Abstract
A 25-year-old man presented with symptoms of syncope, cough, headache and hemoptysis. Cranial MR and venography showed thrombus formation in the right transverse sinus and superior sagittal sinus. Computed tomographic pulmonary angiography (CTPA) showed an embolic thrombus in the right pulmonary truncus and lung abscess. The patient was young, and there were no signs of lower extremity deep venous thrombosis or other major risk factors for pulmonary embolism (PE) including cardiac anomaly. The only risk factor we were able to identify was the presence of the prothrombin G20210A gene mutation. Anticoagulant treatment with oral warfarin (10 mg daily) and imipenem (4X500 mg) was started. The patient was hospitalized for antibiotic and anticoagulation therapies for three weeks and was discharged on lifelong treatment with warfarin (5 mg daily).
Keywords: Prothrombin G20210A gene mutation, pulmonary embolism, cerebral venous thrombosis
Özet
Venöz tromboemboli (VTE) geniş klinik manifestasyonlarla ortaya çıkabilir. VTE gelişiminde trombofili varlığı olası nedenlerden biridir. Vaka: 25 yaşında erkek hasta senkop, öksürük, başağrısı ve hemoptizi ile başvurdu. Kranyal MR ve venografi ile sağ transvers sinus ve superior sagital sinusta thrombus saptandı. Bilgisayarlı tomografik pulmoner anjiografi ile sağ pulmoner trunkusta embolik trombüs ve akciğer absesi izlendi. Hasta genç olup pulmoner emboli açısından alt ekstremitede derin ven trombüsü bulgusu veya herhangi bir major risk faktörü saptanmadı. Hastada saptanan tek risk faktörü protrombin G20210A gen mutasyonu olarak bulundu. Hastaya günlük 10 mg oral warfarin ve imipenem 4X500 mg 3 hafta verildi. Tedavi sonrası günlük 5 mg warfarin ömür boyu kullanması önerilerek taburcu edildi. Sonuç: Genç bir hastada serebral venöz trombüsün komplikasyonu olarak gelişen genetik kaynaklı pulmoner emboli ve akciğer absesi nadir olup akılda tutulması önerilir.
Introduction
Venous thromboembolism (VTE) has a wide spectrum of clinical manifestations. The presence of thrombophilia in patients can provide a possible explanation for development of VTE. The most common genetic causes of thrombophilia include two mutations in the genes coding for coagulation factor V and prothrombin [1]. Cerebral venous thrombosis (CVT) is a rare event and often occurs in young people [2]. We report a case of non-traumatic CVT with secondary PE associated with the prothrombin G20210A gene mutation.
Case Report
A 25-year-old man presented with symptoms of fever, cough, headache, hemoptysis and syncope. Upon exam, he had crackles in the right lung. No signs of lower extremity deep venous thrombosis were detected. Electrocardiography, ecocardiographic evaluation and arterial blood gas analysis were normal. Chest X-ray showed a closed right costal phrenic sinus and consolidation and a cavitary lesion in the lower right zone. X-ray computed tomographic pulmonary angiography (CTPA) showed an embolic thrombus in the right pulmonary truncus (Figure 1). Cranial MR and venography revealed a thrombus in the right transverse sinus and superior sagittal sinus (Figure 2). Thorax CT showed pleural effusion 3 cm thick in the right pleura, as well as consolidation and a cavitary lesion in the right lower lobe. The patient was young and neither signs of lower extremity deep venous thrombosis nor other major risk factors for pulmonary emboli were detected. The only risk factor we were able to identify was the presence of the prothrombin G20210A gene mutation. Anticoagulant treatment with warfarin (10 mg daily) and imipenem (4x500 mg) was started. The patient was hospitalized for antibiotic and anticoagulation therapies for 3 weeks and was discharged on life-long treatment with warfarin (5 mg daily).
Figure 1.
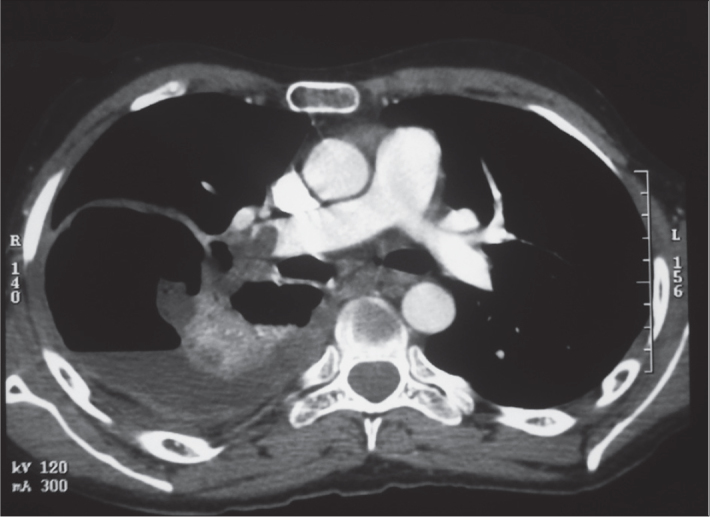
Computed tomographic pulmonary angiography (CTPA)
Figure 2.

