Abstract
Objective:
To evaluate the effects of two different spinal isobaric levobupivacaine doses on spinal anesthesia characteristics and to find the minimum effective dose for surgery in patients undergoing transurethral resection (TUR) surgery.
Materials and Methods:
Fifty male patients undergoing TUR surgery were included in the study and were randomized into two equal groups: Group LB10 (n=25): 10 mg 0.5% isobaric levobupivacaine (2 ml) and Group LB15 (n=25): 15 mg 0.75% isobaric levobupivacaine (2 ml). Spinal anesthesia was administered via a 25G Quincke spinal needle through the L3–4 intervertebral space. Sensorial block levels were evaluated using the ‘pin-prick test’, and motor block levels were evaluated using the ‘Bromage scale’. The sensorial and motor block characteristics of patients during intraoperative and postoperative periods and recovery time from spinal anesthesia were evaluated.
Results:
In three cases in the Group LB10, sensorial block did not reach the T10 level. Complete motor block (Bromage=3) did not occur in eight cases in the Group LB10 and in five cases in the Group LB15. The highest sensorial dermatomal level detected was higher in Group LB15. In Group LB15, sensorial block initial time and the time of complete motor block occurrence were significantly shorter than Group LB10. Hypotension was observed in one case in Group LB15. No significant difference between groups was detected in two segments of regression times: the time to S2 regression and complete sensorial block regression time. Complete motor block regression time was significantly longer in Group LB15 than in Group LB10 (p<0.01).
Conclusion:
Our findings showed that the minimum effective spinal isobaric levobupivacaine dose was 10 mg for TUR surgery.
Keywords: Levobupivacaine, Spinal anesthesia, Transurethral surgery
Özet
Amaç:
Spinal anestezi özellikleri iki farklı spinal izobarik levobupivakain dozlarının etkilerini değerlendirmek ve transüretral rezeksiyon (TUR) ameliyatı geçiren hastalarda cerrahi için etkili en düşük dozu bulmak.
Gereç ve Yöntem:
TUR ameliyatı Elli erkek hasta çalışmaya alındı ve iki eşit gruba ayrıldı: Grup LB10 (n=25): 10mg %0.5 izobarik levobupivakain (2 ml) ve Grup LB15 (n=25): 15 mg %0.75 izobarik levobupivakain (2 ml). Spinal anestezi L3–4 intervertebral uzayda bir 25G Quincke spinal iğne ile uygulandı. Duyusal blok seviyeleri ‘pin-prick testi’ ile değerlendirildi ve motor blok seviyeleri ‘Bromage ölçeği’ ile değerlendirildi. Spinal anestezi ile intraoperatif ve postoperatif dönem ve iyileşme süresi boyunca hastaların duyusal ve motor blok özellikleri değerlendirildi.
Bulgular:
Grup LB10 üç durumlarda, duyusal blok seviyesi T10 ulaşmadı. Komple motor blok (Bromage=3) Grup LB10 ve Grup LB15 beş olguda sekiz olguda görülmedi. Tespit edilen en yüksek duyusal dermatomal Düzeyli Grup LB15 daha yüksekti. Grup LB15 olarak, duyusal blok başlangıç zamanı ve tam motor blok oluşma süresi Grup LB10 anlamlı olarak kısa bulundu. Hipotansiyon Grup LB15 bir durum gözlenmiştir. S2 regresyon ve tam duyusal blok gerileme zaman zaman: Gruplar arasında anlamlı bir fark regresyon kez iki segment saptandı. Komple motor blok gerileme zamanı Grup LB10 (p<0.01) daha Grubu LB15 anlamlı olarak daha uzundu.
Sonuç:
Bu bulgular en az etkili spinal izobarik levobupivakain doz TUR ameliyatı için 10 mg olduğunu gösterdi.
