Abstract
Senior-Loken syndrome refers to a disorder in which there is a combination of nephronophthisis and retinal dystrophy. The earliest presenting signs of the renal component are polyuria and polydipsia secondary to defective urinary concentrating ability. Nephronophthisis progresses to end-stage renal disease during the second decade. The retinal lesions are variable, ranging from severe infantile onset retinal dystrophy to more typical retinitis pigmentosa. There is a spectrum of other associated features, including skeletal, dermatological and cerebellar anomalies, observed in this entity. Here, we report a case of Senior-Loken syndrome associated with small hand (short metacarpals) and madarosis. To date, there are no cases reported in the literature describing the association of madarosis with this syndrome, and the presence of small hands has been reported only once.
Keywords: Madarosis, nephronophthisis, retinitis pigmentosa, Senior-Loken syndrome, small hands
Özet
Senior-Loken sendromu, nefronofitizis ve retinal distrofinin birlikte olduğu bir hastalıktır. Renal komponentinin erken başvuru bulguları idrar konsantrasyon yeteneğindeki defekte sekonder gelişen poliüri ve polidipsidir. Nefronofitizis ikinci dekatta son dönem böbrek hastalığına doğru ilerler. Retinal lezyonlar, şiddetli infantil başlangıçlı retinal distrofiden daha tipik retinitis pigmentosaya kadar değişkenlik gösterir. Bu olguda iskelet, dermatolojik ve serebellar anomalileri içeren diğer ilişkili özelliklerin bir spekturumu izlendi. Burada, kısa metakarp ve madarozis ile ilişkili Senior-Loken sendromlu bir olgu sunulmuştur. Bugüne kadar, bu sendrom ile ilişkili madarozisi açıklayan literatürde hiçbir vaka bulunmamaktadır ve kısa metakarp varlığı sadece bir kez rapor edilmiştir.
Introduction
Senior-Loken syndrome refers to a disorder in which there is a combination of nephronophthisis and retinal dystrophy. It was first described in 1961 by Senior et al. [1], who described a family in which six of 13 children had nephronophthisis and tapeto-retinal degeneration. In the same year, Loken et al. [2] described the same condition in two siblings; both siblings had blindness and severe renal failure, and a kidney biopsy showed renal tubular atrophy and dilatation. This syndrome causes 10 to 15 percent of the cases of childhood genetic kidney diseases known as nephronophthisis, a group of illnesses affecting approximately 1 in 50,000 births. The earliest presenting signs of the renal component are polyuria and polydipsia secondary to defective urinary concentrating ability. The onset is insidious, and most cases do not present until renal failure is advanced. The retinal lesions in Senior-Loken syndrome are variable, ranging from severe infantile onset retinal dystrophy to more typical retinitis pigmentosa. There is a spectrum of other associated features, including skeletal, dermatological and cerebellar anomalies, observed in this entity. Here, we report a case of Senior-Loken syndrome associated with small hands (short metacarpals) and madarosis.
Case Report
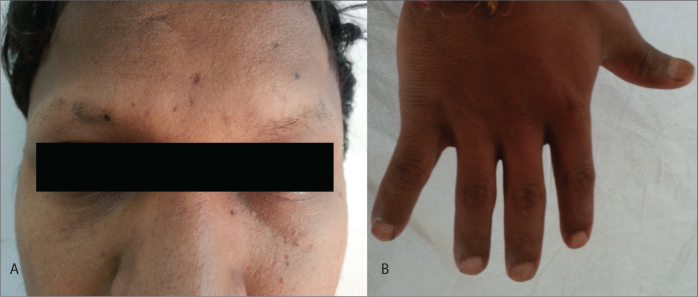
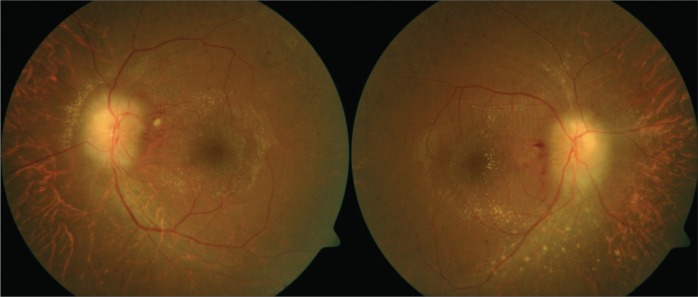
A 19-year-old male student presented to our institute with complaints of headache, dizziness and decreased urine output for one month. On detailed history, he complained of polyuria, nocturia and excessive thirst in his childhood. Further questioning revealed a history of progressive vision deterioration, especially in the dark, for the last 5 years. He also noted the gradual loss of eyebrows during the past 6 months. There was no history of hematuria or facial puffiness, and no similar complaints were elicited among family members. On examination, the patient was of average build, with a height of 162 cm and weight of 58 kgs, and he maintained a normal upper segment to lower segment ratio. He was hypertensive, with a blood pressure of 186/110 mm Hg on presentation. Further examination revealed madarosis and small hands (Figures 1A and 1B). There was no evidence of abnormal sexual development or any spinal deformity. Systemic examination was unremarkable. On ophthalmological examination, the patient had a visual acuity of 6/24 in both eyes, and his indirect ophthalmoscopy revealed papilledema and a macular star with pigmentation at the periphery, suggestive of retinitis pigmentosa (Figure 2). Electroretinogram showed decreased scotopic and photic responses. Brain MRI and audiometric analyses results were within normal physiological limits.
