Abstract
Parent involvement in prevention efforts targeting adolescents increases the impact of such programs. However, the majority of risk-reduction intervention programs that are implemented through schools do not include parents, in part because most existing parental interventions require significant time commitment by parents. We designed a brief parent-adolescent sexual risk communication intervention to be delivered with an effective HIV prevention intervention as part of a randomized, controlled trial among 2564 grade 10 students and their parents in The Bahamas. Mixed effects modeling analysis was conducted to evaluate the effect of the brief parent-adolescent communication intervention using four waves of longitudinal data. Results indicate that a brief parent-adolescent communication intervention is effective in improving parent-adolescent communication on sex-related issues and perceived parental monitoring as well as the youth's condom use skills and self-efficacy. There is a marginal effect on consistent condom use. In addition, there is an apparent dose effect of the brief parent intervention on perceived parent-adolescent sexual risk communication and adolescent outcomes. These findings suggest that adolescent risk reduction interventions should include a brief parent-adolescent communication intervention which should be reinforced by periodic boosters in order to enhance the impact of adolescent HIV prevention programs.
Keywords: adolescent, condom use skills, self-efficacy, parent-adolescent communication, brief parental intervention, risk behaviors, The Bahamas
Introduction
Adolescent behavior is influenced by family, peers, school, neighborhood, and the broader socio-cultural context (Bronfenbrenner, 1979; Jackson, Henderson, Frank, & Haw, 2012), with family being especially influential (Perrino, González-Soldevilla, Pantin, & Szapocznik, 2000). Parents are positioned to assume a central role in protecting against adolescent involvement in risk behaviors (Mayberry, 2011; Willoughby & Hamza, 2011). Parents may exert their influence on adolescent risk behaviors through different pathways including parent-adolescent communication and parental monitoring (Deptula, Henry, & Schoeny, 2010; Hutchinson, Jemmott, Jemmott, Braverman, & Fong, 2003). Studies have shown that parent-adolescent communication about sexual behavior (especially communication before the onset of youth sexual activity) promotes healthy sexual decision-making and decreases adolescent involvement in sexual risk behaviors (Atienzo, Walker, Campero, Lamadrid-Figueroa, & Gutiérrez, 2009; Buzi, Smith, & Weinman, 2009). Less frequent parent-adolescent communication has been associated with adolescents’ non-use of contraceptives and lower self-efficacy to negotiate safer sex (DiClemente at al., 2001). As well, increases in positive parent-adolescent communication negatively predict adolescent cigarette smoking and binge drinking (Schwartz et al. 2012). Problematic parent-adolescent communication has consistently been associated with increases in a wide range of adolescent risk behaviors (including delinquency, substance use and sexual risk behaviors) (Wang et al., 2013). Healthy parent-adolescent communication provides an environment in which adolescents feel comfortable sharing information about their activities with their parents (Kopko & Dunifon, 2010), which in turn enhances parental monitoring. Effective parental monitoring and supervision prevent adolescent association with deviant peers (Sieverding, Adler, Witt, & Ellen, 2005; Van Ryzin, Fosco, & Dishion, 2012) and reduce adolescent involvement in risk behaviors (Stanton et al., 2004; Véronneau & Dishion, 2010).
Given the prominent impact of parents on adolescent behavior, numerous family interventions have been designed and implemented with a focus on improving parent-adolescent communication and parental monitoring to reduce adolescent risk behaviors. Family-based interventions have generally shown positive effects on improved parent-adolescent communication and reduction of adolescent risk behaviors. For example, at 22 months post-intervention, adolescents participating in the Strong African American Families-Teen (SAAF-T) program exhibited lower rates of conduct problems, substance use, and depressive symptoms (Brody et al., 2011). A family intervention targeting high-risk Hispanic adolescents (“Familias Unidas”) was found to increase parent-adolescent communication and adolescent condom use, and to reduce the number of adolescent sexual partners (Prado et al., 2012). A recent systematic review found that family interventions which focused on the parenting skills of adolescents’ parents and caregivers were effective in reducing adolescent risk behaviors and improving adolescent health (Burrus et al., 2012). Another parent-adolescent intervention study reported that parental participation in a sexual risk communication intervention increases general communication, sexual risk communication and comfort with communication among parents and youth (Villarruel, Cherry, Cabriales, Ronis, & Zhou, 2008). A combined family-based substance abuse and HIV prevention intervention conducted in Bangkok, Thailand (“Thai Family Matters”) found that the intervention increased the frequency of general parent-child communication but had only a marginal impact on the frequency of parent-youth communication about sexual issues (Cupp et al., 2013). However, a second systematic review summarizing twelve parent-adolescent communication interventions found that these interventions improved the frequency and content of discussion about sex between parents and their adolescents, but had no effect on youth outcome expectations (related to not having sex) (Akers, Holland, & Bost, 2011).
Most existing family-based interventions are of considerable length and involve face-to-face facilitated formats which require significant time commitment by parents (Akers et al., 2010). The Strong African American Families (SAAF) program consists of seven consecutive weekly meetings, each including separate and concurrent training sessions for parents and children, followed by a joint parent-child practice session; parents and youths receive 14 hours of prevention training (Murry et al., 2011). The Familias Unidas intervention includes eight parent-centered 2-hour group sessions and four 1-hour family visits (which involves both parents and youths) (Prado et al., 2012). The parent-adolescent intervention designed by Villarruel and colleagues (2008) consists of six 1-hour modules for parents and adolescents implemented on two consecutive Saturdays by specially trained adult facilitators. The Thai family Matters intervention provides parents with a series of five booklets and health educators contact the parents weekly for ten weeks to discuss the exercises within the booklets (Cupp et al., 2013). Although these family interventions appear to have a positive impact on youth outcomes, they may be difficult to deliver across a wide community because of the substantial time and resources required by staff and involved parents and children.