Introduction
Endoscopic surgical interventions are preferred over open surgery methods because of the ease of application and the shorter hospital discharge times. Most of these patients have a risk of severe respiratory and cardiovascular diseases due to advanced age. Therefore, spinal anesthesia is the widely preferred anesthesia method for urologic surgical interventions because complications are seen less frequently compared to general anesthesia [1–4].
Levobupivacaine is an S(−) enantiomer of bupivacaine and a long-acting local anesthetic with an amide structure [5, 6]. Levobupivacaine is available in isobaric form in 0.25%, 0.5% and 0.75% concentrations. All three forms are used in various surgical interventions and delivery, including spinal anesthesia, epidural analgesia, postoperative pain management and peripheral blocks [7, 8]. Levobupivacaine is more favorable compared to bupivacaine and ropivacaine in terms of cardiovascular and central nervous system toxicity, which has been proven in preclinical and clinical studies [9–11].
The effects of levobupivacaine and bupivacaine in spinal anesthesia for geriatric patients who undergo transurethral surgery have been compared [1–3]. Although the effectiveness of hyperbaric and isobaric forms of levobupivacaine in similar doses has been investigated for TUR surgery [4], no studies are available on the required minimum dose of levobupivacaine for spinal anesthesia in this patient group.
In this study, 10 mg and 15 mg of isobaric levobupivacaine were administered into the subarachnoid space for spinal anesthesia in TUR operations while keeping the major factors that could affect local anesthetic distribution in CSF constant. We aimed to determine which dose would provide sufficient anesthesia for TUR surgery by evaluating its effects on sensorial and motor characteristics following spinal anesthesia.
Materials and Methods
Our study was conducted after ethical approval of Uludag University Medical Faculty had been obtained (29.04.2008, number 2008-9/25). A total of 50 male patients between 40–80 years of age and ASA (American Society of Anesthesiologists) I–II who would undergo elective endoscopic TUR surgery were included in the study. All patients were orally informed about the aim of the study and details prior to operation, and written informed consent was obtained from the volunteers who accepted to participate. Patients who had a known allergy to local anesthetics, an infection or a previous operation that concerned the intervention site, coagulation disorder or anticoagulant drug use and patients who did not accept spinal anesthesia were excluded.
Patients were divided into two equal groups before spinal anesthesia by randomization according to the closed envelope method:
Group LB10 (n=25): 10 mg (2 ml) of 0.5% isobaric levobupivacaine
Group LB15 (n=25): 15 mg (2 ml) of 0.75% isobaric levobupivacaine
Patients who were taken to the operation room without premedication were monitored with electrocardiography (ECG), noninvasive blood pressure and pulse oximetry. Ringer lactate infusion (1000 ml) was initiated by an intravenous route before spinal anesthesia. Spinal anesthesia was conducted in the left lateral decubitus position using a midline approach from the L3–4 intervertebral space and 25G Quincke spinal needle. After CSF flow was seen, 2 ml of different doses of isobaric levobupivacaine was injected into the subarachnoid space to provide spinal anesthesia in both groups. Subjects were turned to the supine position just after the injection. Sensorial block dermatome level was assessed using the pin-prick test (analgesia test with needle) and motor block was assessed using the Bromage scale [12] (0: no motor block; 1: knee flexion is present, hip flexion is absent; 2: foot flexion is present, knee flexion is absent, 3: no movement in lower extremity).
Intraoperatively, sensorial and motor functions were assessed with 2 min intervals for 20 minutes after spinal anesthesia. During the postoperative period, assessments were performed every 20 minutes until motor and sensorial functions were fully regained. Anesthetists who evaluated intraoperative and postoperative parameters and subjects were blinded to the study.
