Abstract
Objective:
Blunt and penetrating hepatic injuries are conditions that are frequently encountered in emergency surgeries, and they involve high mortality morbidity. In the handling of such injuries, methods ranging from the application of simple cauterization and suturing for hemostasis to hepatic lobectomies, which might involve the removal of the greater part of the organ, have been defined. Due to the organ’s fragility and susceptibility to bleeding, elective hepatic resections necessitate both surgical experience and technological equipment. Therefore, the demand still exists for an affordable and easy-to-use-method that could be applied by all centers.
Materials and Methods:
To meet this demand, we have developed a method of hemorrhage control via sutures supported by absorbable plaques that provide effective compression and prevent the suture from cutting the tissue during the application of the sutures in the treatment of such fragile organs as the liver.
In our method, we have achieved hemostasis by bilaterally compressing the tissue through strong ties after placing, on the part of the tissue on which the sutures are applied, absorbable and flexible plaques that prevent the suture from cutting the tissue during the application of a polyglactin suture to the solid organ. To prevent dislocation of the plaques, we have fastened the sutures by reeving them through the holes made in the plaques.
Results:
We have demonstrated the success and the practicality of our method by applying it on four pigs; we experimentally inflicted hepatic injuries on two pigs, and we performed resection on the other two pigs. The hepatic hemorrhages we developed in both of the animals were successfully restrained by the use of our method. On the other hand, two resections were performed on the right and left lobes of the other two animals. There were no hemorrhages during the surgery, and the procedure took 45 minutes in total. No postoperative complications occurred. While the liver function test values were high on the seventh day, due to the operation, they were observed to be normal on the thirtieth day. After the laparotomies, performed six months later, we observed that the plaques as well as the sutures were absorbed and that the injured tissues were completely healed. Additionally, it was observed during the pathological examination that the tissues beneath the area of application were healed through fibrosis and that the liver had no other pathologies.
Conclusions:
In conclusion, we believe that the method can be safely used in hepatic resections or traumatic hemorrhages in the proper locations.
Keywords: Hepatic resection, Hepatic trauma, Plaque and suture
Özet
Amaç:
Künt ve penetran hepatik yaralanmalar acil cerrahide sık karşılaşılan durumlardır ve yüksek mortalite, morbidite riski taşırlar. Bu tip yaralanmaların tedavisinde tanımlanan metodlar hemostaz için yapılan basit sütürasyon ve koterizasyondan organın büyük bir kısmının çıkarılmasını gerektiren lobektomilere kadar değişebilir. Karaciğerin fragil ve kanamaya meyilli yapısı nedeniyle elektif rezeksiyonlar cerrahi tecrübe ve teknolojik ekipman gerektirir. Bu nedenle her merkezde ve kolayca uygulanabilecek bir metod arayışı halen sürmektedir.
Gereç ve Yöntem:
Karaciğer gibi frajil organlarda hemoraji kontrolü için efektif doku kompresyonu sağlarken sütürlerin dokuyu kesmesini engelleyen absorbe olabilen plaklarla desteklenmiş sütür kullanımı metodunu geliştirdik.
Metodumuzda dokuyu kuvvetli polyglactin sütürlerden oluşan bağlamalarla iki taraflı komprese eden ve aynı zamanda solid organın sütür tarafından kesilmesini de engelleyen absorbe olabilir ve esnek plaklar kullanarak hemostazı sağladık. Plakların yerinden kaymasını engellemek için sütürleri plaklara açılmış olan deliklerden ve karaciğer dokusundan geçirerek bağladık.
Bulgular:
Metodumuzun başarısını ve pratikliğini dört domuz üzerinde uygulayarak gösterdik. İki domuzda deneysel karaciğer yaralanması oluşturduk ve diğer ikisinde rezeksiyon gerçekleştirdik. Hepatik yaralanma oluşturduğumuz iki domuzda metodumuzu kullanarak kanama denetimi başarıyla gerçekleştirildi. Öbür iki domuzda sağ ve sol loblara ikişer rezeksiyon yapıldı. Operasyon süresince hiç kanama olmadı ve işlem toplam 45 dakika sürdü. Postoperatif dönemde komplikasyon görülmedi. Karaciğer fonksiyon testleri yedinci günde operasyona bağlı olarak yüksek bulunurken otuzuncu günde normal sınırlardaydı. Altı ay sonra yapılan laparotomilerde sütür ve plakların emildiği ve yaralanan dokuların tamamen iyileştiği görüldü. Yapılan histopatolojik incelemede plak aplikasyon bölgesinin fibrozisle iyileştiği gözlendi ve başka patoloji saptanmadı.
