Abstract
Objective:
Because renal venous variations possess potential hazards during abdominal aortic surgery or laparoscopic donor nephrectomy, the detailed preoperative evaluation of the renal vessels with angiography should be performed to avoid vascular injuries. We present multidetector row computed tomography (MDCT) findings of the retroaortic left renal vein (RLRV) with other vascular variations.
Materials and Methods:
Twenty-two patients with RLRV were evaluated with MDCT using multiplanar images, MIP images, and 3D volume rendering.
Results:
The RLRVs with accessory renal vessels and other variant veins draining into the left renal vein were effectively evaluated in all patients.
Conclusions:
MDCT angiography is an effective technique for evaluating abdominal vessels, and it presents adequate images of renal vessels and vascular variations, which pose importance before abdominal surgery.
Keywords: Multidetector row CT, Retroaortic left renal vein, Vascular anomalies
Özet
Amaç:
Böbrek veni varyasyonları, abdominal aortik cerrahi veya laparoskopik donör nefrektomisi esnasında potansiyel tehlike taşıdığından dolayı, damar yaralanmalarını önlemek için böbrek damarlarının operasyon öncesi anjiografi ile değerlendirilmesi gerekir. Biz bu çalışmada diğer damarsal varyasyonlarla birlikte retroaortik sol renal venin (RSRV) çok kesitli bilgisayarlı tomografi (ÇKBT) bulgularını sunduk.
Gereç ve Yöntem:
RSRV’ li 22 hasta, multiplnar görüntüler, MIP görüntüler ve 3D volume rendering görüntüler kullanılarak ÇKBT ile değerlendirildi.
Bulgular:
RSRV, aksesuar böbrek damarları ve sol renal vene açılan venlerdeki değişiklikler ile birlikte başarılı birşekilde görüntülendi.
Sonuç:
ÇKBT anjiyografisi abdominal damarların değerlendirilmesinde etkili bir tekniktir ve özellikle abdominal cerrahi öncesi böbrek damarları ve damar varyasyonları hakkında yeterli görüntüler verir.
Introduction
Renal vessels may show many variations with respect to their origins and drainage patterns; these variations become important in surgical and endourologic procedures and vascular interventions. Although the most commonly encountered renal vascular variations are the numbers of the renal arteries [1], more uncommon variations are the renal vein variations with their numbers, course, origins, and drainage sites. Recently, these variations can be easily detected in modern imaging techniques. We present multidetector row computed tomography (MDCT) findings of the retroaortic left renal vein (RLRV) with other associated vascular variations.
Materials and Methods
Twenty-four patients with RLRV were evaluated with 16 row MDCT. The mean age was 49 years (range, 30–74 years). The RLRVs were detected on the CT scan in eleven patients with pelvic venous congestion, in seven patients with internal malignities, and in six cases prior to renal transplantation. In five cases, the RLRV and left ovarian vein dilatation were detected on abdominal ultrasound (US), and then they were evaluated with a CT scan for accompanying vessel anomalies. On imaging, non-ionic contrast material was administered via an upper extremity vein by a power injector at 2.0 mL/sec through a 20-gauge catheter. CT scanning was obtained at 25 and 50 sec after the start of the contrast material injection with collimation of 1.5 mm, slice thickness of 1.0 mm, table speed of 7.5 mm per rotation with rotation time of 0.5 seconds, 120 kVp, and 250 mA. After scanning, axial, coronal, sagittal, maximum intensity projection (MIP), and 3D images were evaluated for the numbers and insertion-origin levels of renal arteries and veins with gonadal and adrenal veins.
Results
The RLRV was clearly detected in all patients using multiplanar images and 3D volume rendering images (Figure 1a, b). Although the RLRV drained into the inferior vena cava (IVC) at a normal level in fifteen patients, it joined at a lower level to the IVC in seven cases (Fig. 2a, b and c). In eight patients, there were dilatations of the left gonadal vein and adrenal vein due to renal vein compression by the aorta (Fig. 3a, b). One case showed an accessory vein on the right side (Fig. 4a, b and c). The accessory vein originated from the inferior pole of the right kidney and it drained into the inferior vena cava on the anterior side at lower level. One case had a supplementary artery on the right side and another showed an inferior supplementary artery on the left side with RLRV (Fig. 5). Two cases were presented as the circumaortic left renal vein.
Figure 1.

