Abstract
Female adnexial tumors of probable Wolffian origin (FATWO) are rare tumors derived from the remnants of the mesonephric duct. These tumors generally exhibit a low malignant potential, but recurrence and or metastasis is possible during the course of the disease according to the tumors’ possible malignant potential. We report a case of FATWO without estrogen and progesterone receptors and with negative immunostaining for Ki-67 (a proliferation marker) as a probable low-malignant-potential tumor. A 55-year-old woman presented with a complaint of heavy menstrual bleeding and pelvic pain. Pre-operative ultrasonographic evaluation revealed an intramural uterine leiomyoma of 4 cm in diameter and a right adnexial solid mass measuring 5 cm in diameter. Following total abdominal hysterectomy and bilateral salpingo-oophorectomy, immunostaining based on the labeled streptavidin-biotin method was performed on sections from representative blocks of paraffin-embedded tissues sampled from the mass, revealing a low mitotic index with negative Ki-67 immunostaining. Immunohistochemical staining with promising new markers and pathological investigation of the entire tumor are needed to determine the malignant behavior of an individual FATWO. Ki-67 is a helpful marker for determining Wolffian duct tumors’ potential malignant behavior.
Keywords: FATWO, Immunostaining, Ki-67, Low malignant potential, Rare
Özet
Muhtemelen Wolff kaynaklı dişi adneksial tümörleri (FATWO) mezonefrik kanal artıklarından kaynaklanan nadir tümörlerdir. Bu tümörler genellikle düşük malign potansiyel gösterirler fakat olası malign davranışa göre rekürrensler ve/veya metazstaz da hastalığın gidişatı esnasında mümkümdür. Östrojen ve progesteron reseptörleri olmayan ve bu tip tümörler için düşük malign potansiyel özelliği olan Ki-67 proliferasyon işaretçisinin immün boyamada negatif olduğu bir FATWO olgusu sunuyoruz. Elli beş yaşında bir kadın ağır menstrüel kanama ve pelvik ağrı şikayeti ile başvurdu. Preoperatif ultrasonografik değerlendirme 4 cm uterin intramural myom ve sağ adnekste 5 cm çaplı solid bir kitleyi gösterdi. Total abdominal histerektomi ve bilateral salpingooforektomiyi takiben kitleden alınan doku örneklerinden hazırlanan parafin iliştirilmiş temsili bloklardan kesitler alınarak işaretli streptavidin- biotin metodu bazlı immün boyama yapıldı ve Ki-67 ile immün boyanma göstermeyen düşük mitotik indekse sahip olduğu gösterildi. Hastanın fertilite isteğine bağlı olarak total abdominal histerektomi ve bilateral salpingooforektomi ile birlikte yapılan cerrahi debulking en uygun ilk cerrahi işlemdir. Bir FATWO hastasının malign davranışına karar vermeden önce yeni ümit verici işaretçilerle immünhistokimyasal boyanması ve tüm tümörün patolojik incelemesi gereklidir. Ki-67 Wolff kanalı tümörünün potansiyel malign davranışını tespit etmede yardımcı bir işaretçidir.
Introduction
Female adnexal tumors of probable Wolffian origin (FATWO) are rare tumors derived from the remnants of the mesonephric duct. Kariminejad and Scully have reported nine cases and classified this type of tumor as FATWO based on its location, where the remnants of the Wolffian duct remain congenitally [1]. These tumors generally exhibit a low malignant potential, but recurrence and/or metastasis is possible during the course of the disease according to the tumors’ possible malignant behavior [2]. The majority of these tumors have presented in the broad ligament with close proximity to the fallopian tube, paravaginal region and hilum ovarii [3]. The male genital tract and retroperitoneal space are other possible sites for this tumor [4]. Approximately 71 cases of FATWO have been reported, and the majority of them have been considered to have a benign course with indolent behavior. Only nine cases with evidence of recurrence and/or metastasis have been reported in the English-language literature. Microscopically, FATWO are well-differentiated epithelial tumors growing in a tubular, sieve-like, diffuse architecture containing eosinophilic secretions. The rarity of this type of tumor impedes the execution of prospective controlled treatment studies. Our current limited knowledge is based on case series, which is not sufficient to define effective treatment modalities. We report a case of FATWO without estrogen and progesterone receptors and with negative immunostaining for the proliferation marker Ki-67. These features indicate the low-malignant-potential properties of FATWO.