In response to the evidence for the potential role parents can play in risk reduction interventions and the desire to make such interventions less time- and labour-intensive, we designed and evaluated a brief intervention for dyads of parents and early-mid adolescents in the USA [Informed Parents and Children Together (ImPACT)]. ImPACT consists of a 20 minute video emphasizing the importance of parent-adolescent communication, parental monitoring and safer sex practices. The video addresses the following points through real-life examples: 1) Children are uncomfortable talking about sex to their parents; 2) Parents find it difficult to talk to their children about sex; 3) Parents should talk to their children about sex before they become sexually active; 4) Choose a good time to talk with your children about difficult subjects; 5) Parents need to be informed about HIV/AIDS in order to talk with their children about it, including knowledge about how to use a condom; 6) Parents should “monitor” their teens: parents should know where their teens are, with whom they are and what they are doing; 7) Parents need to know how to use a condom; 8) Condoms are the best protection available against HIV for those who are sexually active; and, 9) Parents should talk directly with children about their values regarding sex and relationships. The video is followed by a review of communication pointers for parents and adolescents and a condom demonstration. The parent and child engage in a discussion and play-acting to improve communication about difficult subjects and situations. The session concludes with the youth and parent participating in a condom race to underscore the correct use of condoms. Evaluations found that the parent-child communication alone (e.g., ImPACT) increased communication but did not reduce risk behavior; however, when ImPACT was delivered in combination with an evidence-based effective sexual risk reduction intervention [“Focus on Youth” (FOY)] (Stanton et al., 1996), the combined parent-youth intervention was more effective than FOY alone (Wu et al., 2003; Stanton et al., 2004).
Subsequently both FOY and ImPACT were adapted for use among Bahamian pre-early adolescents (grade six students) and their parents: Focus on Youth in the Caribbean (FOYC) and, Caribbean ImPACT (CImPACT). Similar to our earlier experience with FOY in the USA, evaluations among the grade six Bahamian students indicate that FOYC plus CImPACT was more effective that FOYC alone or FOYC plus a parenting goal-setting intervention [Goal For It (GFI)] in improving youth's preventive knowledge and skill, perceptions, and condom use intention (Chen et al., 2009; Gong et al., 2009). (The GFI parent intervention is also a 22 minute video which is delivered to parents regarding setting goals for career development, whether their own careers or long-term planning for their youth). CImPACT was delivered to the parent with, if possible, the youth (each parent received a copy of the video) while GFI was delivered to the parent (each parent received a copy of the video) with or without the youth. Both were delivered in the evenings or weekends at the youth's school. Thus CImPACT demonstrated additional protective effects among pre- and early adolescents; however, the effects of this brief parent intervention component among older adolescents (high school) have not been explored in either the USA or The Bahamas.
In response, the research team, including the Bahamian Ministries of Education and of Health, adapted FOYC and CImPACT for use among grade 10 students [e.g., Bahamian Focus on Older Youth (BFOOY) plus CImPACT] and conducted a randomized controlled trial of the interventions among 2,564 Grade 10 youth and their parents beginning in 2008. Results at six, 12 and 18 months follow-up described elsewhere (Dinaj-Koci et al., 2014; Stanton et al., submitted) indicate that BFOOY is an effective sexual risk-reduction intervention. This present analyses offer the unique opportunity to examine whether (and if so how) a brief parent-adolescent sexual risk communication intervention in addition to an effective adolescent intervention would confer added benefit among older adolescents who are gradually engaging in more risky behaviors. The analyses presented herein address the following questions about a parent-adolescent communication intervention: 1) Will parents of older youth (mid/late adolescence) participate in such an intervention?; 2) Will such an intervention result in improved parent-adolescent communication among high-school age students?; 3) Will such an intervention result in improved outcomes among the adolescents (including condom use skill, self-efficacy and risk behaviors)?; and, 4) Is there a dosage effect of the intervention?
Methods
Study site
The Bahamas has one of the highest HIV adult prevalence rate (2.8%) in the Caribbean (UNAIDS, 2012). AIDS is the leading cause of death among adults 15 to 49 years of age. The primary route of HIV transmission is heterosexual contact (approximately 87%). Sixty-five percent of the entire Bahamian population and 86% of individuals infected with HIV live on the island of New Providence (Bahamian Ministry of Health, 2006).
Participants
The research protocol, including the questionnaires, was approved by the institutional review boards at Wayne State University and The Princess Margaret Hospital in The Bahamas. All eight of the government high schools (grade 10 through 12) in New Providence participated in this study. Parents and students were informed that participation was voluntary, and their answers were confidential. Written youth assent and parent consent were required for youth participation in the study. Parents who consented for their youth to participate were eligible to participate in the parent intervention component of the study. Among the 2564 students who enrolled in the study (about two-thirds of all grade 10 students in the eight participating high schools), 1833(71.5%) parents participated in the parent intervention component. Each student and parent was given a voucher worth $10 Bahamian after completing each assessment. Longitudinal data were obtained from four surveys of the youth [a baseline survey (Time 1) and three follow-up surveys conducted at six (Time 2), 12 (Time 3) and 18 (Time 4) months after the intervention]. The follow-up rate was 84% at six months, 78.6% at 12 months, and 77.7% at 18 months post-intervention. The mean age of youth at baseline was 14.5 years (range 13 to 17 years). Ninety-nine percent of youth were of African descent.
Intervention Components
Randomization occurred at the level of the class, through which students were assigned to one of two study conditions and their parents were involved in one of three study conditions. For youth, the control condition was the existing Bahamian Health and Family Life Education (HFLE) Curriculum, which focuses on a range of health topics, including a factual presentation of HIV and pregnancy prevention and discussions about marriage and parenting. The youth experimental condition was BFOOY, an age-appropriate adolescent risk reduction program based on a social cognitive model, Protection Motivation Theory (Rodgers 1983). BFOOY contains ten-sessions which include interactive discussions, role-plays, games and homework exercises to reinforce main messages and increase knowledge and skills regarding risk avoidance. An ongoing story throughout the sessions focuses on a fictional family story to contextualize decision-making and the importance of carefully considering long-term consequences of actions (Deveaux et al., 2007). A decision-making model (Stop/Options/Decision/Action) is emphasized throughout BFOOY to provide guidance and practice in consequential thinking and action. Multiple exercises in communication emphasize effective delivery of a message and the need to listen.
The youth's parents were randomized to receive the parent-adolescent sexual risk communication intervention (CImPACT), or the goal-setting intervention (GFI) described earlier in this manuscript, or no intervention.