Sagittal reformatted image (a) and 3D volume rendering image (b) show the RLRV draining into the IVC at a normal level
Arrows: RLRV, IVC: inferior vena cava, AO: aorta, SMV: superior mesenteric vein
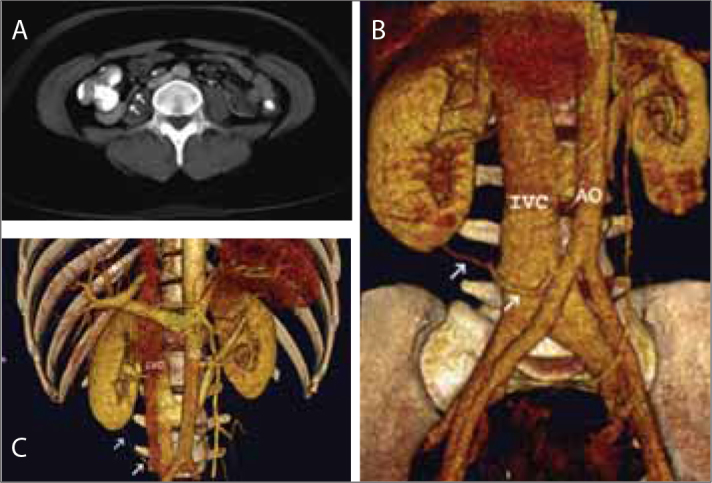
Figure 2.

Axial image (a), coronal reformatting image (b), and 3D image (c) reveal that the RLRV draining into the IVC at a lower level in a 74-year-old female. The RLRV is opening into the IVC at just prior the IVC bifurcation
Arrows: RLRV, IVC: inferior vena cava, AO: aorta
Figure 3.

A 60-year-old female with primary gastric cancer and liver metastasis. On 3D volume rendering images on anterior oblique (a) and posterior oblique views (b), there is the RLRV with dilations of the gonadal and adrenal veins. There are also the left paravertebral vein draining into the left adrenal vein and calcified atheroma plaques on the aorta
L: live, AO: aorta, white arrows: gonadal vein, open arrow: adrenal vein, arrowhead: paravertebral vein
Figure 4.
A 38-year-old female. 3D MIP contrast-enhanced computed tomography scan (a) shows an accessory vein on the right (arrows). 3D volume rendering images with oblique view (b) and anterior view (c) reveals that the accessory vein originated from the inferior pole of the right kidney and drained into the IVC on the anterior side and that the retroaortic left renal vein with an oblique course drained into the IVC at a normal level. Both kidneys with ordinal renal arteries and veins are situating at a normal level and the hilus of them are opening medially
White arrows: accessory vein, IVC: inferior vena cava, AO: aorta
Figure 5.

A 51-year-old female has primary colon cancer with liver metastasis and ascites. On the left oblique 3D image, there is a supplementary renal artery extending from the aortic bifurcation to the inferior pole of the left kidney
AO: aorta, white arrows: supplementary artery
Conclusions
Overall, 92% of people have one renal vein on each side. The left renal vein is approximately 7.5 cm long, and the right renal vein is approximately 2.5 cm long [2]. Variations in the course, number, and arrangement of the renal veins are less common from the renal arterial variations. Renal venous variations and multiple veins are seen more often on the right side than on the left side [2–4].
With an incidence of 1.2%–3.3% [2, 3], the retroaortic left renal vein is a more frequently encountered variation in abdominal surgery or routine cadaveric dissections and in radiological investigations. It consists of the left renal vein crossing posterior to the aorta and has potential hazards to the surgeon during abdominal aortic surgery [4]. It is accepted that a retroaortic left renal vein forms if the dorsal part of the sub-supracardinal anastomosis and the intersupracardinal anastomosis persist, whereas the ventral part of the subsupracardinal anastomosis and the intersubcardinal anastomosis regress. Although a retroaortic left renal vein usually drains into the IVC at a normal level or at a lower level (Fig. 4), it may join with the left common iliac vein and may present with a history of hematuria, dysuria, or recurrent flank pain [5].
The presence of accessory arteries is 32.25% and that of accessory veins is 14.4% [2, 3]. When any accessory vein emerges separately from the kidney and has a separate opening into the inferior vena cava, it is termed an additional renal vein, supernumerary vein, or accessory vein [3]. Accessory veins are seen more frequently on the right side (4.2-26-27.8%) than on the left side (0-1-2.6%). One case in the presented study also showed an accessory renal vein on the right side. While the accessory veins may emerge from kidneys with different origins, they may also show various drainage patterns. They may present one fused opening or separate insertions in the IVC or in another vein. An accessory vein can act as an alternate channel, and its presence or absence can influence the technical feasibility of surgical procedures, such as renal transplantation and endourologic procedures. A large accessory vein could also result in significant bleeding during and after surgery or ureterorenoscopy [3].
We detected two supplementary renal arteries in two cases. The supplementary renal arteries most commonly arise from the abdominal aorta and supply the inferior pole. However, they can also originate from the celiac, superior mesenteric, inferior mesenteric, or iliac arteries. The accessory arteries, which traverse the renal hilum before entering the renal parenchyma, are called polar arteries. They directly enter the renal parenchyma and virtually always supply the superior renal pole [6].