Sonuç:
Sonuç olarak bu metodun uygun lokalizasyondaki travmatik yaralanmalar ve elektif rezeksiyonlarda güvenle kullanılabileceği kanaatindeyiz.
Introduction
Hepatic trauma surgery and elective hepatic resections always assume a high risk of intraoperative and postoperative hemorrhage. Although the mortality rate is decreasing with the refinement of surgical techniques, instruments, postoperative care, and bleeding during parenchyma transection remain critical hurdles to overcome [1]. Currently, some instruments, such as the Cavitron ultrasound aspirator [1, 2], water jet knife [1, 3], Harmonic scalpel [1, 4] and microwave coagulator [1, 5] are used to facilitate hepatic resections. But such equipment is expensive and can only be found in special centers. An easy and cheap method that can be applied in every center is still desired. We have designed a method to further simplify hemorrhage control and parenchyma transection procedures for various types of hepatic resection. We decided to test our method first in the pig model and designed a preliminary study involving four pigs.
Materials and Methods
The approval of the GATA Ethics Committee was received for the study. The four pigs were divided into two groups; hepatoraphy related to traumatic injury was performed on two of the pigs, whereas elective irregular, extensive hepatectomies were applied on the right and left lobes of the other two pigs. To determine their value in the early stages, post-anesthetic blood samples were taken from the subjects, and their ALP, AST, ALT, bilirubin and hemoglobin values were studied. The hemoglobin value was also checked by drawing blood at the end of the operation. Subjects were monitored, and arterial blood pressure and pulse follow-ups were carried out.
Blunt lacerations were generated in three separate areas, including two on the right lobes and one on the left lobes in the pigs in the traumatic group. After that, hemostasis was obtained by suturing these lacerations with the help of the absorbable plaques. The absorbable plaques used in this study are shown in Figure 1.
Figure 1.
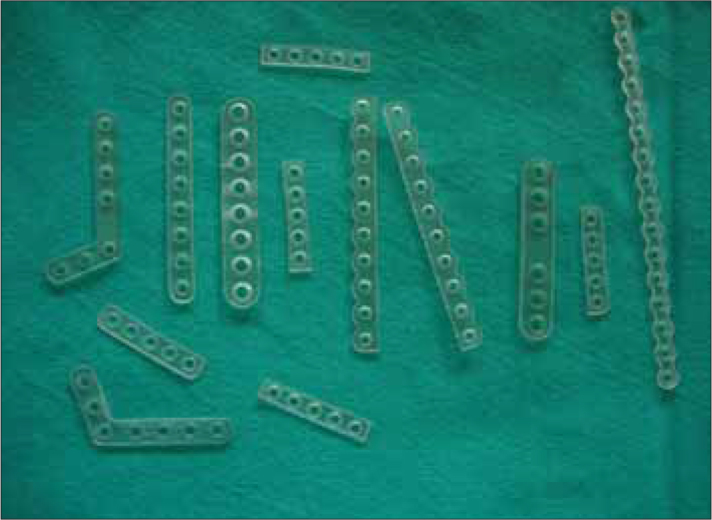
Absorbable plaques used
As for the elective hepatectomy group, sutures supported by absorbable plaques were first bound to the areas where resection would be performed to obliterate the bile ducts and stop the bleeding in the area of resection. Then, irregular hepatectomies were formed on the right and left lobes by performing resection on the areas that would be resected directly by the use of the scalpel.
A 12-cm long, straight needle and vicryl no. 1 were used for the plaque-supported suture. The suture that had initially been passed through the hole at one end of the plaque was then reeved entirely through the application area of the liver. After that, the same suture was passed through the hole at the other end of the plaque and the liver entirely, and once it was reeved through the two plaques on the other side of the liver, the suture was made ready for tying. While the first assistant pressed the two plaques together to compress the liver tissue, the operator tied a knot, and thus the liver tissue was compressed between the two plaques (Figures 2, 3).
Figure 2.
