Abstract
Silicosis is a well-known occupational lung disease that was discovered by the ancient Greeks and Romans. In 2001, it has emerged again in an unexpected occupation: denim sandblasting. Exposure to crystalline silica, with or without clinical disease, is one of the most important predisposing factors for the development of tuberculosis; however, there has been no previous report of tuberculosis among cases of silicosis due to denim sandblasting. Herein, we report the first case of a denim sandblaster with silicosis who developed both pulmonary tuberculosis and tuberculous meningitis.
Keywords: Denim sandblaster, Pulmonary tuberculosis, Tuberculous meningitis
Özet
Silikozis antik Yunan ve Romalılar tarafından keşfedilmiş iyi bilinen mesleksel bir akciğer hastalığıdır. 2001’de beklenmeyen bir şekilde tekrar ortaya çıktı: Kot kumlama. Silika kristallerine maruziyet, klinik hastalıkla birlikte veya birlikte olmadan, tüberküloz gelişiminde en önemli predispoze faktörlerden birisidir. Bununla beraber kot kumla-maya bağlı silikozis vakaları arasında daha önce tüberküloz gelişimi bildirilmemiştir. Bu noktada, hem tüberküloz menenjit hemde akciğer tüberkülozunun geliştiği silikozisli ilk kot kumlama vakasını bildirdik.
Introduction
It is well known that silicosis, or even silica exposure without silicosis development, is one of the most important risk factors in the development of tuberculosis [1–3]. Silicosis due to denim (or jean) sandblasting in the textile industry has recently been reported as a new cause of silicosis [4–6]. In this process, sifted sea sand has been used as an abrasive to produce worn-out jeans. Because of high silica exposure and younger worker population, silicosis has developed in a relatively short period of time with fatal outcomes [6, 7]. Although some cases had been initially misdiagnosed as tuberculosis [4], there has been no previous report of tuberculosis among the cases of silicosis due to denim sandblasting. Herein, we report the first case of a denim sandblaster with silicosis who developed both pulmonary tuberculosis and tuberculous meningitis.
Case Report
A 21-year-old man was admitted to our hospital with a history of malaise, dry cough and fever with chills for the previous fifteen days. He was prescribed ceftriaxone 1 gram twice daily for one week with no benefit. On admission, the patient still had a fever (40 °C), although the rest of the physical examination was unremarkable. Based on his occupational history, five years ago, he had worked in a textile factory for approximately four months. His primary job was sandblasting of jeans to abrade them to produce a worn-out appearance. He had been diagnosed with silicosis two years ago. Laboratory investigations revealed a WBC of 13,000 cells/mm3 with increased neutrophils (85%), a CRP of 2.5 mg/dl and an erythrocyte sedimentation rate of 40 mm/h. Sputum analysis for tuberculosis and the tuberculin skin reaction were both negative. Other laboratory tests, including assays for Brucella because of its endemicity in our region, were unremarkable except for a real time polymerase chain reaction (RT-PCR) assay of the blood that revealed positivity for Mycobacterium tuberculosis. The patient’s chest x-ray showed a reticular pattern in the middle and lower part of both lungs, and high resolution computerized tomography revealed multiple micronodular opacities that were compatible with his previous diagnosis of silicosis (Figure 1a, b, c). A bronchoscopic investigation was planned to obtain a lung tissue sample to confirm or rule out tuberculosis, but the patient refused all interventions. Then, he was given empirical anti-tuberculosis treatment, but he decided leave the hospital against medical advice.
