Abstract
Malignant glioma development after trauma is a rare occurrence. We report a glioblastoma multiforme case that developed after a depressed skull fracture. A 65-year-old man was admitted because of right sided hemiplegia, epilepsy and changes in consciousness due to a malignant glial tumor. He had been operated on for a left calvarial depression fracture caused by cerebral laceration thirty-five years before. Radiologic imaging revealed a large contrast-enhanced mass lesion at the left frontotemporoparietal junction under the depression site. The patient underwent urgent surgery, and radical excision of the mass was achieved. The histopathologic diagnosis was a high-grade glial tumor. Although the possibility of a pre-existing tumor rather than a trauma-induced tumor is very high, the presented case suggests that traumatic cerebral lesions may also be a predisposing factor for the development of malignant glial tumors.
Keywords: Brain injury, Glial cell tumors, Trauma
Özet
Travma sonrasında malign glioma gelişimi çok nadir gelişen bir durumdur. Atmışbeş yaşındaki erkek hasta malign glial tümör nedeniyle gelişen sağ hemipleji, epilepsi ve bilinç kaybı ile kliniğimize kabul edildi. Hasta 35 yıl önce sol kalvaryal depresyon fraktürüne bağlı serebral laserasyon nedeniyle ameliyat edilmiştir. Radyolojik görüntülemede depresyon alanının altında sol frontotemporoparyetal loblarda kontrast tutan büyük bir kitle lezyonu göstermekteydi. Hasta acil operasyona alınarak radikal kitle eksizyonu uygulandı. Önceden mevcut bir tümör olma olasılığı travma kaynaklı tümörden çok yüksek olmasına rağmen, sunulan olguda travmatik beyin lezyonu malign glial tümör gelişiminde predispozan bir faktör olabilir.
Introduction
Trauma has been implicated as a predisposing factor in patients with malignant gliomas [1–16]. However, only a few authors have provided definite evidence for a causative role of trauma in this disease [7, 15]. A proposed pathologic criteria for the diagnosis of a posttraumatic glioma includes traumatic brain injury, good status prior to the trauma, an identical location of the injury and tumor, adequate latent period, computed tomography (CT) or magnetic resonance imaging (MRI) soon after the trauma that show evidence of brain injury but no tumor and histopathological confirmation [13, 16, 17]. We present a patient in whom a glioblastoma multiforme developed 35 years after surgery for traumatic cerebral injury with no tumor found during surgery.
Case Report
A 65-year-old man was admitted to the emergency department because of right-sided hemiplegia, epilepsy and change in consciousness. Thirty-five years previously, the patient was operated on for a left frontotemporoparietal depression fracture and cerebral laceration due to a stone strike on his head. He experienced a speech disorder for 35 years as a result of the trauma. In addition, he had undergone coronary bypass surgery five years earlier. One year after the cardiac surgery, he was hospitalized for a cerebrovascular embolic attack that was diagnosed by MRI, and antiembolicantiepileptic drugs were given in the hospital. On examination, a fragmented wound scar and slightly depressed bones were observed over the left frontotemporoparietal region (Figure 1). His neurologic examination revealed a comatose state, epileptic contractions, bilateral papilledema, right-sided hemiplegia and cardiorespiratory disturbances. A non-contrast CT revealed a repaired depression fracture at the left temporoparietal junction, and a large hypointense mass lesion causing subfalcine herniation was detected under the depressed bones. A contrast-enhanced CT showed that the mass was localized at the left frontotemporoparital junction with evidence of extensive brain edema, left lateral ventricular compression and subfalcine herniation (Figure 2). Based on the imaging results, he underwent urgent surgery, and radical excision of the malignant glial tumor-like lesion was achieved. Defective duramater was repaired with temporal fascia. The excised materials were stained with immunohistochemical dyes including vimentine, P-53, Ki-67, GFAP (Figure 3) and S-100 (Figure 4). All results were strongly and diffusely positive for all immunohistochemical analyses. Cellular proliferation, mitosis and necrosis were observed, and the histopathological diagnosis was high-grade glioblastoma multiforme. Postoperative axial contrast CT showed no remaining mass lesion on post-operative day 6 (Figure 5). The patient healed without surgical complications and was discharged six days after the operation. He elected for whole-brain fractionated external radiation therapy and chemotherapy.
