisher's exact test-2 tailed).
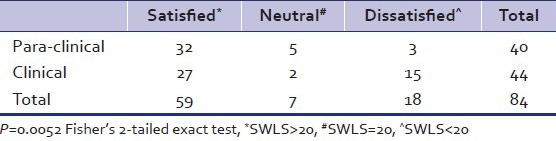
Also, 61.3%of the residents in the clinical faculties were satisfied with their lives on applying SWLS compared to 80% of those from para-clinical faculties. The difference was again found to significant (P = 0.0052 by Fisher's exact test-2 tailed, Table 3). There was a positive correlation (r = 0.265) between PSQI and SWLS scores in the clinical group and a negative correlation (r = −0.057) in the para-clinical group. The difference between the correlation coefficients was not found to be significant (P = 0.14 by Fisher's exact test-2 tailed).
Table 3.
Comparison of satisfaction with life scale scores between clinical and para-clinical groups
We found that 52.2% of clinical group reported having used at least one addictive substance during the residency period, compared with 37.5% of the para-clinical residents. The difference between the two groups was not found to be significant (P = 0.194 by Fisher's exact test-2 tailed). Alcohol, nicotine-containing products, and non-opioid sedatives were the three most commonly used substances in both the groups (43%, 22%, and 16%, respectively). A small percentage reported use of opioids, cannabis, and stimulant medications.
DISCUSSION AND CONCLUSIONS
As per a report by the Ministry of Health and Family Welfare, Government of India, in 2011, the doctor–patient ratio was approximately 1:2000. Going by this data, it is not unnatural to expect that the number of patients that a resident doctor belonging to a clinical faculty of a teaching hospital treats is very high. This shortage of workforce is associated with increased individual workload and consequently, increased stress levels. Working hours for a resident at our institute are not well-defined. It is known that residents belonging to the clinical faculties have responsibilities including out-patient department (OPD), in-patient department (IPD) duties, emergency on-calls, and consultation-liaison duties. These are not divided among the residents and hence each resident is expected to perform all the above duties to variable extents on most of the working days. This results in long working hours ranging from 15 hours to 36 hours at a stretch. Among the para-clinical residents the working hours are more structured with regular departmental/laboratory work of approximately 8 hours with emergency duties on rotational basis.
Our study found that a significant number of residents at our institute were experiencing poor sleep, more day-time sleepiness, were less satisfied with life and were likely to use substances of addictive potential at some time during their residency. The disturbances were higher among those whose work involved direct patient contact and care. Residents face a tough situation–in that they are required to memorize vast amounts of essential matter, ensure a pleasant and empathic approach towards patients and their relatives and make critical therapeutic decisions. But they are often so fatigued that the very same causes get defeated. The effects of sleep restriction and fatigue on non-medical personnel have been discussed above.[7,11] A study conducted on Obstetrics and Gynecology residents at Emory University, demonstrated a definitive cognitive decline towards the end of a night call shift.[22,23] Our study did not evaluate the temporal association between working hours and sleep quality/day-time sleepiness or satisfaction with life. Our findings could be expected to be varied at various times of evaluation–e.g. worse subjective sleep quality reported by residents at the end of 36 hours shifts relative to at the beginning of a working day. This is a drawback of our study.
There have been some studies on sleep conducted among medical students in India too which reflect our findings.[24,25] These disturbances can lead to making mistakes while at work. There has also been an increase in the number doctors who bear the brunt of angry relatives, especially in the emergency services in public hospitals in the past few years. Could this be the result of an increase in workload, poor sleep, and exhaustion leading to impaired decision-making abilities and poor communication skills?
Our study found that the number of residents working in clinical faculties who had used one or more substance of addictive potential was much greater than those in non-clinical faculties. Though we did not evaluate the pattern of substance use in detail, this finding itself is alarming. Drug-seeking/self-medication can be expected to be a result of acute/chronic sleep disturbances, among others. This can potentially further hamper performance leading to a vicious cycle of sleep disturbances, drug use, and poor performance.