Figure 1.
A) Picture of the patient showing madrosis. B) Picture showing small hands.
Figure 2.
Retinal photographs demonstrating widespread pigmentary abnormalities, suggestive of Retinitis Pigmentosa.
Biochemical investigations were ordered and revealed severe renal dysfunction, with blood urea 312 mg/dL and serum creatinine 10.2 mg/dL, and metabolic acidosis on arterial blood gas analysis. Blood sugar and liver function tests were normal. On imaging, chest X-ray suggested cardiomegaly, and X-ray of the hand showed short metacarpal bones. The echocardiographic findings were consistent with left ventricular hypertrophy with slightly dilated heart chambers. On ultrasonography, bilateral kidneys revealed increased echogenicity with a loss of corticomedullary differentiation. His thyroid function test, serum testosterone, FSH, LH and estradiol levels were normal. Due to advanced renal failure, the patient was admitted for maintenance hemodialysis and provided adequate supportive therapy, including aggressive anti-hypertensive treatment.
Discussion
Cystic disorders of the renal medulla were first noted by Smith and Graham in 1941 and Fanconi in 1951 and led to the term juvenile familial nephronophthisis. The association of nephronophthisis and tapeto-retinal degeneration was described by both Senior and Loken in 1961 [1, 2]. It occurs in approximately 10–15% of all cases of nephronophthisis. Senior-Loken syndrome is also known as renal dysplasia-blindness, hereditary renal-retinal syndrome, and renal-retinal dysplasia.
Renal involvement is in the form of nephronophthisis and is characterized by chronic tubulointerstitial nephritis that progresses to end-stage renal disease during the second decade. Mutations in 9 genes (NPHP1-9) are responsible for nephronophthisis [3]. There are three clinical variants of nephronophthisis depending on the age of onset of end-stage renal disease: severe infantile, juvenile and adolescent, [4]. The initial symptoms are polyuria, polydipsia and enuresis due to a concentrating defect, which is consistent with the symptomology of our patient during early childhood. The disease progresses to end-stage renal disease before the age of 20, although late onset in the third decade has also been reported [5]. Renal histology is characterized by the triad of interstitial infiltration, renal tubular cell atrophy with cyst development and renal interstitial fibrosis [6]. The ultrasonographic findings of juvenile nephronophthisis may be normal, or they may show increased echogenicity of the renal parenchyma, poor cortico-medullary differentiation, a small kidney, and medullary cysts. However, the absence of medullary cysts at presentation does not rule out the diagnosis of juvenile nephronophthisis [7].
The ocular involvement takes several forms: it could be early and severe congenital amaurosis of the Leber type or late-onset pigmentary retinal degeneration. Tapeto-retinal degeneration varies in its nature and severity and is the commonest form. It is characterized by a progressive degeneration of the choroid and the retina. In contrast, retinitis pigmentosa involves bone spicule degeneration that begins from the periphery of the retina and extends to involve the entire retino-choroid [8]. Other ocular findings include cataracts, Coat’s disease and keratoconus. The disease begins in childhood or early adolescence and produces a visual handicap ranging from night blindness, as found in our patient, to functional blindness. The electroretinogram (ERG) is decreased or absent, suggesting a decreased function of rods. ERG helps in the early diagnosis before symptom presentation or fundoscopic examination. In our case, retinitis pigmentosa was observed, as documented on indirect ophthalmoscopy, with a corresponding decreased ERG response. The retinal disease may become progressive; therefore, annual eye examinations beginning at the time of the diagnosis are recommended.
Although less common, some features may also be present in few individuals: A) underdevelopment (hypoplasia) or complete lack (aplasia/agenesis) of the cerebellar vermis, usually indicated by the “molar tooth” sign found on an axial view of a brain MRI scan; B) developmental delays/mental retardation of variable severity; C) difficulty in coordinating voluntary muscle movements or uncoordinated movements (ataxia); D) poor visual function accompanied by rapid, involuntary movements of the eyes (nystagmus), sluggish pupillary responses, intolerance to light (photophobia), and far-sightedness (hyperopia); and E) vascular hypertension as a result of the affected kidneys. Apart from hypertension, our patient showed none of the above-mentioned associations, despite extensive investigations to identify them.