Figure 1.

The patient had been operated on for a posttraumatic left temporoparietal depression fracture and cerebral lesion 35 years earlier. Traumatic and surgical incision scars are shown in the left temporoparietal region.
Figure 2.
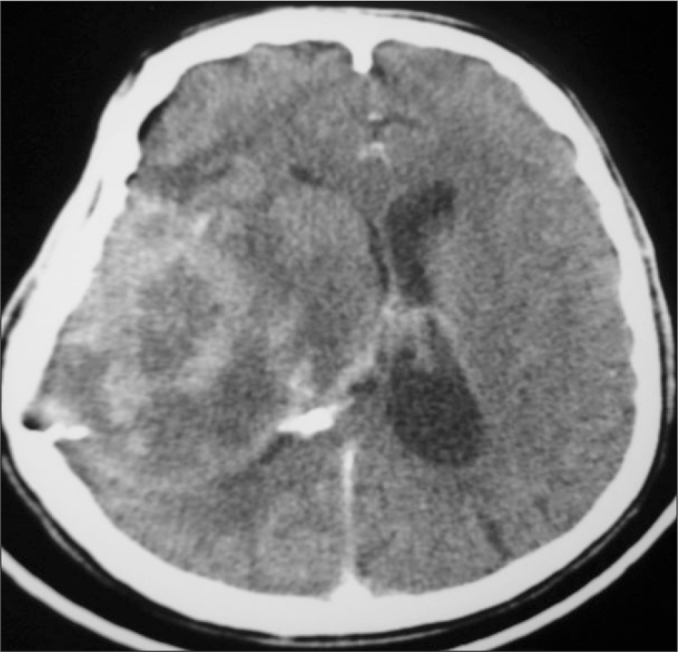
Axial contrast CT imaging revealed a contrast-enhancing mass lesion at the left lateral ventricular slit causing subfalcine herniation under the depressed temporal bone.
Figure 3.
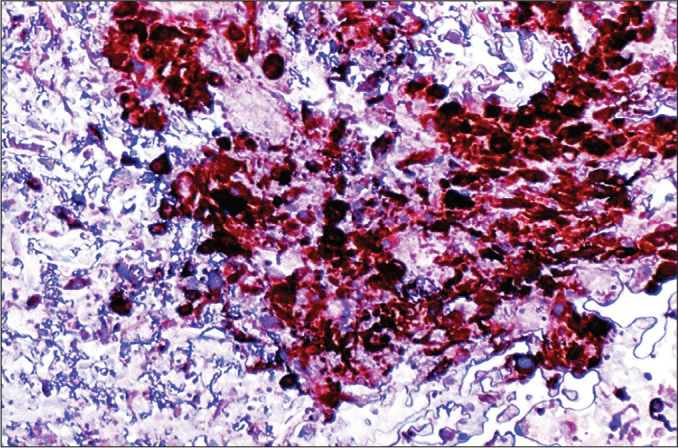
High-grade glioblastoma multiforme. Many of neoplastic cells show immunoreactivity to GFAP (GFAP, LM, ×100).
Figure 4.
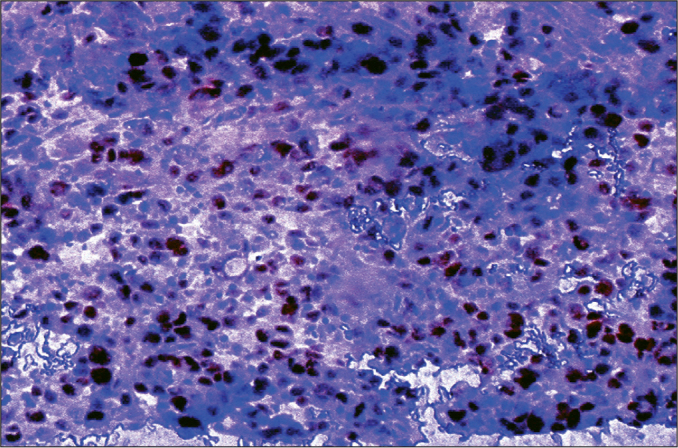
High-grade glioblastoma multiforme. Many of neoplastic cells show immunoreactivity to S-100 (S-100, LM, ×100).