During the intraoperative period, vital parameters (mean arterial blood pressure (MAP), heart rate (HR) and peripheral oxygen saturation (SpO2) were measured and recorded every 5 minutes. Spinal anesthesia characteristics, such as sensorial block initiation time (time until maximum sensorial block), complete motor block time (time until Bromage score was 3 in both lower extremities), uppermost sensorial block dermatome level and complications (emesis, vomiting, hypotension, bradycardia, shivering, arrhythmia, etc.), were recorded. A 20% or more reduction in basal value of mean arterial pressure was accepted as intraoperative hypotension; heart rate below 50 bpm was accepted as intraoperative bradycardia. Ephedrine HCl (10 mg) was administered when hypotension developed, and 0.5 mg of atropine was administered when bradycardia developed.
During the postoperative period, the time to two segment regression of sensory block, the time to the regression of sensorial block dermatome level to S2, complete regression time of sensory block (i.e., time to first pain sensation of the patients), motor block complete regression time (time to Bromage=0) and complications (postspinal headache, low back pain, transient neurological symptoms and the other complications) were recorded. Urinary retention could not be evaluated as a complication because the urethral catheter remained in patients for two postoperative days. When a patient complained of postoperative pain, 75 mg of intramuscular diclofenac sodium was administered, and doses were recorded.
Statistical analysis of data was performed using the SPSS 13.0 statistical analysis program in the laboratory of Uludag University, Department of Biostatistics. Kruskal-Wallis and Mann-Whitney U tests were used for intergroup comparisons. Wilcoxon Signed Ranks test was used for within group comparisons. Fisher’s Exact test was applied for the analysis of categorical data. Constant variables are presented as the mean±standard deviation (SD) or median (minimum-maximum). A p value of <0.05 was taken as statistical significance.
Results
Demographic data
No significant differences between groups were detected in demographic data or operation time (p>0.05) (Table 1).
Table 1.
Demographic data of the patients
| Group LB10 (n=25) | Group LB15 (n=25) | p | |
|---|---|---|---|
| Age (year) | 64±8 | 64±12 | >0.05 |
| Weight (kg) | 74±12 | 79±13 | >0.05 |
| Height (cm) | 170±6 | 170±6 | >0.05 |
| ASA I/II | 8/17 | 9/16 | >0.05 |
| Operation time (min) | 63±36 | 47±23 | >0.05 |
Data are given as median±SD or case number (n), ASA: American Society of Anesthesiologists
Vital signs
Basal values of the patients before spinal anesthesia and changes in HR, MAP and SpO2 with time are presented in Figures 1, 2 and 3, respectively. No statistically significant differences were found between groups in intraoperative mean HR, MAP and SpO2 values (p>0.05).
Figure 1.
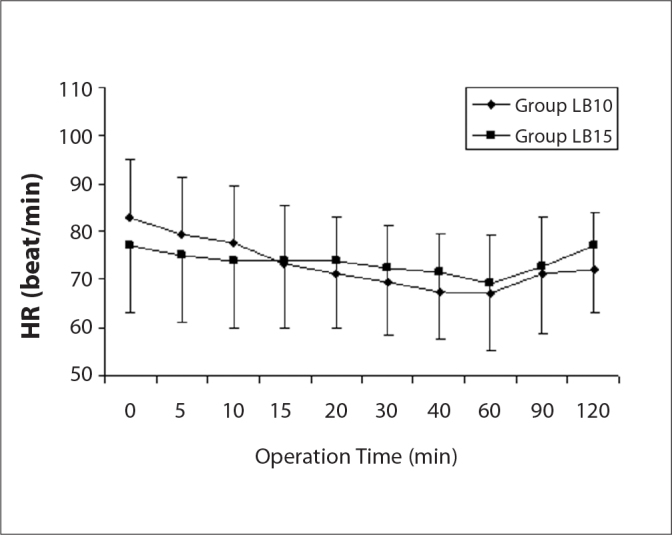
Preoperative heart rate (HR) values (mean±SD). p>0.05 at all times.
Figure 2.

Preoperative mean arterial pressure (MAP) (mean±SD). p>0.05 at all times.
Figure 3.

Preoperative peripheral oxygen saturations (SpO2) (mean±SD). p>0.05 at all times.
