Abstract
Objective:
Tracheal diverticulum (DV) is an incidental finding in thoracic computed tomography examinations. Tracheal DV may be associated with chronic cough and chronic obstructive pulmonary disease (COPD). A few studies have investigated the relationship between tracheal DV and COPD. There is still no consensus on the relationship. The purpose of this study was to determine the incidence of tracheal DV and its coexistence with bronchial DV and hyperaeration.
Materials and Methods:
For the study, 299 patients from a total number of 12 800 patients who underwent a thoracic computed tomography examination were included. Tracheal diverticula were evaluated for localization, size, contour, wall thickness and communication with the tracheal lumen. The association of tracheal DV with bronchial DV and hyperaeration was also noted. The relationship between tracheal DV and hyperaeration was analyzed.
Results:
Of the 299 patients, a total of 412 tracheal diverticula were observed. Out of these, 148 of the tracheal diverticula were in females, and 264 of the tracheal diverticula were in male patients. The incidence of tracheal DV was determined to be 2.38% in this study. In total, 400 of the tracheal diverticula (97.1%) were located at the right posterolateral aspect of the trachea, and 320 of the tracheal diverticula were associated with hyperaeration. There was no significant relation between the tracheal DV and hyperaeration. However, 84 of 412 tracheal diverticula had a bronchial DV, and 72 of 84 of these bronchial DV were associated with COPD. Statistical analysis indicated a significant correlation with COPD and bronchial DV (p<0.05).
Conclusion:
Tracheal DV is often asymptomatic and mostly located in the right posterolateral aspect of the trachea. Tracheal DV is more common in men than in women. The incidence of tracheal DV was 2.38% in this study. Our data demonstrate that there was no significant association between tracheal DV and COPD. However, there was a significant association between subcarinal bronchial DV and COPD.
Keywords: Bronchi, Chronic Obstructive Pulmonary Disease, computed tomography, diverticula, trachea
Özet
Amaç:
Trakeal divertiküller, toraks bilgisayarlı tomografi incelemesinde insidental olarak saptanır. Kronik öksürük ya da kronik obstrüktif akciğer hastalıkları ile birlikte görülebilir. Literatürde trakeal divertikül ve kronik obstrüktif akciğer hastalıkları arasındaki ilişkiyi araştıran az sayıda çalışma olmakla birlikte çalışmalar arasında hala çelişki bulunmaktadır. Bizim bu çalışma ile amacımız trakeal divertiküllerin insidansını ve trakeal divertikülün, bronşial divertikül ve havalanma fazlalığı ile ilişkisini araştırmaktır.
Gereç ve Yöntem:
Kasım 2009–2011 tarihleri arasında toplamda 12 800 hastaya toraks bilgisayarlı tomografisi yapıldı ve çalışmaya sadece 299 olgu dahil edildi. Trakeal divertiküllerin lokalizasyonu, boyutu, konturu, duvar kalınlığı ve trakea lümeni ile ilişkisi değerlendirildi. Ayrıca bronşial divertikül ve havalanma fazlalığı ile ilişkisi araştırıldı. İstatiksel analizde SPSS 18 programı kullanıldı. Trakela divertikül ve hiperareasyon arasındaki ilişki istatistiksel olarak değerlendirildi.
Bulgular:
Toplamda 299 hastada 412 trakeal divertikül saptanmış olup bunların 148’i kadınlarda, 264’ü erkeklerde izlendi. Bizim çalışmamızda trakela divertikül insidansı %2.38 dir. Trakeal divertiküllerin 400’ü (%97.1), trakeanın sağ posterolateral kesiminde saptandı. Toplamda 320 trakela divertikülün havalanma fazlalığı ile birlikteliği tespit edilmekle birlikte trakeal divertiküller ile havalanma fazlalığı arasında anlamlı ilişki saptanmadı. Ayrıca 412 olgudan 84’ünde bronşial divertikül izlenmiş olup 84 olgunun 72’sinde kronik obstrüktif akciğer hastalığı tespit edildi. Yapılan istatistiksel analizde kronik obstrüktif akciğer hastalıkları ile bronşial divertiküller arasında anlamlı ilişki saptandı (p<0.05).
Sonuç:
Sonuç olarak, bizim çalışmamızda trakeal divertikül insidansı %2.38 dir. Trakeal divertiküller sıklıkla asemptomatik olup genellikle trakeanın sağ posterolateral kesiminde yerleşim gösterir. Bizim çalışmamızda trakeal divertiküller kadınlara göre erkeklerde daha sık saptandı. Ayrıca yapmış olduğumuz istatistiksel analizde trakeal divertiküller ile kronik obstrüktif akciğer hastalıkları arasında anlamlı ilişki saptanmadı. Ancak subkarinal bronşial divertiküller ile kronik obstrüktif akciğer hastalıkları arasında anlamlı ilişki tespit edildi.
