Abstract
Atlantoaxial instability frequently causes extrinsic cervical myelopathy via anterior displacement of the posterior arch of the atlas. However, upper cervical myelopathy resulting from atlantodental osteo-arthritis with the hypertrophic dens due to atlantoaxial instability is very rare. We present a case of upper cervical myelopathy secondary to atlantoaxial instability and atlantodental osteoarthritis. Although there was no atlantoaxial subluxation on the flexion and extension radiographies, hypertrophic changes of the anterior arch of the atlas with the dens axis and a fusion of the atlanto-dental joint resulting from atlantoaxial instability were determined on computed tomography and magnetic resonance imaging.
Keywords: Atlantodental osteoarthritis, Cervical myelopathy, X-Ray, CT, MR
Özet
Atlantoaksial instabilite, atlasın arka arkının öne doğru yer değiştirmesi ile sıklıkla ekstrensek servikal miyelopatiyes ebep olur. Ancak atlantoaksial instabilite sonucu atlantodental osteoartrit ve hipertrofik dense bağlı servikal miyelopati nadirdir. Biz atlantoaksial instabilite ve atlantodental osteoartrite sekonder üst servikal miyelopatili bir hastyı sunduk. Hastanın fleksiyon ve ekstansiyon radyografilerinde belirgin atlantoaksial subluksasyon izlenmemekle birlikte, Bilgisayarlı Tomografi ve Manyetik Rezonans görüntülemede, atlantoaksial instabiliteye bağlı dens aksis ile atlasın ön arkındaki hipertrofik değişiklikler ve atlantodental eklem füzyonu tespit edildi.
Introduction
Cervical myelopathy may result from various extrinsic or intrinsic factors. An abnormal dens axis is a cause of extrinsic myelopathy on the cranio-cervical junction. This abnormality may be congenital, as in a dolichoodontoid, or acquired, as in hypertrophied dens. Atlantooaxial subluxation due to vertebral pathologies (such as rheumatoid arthritis (RA) and trauma) frequently causes upper cervical myelopathy by anterior displacement of the posterior arch of the atlas. However, a few cases were reported in the literature concerning cervical myelopathy secondary to atlantodental osteoarthritis (ADO) with atlantoaxial subluxation (AAS) [1].
Case Report
In this report, 70-year-old female patient is presented. She had suffered from neck pain, weakness and numbness in all extremities, and progressive difficulty in walking for six months. Neurological examination revealed weakness, spasticity, hyperactive deep tendon reflexes in all extremities, and bilateral Babinsky and Hoffmann signs without normal sensation. There was also impaired mastication and deglutition with the pharyngeal reflex lost. Rheumatoid factor (0.00 IU/ml), C-reactive-protein (0.0 mg/l), and antistreptolysin O (80 IU/ml) values were within normal ranges. There were no previous cervical trauma or clinical/ radiological signs of rheumatic disease. Movements of the neck were limited in all plains. However, the atlantoaxial junction was not clearly assessable due to overlaying bone structures; except for irregularity and sclerosis of the apex of the dens axis, apparent instability was not detected on flexion and extension roentgenograms. There was also mild osteoporosis, with spur and ossicle formations on the vertebral bodies. Using an axial plain computed tomography (CT) scan, the hypertrophic dens within the foramen magnum was determined to be a high attenuation structure (159–167 HU) with irregular margins (Figure 1A). The cervical cord was compressed between the hypertrophic dens and the posterior arch of the atlas. The antero-posterior diameter of the hypertrophic dens was 18 mm, and hypertrophic changes were prominent on the apical portion of the dens, which is the attachment site of the ala ligament (Figure 1B). The anterior atlas arch was also hypertrophied, with a 21 mm anteroposterior diameter without a small atlas ring, and there was bone fusion between the anterior atlas arch and the dens. Magnetic resonance (MR) imaging clearly showed the hypertrophic dens and its relationship with the atlas ring, foramen magnum, and cervical cord (Figures 2A–B). There was no abnormal intensity within the cervical cord except for its angulation and decreased thickness. Because surgical treatment was refused, palliative therapy was performed. The case is still being followed.