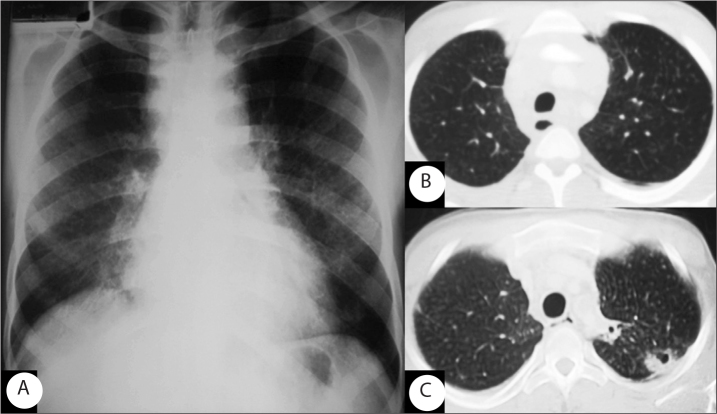
Figure 1.
Chest radiograph shows a reticular pattern in the middle and lower regions of both lungs (A). Axial CT images (lung window) obtained at the level of the upper mediastinum show multiple micronodular opacity in the upper lobe (B) and ill-defined cavities in the left upper lobe (C) on the first and second admission, respectively.
Five months later, the patient was re-admitted to our hospital with a history of fever, productive cough, headache, agitation and vomiting. On physical exam, he had ptosis of the right eyelid, neck stiffness, reduced cognitive function, and positive Kernig’s and Brudzinski’s signs. He had used his antituberculosis drugs for only twenty days after discharge. Magnetic resonance imaging of the brain showed multiple lesions indicative of tuberculomas (Figure 2). A lumbar puncture (LP) was performed, and 70 cells per mm3 were counted with a lymphocyte predominance. Glucose level in the CSF was low (28 mg/dl) compared with the measurement of 113 mg/dl in the blood. The protein level in the CSF was 300 mg/dl. Gram stain and culture of the CSF were negative. An AFB stain of the CSF was negative, but RT-PCR showed positivity for Mycobacterium tuberculosis. Although there were lung cavitations on the second High Resolution Computed Tomography (HRCT) on his second admission, the sputum analysis for tuberculosis was still negative. Tuberculosis treatment was reinitiated, and both clinical and laboratory findings, including control LP, of the patient improved within ten days.
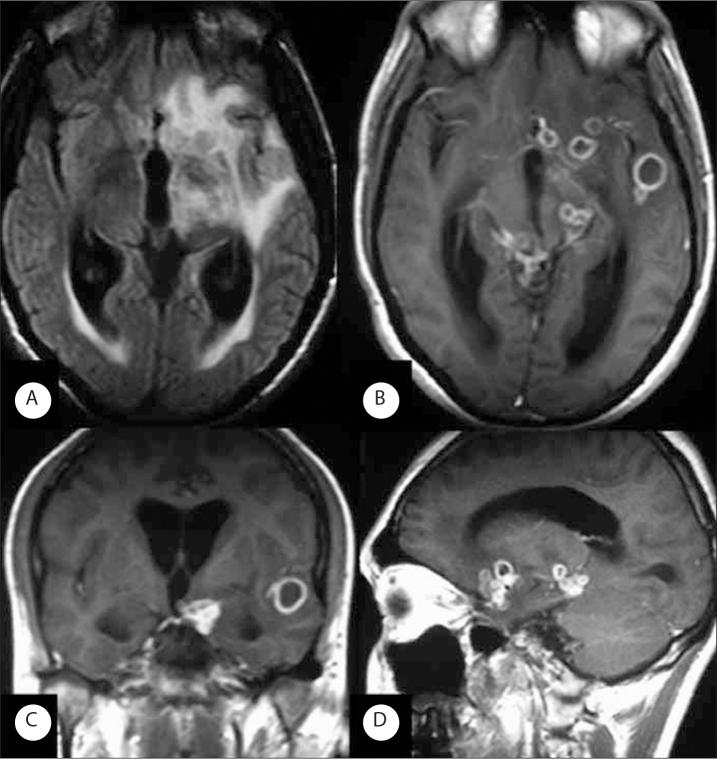
Figure 2.