There are no proven treatments for nephronophthisis. Management primarily depends on delaying the progression of renal failure and the need for dialysis and transplantation. Newer agents, such as vasopressin V2 receptor antagonists, which alter the cystogenesis and progression of the disease, may be available for future use [9].
The case presented here, apart from the classical association of renal dysfunction with retinal degeneration, is notable for several reasons, including presentation with end-stage renal disease and association of this syndrome with small hands (short metacarpals) and loss of eyebrows. Madarosis is derived from the ancient Greek word “madaros”, meaning “bald”, and is defined as hair loss of the eyebrows (superciliary madarosis) or loss of eyelashes (ciliary madarosis). This seemingly innocuous sign may be an important manifestation of many local or systemic disorders, including endocrine disorders, malignancy, drugs and toxin exposure. In the absence of any of the aforementioned causes despite thorough investigations, we attributed madarosis to the syndrome itself, regarding it as a unique manifestation of Senior-Loken syndrome.
To date, there are no cases reported in the literature describing the association of madarosis with this syndrome, and the presence of small hands has been reported only once [10]. Although genetic analysis would have enabled a better understanding of this rare entity, we had to stop short due to the lack of expertise and monitory constraints involved in carrying out such studies.
Senior-Loken syndrome dramatically impacts the lives of those it afflicts. Patients with the disorder require dialysis or a kidney transplant by the time they reach adolescence. At approximately the same time, their retinas deteriorate, leaving them blind. Awareness of the possibility of familial juvenile nephronophthisis in patients with Leber’s amaurosis is important because it leads to end-stage renal disease, requiring renal replacement therapy. It is now agreed that patients with nephronophthisis should undergo detailed ophthalmic assessments, including an electroretinogram, periodically. Children with primary tapeto-retinal degeneration should have routine measurements of blood pressure, urinary concentrating ability and renal ultrasound scan. Early diagnosis, hypertension control and protein intake restriction may delay renal replacement therapy.
Footnotes
Conflict of interest statement: The authors declare that they have no conflict of interest to the publication of this article.
References
- 1.Senior B, Friedmann AI, Braudo JL. Juvenile familial nephropathy with tapetoretinal degeneration. A new oculorenal dystrophy. Am J Ophthalmol. 1961;52:625–33. doi: 10.1016/0002-9394(61)90147-7. [DOI] [PubMed] [Google Scholar]
- 2.Loken AC, Hanssen O, Halvorsen S, Jolster NJ. Hereditary renal dysplasia and blindness. Acta Paediatr. 1961;50:177–84. doi: 10.1111/j.1651-2227.1961.tb08037.x. [DOI] [PubMed] [Google Scholar]
- 3.Otto EA, Tory K, Attanasio M, et al. Hypomorphic mutations in meckelin (MKS3/TMEM67) cause nephronophthisis with liver fibrosis (NPHP11) J Med Genet. 2009;46:663–70. doi: 10.1136/jmg.2009.066613. [DOI] [PubMed] [Google Scholar]
- 4.Salomon R, Saunier S, Niaudet P. Nephronophthisis. Pediatr Nephrol. 2009;24:2333–44. doi: 10.1007/s00467-008-0840-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Godel V, Iaina A, Nemet P, Lazar M. Sector retinitis pigmentosa in juvenile nephronophthisis. Br J Ophthalmol. 1980;64:124–6. doi: 10.1136/bjo.64.2.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Waldherr R, Lennert T, Weber HP, Födisch HJ, Schärer K. The nephronophthisis complex. A clinicopathological study in children. Virchow Arch A Pathol Anat Histol. 1982;394:235–54. doi: 10.1007/BF00430668. [DOI] [PubMed] [Google Scholar]
- 7.Blowey DL, Querfeld U, Geary D, Warady BA, Alon U. Ultrasound findings in juvenile nephronophthisis. Pediatr Nephrol. 1996;10:22–4. doi: 10.1007/BF00863431. [DOI] [PubMed] [Google Scholar]
- 8.Fillastre JP, Guenel J, Riberi P, Marx P, Whitworth JA, Kunh JM. Senior-Loken syndrome (nephronophthisis and tapeto-retinal degeneration): A study of 8 cases from 5 families. Clin Nephrol. 1976;5:14–9. [PubMed] [Google Scholar]
- 9.Gattone VH, 2nd, Wang X, Harris PC, Torres VE. Inhibition of renal cystic disease development and progression by a vasopressin V2 receptor antagonist. Nat Med. 2003;9:1323–6. doi: 10.1038/nm935. [DOI] [PubMed] [Google Scholar]
- 10.Singh NP, Anuradha S, Gupta S, Rizvi SN, Arora R. Senior Loken syndrome with unusual manifestations. J AssocPhysician India. 1998;46:740–2. [PubMed] [Google Scholar]