Abstract
Objective:
The aim of this study is to present our clinical experience with rhomboid flaps.
Materials and Methods:
Twenty-four patients who were operated on between January 2006 and October 2010 were included in the study. All defects were reconstructed using rhomboid flaps.
Results:
Twenty-four patients were operated on for various reasons, and 26 rhomboid flaps were performed. Eleven of the 24 cases were male, and the median age of participants was 47.5 years. Eight cases were operated on under general anesthesia, and 13 were locally anesthetized; the remaining cases were operated on under regional anesthesia. In 17 cases, the defect was due to a benign or malignant tumor excision, and five cases were operated on due to burn contracture. There were no occurrences of partial or total flap necrosis or hematoma in our series.
Conclusion:
Our series indicates that rhomboid flaps can be safely used to reconstruct small to moderately sized skin defects.
Keywords: Dufourmentel flap, Limberg flap, Rhomboid flap
Özet
Amaç:
Çalışmanın amacı rhomboid fleplerle elde ettiğimiz deneyimlerin sunulmasıdır.
Gereç ve Yöntem:
Ocak 2006 ve Ekim 2010 arasında opere edilen 24 hasta çalışmaya dahil edildi. Tüm defektler rhomboid fleple rekonstrükte edilmişti.
Bulgular:
Çeşitli nedenlerle opera edilen hastalarda 26 romboid flep uygulandı. 24 hastanın 11’I erkekti. Medyan yaş 47.5 idi. 8 hastada genel, 13 hastada lokal anestezi kullanılırken diğer hastalara bölgesel anestezi verilmişti. 17 hastada benign ya da malign tumor eksizyonu nedeniyle rekonstrüksiyon yapıldı. 5 olgu yanık kontraktürüne bağlı opera edilmişti. Seride kısmi ya da tam flep nekrozu ve hematom görülmedi.
Sonuç:
Serimizden elde edilen sonuçlar, orta veya küçük boy cilt defektlerin rekonstrüksiyonunda romboid fleplerin güvenle kullanılabileceğini göstermektedir.
Introduction
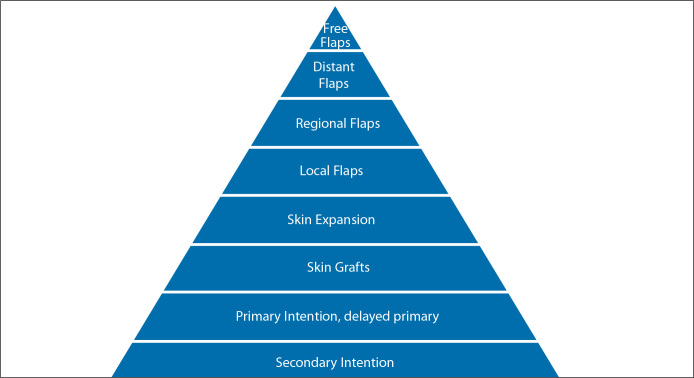
The concept of the “reconstructive ladder” suggests that primary closure of a defect is the first choice in reconstruction [1] (Figure 1). However, a considerable number of cases are not eligible for primary closure. In these circumstances, local flaps become the second option. Although defect size is a limiting factor, texture, pliability and color match of a local flap favor its use [2]. Of local flaps, a rhomboid flap is a prominent flap that can be used to reconstruct defects in any part on the body.
Figure 1.
Reconstructive ladder, procedures ranging from simplest to complex.
Alexander Alexandrovich Limberg was an outstanding surgeon who greatly contributed to the modern practice of plastic surgery. He defined the rhomboid flap and presented his studies in English in 1963 [3]. A rhomboid flap has equal edges with opposing angles of 120° and 60° (Figure 2A). Any defect that can be projected in a rhomboidal shape can be reconstructed with a Limberg flap. Four individual flap choices are theoretically possible for any defect. However, the surgeon must choose the most suitable one. Skin laxity in the donor area determines the preferred flap (Figure 2A).
Figure 2.
