Abstract
Objective:
Occupational lung disease due to silica dust is one of the most common work-related injuries. In denim sandblasting, workers are exposed to silica that may cause immediate mortality, especially in young people. The aim of this study was to assess the multidetector computed tomography (MDCT) findings of silicosis in denim sandblasters and to better define the role of MDCT in the early detection of silicosis.
Materials and Methods:
The study included 12 consecutive male patients who were admitted to a pulmonary outpatient clinic between April 2009 and December 2009. All patients had been working as sandblasters for at least one year. All patients underwent chest CT examinations for suspected silicosis. Two radiologists independently assessed the images for the presence and distribution of airspace consolidation, ground-glass opacity, nodules, interlobular septal thickening, parenchymal bands, fibrosis, masses, traction bronchiectasis, honeycombing, lobular low-attenuation areas, emphysema, pleural effusion or thickening, and mediastinal or hilar adenopathy.
Results:
MDCT detected parenchymal abnormalities in the lungs in eight (67%) of the twelve patients. The most common MDCT finding was ground glass opacity (58%). Other common findings were parencyhmal nodules and interlobular septal thickening, predominantly in the upper zones. Nodules were detected in six (50%) of the twelve patients. In four cases (67%), the nodules were numerous (>10), were predominantly smaller than 10 mm, and were centrilobular in distribution. In five (42%) of the 12 patients, interlobular septal thickening was detected. Only one (8%) patient presented with airspace consolidation; this was bilateral in the upper zones and associated with air bronchograms. In one (8%) patient there were several traction bronchiectases in the upper zones. None of the patients presented with pleural effusion, thickening, or honeycombing. Enlarged mediastinal nodes were identified in half of the patients, predominantly in the precarinal, paratracheal, and prevascular regions. No egg-shell calcification was detected. One (8%) patient presented with punctate calcification in the hilar region.
Conclusions:
Early detection of silicosis is important because it may cause immediate mortality, especially in young people. Enlarged mediastinal lymph nodes, centrilobular nodules, interlobular septal thickening, and patchy ground glass opacity may be early MDCT findings of silicosis. Thus, MDCT plays an important role in the early detection of silicosis in denim sandblasters.
Keywords: Denim sandblaster, Multidedector computed tomography, Silicosis
Özet
Amaç:
Silika tozuna bağlı gelişen mesleksel akciğer hastalığı yaygın iş yaralanmaları arasında yer alır. Kot kumlama işinde çalışanlar silika tozuna maruz kalırlar ve bu da özellikle genç insanlarda ölüme neden olabilir. Biz bu çalışmada kot kumlama işine bağlı gelişen silikozisin multidedektör bilgisayarlı tomografi (MDBT) bulgularını ve erken dönemde BT’nin rolünü göstermeyi amaçladık.
Gereç ve Yöntem:
Çalışmamıza Nisan ve Aralık 2009 tarihleri arasında göğüs hastalıkları polikliniğine başvuran 12 ardışık erkek genç erişkin hasta dahil edildi. Tüm hastalar en az 1 senedir kot kumlama işinde çalışıyordu. Tüm hastalara akciğer BT’si çekilerek iki radyolog tarafından birbirinden bağımsız olarak değerlendirildi. Radyologlar tarafından konsolidasyon, buzlu cam görünümü, nodül, interlobüler septal kalınlaşma, parankimal band, fibrozis ya da kitle, traksiyon bronşiektazisi, balpeteği akciğer, amfizem, plevral efüzyon ya da kalınlaşma, mediastinal ya da hiler lenfadenopati varlığı ve yaygınlığı değerlendirildi.
Bulgular:
MDBT 12 hastanın 8‘inde (%67) akciğerlerde parankimal anormallik tespit etti. En çok görülen MDBT bulgusu buzlu cam görünümüydü (%59). Diğer çok görülen bulgular özellikle üst zonlarda olmak üzere nodüller ve interlobuler septal kalınlaşmaydı. Hastaların %50’sinde parankimal nodül tespit edildi. Nodülü olan hastaların 4‘ünde (%67) nodüller 10’dan fazla, 10 mm‘den küçük ve ağırlıklı olarak sentrilobuler yerleşimliydi. Oniki hastanın 5’inde (%42) interlobuler septal kalınlaşma tespit edildi. Sadece 1 (%8) olguda üst lobları tutan ve hava bronkogramları içeren konsolidasyon vardı. Hiçbir olguda plevral efüzyon, kalınlaşma ya da balpeteği akciğer görünümü saptanmadı. Hastaların yarısında özellikle prekarinal, paratrakeal ve prevasküler alanları tutan lenf nodu büyümesi vardı. Hiçbir lenf nodunda yumurta kabuğu kalsifikasyon yoktu. Sadece 1 (%8) hastada sol hiler bölgede punktat kalsifikasyon içeren lenf nodu tespit edildi.