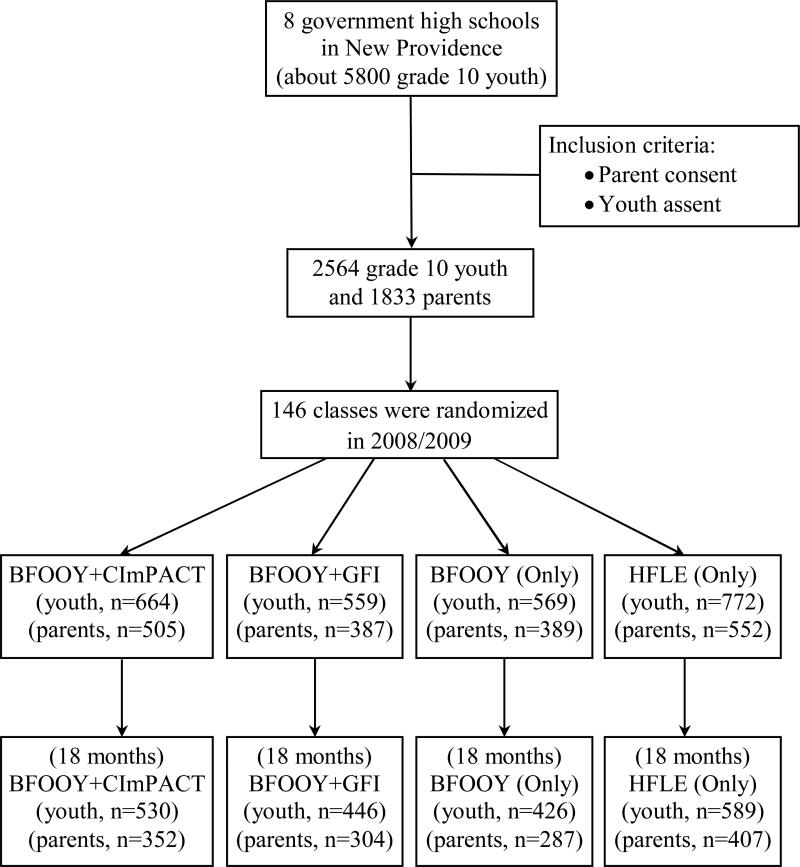
The combination of the two youth study conditions (BFOOY and HFLE) and the three parent conditions (CImPACT, GFI and no-intervention) resulted in four youth study conditions randomized at the level of the classroom: BFOOY+CImPACT; BFOOY+GFI; BFOOY (Only); and HFLE (Only) (See Figure 1).
Figure 1.
Flowchart for 2008/2009 randomized, controlled trial of Bahamian Focus on Older Youth (BFOOY)
Data collection procedures
Data were collected using the Bahamian Youth Health Risk Behavioral Inventory (BYHRBI), a paper-and-pencil questionnaire administered in the classroom setting (Deveaux et al., 2007). Students completed self-administered questionnaires in their classrooms, which required approximately 45 minutes to complete. Teachers were required to leave the classroom while the assessments were completed. Parents completed questionnaires in the evenings which took about 20 minutes to complete. At the completion of the questionnaire, parents received one of the two interventions (CImPACT or GFI) or no intervention. Trained personnel provided explanations and instructions for completing the surveys. Regardless of intervention assignment, all parents were asked to complete questionnaires at baseline, and at six and 12 months follow-up.
Measures
Condom use skills
Condom use skills were assessed using the Condom use Skills Checklist (Stanton et al., 2009). The validated scale includes 16 true and false statements describing the detailed steps of condom use from opening a condom pack for use to disposal after use (e.g., “unroll condom before placing on the penis”). The internal consistency estimate (Cronbach's alpha) of these items was 0.56. Correct responses were scored 1 and incorrect 0, resulting in a summary score of 1 to 16 for each participant.
Condom use self-efficacy
A six-item scale was used to assess condom use self-efficacy (e.g., “I could put a condom on correctly”). Agreement was measured through a five-point Likert scale (1=strongly disagree to 5=strongly agree). The internal consistency estimate of the scale was 0.81. A composite score was calculated as a mean score across the six items (range 1 to 5).
Parental monitoring
A validated eight-item parental monitoring scale (Small & Kerns, 1993) was employed to assess youth perceptions of parents’ knowledge about their whereabouts and parents’ monitoring efforts. Sample items included “my parents/guardian know where I am after school” and “when I go out, my parents/guardian tell me what time I’m to return.” Responses to these items were based on a five-point Likert scale (1=never to 5=always). The internal consistency of the scale was 0.85. Individual items were averaged to yield a composite score of 1 to 5.
Parent-adolescent communication about sex
The questionnaire contains eight items assessing the level of communication between parents and their adolescent children about sex-related issues. Adolescents were asked how much information their parents gave them about topics including birth control, sexually transmitted diseases, HIV/AIDS, condoms, how to protect themselves from HIV and AIDS, postponing or not having sex, peer pressure to have sex and how to handle sexual pressure. Responses to these items were based on a five-point Likert scale (1=none to 5=extensive). The internal consistency of the scale was 0.89. Individual items were averaged to yield a composite score of 1 to 5.
Adolescent sexual risk behavior
Youth were asked two questions to assess sexual behavior and condom use: Had they engaged in sexual intercourse during the last six months (yes/no); and, how often had they used a condom when they had sex (always, sometimes or never).
Analysis
Baseline equivalence and attrition to follow-ups between groups were examined using the chi-square test for categorical variables and analyses of variance (ANOVA) for continuous variables. In evaluating overall effect of the interventions, bivariate analyses (ANOVA and chi-square test) were first used to examine the difference in youth's perception of parent-adolescent communication about sexual risk behaviour and parental monitoring, youth's condom use skills and perceived self-efficacy in condom use, and sexual behaviour including condom use among the three intervention and one control groups at each assessment (i.e., baseline, 6 months, 12 months, and 18 months post-intervention). The change over time in perceived parental monitoring and sexual risk communication as well as youth's condom use skills and self-efficacy within each group was examined using repeated measures ANOVA. To examine whether there was a dose effect of the brief parental intervention, we narrowed the analysis to those youth whose parents were assigned to receive CImPACT or GFI; perceived parent-adolescent communication and parental monitoring and adolescent outcomes were compared at each time according to level of parental participation of CImPACT (i.e., parents who did not attend any session, parents who attended one or two sessions, and parents who attended all three sessions). Parents who participated in one or two sessions were combined because of their low frequency in the one-session category and the absence of a significant difference in changes in student outcomes between the two groups
The effect of the intervention on parent-adolescent sexual risk communication, parental monitoring and adolescent outcomes was further assessed using mixed effects models, controlling for the dependence of repeated measures and the clustering effects of school and classroom (students clustered within classes in eight high schools). As the focus of this evaluation is the impact of the brief parental intervention, the adolescent risk reduction intervention group “BFOOY (Only)” was used as the control to rule out the effect of the youth-focused intervention in the mixed models. Independent variables included age, sex, level of parental participation, intervention group assignment, time (baseline, six, 12, and 18 months follow-up). Mixed effects models also included interaction between BFOOY+CImPACT (or BFOOY+GFI) and time. Regression coefficients were calculated for each independent variable. All statistical analyses were performed using the SAS 9.3 statistical software package (SAS Institute Inc., Cary, NC, USA). A significance level of 0.05 was adopted in bivariate and multivariate analyses.