Fig. 1.

A: On the axial plain CT scan of the brain, the apical portion of the hypertrophic dens is seen as a hyperattenuated structure within foramen magnum (arrow). B:The bone window of the axial CT scan showed the hypertrophic dens axis (arrow) with the hypertrophic anterior arch of the atlas and a narrowed atlanto-dental joint space with bone fusion on the right (arrowhead).
Fig. 2.
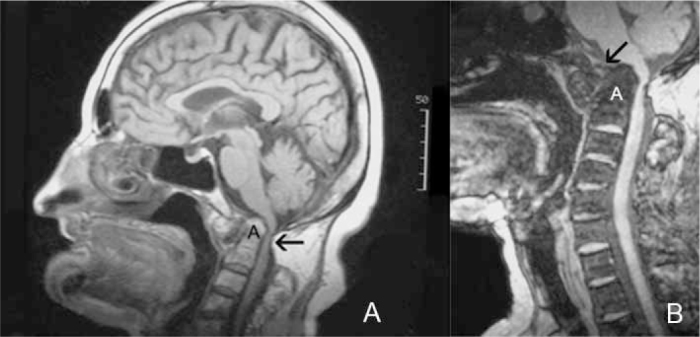
Midsagittal A: T1 weighted and B: T2 weighted MR images show hypertrophic changes of the anterior arch of the atlas and dens axis (A) with atlanto-dental joint sclerosis (white arrow). There are prominent medullar compression with angulation and degenerative changes on the vertebral bodies (black arrow).
Discussion
The most common causes of extrinsic upper cervical myelopathy are basilar impression, a developmentally small atlas ring, atlanto-occipital fusion, atlantoaxial instability, laxity of the transverse atlantal ligament, and anomalies of the odontoid process [1,2]. In adults, an abnormally shaped dens axis may result from acquired hypertrophy, and this condition is often secondary to RA, traumatic spinal fractures, atlantoaxial instability, osteomyelitis, and osseous tumors, such as plasmacytoma. However, ADO complicated with hypertrophic changes of the atlantodental joint is a rare cause of cervical myelopathy. ADO often results from atlantoaxial instability. A mechanical dysfunction and an instability of the atlantoaxial joint cause the hypertrophy of connective tissue elements and fibrous granulation tissue in the periodontoid area. This reactive tissue formation is referred to as a pseudotumor by some authors [3,4]. Lansen et al. [3] reported that the pseudotumor appearance resulted from atlantoaxial instability, and that the pseudotumor subsided after posterior cervical fusion. Enlargement on the anterior arch of the atlas is also an important finding for atlantoaxial instability. Holt et al. [5] stressed that this hypertrophic change may be a reaction to chronic stress on the atlantoaxial junction. A small atlas ring may also be a pre-disposing factor for cervical myelopathy. In the presented case, hypertrophic changes of the dens axis and the atlantodental joint involving the raised thickness of the anterior arch of the atlas without a small atlas ring are seem as evidence of an undetected prior atlantodental instability with osteoarthritis. On flexion and extension roentgenograms, non-visualized instability may be due to inconclusive radiographies performed at inadequate positions because of the failure of the neck movements secondary to the bone fusion of the atlantodental joint.
Clinically neck stiffness, nystagmus, and variable corticospinal tract signs may be correlated with the degree of medullary compression. It is reported that essential hypertension may occur due to medullary compression by the central regulation mechanism of tension and that the resolution of hypertension may be achieved by odontoidectomy [6].
AAS, either horizontal or vertical, may also be found in RA. There is usually periodontoid granulomatous pannus formation in the atlantoaxial joint, sometimes also leading to spinal cord compression. However, as different features from ADO, RA may show local extra-articular involvement, such as tenosynovitis, “rice-bodies” bursitis, and Baker’s cyst rupture and some complications of RA, such as tendinous ruptures, osteonecrosis, stress fractures, and septic arthritis/osteomyelitis. Rheumatoid factor is also usually negative in ADO.