Sonuç:
Silikozisin erken tesbiti özellikle genç popülasyonda ölüme neden olması açısından önemlidir. Genişlemiş mediastinal lenf nodları, sentrilobuler nodüller, interlobuler septal kalınlaşmalar ve buzlu cam görünümü silikozisin erken dönem MDBT bulguları olabilir ve kot kumlayıcılarında bu bulguların erken tespitinde MDBT önemli bir rol oynar.
Introduction
Occupational lung disease due to silica dust is one of the most common work-related injuries. Exposure to silica dust can affect shipyard workers, sandblasters, and coal miners [1]. Silicosis is caused by the inhalation of crystalline silica dust, which results in a fibrotic tissue reaction to its presence in the lungs [2].
In denim sandblasting, workers are exposed to silica because they project silica or silica-containing sand as an abrasive onto denim surfaces to produce a “worn-in” appearance. This kind of exposure is very dangerous because of intense exposure during long hours of work under very poor hygienic conditions without any serious respiratory protection [3–6].
Due to its non-specific clinical symptoms and unrecognizable shadows on roentgenograms in the early phase of the disease, silicosis may fail to be recognized and tends to be underestimated [7, 8]. Multidetector computed tomography (MDCT) has been shown to be helpful for detecting diffuse pulmonary parenchymal abnormalities at early stages [3]. Therefore, the aim of this study was to better define the role of MDCT for the early detection of silicosis by assessing MDCT findings in patients with silicosis from denim sandblasting.
Materials and Methods
Our institutional review board approved this retrospective study and written informed consent was obtained from the parents or relatives of all the affected subjects.
The study included 12 consecutive male patients in whom the diagnosis of silicosis was confirmed based on their occupational history and radiological alterations compatible with the disease. The study group was chosen from the patients who were admitted to a pulmonary out-patient clinic between April 2009 and December 2009. All patients had been working as sandblasters. Those patients with a smoking history of 10 pack-years or a history of previous tuberculosis were excluded from the study. The diagnosis was made based mainly on the clinical history, occupational exposure to silica dust, and MDCT findings.
CT was performed with a 16-detector-row CT system (Light Speed 16, GE Medical Systems, Milwaukee, Wis, USA). The patients were examined during breath holding after deep inspiration in a supine position with 3-mm collimation at 10-mm intervals, using settings of 120kV, 300mA, and a 0.5 s acquisition time. Lungs were scanned from apex to base without contrast material, and all images were obtained with both lung and mediastinal window settings. The scans were examined at a window of 1,000–1,500 Hounsfield units (HU) and a level of −700 to −800 HU for pulmonary parenchyma, and a window of 500–800 HU and a level of 20–60 HU for mediastina.
Two radiologists independently assessed the examinations. In cases of discrepancy between the readers, the CT scans were reviewed once more by both observers together and a final decision was made by consensus.
The reviewers evaluated the images for the presence and distribution of airspace consolidation, ground-glass opacity, nodules, interlobular septal thickening, parenchymal bands, fibrosis, masses, traction bronchiectasis, honeycombing, lobular low-attenuation areas, emphysema, pleural effusion or thickening, and mediastinal or hilar adenopathy.
Results
The age of the patient group ranged from 19.2–25.4 yr (21.2±1.2 (mean±SD) yr). The exposure time ranged from 1.0–5.2 yr [3.7±1.4 (mean±SD) yr]. The latency period was the same as the exposure time because the patients were still working in sandblasting work. All patients had been working six days per week and 12 hours per day and they had been using a facial mask for protection.
MDCT depicted parenchymal abnormalities in eight (%67) of the twelve patients. The most common findings were nodules, ground glass opacity, and interlobular septal thickening predominantly in the upper zones. Nodules were depicted in six (50%) of the twelve patients. In four cases (67%), the nodules were numerous (>10), were predominantly smaller than 10 mm, and were centrilobular in distribution (Figures 1a, b). In five (42%) patients, interlobular septal thickening was detected. Seven (58%) patients presented with ground glass opacity (Figure 2). One (8%) of the patients presented with airspace consolidation; this was bilateral in the upper zones and associated with air bronchograms. In one (8%) patient there were several traction bronchiectases in the upper zones (Figure 3). None of the patients presented with pleural effusion, thickening, or honeycombing.