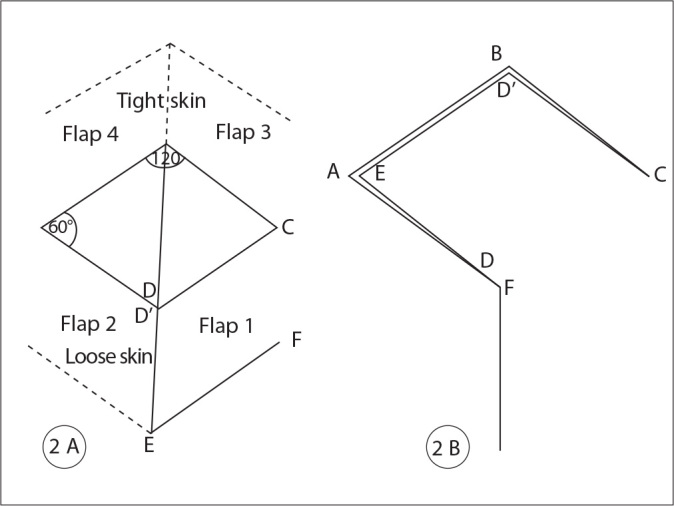
A) Limberg flap design. For any defect there are 4 possible flaps. B) Point A corresponds to E, B corresponds to D’, D corresponds to F.
In 1962, Claude Dufourmentel [4] modified the rhomboid flap. In his design, the distal border of the flap is placed on the line that bisects the angle between the short diagonal of the rhomboid defect and its adjacent side; the acute angle of the flap is still 60°. This modification widens the pedicle width and increases the safety of the flap (Figure 3). Webster [5] described another modification that combined a 30° transposition flap with an M-plasty to repair rhomboidal defects.
Figure 3.
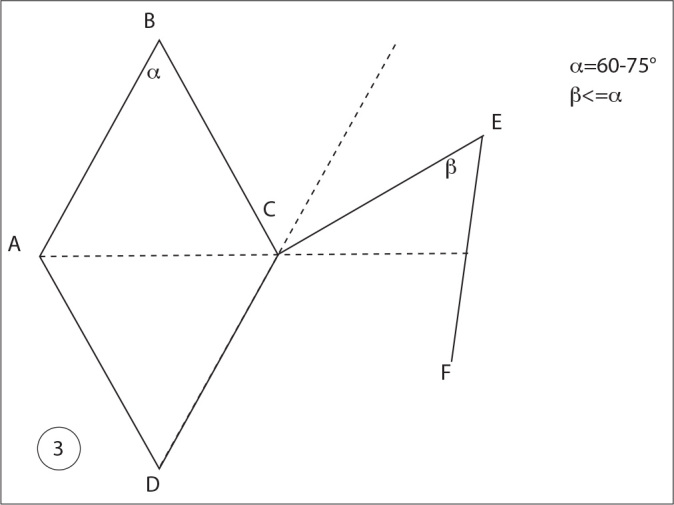
Dufourmentel flap design. Note alpha angle ranges between 60–75°.
Rhomboid flaps can be used anywhere, without any limitations that are due to defect etiology, age or other patient factors. Tumor resection is the primary etiologic factor for this flap, and its use for skin cancers is most often in the head and neck regions. In addition, there have been efforts to use this flap in hand reconstruction, breast reconstruction and pilonidal sinus resection and reconstruction.
We have been using Limberg flaps in our daily plastic surgery practice for the reconstruction of any defect. In this paper, we review operations that we have performed during the past 4 years.
Materials and Methods
Patients with skin defects that were closed with rhomboid flaps between January 2006 and October 2010 were included in this study. There were no limitations in regards to etiology, location, size, age, sex or any other patient factors.
Operative Technique
Regardless of the defect’s size, location or etiology, the defect was prepared as follows. A diagonal line bisecting the 120° angle was elongated outside the defect on neighboring tissue with the same length as the diagonal. Next, on the basis of skin laxity around the defect, we chose a donor area that could be closed primarily without tension and would result in a scar parallel to skin tension lines. Then, a line parallel to the defect side was drawn that was as long as the length of the defect (Figure 2A).
After planning, the flap was elevated and transposed over the defect. The points D’, E and F of the flap corresponded to the points B, A and D of the defect, respectively (Figure 2B). After hemostasis was achieved, a penrose drain was placed under the flap and the donor area. According to the defect’s location and size, the subcutaneous tissues and skin were sutured using appropriately sized suture thread.
Results
There were 24 patients who underwent surgical procedures for various reasons, for a total of 26 elevated rhomboid flaps. Eleven of the 24 cases were male and the median patient age was 47.5 years (Table 1).