Results
1) Baseline equivalence and parent participation in the intervention
A total of 2,564 youth (1447 females, 56.4%) in grade 10 enrolled at baseline; 1792 were randomized at the level of the classroom (n=101) to one of the three BFOOY conditions [BFOOY+CImPACT, BFOOY+GFI, and BFOOY (Only)] and 772 to the control condition [HFLE (Only)]. The mean ages of youth in the intervention and control groups were 14.5 at baseline. The four groups did not differ with regard to age and sex distributions.
Of the 664 youth randomized to BFOOY+CImPACT, 76% of their parents attended the first evening intervention session (i.e., CImPACT); 45% and 53% attended the first and second “booster” sessions (e.g., the six and 12 month follow-ups, respectively). Among the 559 youth in BFOOY+GFI, 69% of their parents attended the first evening intervention session (i.e., GFI); 46% attended the six months “booster session”, and 54% completed the 12 months follow-up questionnaires (there was no “booster” session at 12 months for GFI). Approximately 38% of parents attended all three CImPACT sessions and 41% of parents attended all three GFI sessions. The parent attendance rates were not significantly different between the two groups except the baseline attendance rate was higher among parents in BFOOY+CImPACT (76% vs. 69.2%, t= 7.16, p<0.01). Among the 569 youth in BFOOY (Only), 68.4%, 44.1% and 50.4% of their parents attended the baseline, six months and 12 months assessments, respectively. Of the 772 youth in HFLE (Only) group, 71.5%, 49.4% and 52.7% of their parents attended the baseline, six months and 12 months assessments, respectively. About 37% and 41.6% of parents in BFOOY (Only) and HFLE (Only) groups attended all three assessments.
2) Overall program effects
Table 1 depicts the change in condom use skills and perceived condom use self-efficacy, parent-adolescent communication, and parental monitoring over 18 months post-intervention according to intervention group assignment. Condom use skills were higher among youth in the BFOOY (Only) group than in the HFLE (Only) group, while self-efficacy was comparable among the four groups at baseline. Condom use skills and self-efficacy increased significantly among all groups over the 18 months follow-up. At six months post-intervention, condom use skills were significantly higher among all three BFOOY groups compared to HFLE (Only) (F=18.77, P<0.0001). At the 12 months and 18 months follow-ups, condom use skills were highest in the BFOOY+CImPACT group, followed by BFOOY+GFI and BFOOY (Only), with the HFLE (Only) group demonstrating the lowest skills (F=15.85, P<0.001 for 12 months; F=18.87, P<0.001 for 18 months). At the 12 months follow-up, condom use self-efficacy was significantly higher among the BFOOY+CImPACT youth compared to those in the HFLE (Only) and BFOOY+GFI groups (F=3.47, P<0.05).
Table 1.
Condom use skills, and perceived self-efficacy, parent-adolescent sexual risk communication and parental monitoring among youth in the four intervention and control groups over 18 months observation
| Variables | Overall | Intervention groups |
F | Post-hoc | |||
|---|---|---|---|---|---|---|---|
| HFLE (Only) (1) | BFOOY+CImPACT (2) | BFOOY+GFI (3) | BFOOY (Only) (4) | ||||
| Condom use skills | (2,564) | (772) | (664) | (559) | (569) | ||
| Baseline | 10.4(2.2) | 10.3(2.2) | 10.5(2.1) | 10.5(2.2) | 10.6(2.1) | 3.49* | (1,4) |
| 6-month follow-up | 11.5(2.3) | 10.9(2.2) | 11.9(2.4) | 11.5(2.3) | 11.6(2.0) | 18.77*** | (1,2) (1,3) (1,4) |
| 12-month follow-up | 11.7(2.2) | 11.2(2.3) | 12.2(2.2) | 11.7(2.2) | 11.8(2.2) | 15.85*** | (1,2) (1,3) (1,4) (2,3) (2,4) |
| 18-month follow-up | 11.7(2.3) | 11.3(2.2) | 12.3(2.1) | 11.7(2.4) | 11.7(2.2) | 18.87*** | (1,2) (1,3) (1,4) (2,3) (2,4) |
| Increase (18-month-baseline) | 1.2(2.5) | 1.0(2.5) | 1.7(2.5) | 1.2(2.5) | 1.0(2.6) | 9.24*** | (1,2) (2,3) (2,4) |
| Self-efficacy | |||||||
| Baseline | 3.9(1.1) | 3.9(1.1) | 3.9(1.2) | 3.8(1.2) | 4.0(1.1) | 1.49 | |
| 6-month follow-up | 4.2(0.9) | 4.2(1.0) | 4.3(0.8) | 4.3(0.9) | 4.2(1.0) | 1.19 | |
| 12-month follow-up | 4.4(0.8) | 4.3(0.8) | 4.5(0.7) | 4.3(0.8) | 4.3(0.8) | 3.47* | (1,2) (2,3) |
| 18-month follow-up | 4.4(0.8) | 4.4(0.8) | 4.5(0.7) | 4.4(0.8) | 4.4(0.8) | 2.11 | |
| Increase (18-month-baseline) | 0.5(1.1) | 0.5(1.1) | 0.6(1.1) | 0.5(1.2) | 0.4(1.0) | 0.95 | |
| Communication | |||||||
| Baseline | 2.7(1.2) | 2.7(1.2) | 2.7(1.2) | 2.7(1.2) | 2.7(1.2) | 0.39 | |