In conclusion, our study highlights the need for early identification of sleep disturbances, interventions to introduce flexible working hours and shifts of manageable durations and education regarding the principles, and practice of sleep hygiene among medical residents. Such action will ensure an alert and productive resident who functions at his optimal best in providing patient-care. This is the ultimate goal of the practice of medicine itself.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Banks S, Dinges DF. Behavioral and physiological consequences of sleep restriction. J Clin Sleep Med. 2007;3:519–28. [PMC free article] [PubMed] [Google Scholar]
- 2.Diekelmenn S, Born J. The memory function of sleep. Nat Rev Sci. 2010;11:114–26. doi: 10.1038/nrn2762. [DOI] [PubMed] [Google Scholar]
- 3.Born J, Rasch B, Gais S. Sleep to remember. Neuroscientist. 2006;12:410–24. doi: 10.1177/1073858406292647. [DOI] [PubMed] [Google Scholar]
- 4.Marshall L, Helgadottir H, Molle M, Born J. Boosting slow oscillations during sleep potentiates memory. Nature. 2006;444:610–3. doi: 10.1038/nature05278. [DOI] [PubMed] [Google Scholar]
- 5.Ribeiro S. Sleep and plasticity. Pflugers Arch. 2012;463:111–20. doi: 10.1007/s00424-011-1031-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Frank MG, Issa NP, Stryker MP. Sleep enhances plasticity in the developing visual cortex. Neuron. 2001;30:275–87. doi: 10.1016/s0896-6273(01)00279-3. [DOI] [PubMed] [Google Scholar]
- 7.Belenky G, Wesensten NJ, Thorne DR, Thomas ML, Sing HC, Redmond DP, et al. Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: A sleep dose response study. J Sleep Res. 2003;12:1–12. doi: 10.1046/j.1365-2869.2003.00337.x. [DOI] [PubMed] [Google Scholar]
- 8.Van Dongen HP, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: Dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26:117–26. doi: 10.1093/sleep/26.2.117. [DOI] [PubMed] [Google Scholar]
- 9.Cordova CA, Said BO, McCarley RW, Baxter MG, Chiba AA, Strecker RE. Sleep deprivation in rats produces attentional impairments on a 5-choice serial reaction time task. Sleep. 2006;29:69–76. [PMC free article] [PubMed] [Google Scholar]
- 10.Vgontzas AN, Zoumakis E, Bixler EO, Lin HM, Follett H, Kales A, et al. Adverse effects of modest sleep restriction on sleepiness, performance, and inflammatory cytokines. J Clin Endocrinol Metab. 2004;89:2119–26. doi: 10.1210/jc.2003-031562. [DOI] [PubMed] [Google Scholar]
- 11.Stutts JC, Wilkins JW, Scott Osberg J, Vaughn BV. Driver risk factors for sleep-related crashes. Accid Anal Prev. 2003;35:321–31. doi: 10.1016/s0001-4575(02)00007-6. [DOI] [PubMed] [Google Scholar]
- 12.Dinges DF, Pack F, Williams K, Gillen KA, Powell JW, Ott GE, et al. Cumulative sleepiness, mood disturbance and psychomotor vigilance performance decrements during a week of sleep restricted to 4-5 hours per night. Sleep. 1997;20:267–77. [PubMed] [Google Scholar]
- 13.Spiegel K, Leproult R, Colecchia EF, L’Hermite-Balériaux M, Nie Z, Copinschi G, et al. Adaptation of the 24-h growth hormone profile to a state of sleep debt. Am J Physiol Regul Integr Comp Physiol. 2000;279:R874–83. doi: 10.1152/ajpregu.2000.279.3.R874. [DOI] [PubMed] [Google Scholar]
- 14.Kessler L, Nedeltcheva A, Imperial J, Penev PD. Changes in serum TSH and Free T4 during human sleep restriction. Sleep. 2010;33:1115–8. doi: 10.1093/sleep/33.8.1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spiegel K, Leproult R, Tasali E, Penev P, VanCauter E. Sleep curtailment results in decreased leptin levels and increased hunger and appetite. Sleep. 2003;26:A174. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- 16.Mullington JM, Chan JL, Van Dongen HP, Szuba MP, Samaras J, Price NJ, et al. Sleep loss reduces diurnal rhythm amplitude of leptin in healthy men. J Neuroendocrinol. 2003;15:851–4. doi: 10.1046/j.1365-2826.2003.01069.x. [DOI] [PubMed] [Google Scholar]
- 17.Dinges DF, Douglas SD, Zaugg L, Campbell DE, McMann JM, Whitehouse WG, et al. Leukocytosis and natural killer cell function parallel neurobehavioral fatigue induced by 64 hours of sleep deprivation. J Clin Invest. 1994;93:1930–9. doi: 10.1172/JCI117184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dinges DF, Simpson N. Sleep and Inflammation. Nutr Rev. 2007;65:244–52. doi: 10.1111/j.1753-4887.2007.tb00371.x. [DOI] [PubMed] [Google Scholar]
- 19.Meier-Ewert HK, Ridker PM, Rifai N, Regan MM, Price NJ, Dinges DF, et al. Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J Am Coll Cardiol. 2004;43:678–83. doi: 10.1016/j.jacc.2003.07.050. [DOI] [PubMed] [Google Scholar]
- 20.National Sleep Foundation. Summary of the Sleep in America poll [monograph on the Internet] Washington, DC: National Sleep Foundation; 2005. Sleep in America Poll. Available from: www.sleepfoundation.org/ [Google Scholar]
- 21.Suri JC, Sen MK, Singh P, Kumar R, Aggarwal P. Sleep patterns and their impact on lifestyle, anxiety and depression in BPO workers. Indian J Sleep Med. 2007;2:64–70. [Google Scholar]
- 22.Halbach MM, Spann CO, Egan G. Effect of sleep deprivation on medical resident and student cognitive function: A prospective study. Am J Obstet Gynecol. 2003;188:1198–201. doi: 10.1067/mob.2003.306. [DOI] [PubMed] [Google Scholar]
- 23.Smith-Coggins R, Rosekind MR, Buccino KR, Dinges DF, Moser RP. Rotating shiftwork schedules: Can we enhance physician adaptation to night shifts? Acad Emerg Med. 1997;4:951–61. doi: 10.1111/j.1553-2712.1997.tb03658.x. [DOI] [PubMed] [Google Scholar]
- 24.Mastin DF, Siddalingaiah HS, Singh A, Lal V. Excessive daytime sleepiness, sleep hygiene, and work hours among medical residents in India. J Trop Psychol. 2012;2:e4. [Google Scholar]
- 25.Krishna P, Shwetha S. Sleep quality and correlates of sleep among medical students. Indian J Sleep Med. 2008;3:58–61. [Google Scholar]