Case Report
A 55-year-old woman presented in the outpatient clinic with a complaint of heavy menstrual bleeding and pelvic pain. Pelvic examination revealed right pelvic tenderness with a deep palpation. Preoperative ultrasonographic evaluation exhibited an intramural uterine leiomyoma of 4 cm in diameter and a right adnexal solid mass of 5 cm in diameter. At laparotomy, except from the right adnexal mass in the broad ligament, other pelvic organs appeared normal. A total abdominal hysterectomy and bilateral salpingo-oophorectomy were performed to determine the definitive treatment. The patient was discharged on the 5th postoperative day after an uneventful follow-up period. She was told to see her physician at least 2 times yearly. Further therapy has not been required to date.
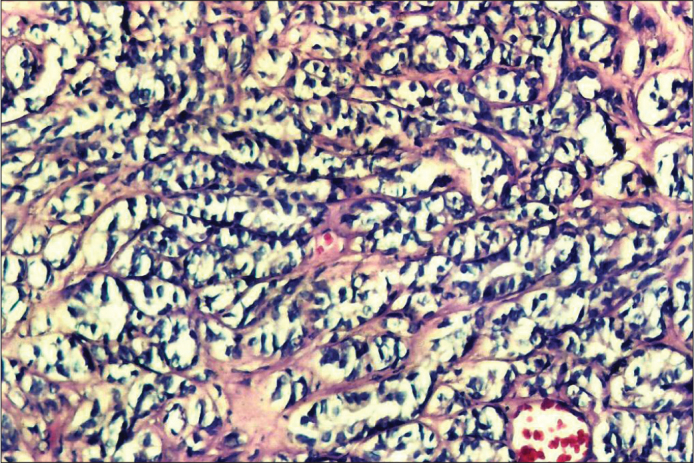
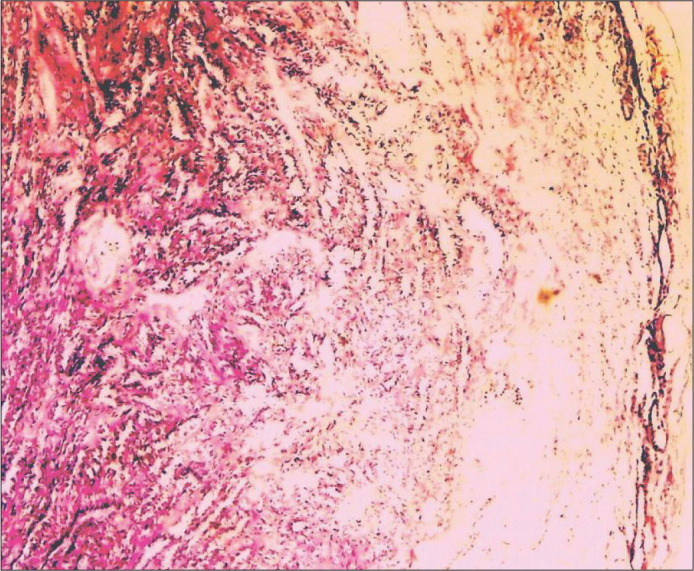
The anatomic study of the mass showed a fairly encapsulated tumoral mass measuring 3×4×5 cm. Macroscopically, this mass was entirely solid and contained calcified areas. The pathological examination of the right adnexal mass revealed a Sertoli-Leydig cell tumor before immunohistochemical staining for the distinct diagnosis. Both ovaries were tumor-free, and the entirety of this mass was located in the right broad ligament. The formalin-fixed, paraffin-embedded tissues were evaluated microscopically after hematoxylin and eosin (H&E) staining. A low mitotic index without cellular pleomorphism was seen in all tissue sections (Figures 1–3). Immunostaining based on the labeled streptavidin-biotin method (LSAB kit, Dako, Carpinteria, CA) was performed on sections from representative blocks of the paraffin-embedded tissues sampled from the mass. The results of immunohistochemical staining of the tumoral tissue for vimentin, keratin, Epithelial Membrane Antigen (EMA), inhibin, estrogen receptor, progesterone receptor and Ki-67 are detailed in Table 1.
Figure 1.
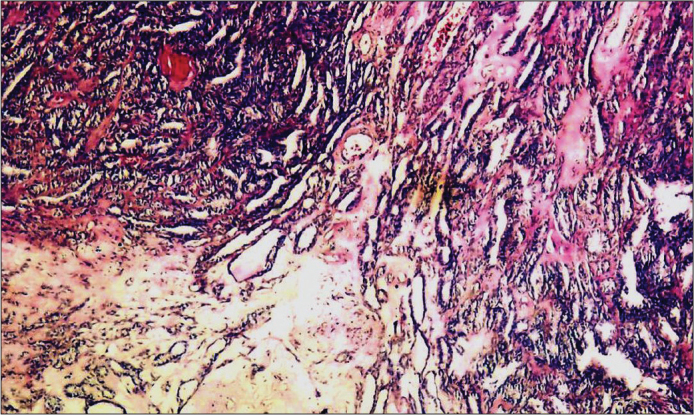
Cystic structures and tumoral cells forming tubal shapes (HE×40).