Because renal vascular variations may be responsible for the failure of vascular restoration such as in the resection of a renal tumor or in renal transplantation, or in abdominal aortic surgery, prior knowledge of possible variations of the renal arteries and veins is important to avoid an eventful postoperative course due to inadvertent injury and unwelcome bleeding [4]. Especially, laparoscopic donor nephrectomy with limited operative visibility requires detailed preoperative evaluation of the renal arteries, veins, and collecting system. Therefore, an angiographic evaluation prior to renal surgery should be performed to assess possible renal vascular variations or lesions. The left adrenal and gonadal veins must be evaluated preoperatively because preoperative imaging of these veins may facilitate the dissection of these veins and avoid vascular injury.
Spiral computed tomographic (CT) angiography, a less invasive technique than standard angiography is a generally accepted method in the evaluation of the renal vessels. CT angiography is a technique that is safe, fast, minimally invasive, and relatively inexpensive, and it presents excellent agreement with both catheter angiography and surgery in predicting the variations of the renal vessels. It can also provide preoperative information about other renal vascular diseases, such as aneurysm, arteriovenous malformation, or stenosis [2]. Kim et al. reported that the respective sensitivity and specificity of CT angiography were 86% and 100% for supernumerary arteries, 100% and 100% for early-branching arteries, and 75% and 100% for supernumerary veins [7]. With short data acquisition time, narrow collimation, good spatial resolution, and detailed data sets, MDCT presents excellent anatomic information, increased contrast enhancement of the arteries and veins, thinner section imaging, and improved longitudinal spatial resolution [2]. Therefore, it provides reduced motion and partial volume artifacts during a single breath hold [7].
CT images of renal arteries and veins are usually obtained at 25 and 55 sec from the start of IV contrast injection, respectively [8]. If a short scanning delay is used, supernumerary veins and early venous bifurcations are missed due to poor opacification of the venous system. A delayed topogram may be obtained 5 minutes after intravenous contrast material administration for evaluation of the renal collecting system and ureters [2].
In conclusion, preoperative evaluation of the renal vasculature due to its complex nature and composition is essential in correct surgical planning and in avoiding serious vascular injury. Especially MDCT with multiplanar and 3D reformatted images can help assess well the renal vasculature and variations with renal anatomy, urinary tract, and renal parenchyma [2, 6, 7].
Footnotes
Conflict of interest statement The authors declare that they have no conflict of interest to the publication of this article.
References
- 1.Bordei P, Sapte E, Iliescu D. Double renal arteries originating from the aorta. Surg Radiol Anat. 2004;26:474–9. doi: 10.1007/s00276-004-0272-9. [DOI] [PubMed] [Google Scholar]
- 2.Kawamoto S, Montgomery RA, Lawler LP, et al. Multi-detector row CT evaluation of living renal donors prior to laparoscopic nephrectomy. Radiographics. 2004;24:453–66. doi: 10.1148/rg.242035104. [DOI] [PubMed] [Google Scholar]
- 3.Dhar P. An additional renal vein. Clinical Anatomy. 2002;15:64–6. doi: 10.1002/ca.1095. [DOI] [PubMed] [Google Scholar]
- 4.Kudo FA, Nishibe T, Miyazaki K, et al. Left Renal Vein Anomaly Associated with Abdominal Aortic Aneurysm Surgery: Report of a Case. Surg Today. 2003;33:609–11. doi: 10.1007/s00595-003-2536-0. [DOI] [PubMed] [Google Scholar]
- 5.Brancatelli G, Galia M, Finazzo M, et al. Case report: Retroaortic left renal vein joining the left common iliac vein. Eur Radiol. 2000;10:1724–5. doi: 10.1007/s003300000383. [DOI] [PubMed] [Google Scholar]
- 6.Tran T, Heneghan JP, Paulson EK. Preoperative evaluation of potential renal donors using multidetector CT. Abdom Imaging. 2002;27:620–5. doi: 10.1007/s00261-001-0139-z. [DOI] [PubMed] [Google Scholar]
- 7.Kim JK, Park SY, Kim HJ, et al. Living donor kidneys: Usefulness of multi-detector row CT for comprehensive evaluation. Radiology. 2003;229:869–76. doi: 10.1148/radiol.2293021098. [DOI] [PubMed] [Google Scholar]
- 8.Kawamoto S, Lawler LP, Fishman EK. Evaluation of the renal venous system on late arterial and venous phase images with MDCT angiography in potential living laparoscopic renal donors. Am J Roentgenol. 2005;184:539–45. doi: 10.2214/ajr.184.2.01840539. [DOI] [PubMed] [Google Scholar]