Figure 1.
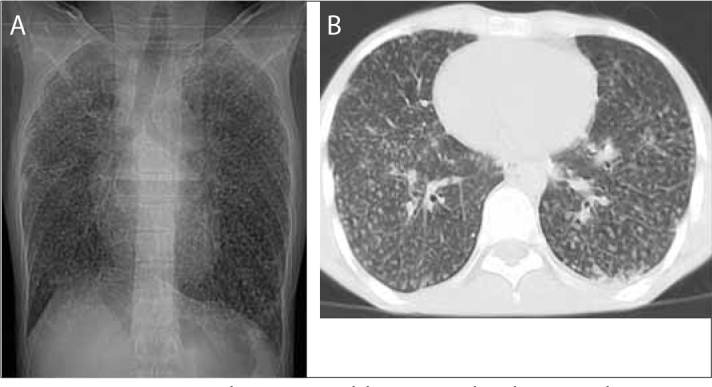
A twenty-three-year-old man with silicosis. Chest x-ray demonstrates innumerable centrilobular nodules and linear opacities (a). Thorax MDCT scan demonstrates innumerable ill-defined centrilobular nodules and linear opacities (b)
Figure 2.
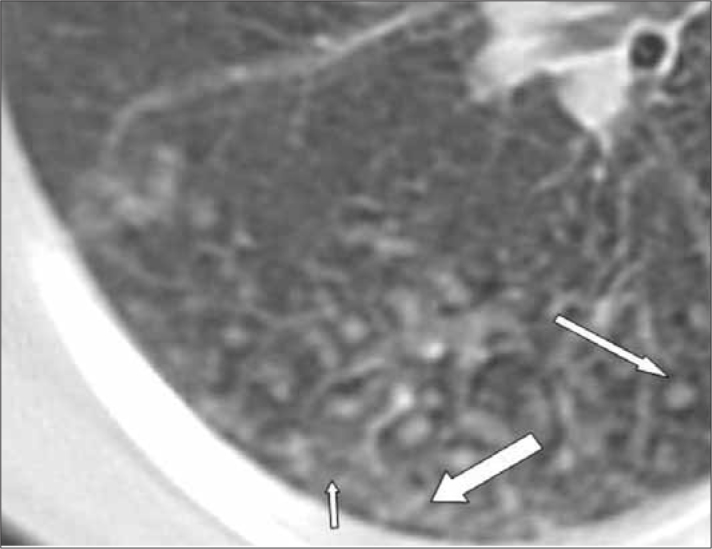
A twenty-one-year-old man with silicosis. MDCT scan demonstrates ground glass opacity (short arrow), centrilobular nodules (long arrow) and interlobular septal thickening (thick arrow) in the superior segment of the lower lobe of the right lung
Figure 3.

A twenty-year-old man with silicosis. MDCT scan shows several traction bronchiectases (short arrow) with some subpleural nodules (long arrow) in the upper lobe of the right lung
Enlarged mediastinal nodes, defined as lymph nodes larger than 1 cm in short-axis diameter, were identified in half of the patients, predominantly in the precarinal, paratracheal, and prevascular regions (Figure 4a). No eggshell calcification was detected. One (8%) of the patients presented with punctate calcifications in the left hilar region (Figure 4b).
Figure 4.
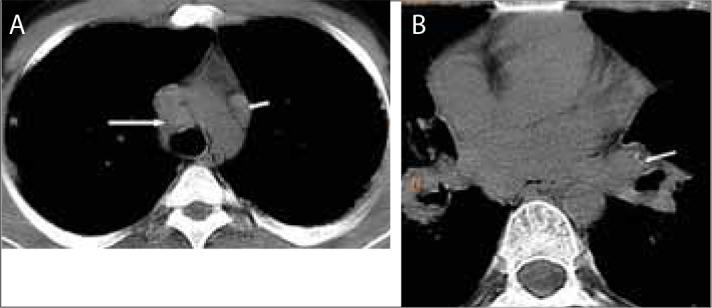
A twenty-three-year-old man with silicosis. MDCT scan shows lymph nodes larger than 1 cm in short-axis diameter in the paratracheal (long arrow) and prevascular regions (short arrow) (a). MDCT scan shows a lymph node with punctate calcifications in the left hilar region (arrow) (b)
Discussion
Silicosis is the most common and oldest recognized occupational lung disease [9]; however, silicosis associated with denim sandblasting is not common. It may develop quickly and can cause immediate mortality, especially in young people [3, 4]. It is a preventable but untreatable environmental pulmonary disease. Therefore, imaging findings capable of detecting silicosis in the early stages are urgently needed.