| 6-month follow-up | 2.7(1.2) | 2.6(1.2) | 2.8(1.2) | 2.7(1.2) | 2.6(1.3) | 1.89 | |
| 12-month follow-up | 2.7(1.2) | 2.7(1.2) | 2.8(1.2) | 2.6(1.2) | 2.5(1.2) | 3.59* | (1,4) (2,4) |
| 18-month follow-up | 2.7(1.3) | 2.6(1.2) | 2.8(1.3) | 2.6(1.3) | 2.6(1.2) | 3.81** | (1,2) (2,4) |
| Increase (18-month-baseline) | 0.0(1.2) | 0.0(1.2) | 0.2(1.3) | −0.1(1.2) | −0.1(1.2) | 3.90** | (2,3) (2,4) |
| Parental monitoring | |||||||
| Baseline | 4.2(0.8) | 4.2(0.7) | 4.2(0.8) | 4.2(0.8) | 4.2(0.8) | 0.76 | |
| 6-month follow-up | 4.2(0.8) | 4.2(0.7) | 4.2(0.8) | 4.2(0.7) | 4.1(0.8) | 0.49 | |
| 12-month follow-up | 4.1(0.8) | 4.2(0.8) | 4.2(0.8) | 4.1(0.8) | 4.1(0.8) | 2.11 | |
| 18-month follow-up | 4.1(0.8) | 4.1(0.8) | 4.2(0.8) | 4.2(0.8) | 4.0(0.9) | 2.65* | (2,4) |
| Increase (18-month-baseline) | −0.1(0.8) | −0.1(0.8) | −0.1(0.7) | −0.1(0.8) | −0.2(0.8) | 1.32 | |
Note: BFOOY= Bahamian Focus on Older Youth; CImPACT= Caribbean Informed Parents and Children Together; GFI=Goal for It; HFLE=Bahamian Health and Family Life Education. BFOOY+CImPACT represents youth assigned to the adolescent sexual risk reduction intervention whose parents were assigned to the communication/sexual risk reduction intervention; BFOOY+GFI represents youth assigned to the adolescent sexual risk reduction intervention whose parents were assigned to the goal-setting intervention; BFOOY (only) represents youth assigned to the adolescent sexual risk reduction intervention whose parents did not receive an intervention; HFLE represents youth who received the school's standard of care and their parents received no intervention.
P<0.05
P<0.01
P<0.001.
Perceived parent-adolescent sexual risk communication and parental monitoring were comparable among the four groups at baseline. Parent-adolescent communication was relatively stable over time while parental monitoring decreased significantly among all groups over the 18 months follow-up. At the 12 months and 18 months follow-ups, parent-adolescent communication about sexual issues was higher in the BFOOY+CImPACT group compared to BFOOY (Only) and HFLE (Only) (F=3.59, P<0.05 for 12 months; F=3.81, P<0.01 for 18 months) and parental monitoring was significantly higher in the BFOOY+CImPACT group compared to BFOOY (Only) at 18 months (F=2.65, P<0.05).
3) Dose effects of CImPACT
Tables 2 and 3 depict the changes in youth condom use skills, and perceived self-efficacy, parent-adolescent sexual-risk communication and parental monitoring over 18 months post-intervention according to level of parental participation in the intervention. For youth in the BFOOY+CImPACT group, all four outcomes were comparable at baseline among youth according to parental participation in CImPACT (e.g., parents did not attend any CImPACT session, parents attended one or two sessions, and parents attended all three sessions). At six months and 12 months post-intervention, condom use skills were significantly higher among youth whose parents attended all three CImPACT sessions compared to youths whose parents did not attend any session (12.2 vs. 11.8 vs. 11.3, F=5.63, P<0.01 at six months; 12.4 vs. 12.0 vs. 11.9 at 12 months, F=3.07, p<0.05). Condom use skills at 18 months follow-up were the highest among youths whose parents attended all three CImPACT sessions, followed by youth whose parents attended once or twice, with youth whose parents did not attend CImPACT demonstrating the lowest skills (12.7 vs. 12.2 vs. 11.5, F=12.67, P<0.001). At 18 months post-intervention, self-efficacy was significantly higher among youth whose parents attended all three CImPACT sessions compared to youths whose parents did not attend any session (4.58 vs. 4.49 vs. 4.27, F=7.77, P<0.001). At 12 months and 18 months post-intervention, parent-adolescent communication was significantly higher among youth whose parents attended all three CImPACT sessions compared to youths whose parents did not attend any session or attended only one or two sessions (2.89 vs. 2.58 vs. 2.67 at 12 months, F=3.04, P<0.05; 3.09 vs. 2.67 vs. 2.61 at 18 months, F=8.23, p<0.001). There was no significant difference in youth perception of parental monitoring at six, 12 and 18 months post-intervention according to parental participation in CImPACT. However, parental monitoring was relatively stable among youth whose parents attended all three CImPACT sessions while it decreased significantly among youths whose parents did not attend any session or attended only one or two sessions over the 18 months follow-up.
Table 2.