Table 1.
Summary of the cases
| Case no | Age/Sex | Site | Flap size | Etiology | Anesthesia | Complication |
|---|---|---|---|---|---|---|
| 1 | 13/M | Finger | 2×1.5 | Burn Contracture | GA | None |
| 2 | 9/M | Axilla | 10×14 | Burn Contracture | GA | None |
| 3 | 57/M | Nose | 2×2 | BCC | LA | None |
| 4 | 16/F | Neck | 12×10 | Burn Contracture | GA | None |
| 5 | 10/F | Hand | 5×3 | Burn Contracture | GA | None |
| 6 | 50/M | Nose | 2×1 | BCC | LA | None |
| 7 | 33/F | Cheek | 5×8 | Melanoma | LA | None |
| 8 | 57/F | Temple | 3×5 | BCC | LA | None |
| 9 | 42/F | Arm | 8×9 | Burn Contracture | RA | None |
| 10 | 60/F | Cheek | 5×3 | BCC | LA | None |
| 11 | 43/M | Cheek | BCC | LA | None | |
| 12 | 45/F | Bilateral Temporal | 3×2,3×3 | BCC | LA | None |
| 13 | 63/M | Temporal | 3×2 | BCC | LA | None |
| 14 | 83/F | Cheek | 7×9 | Melanoma | GA | None |
| 15 | 74/M | Cheek | 2×3 | BCC | LA | None |
| 16 | 8/F | Medial Cantus | 3×2 | Nevus | GA | None |
| 17 | 43/M | Temple | 3×2 | BCC (Double opposing flaps) | LA | None |
| 18 | 61/F | Cheek | 6×5 | Melanoma | GA | None |
| 19 | 72/F | Cheek | 7×5 | Melanoma | LA | None |
| 20 | 76/F | Nose | 3×2 | SCC | LA | None |
| 21 | 53/M | Thigh | 10×13 | SCC | RA | None |
| 22 | 67/M | Knee Stump | 12×14 | Buerger Disease | RA | Suture separation |
| 23 | 28/M | Achilles | 3×2 | Fibroma | LA | None |
| 24 | 45/F | Cheek | 8×12 | Gun Shot Injury | GA | None |
Eight cases were operated on under general anesthesia while 13 were locally anesthetized. The other operations were performed under regional anesthesia. In 17 cases, the defect was due to a benign or malignant tumor excision, and five cases were operated on due to burn contractures. Seventeen cases were performed in the head and neck regions, but the flap can also be used in the torso, lower extremity and upper extremity.
The largest flap was 12×14 cm and was used to correct a defect over the stump of a patient with Buerger disease who underwent amputation below the knee. The only complication reported in our study, which was a suture separation, occurred in this patient. There were no events of partial or total flap necrosis or hematomas.
Cases
Case 8
A 57-year-old female patient was operated on because of a BCC on her left temple region. The donor area was on her cheek (Figure 4A and B).
Figure 4.

A) BCC on left temple. Rhomboid flap designed. B) BCC excised and flap transposed from cheek.
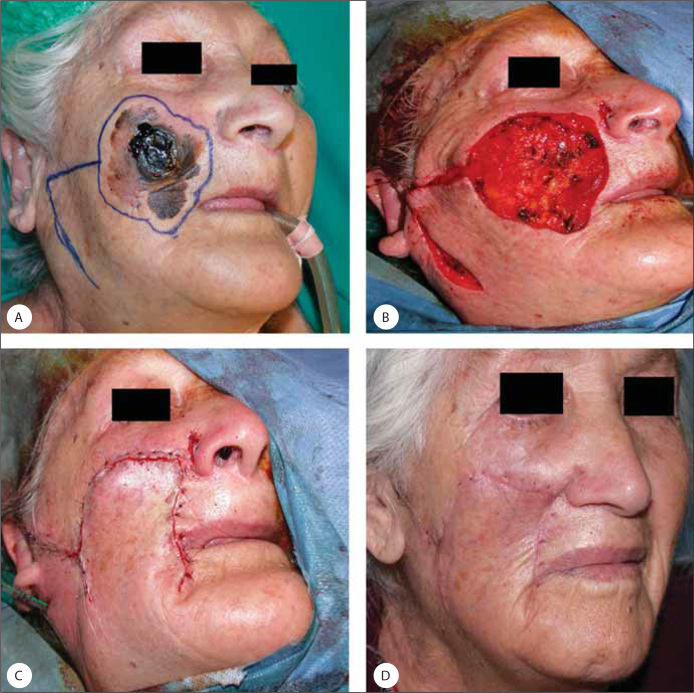
Case 14
An 83-year-old female patient was operated on because of a malignant melanoma on her left cheek. The donor area was on her cheek (Figure 5A, B, C and D).