Introduction
Tracheal diverticulum (DV) is a paratracheal air cyst that pouches out of the tracheal wall. It is histopathologically a lymphoepithelial or bronchogenic cyst. All of these cysts consist of ciliated columnar epithelia and may be connected to the trachea with a thin neck [1].
Multidetector computed tomography (MDCT) is important for the diagnosis of tracheal DV and co-existing parenchymal pathologies. Goo et al. [1] demonstrated that tracheal DV and bronchial DV may be accompanied by chronic obstructive pulmonary disease (COPD). The aim of the current study was to determine the incidence of tracheal DV and its coexistence with bronchial DV and hyperaeration.
Materials and Methods
Twelve-thousand and eight-hundred consecutive patients underwent chest CT (64 slice MDCT, Toshiba Aquilion, Chicago, USA) at our institution between November 2009 – November 2011. These patients were retrospectively evaluated by a single radiologist expert in the field of thoracic radiology. Patients with mediastinal injury were not included in the study. The CT examinations were performed in a caudalcranial direction with a 1-mm slice thickness and full inspiration in the supine position. The window width was 1500 Hounsfield Units (HU) for the lung window and 400 HU for the mediastinal window. The window level was −700 HU for the lung window and 10 HU for the mediastinal window. The measurements were made in the axial plane; however, coronal and sagittal images were used if necessary. Intravenous contrast agents were used for all of the scans except for patients with acute or chronic renal insufficiency. A total of 288 examinations, including trauma, additional or follow-up, were also excluded. Overall, a total of 12 512 patients were included in the study. A total of 412 tracheal diverticula were detected in 299 of the 12 512 patients.
The localization, size, contour and wall thickness of all detected diverticula and DV necks were noted. Because of the high reported incidence of tracheal and bronchial DV association with the COPD, observed hyperaeration was also noted in each DV patient. Parenchymal attenuation values below −950 HU were accepted as hyperaeration [2].
The anterior-posterior (AP) and transverse (Tr) diameters of the tracheal DV were measured on the axial planes. The average diameter and the mean value were calculated for both measurements.
Analysis
SPSS 18 was used for statistical analysis. The relation between bronchial DV and age, gender and hyperaeration was assessed by using a chi-square test.
Results
In this study, the incidence of tracheal DV was calculated to be 2.38%. A total of 412 diverticula were detected in 299 patients The number of tracheal diverticula was one in 226 (75.5%) patients, two in 40 (13.3%) patients, three in 27 (9%) patients and four in six (2%) patients. The AP and Tr diameters of the tracheal diverticula were measured, and the average size of the diverticula were calculated in each patient. The DV size ranged from 2 to 6 mm (mean 4 mm).
In total, 148 tracheal diverticula (36%) were observed in women, and 264 (64%) were observed in men. The mean patient age was 58 years (range 16–93 years). Of all the diverticula, 400 diverticula (97.1%) were located at the right posterolateral aspect of the trachea (Figure 1), and 12 diverticula (2.9%) were located at the left side. In addition, 405 (98.3%) tracheal DV had a well-defined thin wall, whereas 7 (1.7%) tracheal DV had a thick wall. Communication between the trachea and cyst was demonstrated in 53 diverticula (12.9%) (Figure 2a, 2b), but in 359 cases (87.1%), the DV necks were closed. In total, 84 tracheal diverticula (20.4%) were associated with bronchial DV.
Figure 1.
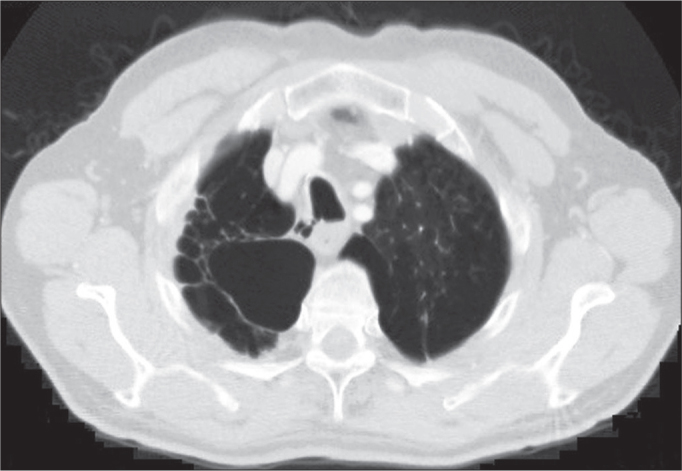
Axial chest CT revealed a lobulated right tracheal diverticulum with a narrow communicating channel and bilateral paraseptal emphysema.