Figure 5.
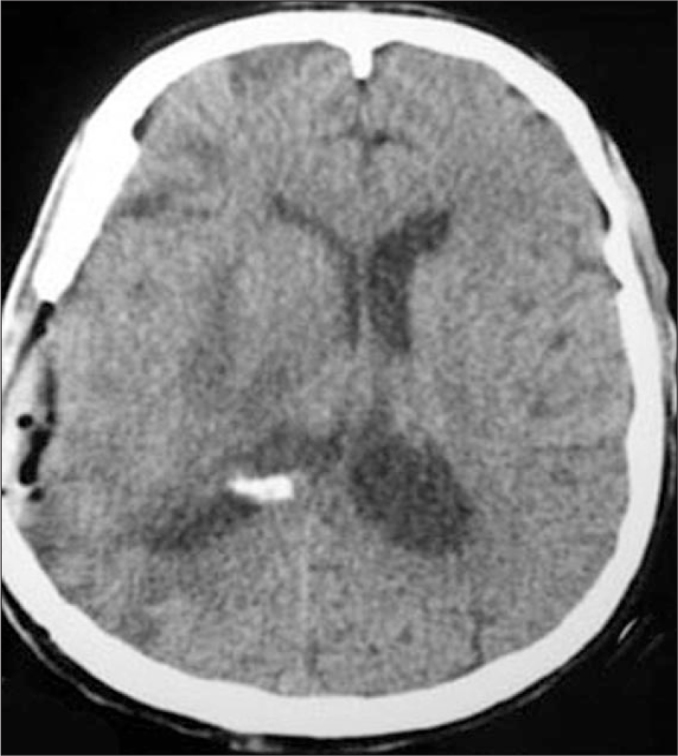
A postoperative axial contrast CT showed no mass lesion 6 days after the operation. The midline shift and left lateral ventricular compression had resolved.
Discussion
Trauma and glial scarring are known to be predisposing factors for the development of malignant glial tumors. The development of glioblastoma multiforme following a traumatic cerebral contusion is possible [18]. There are several case reports in the literature that discuss posttraumatic gliomas [1–12], but some of these cases might only be a statistical coincidence. Hochberg et al. [10] demonstrated that severe head injury is a significant risk factor for the development of glial tumors. Most other authors have not demonstrated a significant association between head trauma and gliomas [2, 19, 20]. In most of these cases, the histopathological diagnosis was a continuation of the gliotic scar of the tumor [3–6, 8, 13, 14, 21], and persisting splinters were found in the glioma nidus many years after penetrating injury (15). Posttraumatic gliomas have been described, but in none of these prior reports has there been documented absence of a tumor at the time of the injury. A posttraumatic malignant glioma with radiological evidence of only a contusion prior to the development of the tumor was reported by Henry et al. [7].
Although epidemiologic studies may not be conclusive, a pathologic basis for development of posttraumatic gliomas has been suggested. Morantz et al. [22] demonstrated that posttraumatic gliosis potentiates the formation of brain tumors in rats. Ludwin [19] demonstrated evidence of mitoses among astrocytes, microglia and oligodendrocytes 24 hours after trauma in mice. Trauma initiates glial cell proliferation by triggering various growth factors that result in malignant neoplasms. Schiffer et al. [23] detected astrocytic proliferation on the ipsilateral injury side in the rat brain two days after trauma, and astrocytic proliferation was demonstrated in regions of fluid percussion injury and deteriorated blood-brain barrier regions [9]. Kernie et al. [12] demonstrated significant astrocyte and neural precursor proliferation in response to traumatic brain injury regions at 60 days after trauma, and Propiono bacterium acnes was isolated within the posttraumatic glioma tissue [15]. Glioblastoma multiforme has also reported at the site of metal splinter injury [15] and gunshot injuries complicated with infectious processes may be responsible for the development of posttraumatic GBM after many years [24]. Glioblastoma multiforme may also develop after neurosurgical operations due to the collection of myelin basic protein in the brain [25].