Figure 5.
A) Malignant melanoma of the right cheek. Flap designed. B) Tumor excised and flap elevated. C) Flap transposed and sutured. D) Six months after the operation.
Case 16
An eight-year-old female patient was operated on because of a congenital nevus over her medial canthal region. The donor area was the glabella (Figure 6A, B, and C).
Figure 6.

A) Medial canthal defect after nevus excision. Flap designed from the glabella. B) Flap transposed and sutured. C) Six months after the operation.
Case 17
A 43-year-old male patient was operated on because of a BCC over his left temple. The defect was closed with double opposing rhomboid flaps (Figure 7A, B and C).
Figure 7.

A) BCC on the left temple. Double flap designed. B) Flaps transposed and sutured. C) Eighteen months after operation.
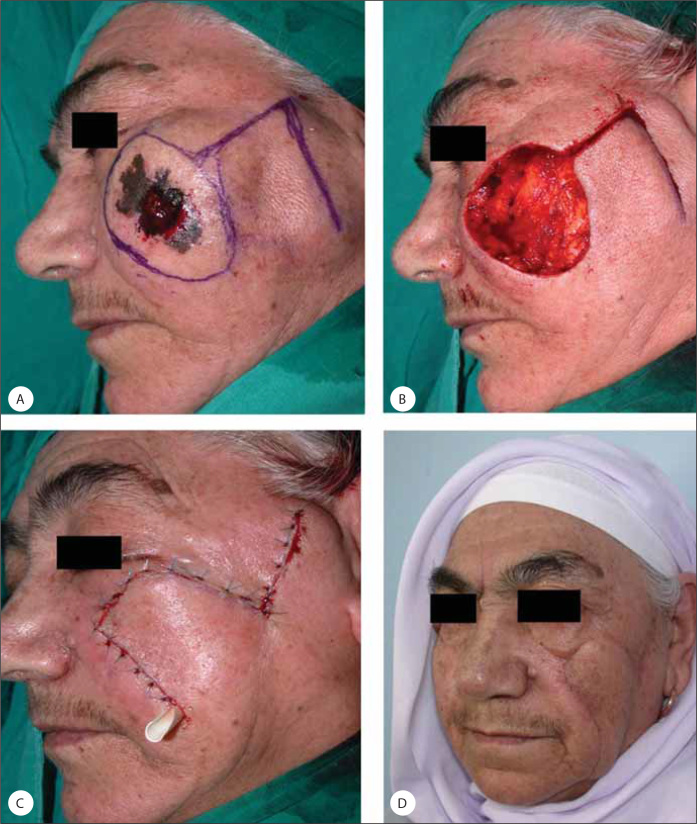
Case 19
A 72-year-old female patient was operated on because of a malignant melanoma on her cheek. The donor area was on her cheek (Figure 8A, B, C and D).
Figure 8.
A) Malignant melanoma of the left cheek. Flap designed. B) Tumor excised and flap elevated. C) Flap transposed and sutured. D) Six months after operation.
Case 21
A 53-year-old male patient was operated on because of an SCC on his distal thigh. The defect was closed with a laterally based rhomboid flap from the thigh (Figure 9A and B).
Figure 9.
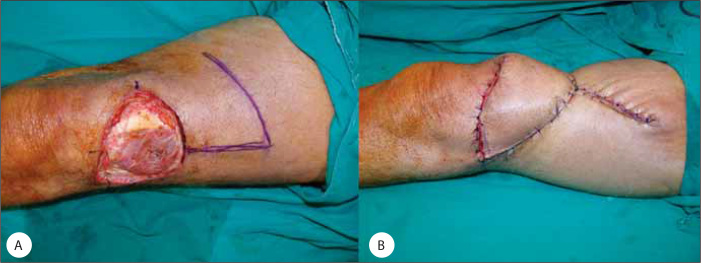
A) Defect on the distal thigh. B) Flap transposed and sutured.