Axial FLAIR brain images (A) shows periventricular hyperintensity and left frontoparietal hyperintensity due to vasogenic edema and isointense multiple tuberculomas. Note the widened occipital horns due to communicating hydrocephalus. Axial (B), coronal (C) and sagittal (D) gadolinium-enhanced T1-weighted MR images show multiple ring-enhancing tuberculoma lesions. The majority of these lesions are near the cortex or deep gray matter, with most being at gray matter-white matter junction.
Discussion
Silicosis is a well-known fibrotic disease of the lungs caused by inhalation, retention and pulmonary reaction to crystalline silica. The clinical course of the disease is dependent on many factors, such as dust concentration, the exposure duration and the latency period. Silicosis has recently been described in denim sandblasters. In denim sandblasting, because of a combination of various factors, silicosis most commonly manifests as acute silicosis even in the cases with relatively short exposure duration [4–6]. Although silicosis mainly affects the lungs, it may have some direct or indirect extra-pulmonary effects [8–10].
In the acute forms of silicosis, the main problem is respiratory insufficiency; however, in the sub-acute and chronic forms of the disease, in addition to respiratory insufficiency, some other problems may affect the prognosis and survival of patients. Exposure to crystalline silica, with or without clinical disease, increases the risk of tuberculosis and other nonmalignant respiratory diseases and contributes to the development of renal or autoimmune respiratory diseases. In addition, crystalline silica has been designated as a known human carcinogen [11].
Although the prevalence of tuberculosis is decreasing in the general population, workers with silicosis are at risk for developing tuberculosis [12]. It is well documented that exposure to silica can lead to impaired cell-mediated immunity. Evidence from experimental studies suggests that silica impairs the metabolism and function of pulmonary macrophages and, with frequent exposure, causes macrophage apoptosis [13]. Alterations in lymphocyte subsets, i.e., a reduced number of T cells, and changes in serum immunoglobulin levels in patients with silicosis have been observed in workers with silicosis [14]. These findings are consistent with observations that the incidence of tuberculosis is higher in dust-exposed workers, even in those without established silicosis, than in workers who are not exposed to dust.
Epidemiologic studies have confirmed that those with chronic silicosis have a 3-fold increased risk of developing tuberculosis (both pulmonary and extrapulmonary) compared with an aged-matched, silica-exposed group without silicosis [15]. The incidence of tuberculosis and non-tuberculosis mycobacterial disease is highest in acute and accelerated silicosis [16].
A study among South African gold miners indicates that the silica dust that miners accumulate in their lungs during exposure is a lifelong risk for the development of pulmonary tuberculosis (PTB), even if silicosis is not present in the lungs. Furthermore, even after the exposure to dust ends, ex-miners continue to be at risk of developing silicosis, and the development of silicosis places them at even greater risk of developing PTB. Moreover, the data show that miners with very few silicotic nodules (negligible and slight degree of silicosis) have a significantly increased risk of developing PTB and that this degree of silicosis is seldom diagnosed radiologically.
This case was an accelerated silicosis case with a relatively short exposure and a latency period. In denim sandblasters, more than half of the workers had developed either acute or accelerated silicosis although they had very short periods of exposure, but possibly heavy exposure, to crystalline silica [6]. In the first cases, it is highly possible that they were misdiagnosed as having tuberculosis [4] because there are no previously reported silicosis cases among denim sandblasters and they were subjected to poor working conditions. To the best of our knowledge, this is the first report of tuberculosis, both PTB and tuberculosis meningitis, among denim sandblasters; however, we can speculate that more cases will be reported given the numbers of denim sandblasters with silica exposure.
With this report, we aimed to present the first case of TB development in a silicosis cases due to denim sandblasting and to draw attention to this issue. Silicosis continues to cause deaths due to respiratory insufficiency. Although there are few new cases of silicosis due to recent silica exposure in denim sandblasting, there is a huge pool of these cases due to past exposure; therefore, the exact extent of this disease burden is unknown, but new tuberculosis cases among these workers are expected.
Footnotes
Conflict of interest statement: The authors declare that they have no conflict of interest to the publication of this article.