Roentgenograms are not perfect because they cannot reveal early parenchymal changes and do not fully demonstrate their extent. Hence, a normal conventional roentgenogram in people exposed to dust does not exclude the presence of silicosis. CT can detect small and multifocal opacities more accurately and earlier than roentgenograms [10].
Silicosis is usually classified as acute, subacute/accelerated, or chronic simple silicosis [11]. Acute silicosis typically occurs after a very large acute exposure to silica dust, primarily among sandblasters [12]. Acute silicosis is usually fatal [13]. Chong et al [14] reported that CT findings of acute silicosis include multiple ill-defined centrilobular nodules, patchy ground glass opacity, and lung consolidation. The study of Alper et al. [3] showed that the most common CT finding was centrilobular nodules (94%). However, in our study the most common CT finding was patchy ground glass opacity (58%). Furthermore, the frequency of nodules (50%) and patchy ground glass opacity (58%) in our study was lower than in the study of Alper et al. This discrepancy can be explained by the shorter exposure time in our patients. In our case, lung consolidation was detected only in one patient. Arakawa et al. [15] reported that parenchymal fibrosis with honeycombing was detected by CT in nearly all patients that had chronic silica exposure. In our study, CT failed to detect honeycombing of the lung in any of the patients, probably due to the fact that our patients were in the early stage of silicosis.
Enlarged or calcified hilar and mediastinal lymph nodes are usually seen in silica-exposed workers [16]. Antao et al. [16] reported that 74% of the silicotic patients had enlarged mediastinal lymph nodes and 66% of them had evidence of lymph node calcification. In our study, enlarged mediastinal nodes were identified in half of all the patients. The development of egg-shell type lymph node calcification is the characteristic manifestation of chronic silicosis [17,18]. The chronic form of silicosis typically manifests after 10–20 years of exposure to low concentrations of silica dust [19]. Egg shell calcification in early stage of silicosis has been reported in a few patients in the literature [20–22]. Lymph node calcification was seen in only one patient in our study, and it was punctate and in the left hilar region. In our study, we did not detect egg shell calcification at a high frequency because our patients were in the early stage of silicosis.
In conclusion, early detection of silicosis is important because it may cause immediate mortality, especially in young people. Enlarged mediastinal lymph nodes, centrilobular nodules, interlobular septal thickening, and patchy ground glass opacity may be early MDCT findings of silicosis. Therefore, MDCT has an important role in the early detection of silicosis in denim sandblasters
Footnotes
Conflict interest statement: The authors declare that they have no conflict of interest to the publication of this article.
References
- 1.Bang KM, Attfield MD, Wood JM, et al. National trends in silicosis mortality in the United States. 1981 to 2004. Am J Ind Med. 2008;51:633–9. doi: 10.1002/ajim.20607. [DOI] [PubMed] [Google Scholar]
- 2.Suganuma N, Kusaka Y, Hering KG, et al. Reliability of the proposed international classification of high-resolution computed tomography for occupational and environmental respiratory diseases. J Occup Health. 2009;51:210–22. doi: 10.1539/joh.l8030. [DOI] [PubMed] [Google Scholar]
- 3.Alper F, Akgun M, Onbas O, et al. CT findings in silicosis due to denim sandblasting. Eur Radiol. 2008;18:2739–44. doi: 10.1007/s00330-008-1061-3. [DOI] [PubMed] [Google Scholar]
- 4.Akgun M, Gorguner M, Meral M, et al. Silicosis caused by sandblasting of jeans in Turkey: a report of two concomitant cases. J Occup Health. 2005;47:346–9. doi: 10.1539/joh.47.346. [DOI] [PubMed] [Google Scholar]