Zulch et al. [16] presented criteria for the diagnosis of a traumatic etiology for a brain tumor. The patient must have been in good health before the accident. The head injury must have been the cause of brain damage. The site of the trauma and the tumor must be related to each other. The latent period between the brain damage and the development of the tumor must not be less than 1 year. Manuelidis [13] has stated that bleeding, edema and scars should be distinguished from traumatic injury. A contrast CT/MR done soon after resolution of the traumatic contusion should not reveal a mass lesion. Otherwise, the possibility of a pre-existing tumor rather than a trauma-induced tumor is very high. A glioma diagnosis should also be confirmed by immunohistochemical tests, such as GFAB, KI-67, P53, S-100 and vimentin positivity [17].
The presented patient lived in good health with only a sensory motor aphasia for 35 years after a traumatic brain laceration due to a left temporal depression fracture. If there were a brain tumor at the site and time of the trauma, he would not have been asymptomatic for 35 years, and the former diagnosis of a cerebrovascular ischemic attack would not have been true. We think that the development of glioblastoma multiforme in our patient originated from a cerebral laceration.
In conclusion, posttraumatic glioblastoma multiforme has rarely been described in the literature, but its occurrence is possible, because trauma can trigger astrocytic proliferation. In our opinion, unknown or forgotten traumatic injuries may be a predisposing factor for GBM.
Footnotes
Conflict of interest statement: The authors declare that they have no conflict of interest to the publication of this article.
References
- 1.Annegers JF, Laws ER, Jr, Kurland LT. Head trauma and subsequent brain tumours. Neurosurgery. 1976;4:203–6. doi: 10.1227/00006123-197903000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Bohnen NI, Kurland LT. Epidemiology of brain tumours. Neuro- Glioblastoma Multiforme Following Cerebral Contusion. In: Vecht CJ, Vinken PJ, Bruyn GW, editors. Surg Neurol. Vol. 61. 2004. pp. 180–2. [DOI] [PubMed] [Google Scholar]
- 3.Di Trapani G, Carnevale A, Scerrati M, Colosino C, Vaccario ML, Mei D. Post traumatic malignant glioma. Report of a case. Ital J Neurol Sci. 1996;17:283–6. doi: 10.1007/BF01997787. [DOI] [PubMed] [Google Scholar]
- 4.Diezel P. Gliom nach trauma. Frankfurt Z Path. 1949;60:316–26. [PubMed] [Google Scholar]
- 5.Hallervorden J. Oligodendroglion nach hirntrauma. Nervenartz. 1948;19:163–7. [PubMed] [Google Scholar]
- 6.Henderson RD, Campbell SF. Head trauma and brain tumours revisited. J Clin Neurosci. 2000;7:262–4. doi: 10.1054/jocn.1999.0204. [DOI] [PubMed] [Google Scholar]
- 7.Henry PT, Rajshekhar V. Post-traumatic malignant glioma: case report and review of literature. Br J Neurosurg. 2000;14:64–7. doi: 10.1080/02688690042979. [DOI] [PubMed] [Google Scholar]
- 8.Heyck H. Glioblastom nach leukotomie. Monats schr Psychiat Neurol. 1954;128:180–8. doi: 10.1159/000139784. [DOI] [PubMed] [Google Scholar]
- 9.Hill-Felberg SJ, McIntosh TK, Oliver DL, Raghupathi R, Barbarese E. Concurrent loss and proliferation of astrocytes following lateral fluid percussion brain injury in the adult rat. J Neurosci Res. 1999;57:271–9. doi: 10.1002/(SICI)1097-4547(19990715)57:2<271::AID-JNR13>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 10.Hochberg F, Toniolo P, Cole P. Head trauma and seizures as risk factors of glioblastoma. Neurology. 1984;34:1511–4. doi: 10.1212/wnl.34.11.1511. [DOI] [PubMed] [Google Scholar]