Figure 2.
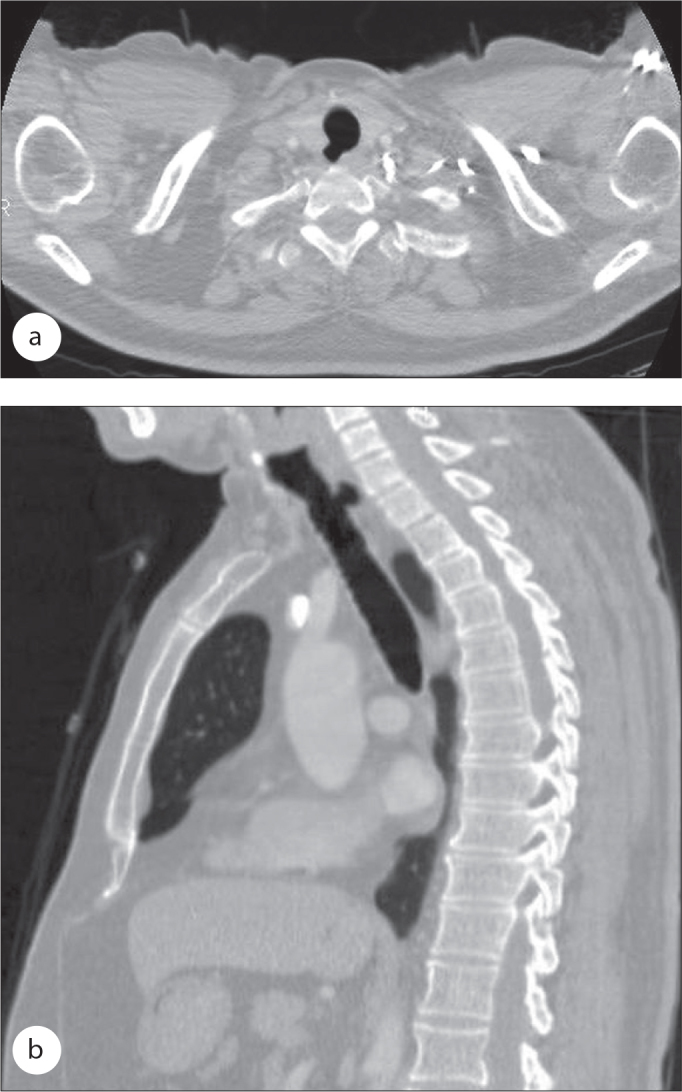
a, b. Axial (a) and coronal (b) chest CT images reveal a well-defined right tracheal diverticulum that has communication with the trachea.
For the patients under the age of 50, 127 (30.9%) tracheal diverticula were observed, 20 of which were accompanied by bronchial DV. For the patients over the age of 50, 285 (69.1%) tracheal diverticula were observed, 64 of which were accompanied by bronchial DV. There was no significant relation between patient age and bronchial DV. In addition, 148 tracheal diverticula were detected in female patients, of which 25 (16.8%) of the diverticula had an accompanying bronchial DV, whereas 123 (83.1%) of the diverticula did not. In total, 264 tracheal diverticula were detected in male patients, of which 59 (22.3%) of the diverticula had an accompanying bronchial DV, whereas 205 (77.6%) of the diverticula did not. There was no significant relation between patient sex and bronchial DV.
A total of 320 tracheal diverticula were associated with hyperaeration. However, there was no significant relation between tracheal DV and hyperaeration. In total, 84 of the 412 tracheal diverticula had a bronchial DV, and 72 of the 84 tracheal diverticula were associated with COPD. Statistical analysis indicated a good correlation between COPD and a bronchial DV (p<0.05) (Figure 3).
Figure 3.
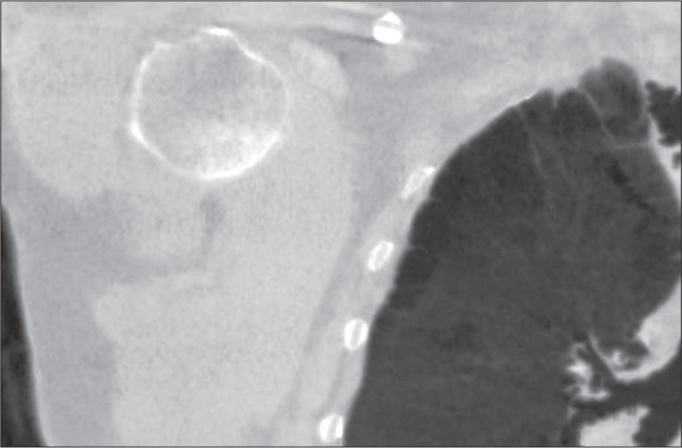
Coronal CT image of the chest shows the multiple right bronchial diverticula of the right upper lobe bronchus and paraseptal emphysema.