Figure 3.
Basal layer of tumoral cells forming tubular like structures in fibrous tissue staining PAS positive (HE×20).
Table 1.
The antibodies used for immunohistochemical study
| Antibodies (clone) | Source | Antigen retrieval | Primary antibody incubation | Positive external control |
|---|---|---|---|---|
| CK 20 (Ks20.8) | DAKO, Carpinteria, CA | Mw | Overnight | Colon |
| Vimentin (V9) | DAKO, Carpinteria, CA | Mw | Overnight | Connective tissue |
| EMA (δ29) | DAKO, Carpinteria, CA | Mw | Overnight | Breast |
| α-inhibin (R1) | Novocastra, Newcastle, UK | Mw | Overnight | Sex cord-stromal tumor |
| ER (1D5) | Novocastra, Newcastle, UK | Mw | Overnight | Breast |
| PR (1A6) | DAKO, Carpinteria, CA | Mw | Overnight | Breast |
| Ki- 67 (MIB1) | Biogenex | Mw | Overnight adenocarcinoma | Colon |
Mw: microwave in pH 6.0, 10 mmol citric acid buffer for 10 minutes, CK: cytokeratin, EMA: epithelial membrane antigen, ER: estrogen receptor, PR: progesterone receptor
Discussion
The mesonephric ducts and tubules form a primitive urinary system in the embryo at the 4th week of embryonic life. The reproductive system cooperates with the mesonephric (Wolffian) duct in the male, while in the female, these structures degenerate and remain remnants, such as Morgagni and Gardner cysts, in adulthood [5, 6].
Macroscopically, the size of FATWO varies widely, ranging from 0.8 to 25 cm in diameter. These tumors’ main feature is a solid, lobulated, and nodular shape. Hemisections of these tumors show a pale yellow or gray, smooth, glistening surface with a faint-bordered outer layer. Focal hemorrhage can also result cystic necrosis in these mostly solid tumors. Microscopically, the tumors’ main visual feature is well-differentiated epithelial cells forming tubular, sieve-like, diffuse patterns of growth. The tumors’ location (where the Wolffian remnants remain), their lack of resemblance to Mullerian-originated neoplasms and the ovarian surface epithelium are the discriminative features of FATWO that support Wolffian origin [7, 8].
Immunohistochemical evidence for Wolffian remnants, such as immunoreactivity to pan-cytokeratin (AE1/3, CK1), CAM 5.2, cytokeratin 7 (CK7) and vimentin, make the diagnosis of FATWO more accurate [2, 9].
The age range of patients with these rare tumors is also wide (15–83 years). The presence of FATWO types exhibiting malignant potential in both young and old patients increases the need for defining more accurate diagnostic criteria to identify malignant Wolffian duct tumors. The presence of necrosis, capsular invasion, a high number of mitoses, cellular pleomorphism, and immunohistochemical positivity for CD117 and, probably, Ki-67 are the currently known properties of FATWO with malignant potential [10]. Recurrence or initial malignant behavior can occur in the absence of these negative prognostic factors.
In our patient, the tumor was located in the right broad ligament and was firmly encapsulated with a pathological appearance of predominantly tubular architecture, supporting the Wolffian origin of the tumor. Dissection of the tumor was easy, and it was exteriorized together with the hysterectomy specimen. The immunohistochemical experiments performed on paraffin-embedded sections of this tumor revealed positivity for vimentin and keratin and negativity for EMA, inhibin, estrogen receptor, progesterone receptor and Ki-67. Interestingly, the basal laminae of the tumoral tissues were PAS (+), demonstrating the presence of mucin (Figure 3).
Female adnexal tumors of probable Wolffian origin has been reported as immunoreactive for pancytokeratin (AE1/3, CK1) (100%), CAM 5.2 (100%), cytokeratin 7 (88%), keratin 903 (17%), EMA (12%), estrogen receptor (78%), inhibin (68%), calretinin (91%), and vimentin (100%) [2–5]. Ki-67 is a nuclear antigen expressed in proliferating but not resting cells, and it provides useful information concerning the growth potential of individual tissues and tumors. Li et al. [4] have reported two cases with Ki-67 labeling indexes of 0% and 3.2%, respectively. In our patient, tumoral tissues were Ki-67 negative, reflecting the low mitotic indexes seen microscopically. This case is the second known instance of FATWO with negative Ki-67 immunostaining. Increasing evidence regarding the clinical benefit of Ki-67 positivity in FATWO may help physicians to estimate the ideal extent of the initial surgical procedure.