References
- 1.Calvert GM, Rice FL, Boiano JM, Sheehy JW, Sanderson WT. Occupational silica exposure and risk of various diseases: an analysis using death certificates from 27 states of the United States. Occup Environ Med. 2003;60:122–9. doi: 10.1136/oem.60.2.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bang KM, Weissman DN, Wood JM, Attfield MD. Tuberculosis mortality by industry in the United States, 1990–1999. Int J Tuberc Lung Dis. 2005;9:437–42. [PubMed] [Google Scholar]
- 3.teWaternaude JM, Ehrlich RI, Churchyard GJ, et al. Tuberculosis and silica exposure in South African gold miners. Occup Environ Med. 2006;63:187–92. doi: 10.1136/oem.2004.018614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akgun M, Gorguner M, Meral M, et al. Silicosis caused by sand-blasting of jeans in Turkey: a report of two concomitant cases. J Occup Health. 2005;47:346–9. doi: 10.1539/joh.47.346. [DOI] [PubMed] [Google Scholar]
- 5.Akgun M, Mirici A, Ucar EY, Kantaci M, Araz O, Gorguner M. Silicosis in Turkish denim sandblasters. Occup Med. 2006;56:554–8. doi: 10.1093/occmed/kql094. [DOI] [PubMed] [Google Scholar]
- 6.Akgun M, Araz O, Akkurt I, et al. An epidemic of silicosis among former denim sandblasters. Eur Respir J. 2008;32:1295–303. doi: 10.1183/09031936.00093507. [DOI] [PubMed] [Google Scholar]
- 7.Cimrin A, Sigsgaard T, Nemery B. Sandblasting jeans kills young people. Eur Respir J. 2006;28:885–6. doi: 10.1183/09031936.06.00066406. [DOI] [PubMed] [Google Scholar]
- 8.Yoruk O, Ates O, Araz O, et al. The effect of silica exposure on upper airways and eyes in denim sandblasters. Rhinology. 2008;46:328–33. [PubMed] [Google Scholar]
- 9.Tiwari RR, Sharma YK. Respiratory health of female stone grinders with free silica dust exposure in Gujarat, India. Int J Occup Environ Health. 2008;14:280–2. doi: 10.1179/oeh.2008.14.4.280. [DOI] [PubMed] [Google Scholar]
- 10.Ogawa S, Imai H, Ikeda M. Mortality due to silico-tuberculosis and lung cancer among 200 whetstone cutters. Ind Health. 2003;41:231–5. doi: 10.2486/indhealth.41.231. [DOI] [PubMed] [Google Scholar]
- 11.Fanning F. Hazards of crystalline silica. Engineer. 2004;34:36–41. [Google Scholar]
- 12.Cowie RL. The epidemiology of tuberculosis in gold miners with silicosis. Am J Respir Crit Care Med. 1994;150:1460–2. doi: 10.1164/ajrccm.150.5.7952577. [DOI] [PubMed] [Google Scholar]
- 13.Hnizdo E, Murray J. Risk of pulmonary tuberculosis relative to silicosis and exposure to silica dust in South African gold miners. Occup Environ Med. 1998;55:496–502. doi: 10.1136/oem.55.7.496. Erratum in: Occup Environ Med 1999; 56: 215–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Green FHY, Vallyathan V. Pathologic responses to inhaled silica. In: Castranova V, Vallyathan V, Wallace WE, editors. Silica and silica-induced lung diseases. Boca Raton, FL: CRC Press; 1996. pp. 39–59. [Google Scholar]
- 15.Cowie RL. The epidemiology of tuberculosis in gold miners with silicosis. Am J Respir Crit Care Med. 1994;150:1460–2. doi: 10.1164/ajrccm.150.5.7952577. [DOI] [PubMed] [Google Scholar]
- 16.Ziskind M, Jones RN, Weill H. Silicosis. Am Rev Respir Dis. 1976;113:643–65. doi: 10.1164/arrd.1976.113.5.643. [DOI] [PubMed] [Google Scholar]