Spinal anesthesia characteristics
Intraoperative sensory and motor block characteristics after spinal anesthesia with levobupivacaine are presented in Table 2. In the LB15 group, the uppermost sensory block dermatome level was higher, and sensory block initiation time and complete block onset time were significantly shorter (p<0.05) (Table 2). However, sensory block did not reach to the T10 level in three cases in the LB10 group and in one patient in the LB15 group (p>0.05). Complete motor block (Bromage=3) did not occur in eight cases in the LB10 group and in five cases in the LB15 group (p>0.05). Changes in sensory block dermatome level with time after spinal anesthesia are presented in Figure 4. Statistically significance was detected at 12, 14, 16 and 18 minutes between mean sensory block dermatome levels after spinal anesthesia (Figure 4).
Table 2.
Preoperative sensory and motor block characteristics after spinal anesthesia
| Group LB10 (n=25) | Group LB15 (n=25) | p | |
|---|---|---|---|
| The upper level of sensory block | T8 (T8–T12) | T6 (T6–T11)* | <0.05 |
| Sensory block onset time (min) | 7.8±6.3 | 6.7±5.4 | >0.05 |
| Time to complete motor block (min) | 10.7±5.2 | 8.1±6.5 | >0.05 |
Data are given as mean±SD or median (minimum-maximum)
Figure 4.

Sensory block dermatomal level after spinal anesthesia (mean±SD). *p<0.05, statistical significance.
Sensory and motor block recovery times during the postoperative period after spinal anesthesia are presented in Table 3. A significant difference was not detected between groups in the time to two segment regressions of sensory block, regression time of sensory block level to S2 and complete regression time of sensory block. Complete motor block regression times were significantly longer in the LB15 group compared to the LB10 group (p<0.01) (Table 3).
Table 3.
Sensory and motor block recovery times after spinal anesthesia
| Group LB10 (n=25) | Group LB15 (n=25) | p | |
|---|---|---|---|
| Two segment regression time (min) | 29.2±23.9 | 36.0±24.1 | >0.05 |
| Time to S2 regression (min) | 51.6±34.7 | 58.1±27.9 | >0.05 |
| Complete regression of sensory block (min) | 227±46 | 243±77 | >0.05 |
| Complete regression of motor block (min) | 266±80 | 326±25* | <0.01 |
Data are given as mean±SD
Clinically significant hypotension developed in one case in Group LB15 during the intraoperative period after spinal anesthesia, and 10 mg of intravenous ephedrine HCl was applied to the patient for treatment; an additional dose was not required. Shivering developed in two cases in Group LB15. A significant difference in side effects was not detected between the two groups (p>0.05). Postoperative diclofenac sodium need was observed in one case in the Group LB10. Post-spinal headache and low back pain were not observed.
Discussion
During the preparation phase of our study, 5 cases were administered 5 mg (2 ml) of 0.25% isobaric levobupivacaine for spinal anesthesia (Group LB5). This group was not included in the study because of insufficient sensory and motor block for surgery.
In a vast majority of dose studies, a significant increase in spinal anesthesia level and mean anesthesia time by an increase in local anesthetic dose has been reported. Povey et al. [13] analyzed 25 and 30 mg of isobaric bupivacaine and observed significantly high cephalad spread in the 30 mg group of intrathecal bupivacaine. Siaens et al. [14] compared 10 mg hyperbaric bupivacaine, 10 mg isobaric bupivacaine and 15 mg isobaric bupivacaine in spinal anesthesia and found the highest sensory block level and longest mean anesthesia time in the 15 mg group. Ben-David et al. [15] divided subjects undergoing arthroscopy into 4 groups and used 15, 10, 7.5 and 5 mg of bupivacaine in spinal anesthesia by dilution with saline. They detected the maximum sensory block level as T5 in the 15 mg group and as T8 in the other groups. However in a few studies, the total local anesthetic dose that was injected into subarachnoid space did not directly affect anesthesia level [16, 17]. In our study, the intraoperative uppermost sensory dermatome level was detected in a higher level in the LB15 group compared to the LB10 group. The fact that sensory block was observed in higher levels as the local spinal anesthetic dose increased supports previous studies in the literature.