Differential diagnosis of FATWO includes Sertoli-Leydig cell tumors, clear-cell tumors and granulosa cell tumors. Sertoli-Leydig cell tumors are usually multi-insular or lobulated with cellular and differentiated zones and stromal cells of the steroid-hormone-secreting type, including cell-sparse areas, unlike Wolffian duct tumors. Well-developed hobnail cells, intraluminal mucin, solid aggregates of clear cells, and papillary areas are distinguishing features of clear-cell carcinomas compared to FATWO. Grooved nuclei, scant neoplasm and endocrine manifestations are traits of granulosa cell tumors that resemble Wolffian duct tumors pathologically.
In conclusion, FATWO are rare tumors that usually follow a benign course. According to the desire of the individual patient for fertility, surgical debulking with total abdominal hysterectomy and bilateral salpingo-oophorectomy is the most appropriate initial surgical procedure. Immunohistochemical staining with promising new markers and pathological investigation of the entire tumor are required to determine the malignant behavior of FATWO. Treatment recommendations can still not be made before prospective clinical trials. Ki-67, a proliferation marker, is a helpful marker for determining Wolffian duct tumors’ potential malignant behavior. More data and large, multicenter, multidisciplinary experimental and/or clinical studies are needed to determine the clinical utility of detecting the malignant types of FATWO.
Figure 2.
Tumoral cells forming tubular and cord structures beneath the outlining mesotelial layer (HE×40).
Footnotes
Conflict of interest statement: The authors declare that they have no conflict of interest to the publication of this article.
References
- 1.Steed H, Oza A, Chapman WB, Yaron M, Petrillo DD. Female adnexal tumor of probable Wolffian origin: a clinicopathological case report and a possible new treatment. Int J Gynecol Cancer. 2004;14:546–50. doi: 10.1111/j.1048-891x.2004.014319.x. [DOI] [PubMed] [Google Scholar]
- 2.Ramirez PT, Wolf JK, Malpica A, Deavers MT, Liu J, Broaddus R. Wolffian duct tumors: case reports and review of the literature. Gynecol Oncol. 2002;86:225–30. doi: 10.1006/gyno.2002.6739. [DOI] [PubMed] [Google Scholar]
- 3.Bata MS, Kamal MF. Female adnexal tumour of probable Wolffian origin in a 23-year-old woman. Eur J Obstet Gynecol Reprod Biol. 1999;87:179–82. doi: 10.1016/s0301-2115(99)00108-6. [DOI] [PubMed] [Google Scholar]
- 4.Li CC, Qian ZR, Hirokawa M, et al. Expression of adhesion molecules and Ki-67 in female adnexal tumor of probable Wolffian origin (FATWO): Report of two cases and review of the literature. APMIS. 2004;112:390–8. doi: 10.1111/j.1600-0463.2004.t01-1-apm1120602.x. [DOI] [PubMed] [Google Scholar]
- 5.Abbot RL, Barlogie B, Schmidt WA. Metastasizing malignant juxtaovarian tumor with terminal hypercalcemia: a case report. Cancer. 1981;48:860–5. doi: 10.1002/1097-0142(19810801)48:3<860::aid-cncr2820480333>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 6.Sadler TW. Langman’s medical embryology. 5th ed. Baltimore: Williams&Wilkins; 1989. [Google Scholar]
- 7.Brescia RJ, Cardosa de Almeida PC, Fuller AF, Dickersin GR, Robboy SJ. Female adnexal tumor of probable Wolffian origin with multiple recurrences over 16 years. Cancer. 1985;56:1456–61. doi: 10.1002/1097-0142(19850915)56:6<1456::aid-cncr2820560638>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 8.Tosun M, Tosun E, Avunduk MC. Importance and usage of the cell proliferation markers. Turkiye Klinikleri J Med Sci. 2001;21:235–44. [Google Scholar]
- 9.Tiltman AJ, Allard U. Female adnexal tumours of probable Wolffian origin: an immunohistochemical study comparing tumours, mesonephric remnants and paramesonephric derivetives. Histopathology. 2001;38:237–42. doi: 10.1046/j.1365-2559.2001.01086.x. [DOI] [PubMed] [Google Scholar]
- 10.Atallah D, Rouzier R, Voutsadakis I, et al. Malignant female adnexal tumor of probable Wolffian origin relapsing after pregnancy. Gynecol Oncol. 2004;95:402–4. doi: 10.1016/j.ygyno.2004.07.042. [DOI] [PubMed] [Google Scholar]