Change in adolescents' condom use skills and perceived self-efficacy by level of parental participation in two parental interventions (CImPACT or GFI)
| Variables | Level of parent participation (BFOOY+CImPACT) |
Level of parent participation (BFOOY+GFI) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | 1 | 2 | 3 | 2+3 | F | t | Overall | 1 | 2 | 3 | 2+3 | F | t | |
| Condom use skills | 664 | 159 | 254 | 251 | 559 | 172 | 156 | 231 | ||||||
| Baseline | 10.5 (2.1) | 10.4 (2.1) | 10.5 (2.2) | 10.5 (2.1) | 10.5 (2.1) | 0.18 | 0.47 | 10.5 (2.2) | 10.6 (2.1) | 10.3 (2.3) | 10.5 (2.2) | 10.5 (2.3) | 0.59 | 0.52 |
| 6-month follow-up | 11.9 (2.4) | 11.3 (2.4) | 11.8 (2.5) | 12.2 (2.1) | 12.0 (2.3) | 5.63** | 2.85** | 11.5 (2.3) | 11.3 (2.2) | 11.1 (2.2) | 11.9 (2.4) | 11.6 (2.4) | 4.87** | 1.11 |
| 12-month follow-up | 12.2 (2.2) | 11.9 (2.0) | 12.0 (2.3) | 12.4 (2.1) | 12.2 (2.2) | 3.07* | 1.22 | 11.7 (2.2) | 11.6 (2.0) | 11.4 (2.2) | 11.9 (2.3) | 11.7 (2.3) | 1.80 | 0.56 |
| 18-month follow-up | 12.3 (2.1) | 11.5 (2.2) | 12.2 (2.1) | 12.7 (2.0) | 12.5 (2.1) | 12.67*** | 4.32*** | 11.7 (2.4) | 11.6 (2.1) | 11.4 (2.5) | 11.9 (2.4) | 11.7 (2.5) | 2.21 | 0.63 |
| Increase (18-month-baseline) | 1.7 (2.5) | 0.9 (2.5) | 1.7 (2.3) | 2.1 (2.5) | 1.9 (2.4) | 9.46*** | 3.98*** | 1.2 (2.5) | 1.0 (2.4) | 1.0 (2.9) | 1.5 (2.3) | 1.3 (2.5) | 2.10 | 1.07 |
| Condom use self-efficacy | ||||||||||||||
| Baseline | 3.9 (1.2) | 3.9 (1.2) | 3.9 (1.1) | 3.9 (1.1) | 3.9 (1.1) | 0.05 | 0.24 | 3.8 (1.2) | 3.8 (1.2) | 3.8 (1.2) | 3.9 (1.1) | 3.9 (1.2) | 1.29 | 1.06 |
| 6-month follow-up | 4.3 (0.8) | 4.2 (0.9) | 4.3 (0.8) | 4.3 (0.8) | 4.3 (0.8) | 0.79 | 1.15 | 4.3 (0.9) | 4.2 (1.1) | 4.3 (0.9) | 4.3 (0.9) | 4.3 (0.9) | 0.56 | 0.90 |
| 12-month follow-up | 4.5 (0.68) | 4.4 (0.76) | 4.4 (0.71) | 4.5 (0.60) | 4.5 (0.65) | 2.49 | 0.80 | 4.3 (0.9) | 4.3 (0.8) | 4.3 (0.9) | 4.3 (0.8) | 4.3 (0.9) | 0.12 | 0.23 |
| 18-month follow-up | 4.5 (0.7) | 4.3 (1.0) | 4.5 (0.6) | 4.6 (0.6) | 4.5 (0.6) | 7.77*** | 2.79** | 4.4 (0.8) | 4.3 (0.9) | 4.4 (0.8) | 4.4 (0.8) | 4.4 (0.8) | 0.26 | 0.71 |
| Increase (18-month-baseline) | 0.6 (1.1) | 0.4 (1.2) | 0.6 (1.1) | 0.7 (1.1) | 0.6 (1.1) | 1.85 | 1.76 | 0.5 (1.2) | 0.5 (1.2) | 0.6 (1.2) | 0.5 (1.1) | 0.5 (1.2) | 0.20 | 0.09 |
Note: Level of parental participation: 1=no participation; 2=participated 1 or 2 sessions; 3=parent participated in all three CImPACT sessions. F test was used to compare three group means (Group 1, 2 and 3); t test was used to compare two group means (group 1 vs. group 2+3). BFOOY= Bahamian Focus on Older Youth; CImPACT= Caribbean Informed Parents and Children Together; GFI=Goal for It; BFOOY+CImPACT represents youth assigned to the adolescent sexual risk reduction intervention whose parents were assigned to the communication/sexual risk reduction intervention; BFOOY+GFI represents youth assigned to the adolescent sexual risk reduction intervention whose parents were assigned to the goal-setting intervention.
Table 3.
Change in perceived parent-adolescent sexual risk communication and parental monitoring by level of parental participation in two parental interventions (CImPACT and GFI)
| Variables | Level of parent participation (BFOOY+CImPACT) |
Level of parent participation (BFOOY+GFI) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | 1 | 2 | 3 | 2+3 | F | t | Overall | 1 | 2 | 3 | 2+3 | F | t | |
| Parent-adolescent communication | 664 | 159 | 254 | 251 | 559 | 172 | 156 | 231 | ||||||
| Baseline | 2.7 (1.2) | 2.7 (1.3) | 2.6 (1.2) | 2.7 (1.2) | 2.7 (1.2) | 1.05 | 0.00 | 2.7 (1.2) | 2.7 (1.1) | 2.8 (1.2) | 2.7 (1.2) | 2.8 (1.2) | 0.46 | 0.90 |
| 6-month follow-up | 2.8 (1.2) | 2.7 (1.2) | 2.7 (1.2) | 2.8 (1.3) | 2.8 (1.3) | 0.52 | 0.51 | 2.7 (1.2) | 2.6 (1.2) | 2.8 (1.2) | 2.7 (1.2) | 2.7 (1.2) | 0.59 | 0.85 |
| 12-month follow-up | 2.8 (1.2) | 2.6 (1.2) | 2.7 (1.2) | 2.9 (1.2) | 2.8 (1.2) | 3.04* | 1.69 | 2.7 (1.2) | 2.6 (1.2) | 2.7 (1.2) | 2.7 (1.2) | 2.7 (1.2) | 0.10 | 0.39 |
| 18-month follow-up | 2.8 (1.3) | 2.7 (1.3) | 2.6 (1.3) | 3.1 (1.3) | 2.9 (1.3) | 8.23 | 1.48 | 2.6 (1.3) | 2.5 (1.3) | 2.6 (1.3) | 2.7 (1.3) | 2.7 (1.3) | 0.62 | 1.04 |
| Increase (18-month-baseline) | 0.1 (1.3) | −0.1 (1.3) | 0.0 (1.3) | 0.4 (1.4) | 0.2 (1.3) | 4.88** | 1.98* | −0.1 (1.2) | −0.2 (1.3) | −0.2 (1.1) | −0.0 (1.2) | −0.1 (1.2) | 0.90 | 0.87 |
| Parental monitoring | ||||||||||||||
| Baseline | 4.2 (0.8) | 4.2 (0.9) | 4.2 (0.8) | 4.3 (0.8) | 4.2 (0.8) | 0.91 | 1.18 | 4.2 (0.8) | 4.2 (0.9) | 4.1 (0.8) | 4.3 (0.8) | 4.2 (0.8) | 1.92 | 0.12 |