Discussion
Although the etiology and pathophysiology of the paratracheal air cysts are still unknown, they are mostly considered as tracheal DV [2]. Tracheal DV is usually incidental, and the incidence is 1% in postmortem studies. Tracheal diverticula are mostly located at the right posterolateral aspect of the trachea at the level of the T2 vertebrae, which is the transitional zone of the intrathoracic and extrathoracic trachea [3]. There are two types of tracheal diverticula: congenital and acquired [4]. Tracheal diverticula in adults are mucosal herniations that occur in the weak parts of the tracheal wall due to increased intraluminal pressure. Congenital tracheal diverticula are air sacs with a narrow and small neck that is formed by malformed supernumerary branches of the trachea and are usually placed a few centimeters over the carina. Diverticula may be isolated or associated with other congenital anomalies of the tracheobronchial tree. Acquired tracheal diverticula are larger than congenital diverticula and have wider necks [5].
Tracheal DV is usually asymptomatic. If it becomes a large cavitary lesion filled with secretions, it can cause chronic cough, recurrent respiratory tract infections, hemoptysis, dyspnea or stridor. In addition, tracheal DV can apply pressure to the vocal cords, and thus, dysphonia can occur [5]. CT can also be used to evaluate the complications of tracheal DV such as perforation or inflammation as has been reported in the literature [6].
According to our experience, tracheal DV is not uncommon in the general population. The incidence of tracheal DV varies between 2% and 3.7%, according to the literature [1, 7, 8]. In this study, the incidence of tracheal DV was determined to be 2.4%, which is accordance with literature reports.
Cheng et al. [2] and Buterbough et al. [7] concluded that paratracheal air cysts are more common in females than males. They demonstrated a significant association between paratracheal air cysts and sex; however, in our study, we demonstrated that tracheal and bronchial diverticula were more common in males (64%) than females (36%). In addition, there was no significant relation between sex and bronchial-tracheal diverticula observed in our study.
Buterbough et al. [7] reviewed 26 patients with paratracheal cysts and observed that 9 of them (34.6%) had direct communication with the trachea. Goo et al. [1] also reported that 8% of the tracheal diverticula were communicating with the trachea. The incidence of communicating with tracheal lumen was observed to have a wide range. Tracheal DV necks were observed in 12.9% of the diverticula in our study. Sometimes the neck of the DV may not be clearly observed with MDCT. In such cases, the diverticula cannot be considered to be abnormal paratracheal air cysts because they may have a thin neck or fibrous connection to the tracheal lumen. Coronal and sagittal MDCT images are very useful for demonstrating the communication between the trachea lumen and the DV. Bronchoscopy can be used in the diagnosis of the tracheal DV, but narrow-necked DV and fibrous connections can be easily misdiagnosed [9].
Previous studies reported a relationship between tracheal DV and COPD [1, 8]. Goo et al. [1] reported that right paratracheal air cysts might even be a sign of the COPD. On the other hand, Buterbough et al. [7] concluded that there was no significant association between paratracheal air cysts and COPD in their study, which was published in 2008. Buterbough et al. [7] detected 26 paratracheal air cysts in a study in which 702 trauma patients were evaluated. In their study, none of the patients had findings of emphysema in the lung apices; however, the mean age of the patients was 37, and 5 of the patients were teenagers. Therefore, these lesions might be congenital tracheal diverticula rather than acquired. Although the mean age in our study was 58, we did not observe a significant relation between the tracheal DV and hyperaeration. On the other hand, we detected a significant relation between bronchial diverticula and hyperaeration.