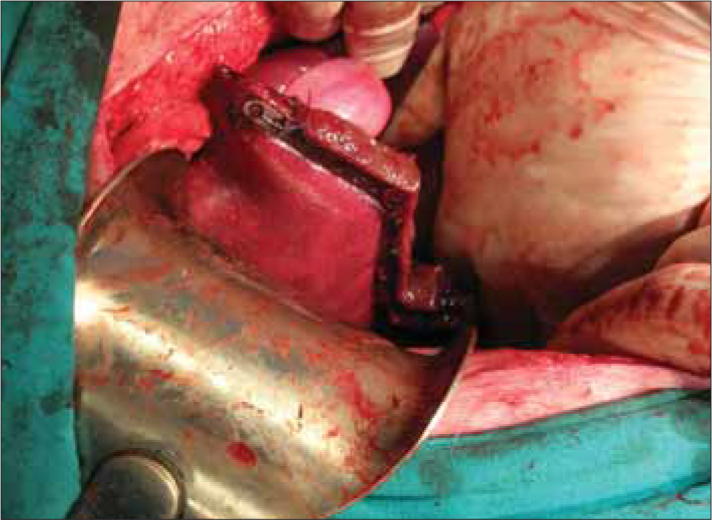
Resected liver after the plaque suture application
Figure 3.
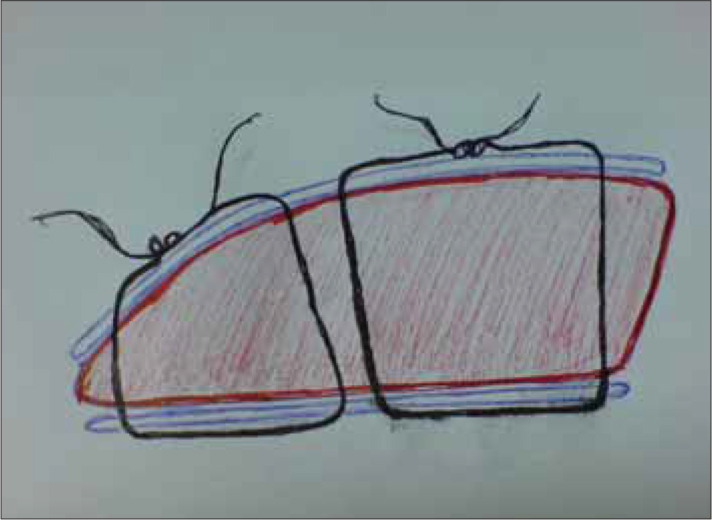
Schematic sketch of absorbable plaque application
The same process was repeated along the planned resection line or the generated KC laceration. Bleeding in the area of hepatorrhaphy stopped, and demarcation occurred in the area where the resection would be performed. Later, the resection was performed with a scalpel by cutting the liver tissue that was on the resection side of the plaques. The operation was concluded after the closure of the abdominal layers.
Animals were given water six hours later and fed the next day. The same tests were repeated by drawing blood from the animals on the seventh and the thirtieth postoperative days. Animals were monitored for six months, and at the end of this period, they were sacrificed by means of high-dose general anesthesia, autopsies were performed, and blood samples were taken. The regions of the liver where hepatorrhaphy and resection had been performed were histopathologically observed.
Results
In the blunt trauma group, it was observed that the plaque-supported sutures applied to the liver immediately stopped the bleeding by compressing the liver tissue adequately and without cutting it; the operation was easily performed without any obstructions. In this group, after the hepatic injury had been generated, hepatorrhaphy was completed in 33 minutes on one of the animals and in 37 minutes on the other. Furthermore, bleeding was successfully stopped, and no biliary leakage was observed.
As for the group on which elective resection was performed, it took 25 minutes to complete the resection on one of the animals, by forming the resection line via plaques and sutures, and 34 minutes on the other. Resections were completed without any bleeding in elective resections. The application of methods, such as the pringle maneuver to interrupt the flow of blood to the liver, was not needed. No biliary leakage from resection lines occurred during the operation.
When the postoperative blood biochemistry of the animals was analyzed on the seventh day, AST and ALT values were observed as being higher than in the beginning. The blood samples taken on the thirtieth day, however, indicated that AST and ALT values were normal. Subjects’ hemoglobin, ALP and bilirubin values remained normal both on the seventh and the thirtieth postoperative days (Table 1).
Table 1.