- 5.Akgun M, Mirici A, Ucar EY, et al. Silicosis in Turkish denim sandblasters. Occup Med. 2006;56:554–8. doi: 10.1093/occmed/kql094. [DOI] [PubMed] [Google Scholar]
- 6.Akgun M, Araz O, Akkurt I, et al. An epidemic of silicosis among former denim sandblasters. Eur Respir J. 2008;32:1295–303. doi: 10.1183/09031936.00093507. [DOI] [PubMed] [Google Scholar]
- 7.Rosenman KD, Reilly MJ, Kalinowski DJ, et al. Silicosis in the 1990s. Chest. 1997;111:779–86. doi: 10.1378/chest.111.3.779. [DOI] [PubMed] [Google Scholar]
- 8.Sampson HL. The roentgenogram in so-called “acute” silicosis. Am J Public Health Nations Health. 1933;23:1237–9. doi: 10.2105/ajph.23.12.1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pendergrass EP. Silicosis and a few of the other pneumoconioses: observations of certain aspects of the problem, with emphasis on the role of the radiologist. AJR. 1958;80:1–41. [PubMed] [Google Scholar]
- 10.Sun J, Weng D, Jin C, et al. The value of high resolution computed tomography in the diagnostics of small opacities and complications of silicosis in mine machinery manufacturing workers, compared to radiography. J Occup Health. 2008;50:400–5. doi: 10.1539/joh.l8015. [DOI] [PubMed] [Google Scholar]
- 11.Danila E, Sileikiene V, Nargela R, Zurauskas E, Loskutoviene G. Different course of silicosis in four brothers of one family. Int J Occup Med Environ Health. 2009;22:51–7. doi: 10.2478/v10001-009-0004-9. [DOI] [PubMed] [Google Scholar]
- 12.Akira M. High-resolution CT in the evaluation of occupational and environmental disease. Radiol Clin North Am. 2002;40:43–59. doi: 10.1016/s0033-8389(03)00108-8. [DOI] [PubMed] [Google Scholar]
- 13.Chan CN, Chan SY. Silicosis-a preventable occupational disease. J Hong Kong Med Assoc. 1994;46:31–6. [Google Scholar]
- 14.Chong S, Lee KS, Chung MJ, Han J, Kwon OJ, Kim TS. Pneumoconiosis: comparison of imaging and pathologic findings. Radiographics. 2006;26:59–77. doi: 10.1148/rg.261055070. [DOI] [PubMed] [Google Scholar]
- 15.Arakawa H, Fujimoto K, Honma K, et al. Progression from near-normal to end-stage lungs in chronic interstitial pneumonia related to silica exposure: long-term CT observations. AJR. 2008;191:1040–5. doi: 10.2214/AJR.07.3871. [DOI] [PubMed] [Google Scholar]
- 16.Antao VC, Pinheiro GA, Terra-Filho M, et al. High-resolution CT in silicosis: correlation with radiographic findings and functional impairment. J Comput Assist Tomogr. 2005;29:350–6. doi: 10.1097/01.rct.0000160424.56261.bc. [DOI] [PubMed] [Google Scholar]
- 17.Marchiori E, Ferrira A, Saez F, et al. Conglomerated masses of silicosis in sandblasters: High-resolution CT findings. EJR. 2006;59:56–9. doi: 10.1016/j.ejrad.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 18.Stark P, Jacobson F, Schaffer K, et al. Standard imaging in silicosis and coal worker’s pneumoconiosis. Radiol Clin North Am. 1992;30:1147–54. [PubMed] [Google Scholar]
- 19.Marchiori E, Souza CA, Barbassa TG, Escuissato DL, Gasparetto EL, Souza AS., Jr Silicoproteinosis: high-resolution CT findings in 13 patients. AJR Am J Roentgenol. 2007;189:1402–6. doi: 10.2214/AJR.07.2402. [DOI] [PubMed] [Google Scholar]
- 20.Buechner HA, Ansari A. Acute silico-proteinosis: a new pathologic variant of acute silicosis in sandblasters, characterized by histologic features resembling alveolar proteinosis. Dis Chest. 1969;55:274–8. doi: 10.1378/chest.55.4.274. [DOI] [PubMed] [Google Scholar]
- 21.Dee P, Suratt P, Winn W. The radiographic findings in acute silicosis. Radiology. 1978;126:359–63. doi: 10.1148/126.2.359. [DOI] [PubMed] [Google Scholar]
- 22.Xipell JM, Ham KN, Price CG, et al. Acute silicoproteinosis. Thorax. 1977;32:104–11. doi: 10.1136/thx.32.1.104. [DOI] [PMC free article] [PubMed] [Google Scholar]