Cranial MR and venography
Discussion
Although venous thrombosis is frequently found simultaneously at several anatomic sites, occurrence of CVT and PE without evidence of systemic venous thrombosis is unusual [2, 3]. Clinical risk factors for venous thromboembolism include increasing age, prolonged immobility, stroke, paralysis, previous venous thromboembolism, cancer, major surgery, trauma, obesity, varicose veins, cardiac dysfunction, pregnancy and nephritic syndrome[4]. Our patient had none of these risk factors. Thrombophilia and oral contraceptives are the most common risk factors for CVT [2]. Factor V (FV) Leiden variant and the prothrombin G20210A mutation are the most common genetic causes of thrombophilia and deep vein thrombosis (DVT). Kovac et al. reported that patients with the prothrombin G2021A mutation had an increased risk of more severe clinical manifestations than those with FV Leiden or without thrombophilia [1].
In contrast to DVT or PE, CVT is a rare disease. The clinical features of CVT consist of headache, focal deficits, seizures and impaired consciousness. In the case study reported above, headache and syncope were the preceding symptoms.
The association of CVT and PE may be explained by a detached thrombus and a global prothrombotic state [3]. PE may be related to a detached thrombus from the cranial venous sinus in our case because neurological symptoms appeared earlier than those of the respiratory symptoms. We think that CVT might have formed before the pulmonary thrombus. Cakmak et al. reported 23 cases of PE in CVT patients and showed that 95% of CVT patients with PE died [3]. Another review of the literature published between 1942 and 1990 yielded 203 cases of intracranial venous thrombosis. The overall mortality rate was 49.3%. In 23 cases (11.3%), the venous sinus thrombosis was associated with pulmonary emboli; in these 23 cases, the overall mortality rate was 95.6%. In the 203 cases reviewed, those patients who received anticoagulation therapy also had significantly better outcomes [5].
To treat the PE in our patient, we chose anticoagulant therapy consisting of low molecular weight heparin and warfarin. In patients with severe thrombophilia who have two or more prothrombotic abnormalities or antiphospholipid syndrome, anticoagulants should be given for life because of the risk for further thrombotic episodes [6]. We also planned the anticoagulant warfarin treatment for life because of the confirmed gene mutation in our patient.
In conclusion, the cause of cerebral venous thrombosis and pulmonary embolism in this young patient was most likely related to the FV Leiden mutation and prothrombin G20210A mutation. PE as a complication of cerebral venous sinus thrombosis with genetic predisposition and lung abscess in a young patient is rare and should be considered in future cases. Prompt treatment for PE and CVT should be applied according to treatment guidelines.
Footnotes
Conflict of interest statement: The authors declare that they have no conflict of interest to the publication of this article.
References
- 1.Kovac M, Mitic G, Mikovic Z, et al. Type and Location of Venous Thromboembolism in Carriers of Factor V Leiden or Prothrombin G20210A Mutation Versus Patients With No Mutation. Clin Appl Thromb Hemost. 2008;16:66–70. doi: 10.1177/1076029608320721. [DOI] [PubMed] [Google Scholar]
- 2.Ferro JM, Canhao P, Stam J, Bousser MG, Barinagarrementeria F. Prognosis of cerebral vein and dural sinus thrombosis:results of international study on cerebral vein and dural sinus thrombosis. Stroke. 2004;35:664–70. doi: 10.1161/01.STR.0000117571.76197.26. [DOI] [PubMed] [Google Scholar]
- 3.Cakmak S, Mighoghossian N, Desestret V, Hermier M, Cartalat-Carel S, Derex L, et al. Pulmonary embolism: An unusual complication of cerebral venous thrombosis. Neurology. 2005;65:1136–7. doi: 10.1212/01.wnl.0000178987.06734.54. [DOI] [PubMed] [Google Scholar]
- 4.Geerts WH, Heit JA, Clagett GP, et al. Prevention of venous thromboembolism. Chest. 2001;119:132–75. doi: 10.1378/chest.119.1_suppl.132s. [DOI] [PubMed] [Google Scholar]
- 5.Diaz JM, Schiffman JS, Urban ES, Maccario M. Superior sagittal sinus thrombosis and pulmonary embolism: A syndrome rediscovered. Acta Neurol Scand. 1992;86:390–6. doi: 10.1111/j.1600-0404.1992.tb05106.x. [DOI] [PubMed] [Google Scholar]
- 6.Khamashta MA, Cuadrado MJ, Mujic F, Taub NA, Hunt BJ, Hughes GR. The management of thrombosis in the antiphospholipid-antibody syndrome. N Engl J Med. 1995;332:993–7. doi: 10.1056/NEJM199504133321504. [DOI] [PubMed] [Google Scholar]