Zapletal et al. [7] described radiologic findings of ADO in 500 consecutive patients who underwent CTs of the brain or paranasal sinuses. They showed that these findings included spur or ossicle formation and joint space obliteration that were similar to findings in the other synovial joints. Although postero-anterior, lateral, and/or oblique radiographies are primarily used for the radiological diagnosis, these images may be inconclusive due to overlaying bony structures, as in the presented case. On CT, osseous abnormalities of the atlantoaxial joint are better visualized than on plain radiographs. MR imaging is more valuable for determination of hypertrophic changes on the atlantodental joint and grading of the subtype of this disorder. Atlantodental joint and adjacent ligaments with the dens axis and their relationship with the neural structures within the foramen magnum may be clearly visualized on MR images. MR imaging may also exclude the inflammatory diseases, such as RA [8].
Surgical treatment of the hypertrophic dens involves a transorally dens resection. Resection of the dens should be performed with posterior occipital fusion because C1/C2 instability will occur due to failure of the transverse atlantal ligament [9].
In conclusion, patients suspected to have AAS should be carefully examined for occult AAS on flexion and extension roentgenograms, and it should be remembered that these patients may present with prominent medullary compression symptoms in the future. For that reason, inconclusive cases should be evaluated with craniocervical junction MRI, on suitable patients.
Footnotes
Conflict interest statement The authors declare that they have no conflict of interest to the publication of this article.
References
- 1.Okada K, Sato K, Abe E. Hypertrophic dens resulting in cervical myelopathy: histologic features of the hypertrophic dens. Spine. 2000;21:1303–7. doi: 10.1097/00007632-200005150-00020. [DOI] [PubMed] [Google Scholar]
- 2.Sato K, Senma S, Abe E, et al. Myelopathy resulting from the atlantodental hypertrophic osteoarthritis accompanying the dens hypertrophy. Two case reports. Spine. 1996;21:1467–71. doi: 10.1097/00007632-199606150-00013. [DOI] [PubMed] [Google Scholar]
- 3.Lansen TA, Kasoff SS, Tenner MS. Occipitocervical fusion for reduction of traumatic periodontoid hypertrophic cicatrix. J Neurosurg. 1990;73:466–70. doi: 10.3171/jns.1990.73.3.0466. [DOI] [PubMed] [Google Scholar]
- 4.Sze G, Brant-Zawadzki MN, Wilson CR, Norman D, Newton TH. Pseudotumour of the craniovertebral junction associated with chronic subluxation: MR imaging studies. Radiology. 1986;161:392–4. doi: 10.1148/radiology.161.2.3763907. [DOI] [PubMed] [Google Scholar]
- 5.Holt RG, Helms CA, Munk PL, Gillespy T. Hypertrophic C-1 anterior arch: Useful sign to distinguish os odontoideum from acute dens fracture. Radiology. 1989;173:207–9. doi: 10.1148/radiology.173.1.2781009. [DOI] [PubMed] [Google Scholar]
- 6.Dickinson LD, Papadopoulos SM, Hoff JT. Neurogenic hypertension related to basilar impression. Case report. J Neurosurg. 1993;79:924–8. doi: 10.3171/jns.1993.79.6.0924. [DOI] [PubMed] [Google Scholar]
- 7.Zapletal J, Hekster RE, Straver JS, Wilmik JT. Atlantoodontoid osteoarthritis: Appearance and prevalence at computed tomography. Spine. 1995;20:49–53. [PubMed] [Google Scholar]
- 8.Prokesch RW, Chocholka P, Bader TW, Ba-Ssalamah A, Trattnig S. Dolichoodontoid. A rare cranio-cervical anomaly--MRI findings. Eur J Radiol. 2000;33:38–40. doi: 10.1016/s0720-048x(99)00072-8. [DOI] [PubMed] [Google Scholar]
- 9.McAfee PC, Bohlman HH, Ducker TB, Zeidman SM, Goldstein JA. One-stage anterior cervical decompression and posterior stabilization. A study of one hundred patients with a minimum of two years of follow-up. J Bone Joint Surg Am. 1995;77:1791–800. doi: 10.2106/00004623-199512000-00001. [DOI] [PubMed] [Google Scholar]