Discussion
The “reconstructive ladder” emphasizes using the simplest procedure to manage skin defects (Figure 1). Most of the time, direct closure of a defect is easily achieved. However, as a defect increases in size, it is harder to close primarily. In such situations, clinical experience suggests a slightly different perspective. Technical ease, aesthetic concerns, continuity of function and follow-up duration direct surgeons toward the use local flaps, thereby bypassing grafts and tissue expansion steps as suggested by the “reconstructive ladder.” Local flaps are distinguished from other techniques by their short operation time, early functionality and fewer out-patient clinic visits. Skin texture and color are also reasons that local flaps are favored.
Transposition flaps planned using rhomboid flap principles have been widely used in clinical practice by plastic surgeons. They are easy to learn and simple to perform. They can be used at any site on the body surface. Modifications by Dufourmentel and Webster have also increased their popularity by increasing the safety and angular ranges of these flaps.
Aesthetics are especially important, even after ablative cancer surgery. Defect closure by primary intention and grafts may offer satisfactory outcomes for some locations. However, a well-planned rhomboid flap with scars parallel to tension lines provides the best results. Naturally, the skin texture and color adjacent to the defect best matches the surrounding skin.
Skin grafts may appear to be the simplest way to reconstruct a defect. However, they are limited by the need to immobilize the graft for at least five days, the need for restrictions in diet, the necessity of greater care with personal hygiene, the prevention of everyday physical activities, and delays in patient functionality. The duration of such issues is much shorter for patients with local flaps.
Skin grafts need more dressing changes than do any other procedure. After five days of tie-over dressings, dressing changes every two days for about ten days is a standard protocol. In contrast, local flaps do not require many dressing changes.
The safety of rhomboid flaps has attracted surgeons to its use for several different purposes. Rhomboid flaps have been used to reconstruct defects after pilonidal sinus resection [6], antecubital burn contractures [7] and breast reconstruction [8].
The modification of rhomboid flaps that is used depends on the individual characteristics of the case and a surgeon’s experience. Our series indicates that rhomboid flaps can be safely used to reconstruct small to moderately sized skin defects.
Footnotes
Conflict of interest statement: The authors declare that they have no conflict of interest to the publication of this article.
References
- 1.Charles H. Thorne, Techniques And Principles In Plastic Surgery. In: Thorne Charles H, Bartlett Scott P, Beasley Robert W, Aston Sherrell J, Gurtner Geoffrey C, Spear Scott L., editors. Grabb and Smith’s Plastic Surgery. 6th Edition. Lippincott Williams & Wilkins; Philadelphia: 2007. pp. 3–14. [Google Scholar]
- 2.Fee WE, Jr, Gunter JP, Carder HM. Rhomboid flap principles and common variations. Laryngoscope. 1976;86:1706–11. doi: 10.1288/00005537-197611000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Limberg AA. Modern trends in plastic surgery. Design of local flaps. Mod Trends Plast Surg. 1966;2:38–61. [PubMed] [Google Scholar]
- 4.Dufourmentel C. Transact Third Int Congr Plast Surg. Amsterdam: Excerpta Medica; 1964. An L-shaped flap for lozengeshaped defects: Principle - technique - applications; pp. 772–3. [Google Scholar]
- 5.Webster RC, Davidson TM, Smith RC. The thirty degree transposition flap. Laryngoscope. 1978;88:85–94. doi: 10.1002/lary.1978.88.1.85. [DOI] [PubMed] [Google Scholar]
- 6.Akin M, Leventoglu S, Mentes BB, Bostanci H, Gokbayir H, Kilic K, et al. Comparison of the classic Limberg flap and modified Limberg flap in the treatment of pilonidal sinus disease: a retrospective analysis of 416 patients. Surg Today. 2010;40:757–62. doi: 10.1007/s00595-008-4098-7. [DOI] [PubMed] [Google Scholar]
- 7.Gümüş N. A new approach to the antecubital scar contracture: rhomboid rotation flap. J Plast Reconstr Aesthet Surg. 2010;63:1392–3. doi: 10.1016/j.bjps.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 8.Gwynn BR, Williams CR. Use of the Limberg flap to close breast wounds after partial mastectomy. Ann R Coll Surg Engl. 1985;67:245–6. [PMC free article] [PubMed] [Google Scholar]