Serum ALP, AST, ALT, bilirubin and hemoglobin levels
| Subject 1 | Subject 2 | Subject 3 | Subject 4 | Normal Ranges | ||
|---|---|---|---|---|---|---|
| Preoperative | ALP | 49 | 66 | 51 | 55 | 35–110 |
| AST | 41 | 39 | 50 | 51 | 30–61 | |
| ALT | 23 | 35 | 27 | 33 | 11–45 | |
| Bilirubin | 0.5 | 0.1 | 0.2 | 0.4 | 0–0.5 | |
| Hemoglobin | 13.4 | 14.2 | 15.1 | 15.3 | 10–16 | |
| ALP | 61 | 68 | 59 | 51 | 35–110 | |
| Postoperative (Day 7) | AST | 98 | 103 | 109 | 95 | 30–61 |
| ALT | 80 | 88 | 91 | 77 | 11–45 | |
| Bilirubin | 0.6 | 0.2 | 0.1 | 0.4 | 0–0.5 | |
| Hemoglobin | 11.1 | 12.4 | 12.9 | 13.2 | 10–16 | |
| ALP | 51 | 59 | 66 | 49 | 35–110 | |
| Postoperative (Day 30) | AST | 49 | 53 | 50 | 48 | 30–61 |
| ALT | 31 | 37 | 30 | 38 | 11–45 | |
| Bilirubin | 0.3 | 0.2 | 0.3 | 0.3 | 0–0.5 | |
| Hemoglobin | 13.6 | 15.1 | 15.4 | 14.9 | 10–16 |
Autopsies performed six months later demonstrated that plaques and sutures were absorbed, resected areas were healed through a thin fibrosis formed in the hepatic resection line, and fibrosis and regeneration took place in the hepatorrhaphy areas. No pathologies were found except for the normal post-laparotomy abdominal adhesions.
Discussion
The liver is the most frequently injured organ in blunt abdominal injuries [6]. Due to its anatomy and fragile tissue, the liver is often affected by blunt trauma. In hepatic injuries, bleeding that is hard to control for the same reasons; the organ’s tender and fragile structure makes it difficult to achieve hemostasis by means of suturing and cauterization. Hemostasis sometimes necessitates high-tech cauterization equipment [1–5], and since such expensive equipment is not available at all centers, many hardships are faced in the treatment of this type of case. Occasionally, segmental or irregular resections are needed in cases of uncontrollable bleeding [6]. The same anatomical and structural particularities cause similar difficulties and obstruct the operation in elective hepatic resections.
The basic reason that constitutes the problem is that, owing to the organ’s fragility, the suture cuts through the tissue during the process of tying, and the defect grows further and sometimes bleeds more. The force that must be applied to the suture to stop bleeding surpasses the force that the liver tissue can handle. Thus, the suture cuts through the tissue, and the operation fails.
Despite the fact that there are many expensive high-tech devices that are used to facilitate hemostasis, these devices are not available at every center because of financial factors. However, traumatic liver injuries can take place anywhere, and any center may have to handle these cases. Therefore, the demand still exists for a practical method that can be applied at every center and by all surgeons regardless of their experience.
One of the easiest, cheapest and most applicable methods is the use of Chang’s needle [1]. This method involves suturing the transection line that covers the liver, using a special apparatus called Chang’s needle, before the transection of the liver itself [1]. But still, bleeding occurs in this method too, as the liver capsule and parenchyma are torn if more than a certain amount of force is applied to tighten the sutures. After the sutures are tied, the major blood vessels and bile ducts encountered during the transection of the liver must be tied in isolation [1]; and if any of these vessels or ducts is overlooked, it later leads to hemorrhage or biliary leakage. Moreover, the isolated tying process extends the duration of the surgery. Other technologically advanced electrosurgical devices also necessitate the isolated tying of major vessels, which, again, results in a loss of time and complications and morbidity caused by unnoticed vessels and bile ducts [1–5].
The distinctiveness of our method lies in the use of absorbable plaques that enable the sutures to be tied by applying an adequate amount of compression without tearing the liver. Since the liver is compressed sufficiently, bile ducts and vessels are obliterated, and the resection is carried out without isolated tying. Traumatic hemorrhages can be contained easily via the same mechanism, while planned resections are conveniently performed.