| 6-month follow-up | 4.2 (0.8) | 4.1 (0.9) | 4.2 (0.8) | 4.2 (0.8) | 4.2 (0.8) | 0.90 | 0.90 | 4.2 (0.7) | 4.1 (0.7) | 4.1 (0.9) | 4.3 (0.7) | 4.2 (0.8) | 1.51 | 0.95 |
| 12-month follow-up | 4.2 (0.77) | 4.1 (0.82) | 4.1 (0.75) | 4.2 (0.77) | 4.2 (0.76) | 0.69 | 0.50 | 4.1 (0.8) | 4.1 (0.8) | 4.2 (0.8) | 4.1 (0.8) | 4.1 (0.8) | 0.10 | 0.08 |
| 18-month follow-up | 4.2 (0.8) | 4.1 (0.9) | 4.2 (0.8) | 4.3 (0.7) | 4.2 (0.8) | 1.48 | 1.22 | 4.2 (0.8) | 4.1 (0.8) | 4.1 (0.9) | 4.2 (0.8) | 4.2 (0.8) | 0.56 | 0.79 |
| Increase (18-month-baseline) | −0.1 (0.7) | −0.2 (0.8) | −0.1 (0.7) | 0.0 (0.7) | −0.1 (0.7) | 0.81 | 0.87 | −0.1 (0.8) | − 0.3 (0.9) | −0.0 (0.8) | −0.1 (0.8) | −0.1 (0.8) | 2.85 | 2.14* |
Note: Level of parental participation: 1=no participation; 2=participated 1 or 2 sessions; 3=parent participated in all three CImPACT sessions. F test was used to compare three group means (Group 1, 2 and 3); t test was used to compare two group means (group 1 vs. group 2+3). BFOOY= Bahamian Focus on Older Youth; CImPACT= Caribbean Informed Parents and Children Together; GFI=Goal for It; BFOOY+CImPACT represents youth assigned to the adolescent sexual risk reduction intervention whose parents were assigned to the communication/sexual risk reduction intervention; BFOOY+GFI represents youth assigned to the adolescent sexual risk reduction intervention whose parents were assigned to the goal-setting intervention.
Among BFOOY+GFI youth, condom use skills were significantly higher at six months post-intervention among youth whose parents attended all three GFI sessions (e.g. the GFI intervention at baseline, booster at six months and 12 months assessment without any intervention) compared to youth whose parents did not attend any session or attended only one or two sessions (11.9 vs. 11.3 vs. 11.1, F=4.87, P<0.01). Condom use self-efficacy and perceived parent-adolescent sexual risk communication did not differ among youth according to parental participation in GFI. Parental monitoring remained relatively stable among youth whose parents attended at least one GFI session while it decreased significantly among youths whose parents did not attend any session over the 18 months period.
Among BFOOY (Only) and HFLE (Only) youth (e.g., parents did not receive any intervention), condom use skills, self-efficacy, perceived parent-adolescent sexual risk communication and parental monitoring did not differ among youth according to parental participation in the baseline, six months and 12 months assessments (i.e., parents did not complete any assessment, parents completed one or two assessments, and parents completed all three assessments) (data available upon request).
4) Mixed-effects models
Mixed-effects models were used to further examine the effects of the brief parent-adolescent communication intervention (CImPACT) or a attention control (GFI) on adolescents’ condom use skills, self-efficacy, parental monitoring, and parent-youth communication, controlling for age, gender, dependence of repeated measures and clustering effect of school/classroom (Tables 4 and 5). For each outcome variable, two mixed models were tested. The first set of mixed models (condom use skills-overall impact, self-efficacy-overall impact, communication-overall impact and monitoring-overall impact) defined the intervention group variable as the original group assignment [(BFOOY+CImPACT, BFOOY+GFI, and BFOOY (Only)] while in the second set of mixed models (condom use skills-dose effect, self-efficacy-dose effect, communication-dose effect and monitoring-dose effect) the BFOOY+CImPACT group were further divided into three categories: parent did not attend CImPACT, parent attended one or two sessions, and parent attended all three sessions (BFOOY+GFI group were divided into two categories: parents did not attend GFI or parent attended one or two sessions). The results of overall effect models indicate that youth assigned to the BFOOY+CImPACT group demonstrated higher levels of condom use skills, self-efficacy and parent-youth communication compared to youth in the BFOOY (Only) group; youth assigned to both BFOOY+CImPACT and BFOOY+GFI groups reported higher level of parental monitoring compared to BFOOY (Only) youth. The results of the four dose-effect models indicate that these intervention effects were significant only among youth whose parents had participated in all three sessions (except for condom use skills for which youth whose parents attended CImPACT one or two times also showed significant improvement).
Table 4.