A spinal anesthesia level above the T10 skin dermatome provides sufficient sensory block [1]. Danelli et al. [5] found the mean highest sensory block level as T11 with intrathecal 3 ml isobaric levobupivacaine and T10 with 2 ml isobaric levobupivacaine. Schmidt et al. [16] found the mean uppermost sensory block level as T7 with 9 ml and 6 ml volumes, as T8 with a 3 ml volume and as T10 with a 2 ml volume in their study on intrathecal isobaric bupivacaine. In this study, cephalad distribution was prominently observed at lower dermatome levels with 2 ml isobaric bupivacaine spinal anesthesia. The choice of 2 ml of local anesthetic was thought to be safer than doses that we would generally study in patients with advanced age.
In our study, high spinal anesthesia levels that required a change to general anesthesia was not obtained in any case. However, significant hypotension developed in one out of 50 cases, and this subject responded to treatment with a single dose of intravenous ephedrine. These outcomes indicated that both of the levobupivacaine doses that were used in a geriatric patient population were safe. When the literature was evaluated, height and body weight were among the other demographic features that affect spinal anesthesia level [6, 18]. In our study, the groups were similar in all of these factors.
When recovery from spinal anesthesia was evaluated, Povey et al. [13] observed that recovery time was longer with 30 mg of 0.5% bupivacaine in spinal anesthesia compared to 25 mg. Siaens et al. [14] compared 10 mg hyperbaric bupivacaine, 10 mg isobaric bupivacaine and 15 mg isobaric bupivacaine in spinal anesthesia and found the longest anesthesia time in the 15 mg group. In our study, motor block recovery times in spinal anesthesia were significantly longer in the LB15 group compared to the LB10 group, which is similar to other studies. A significant difference was not found between groups in sensory block recovery times.
In our study of different doses of isobaric levobupivacaine on anesthesia characteristics in spinal anesthesia, the uppermost sensory block dermatome level was higher in the 15 mg levobupivacaine group compared to the 10 mg levobupivacaine group and sensory and motor block onset times were shorter. Motor block complete regression time was longer in the LB15 group compared to the LB10 group. Although 5 mg of 0.25% isobaric levobupivacaine for spinal anesthesia had insufficient sensory and motor block for surgery, our results indicated that 10 mg of isobaric levobupivacaine administration was the minimum dose for effective sensory and motor block in spinal anesthesia for TUR surgery.
Footnotes
Conflict of interest statement: The authors declare that they have no conflict of interest to the publication of this article.
References
- 1.Lee YY, Muchhal K, Chan CK. Levobupivacaine versus racemic bupivacaine in spinal anesthesia for urological surgery. Anaesth Intensive Care. 2003;31:637–41. doi: 10.1177/0310057X0303100604. [DOI] [PubMed] [Google Scholar]
- 2.Vanna O, Chumsang L, Thongmee S. Levobupivakain and bupivakain in spinal anesthesia for transurethral endoscopic surgery. J Med Assoc Thai. 2006;8:1333–9. [PubMed] [Google Scholar]
- 3.Cuvas O, Er AE, Ongen E, Basar H. Spinal anestesia for transuretral resection operations: bupivakain versus levobupivakain. Minerva Anestesiol. 2008;74:697–701. [PubMed] [Google Scholar]