- 11.Janda J, Mracek Z. Post traumatic astrocytoma. Zentralbl Allg Pathol. 1987;133:55–9. [PubMed] [Google Scholar]
- 12.Kernie SG, Erwin TM, Parada LF. Brain remodeling due to neuronal and astrocytic proliferation after controlled cortical injury in mice. J Neuroci Res. 2001;66:317–26. doi: 10.1002/jnr.10013. [DOI] [PubMed] [Google Scholar]
- 13.Manuelidis EE. Glioma in trauma. In: Minckler J, editor. Pathology of the Nervous System. Vol. 2. New York: McGraw-Hill; 1978. pp. 2237–40. [Google Scholar]
- 14.Perez-Diaz C, Cabello A, Lobato RD, Rivas JJ, Cabrera A. Oligodendrogliomas arising in the scar of a brain contusion. Surg Neurol. 1985;24:581–6. doi: 10.1016/0090-3019(85)90278-2. [DOI] [PubMed] [Google Scholar]
- 15.Sabel M, Felsberg J, Messing-Junger M, Neuen-Jacob E, Piek J. Glioblastoma multiforme at the site of metal splinter injury: a coincidence? Case report. J Neurosurg. 1999;91:1041–4. doi: 10.3171/jns.1999.91.6.1041. [DOI] [PubMed] [Google Scholar]
- 16.Zulch KJ, Meinel HD. The biology of brain tumours. In: Vinkin PJ, Bruyn GW, editors. Tumours of the Brain and Skull Part I. Handbook of Clinical Neurology. Vol. 16. Amsterdam, North Holland: 1974. pp. 1–56. [Google Scholar]
- 17.Candolfi M, Curtin JF, Nichols WS, Muhammad AG, King GD, Pluhar GE, et al. Intracranial glioblastoma models in preclinical neuro-oncology: Neuropathological characterization and tumor progression. J Neurooncol. 2007;85:133–48. doi: 10.1007/s11060-007-9400-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Messimy R, Pecker J. Posttraumatic glioma; difficulties of the problem. Rev Neurol. 1953;89:620–1. [PubMed] [Google Scholar]
- 19.Nygren C, Adami J, Ye W. Primary brain tumours following traumatic brain injury: a population basedcohort study in Sweden. Cancer Causes Control. 2001:733–7. doi: 10.1023/a:1011227617256. [DOI] [PubMed] [Google Scholar]
- 20.Wrench M, Miike R, Lee M, Neuhaus J. Are prior head injuries or diagnostic X-rays associated with gliom in adults? The effects of control selective bias. Neuroepidemiology. 2000;19:234–44. doi: 10.1159/000026261. [DOI] [PubMed] [Google Scholar]
- 21.Finkemeyer H, Behrend RC. Hirntrauma and gliomentstehung. Zentrabl Neurochir. 1956;16:318–20. [PubMed] [Google Scholar]
- 22.Morantz RA, Shain W. Trauma and brain tumours: an experimental study. Neurosurgery. 1978;3:181–6. doi: 10.1227/00006123-197809000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Schiffer D, Giordana MT, Cvalla P, Vigliani MC, Attanasio A. Immunohistochemistry of glial reaction after injury in the rat: double staining and markers of cell proliferation. Int J Dev Neurosci. 1993;11:269–80. doi: 10.1016/0736-5748(93)90085-r. [DOI] [PubMed] [Google Scholar]
- 24.Witzmann A, Jellinger K, Weiss R. Glioblastoma multiforme developing after a gunshot injury of the brain. Neurochirurgia. 1981;24:202–6. doi: 10.1055/s-2008-1054068. [DOI] [PubMed] [Google Scholar]
- 25.Alling C, Karlsson B, Vällfors B. Increase in myelin basic protein in CSF after brain surgery. J Neurol. 1980;223:225–30. doi: 10.1007/BF00313336. [DOI] [PubMed] [Google Scholar]