With the application of this method, planned resections have been completed without any bleeding and in a very short time; trauma-induced hemorrhages have also been swiftly contained. Moreover, no biliary leakage has occurred from laceration surfaces or rehabilitated areas of injury. The animals’ liver enzymes that tested high on the seventh postoperative day were shown to be normal by blood samples taken on the thirtieth day. The high enzyme values were due to hepatocyte injuries occurring in the course of operation, but these values improved later on. It is emphasized in the medical literature that one of the major causes of high liver enzyme values following hepatic resection is the traumatic effect of the resection on the liver [7]. Such high values stemming from hepatocyte injuries are also observed in the postoperative period of surgeries that are performed via conventional methods and of those that apply advanced technological equipment [2–5, 7]. In this respect, this method is not considered to be dissimilar to other methods.
As for the issue of bleeding, trauma-induced hemorrhages were contained in a very short time without disturbing hemodynamic balances. Moreover, planned resections were completed without any bleeding. As a result of this, no significant fluctuations were observed in postoperative hemoglobin values.
In other types of hepatectomies methods, such as the pringle maneuver and hepatic vein or inferior vena cava exclusion that involves interrupting the hepatic blood flow and rendering the liver ischemic for a while which may result in hemodynamic disturbance, are required to reduce bleeding [7, 8]. In our method, blood flow is permanently interrupted by means of plaques and sutures only in the segment that is to be removed; therefore, the operation can be performed without damaging the other segments. This is especially important in the resection of cirrhosis-related malignancies because it protects the other segments from ischemia.
To perform a successful hepatic resection, it is fundamental to have sufficient surgical skills and management to leave the liver tissue intact and functional as well as to cause minimal ischemia and reperfusion injury [1]. In almost all the other methods, stopping the hepatic inflow and outflow as well as causing ischemia and reperfusion injuries-even though it is limited to the liver – cannot be avoided during the course of surgery. However, with our method, the resection can be performed without any of these.
If the plaque-supported sutures used in our method for the control of traumatic bleeding are located anatomically so as to obstruct the bile ducts, the segment whose excretory ducts are obliterated needs to be resected in order not to cause biliary stasis. This can be done in a very short time and without any hemorrhage because the circulation stops along with the biliary drainage.
Within the six months following the resection and hemorrhage control, the materials used in this method are absorbed, and no foreign bodies remain. No abnormal adhesions were observed inside the abdomen after the application of this method. The resected and repaired surfaces of the liver compressed between the two plaques and the suture healed smoothly by a subtle fibrosis.
In conclusion, we believe that the method we have successfully applied on pigs for hepatic resection and control of traumatic bleeding can also be performed on humans in cases of hepatic injuries and resections in suitable localizations.
Footnotes
Conflict of interest statement: The authors declare that they have no conflict of interest to the publication of this article.
References
- 1.Chang YC, Nagasue N, Chen CS, Lin XZ. Simplified hepatic resections with the use of a Chang’s Needle. Ann Surg. 2006;243:169–72. doi: 10.1097/01.sla.0000197380.33169.6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hodgson WJ, DelGuercio LR. Surgical technique: preliminary experience in liver surgery using the ultrasonic scalpel. Surgery. 1984;95:230–4. [PubMed] [Google Scholar]
- 3.Persson BG, Jeppsson B, Tranberg KG, et al. Transection of the liver with a waterjet. Surg Gynecol Obstet. 1989;168:267–8. [PubMed] [Google Scholar]
- 4.Amaral JF. The experimental development of an ultrasonically activated scalpel for laparoscopic use. Surg Endosc Laparosc. 1994;4:92–9. [PubMed] [Google Scholar]
- 5.Tabuse K, Katsumi M, Kobayashi Y, et al. Microwave surgery: hepatectomy using a microwave tissue coagulator. World J Surg. 1985;9:136–43. doi: 10.1007/BF01656265. [DOI] [PubMed] [Google Scholar]
- 6.Günay K, Taviloğlu K, Kemertaş K, Eskioğlu E, Türel Ö. Künt Karaciğer Yaralanmaları 278 Olgunun Değerlendirilmesi. Ulus Travma Acil Cerrahi Derg. 1995;1:1–6. [Google Scholar]
- 7.Giovanni I, Chiarla C, Giuliante F, et al. Analiysis of the componenys of hyper transaminasemia after liver resection. Clin Chem Lab Med. 2007;45:357–60. doi: 10.1515/CCLM.2007.078. [DOI] [PubMed] [Google Scholar]
- 8.Belli G, Limongelli P, Belli A, et al. Ultrasonically activated device for parenchmal division during open hepatectomy. HPB. 2008;10:234–8. doi: 10.1080/13651820802166906. [DOI] [PMC free article] [PubMed] [Google Scholar]