Bronchial diverticula are extraluminal air foci with a thin connection to the bronchi under the carina. They are considered to be bronchial DV although the histopathological correlation has never been performed. Their etiology remains unknown, but they might occur due to weakness of the bronchial wall. In addition, infectious agents or smoking can cause damage to the bronchial wall that might be conducive to the formation of bronchial diverticula [10]. Previous studies have demonstrated that bronchial diverticula have a significant association with COPD and smoking-related lung disease [11, 12]. Sverzellati et al. [12] evaluated the large population of smokers and showed that the existence of more than 3 bronchial diverticula were associated with severe functional impairment (defined by FEV1, FVC and FEV1/FVC ratio values). However, Higuchi et al. [10] reported that there was no significant association between the size of the bronchial DV and FEV1%. In our study, a total of 84 among 299 patients had bronchial diverticula, and 72 of the patients (85.7%) had more than 3 diverticula in our study. In addition, all of the 72 patients presented hyperaeration, and the statistical analysis indicated a significant relation between COPD and bronchial diverticula. However, this does not indicate that bronchial DV is a criterion for COPD, as subcarinal bronchial DV can be observed incidentally or in non-smokers. Still, if a bronchial DV is detected in a CT scan, clinicians should be aware of the possibility of COPD, especially in smokers.
This study has a few limitations. First, it was a retrospective study. Second, there was no histopathological diagnosis of the tracheal diverticula. Third, none of the patients had a bronchoscopy to demonstrate the communication between the DV and the tracheal lumen, although it should be kept in mind that the bronchoscopy may not always clearly reveal the communication between the DV and the tracheal lumen.
In conclusion, the incidence of tracheal DV was 2.38% in this study. Tracheal diverticula were more common in men than in women in our study. Our data demonstrate that there was no significant association between tracheal DV and COPD. However, we observed a significant association between subcarinal bronchial diverticulum and COPD.
Footnotes
Conflict of interest statement: The authors declare that they have no conflict of interest to the publication of this article.
References
- 1.Goo JM, Im JG, Ahn JM, et al. Right paratracheal air cyst in the thoracic inlet: Clinical and radiologic significance. AJR Am J Roentgenol. 1999;173:65–70. doi: 10.2214/ajr.173.1.10397101. [DOI] [PubMed] [Google Scholar]
- 2.Cheng HM, Chang PY, Chiang KH, Huang HW, Lee CC. Prevalance and characteristics of paratracheal air cysts and their association with emphysema in a general population. Eur J Radiol. 2012;81:2673–7. doi: 10.1016/j.ejrad.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 3.Kim JS, Kim AY, Yoon Y. Paratracheal air cyst using low-dose screening chest computed tomography: clinical significance and imaging findings. Jpn J Radiol. 2011;29:644–8. doi: 10.1007/s11604-011-0608-4. [DOI] [PubMed] [Google Scholar]
- 4.Han S, Dikmen E, Aydin S, Yapakci O. Tracheal diverticulum: a rare cause of dysphagia. Eur J Cardiothorac Surg. 2008;34:916–7. doi: 10.1016/j.ejcts.2008.06.022. [DOI] [PubMed] [Google Scholar]
- 5.Shah M, Joshi JM. Tracheal diverticulum. Indian J Chest Dis Allied Sci. 2012;54:39–40. [PubMed] [Google Scholar]
- 6.Polverosi R, Carloni A, Poletti V. Tracheal and Main Bronchial Diverticula: the role of CT. Radiol Med. 2008;113:181–9. doi: 10.1007/s11547-008-0249-6. [DOI] [PubMed] [Google Scholar]
- 7.Buterbaugh JE, Erly WK. Paratracheal air cyst: A common findings on routine CT examinations of the cervical spine and neck that may mimic pneumomediastinum in patients with traumatic injuries. AJNR Am J Neuroradiol. 2008;29:1218–21. doi: 10.3174/ajnr.A1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.MacKinnon D. Tracheal diverticula. J Pathol Bacteriol. 1953;65:513–7. doi: 10.1002/path.1700650223. [DOI] [PubMed] [Google Scholar]
- 9.Kokkonouzis I, Haramis D, Kornezos I, Moschouris H, Katsenos S, Bouchara S. Tracheal diverticulum in an asymptomatic male: a case report. Cases Journal. 2008;1:181. doi: 10.1186/1757-1626-1-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Higuchi T, Takahashi N, Shiotani M, et al. Main bronchial diverticula in the subcarinal region: Their relation to airflow limitations. Acta Radiol. 2012;53:44–8. doi: 10.1258/ar.2011.110222. [DOI] [PubMed] [Google Scholar]
- 11.Sanford MF, Broderick LS. Multidedector computed tomography detection of bronchial diverticula. J Thorac Imaging. 2007;22:265–7. doi: 10.1097/RTI.0b013e31803bb43b. [DOI] [PubMed] [Google Scholar]
- 12.Sverzellati N, Ingegnoli A, Calabro E, et al. Bronchial diverticula in smokers on thin- section CT. Eur J Radiol. 2010;20:88–94. doi: 10.1007/s00330-009-1515-2. [DOI] [PubMed] [Google Scholar]