- 4.Sen H, Purtuloglu T, Sızlan A, Yanarates O, et al. Comparison of intrathecal hyperbaric and isobaric levobupivacaine in urological surgery. Minerva Anestesiol. 2010;76:24–8. [PubMed] [Google Scholar]
- 5.Danelli G, Baciarello M, Di Cianni S, et al. Effects of baricity of 0.5% or 0.75% levobupivakain on the onset time of spinal anesthesia: a randomized trial. Can J Anaesth. 2008;55:501–6. doi: 10.1007/BF03016669. [DOI] [PubMed] [Google Scholar]
- 6.Taivainen T, Tuominen M, Rosenberg PH. Influence of obesity on the spread of spinal analgesia after injection of plain 0.5% bupivacaine at the L3–4 or L4–5 interspace. Br J Anaesth. 1990;64:542–6. doi: 10.1093/bja/64.5.542. [DOI] [PubMed] [Google Scholar]
- 7.Ivani G, Borghi B, van Oven H. Levobupivacaine. Minerva Anestesiol. 2001;9:20–3. [PubMed] [Google Scholar]
- 8.Gautier P, De Kock M, Huberty L, Demir T, Izydorczic M, Vanderick B. Comparison of the effects of intrathecal ropivacaine, levobupivacaine and bupivacaine for Caesarean section. Br J Anaeth. 2003;91:684–9. doi: 10.1093/bja/aeg251. [DOI] [PubMed] [Google Scholar]
- 9.Gristwood RW. Cardiac and CNS Toxicity of Levobupivacaine Strength of Evidence for Advantage Over Bupivacaine Drug Safety. 2002;25:153–63. doi: 10.2165/00002018-200225030-00002. [DOI] [PubMed] [Google Scholar]
- 10.Leone S, Di Cianni S, Casati A, Fanelli G. Pharmacology, toxicology and clinical use of new long acting local anesthetics, ropivacaine and levobupivacaine. Acta Biomed. 2008;79:92–105. [PubMed] [Google Scholar]
- 11.Foster RH, Markham A. Levobupivacaine: a review of its pharmacology and use as a local anaesthetic. Drugs. 2000;59:531–79. doi: 10.2165/00003495-200059030-00013. [DOI] [PubMed] [Google Scholar]
- 12.Gaggero G, Van Gessel E, Forster A, Gosteli P, Gamulin Z, Bromage PR. A comparison of the hydrochloride and carbondioxide salts of lidocaine and prilocaine in epidural analgesia. Act Anaesthesiol Scand. 1965;16:55–9. doi: 10.1111/j.1399-6576.1965.tb00523.x. [DOI] [PubMed] [Google Scholar]
- 13.Povey HM, Olsen PA, Pihl H, Jacobsen J. High dose spinal anaesthesia with glucose free 0.5% bupivacaine 25 and 30 mg. Acta Anaesthesiol Scand. 1995;39:457–61. doi: 10.1111/j.1399-6576.1995.tb04099.x. [DOI] [PubMed] [Google Scholar]
- 14.Siaens A, De Rood M. Effects of baricity and mass of bupivacaine solutions in spinal anesthesia. Acta Anaesthesiol Belg. 1987;38:89–95. [PubMed] [Google Scholar]
- 15.Ben David B, Levin H, Solomon E, Admoni H, Vaida S. Spinal bupivacaine in ambulatory surgery: the effect of saline dilution. Anesth Analg. 1996;83:716–20. doi: 10.1097/00000539-199610000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Schmidt A, Schwagmeier R, Broja E, Nolte H. The effect of volume and dosage of isobaric bupivacaine on the sensory spread of spinal anesthesia. Reg Anaesth. 1990;13:159–62. [PubMed] [Google Scholar]
- 17.Runza M, Albani A, Tagliabue M, Haiek M, LoPresti S, Birnbach DJ. Spinal Anesthesia Using Hyperbaric 0.75% Versus Hyperbaric 1% Bupivacaine for Cesarean Section. Anesth Analg. 1998;87:1099–104. doi: 10.1097/00000539-199811000-00021. [DOI] [PubMed] [Google Scholar]
- 18.Pitkanen MT. Body mass and spread of spinal anesthesia with bupivacaine. Anesth Analg. 1987;66:127–31. [PubMed] [Google Scholar]