Mixed models comparing youth curriculum with a parent intervention component (parent-youth sexual risk communication or parent-only goal setting) with youth curriculum only in condom use skills and self-efficacy
| Variables | Condom use skills | Condom use self-efficacy | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall effect | Dose effect | Overall effect | Dose effect | |||||||||
| β | SE | t | β | SE | t | β | SE | t | β | SE | t | |
| Fixed effect | ||||||||||||
| Intercept | 16.612 | 0.720 | 23.08*** | 16.546 | 0.720 | 22.99*** | 4.513 | 0.311 | 14.53*** | 4.488 | 0.311 | 14.43*** |
| Age | −0.357 | 0.049 | −7.26*** | −0.352 | 0.049 | −7.17*** | −0.020 | 0.021 | −0.92 | −0.018 | 0.021 | −0.84 |
| Gender [male vs. female (ref)] | 0.435 | 0.068 | 6.37*** | 0.434 | 0.068 | 6.37*** | 0.419 | 0.030 | 14.16*** | 0.419 | 0.030 | 14.14*** |
| Intervention groups | ||||||||||||
| BFOOY+CImPACT | 0.514 | 0.142 | 3.63*** | 0.080 | 0.058 | 1.37 | ||||||
| a) Parent did not participate | −0.203 | 0.226 | −0.89 | −0.123 | 0.093 | −1.32 | ||||||
| b) Participated once or twice | 0.441 | 0.189 | 2.34* | 0.078 | 0.078 | 0.99 | ||||||
| c) Participated three times | 0.944 | 0.179 | 5.28*** | 0.186 | 0.074 | 2.50* | ||||||
| BFOOY+GFI | 0.001 | 0.149 | 0.01 | −0.022 | 0.061 | −0.36 | ||||||
| d) Parent did not participate | −0.138 | 0.222 | −0.62 | −0.096 | 0.091 | −1.06 | ||||||
| e) Parent participated in GFI | 0.058 | 0.161 | 0.36 | 0.009 | 0.066 | 0.13 | ||||||
| HFLE | −0.336 | 0.143 | −2.36* | −0.335 | 0.142 | −2.35* | −0.016 | 0.057 | −0.28 | −0.016 | 0.057 | −0.28 |
| BFOOY only (ref) | ||||||||||||
| Time | ||||||||||||
| Baseline | −1.037 | 0.111 | −9.31*** | −1.037 | 0.111 | −9.32*** | −0.443 | 0.044 | −10.07*** | −0.444 | 0.044 | −10.08*** |
| 6-month follow-up | −0.157 | 0.116 | −1.35 | −0.157 | 0.116 | −1.35 | −0.164 | 0.045 | −3.60*** | −0.164 | 0.045 | −3.60*** |
| 12-month follow-up | 0.076 | 0.118 | 0.65 | 0.076 | 0.117 | 0.65 | −0.053 | 0.046 | −1.16 | −0.053 | 0.046 | −1.16 |
| 18-month follow-up (ref) | ||||||||||||
| GroupxTime | ||||||||||||
| BFOOY+CImPACTxTime | 0.203 | 0.048 | 4.20*** | 0.039 | 0.019 | 2.06* | ||||||
| BFOOY+CImPACT(b)×Time | 0.180 | 0.065 | 2.78** | 0.036 | 0.026 | 1.41 | ||||||
| BFOOY+CImPACT(c)×Time | 0.307 | 0.061 | 5.00*** | 0.070 | 0.024 | 2.91** | ||||||
| Random effect | ||||||||||||
| Class† | 0.057 | 0.028 | 2.03* | 0.054 | 0.027 | 2.01* | 0.001 | 0.002 | 0.85 | 0.001 | 0.002 | 0.82 |
| Student (nested within school)† | 1.898 | 0.081 | 23.57*** | 1.892 | 0.080 | 23.54*** | 0.393 | 0.016 | 25.31*** | 0.393 | 0.016 | 25.29*** |
Note: BFOOY= Bahamian Focus on Older Youth; CImPACT= Caribbean Informed Parents and Children Together; GFI=Goal for It; HFLE=Bahamian Health and Family Life Education. BFOOY+CImPACT represents youth assigned to the adolescent sexual risk reduction intervention whose parents were assigned to the communication/sexual risk reduction intervention; BFOOY+GFI represents youth assigned to the adolescent sexual risk reduction intervention whose parents were assigned to the goal-setting intervention; BFOOY (only) represents youth assigned to the adolescent sexual risk reduction intervention whose parents did not receive an intervention; HFLE represents youth who received the school's standard of care and their parents received no intervention.
P<0.05
P<0.01
P<0.001.
z test. ref=reference.
Table 5.
Mixed models comparing youth curriculum with a parent intervention component (parent-youth communication or parent-only goal setting) with youth curriculum only in parental monitoring and communication on sex-related matters
| Variables | Communication on sex-related matters | Parental monitoring | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall effect | Dose effect | Overall effect | Dose effect | |||||||||
| β | SE | t | β | SE | t | β | SE | t | β | SE | t | |
| Fixed effect | ||||||||||||
| Intercept | 1.964 | 0.435 | 4.51*** | 1.900 | 0.435 | 4.36*** | 5.194 | 0.279 | 18.65*** | 5.175 | 0.279 | 18.54*** |
| Age | 0.049 | 0.030 | 1.65 | 0.054 | 0.030 | 1.81 | −0.070 | 0.019 | −3.69*** | −0.069 | 0.019 | −3.61*** |
| Gender [male vs. female (ref)] | −0.186 | 0.042 | −4.47*** | −0.187 | 0.041 | −4.49*** | −0.440 | 0.026 | −16.60*** | −0.441 | 0.027 | −16.62*** |
| Intervention groups | ||||||||||||
| BFOOY+CImPACT | 0.240 | 0.077 | 3.12** | 0.131 | 0.050 | 2.59** | ||||||
| a) Parent did not participate | 0.062 | 0.123 | 0.50 | 0.023 | 0.080 | 0.28 | ||||||
| b) Participated once or twice | 0.053 | 0.103 | 0.52 | 0.124 | 0.067 | 1.84 | ||||||
| c) Participated three times | 0.493 | 0.098 | 5.02*** | 0.195 | 0.064 | 3.03** | ||||||
| BFOOY+GFI | 0.032 | 0.081 | 0.40 | 0.139 | 0.053 | 2.64** | ||||||
| d) Parent did not participate | −0.163 | 0.120 | −1.36 | 0.042 | 0.078 | 0.53 | ||||||
| e) Parent participated in GFI | 0.112 | 0.088 | 1.27 | 0.177 | 0.058 | 3.07** | ||||||
| HFLE | 0.061 | 0.076 | 0.79 | 0.062 | 0.076 | 0.81 | 0.116 | 0.050 | 2.29* | 0.116 | 0.050 | 2.30* |
| BFOOY only (ref) | ||||||||||||
| Time | ||||||||||||
| Baseline | 0.085 | 0.053 | 1.60 | 0.085 | 0.053 | 1.60 | 0.158 | 0.036 | 4.44*** | 0.158 | 0.036 | 4.44*** |
| 6-month follow-up | 0.027 | 0.055 | 0.49 | 0.027 | 0.055 | 0.49 | 0.098 | 0.037 | 2.67** | 0.098 | 0.037 | 2.67** |
| 12-month follow-up | −0.052 | 0.055 | −0.94 | −0.052 | 0.055 | −0.94 | 0.012 | 0.037 | 0.34 | 0.012 | 0.037 | 0.34 |
| 18-month follow-up (ref) | ||||||||||||
| Group×Time | ||||||||||||
| BFOOY+CImPACT×Time | 0.083 | 0.023 | 3.68*** | 0.033 | 0.015 | 2.16* | ||||||
| BFOOY+CImPACT(b)×Time | 0.045 | 0.031 | 1.48 | 0.021 | 0.021 | 1.03 | ||||||
| BFOOY+CImPACT(c)×Time | 0.141 | 0.029 | 4.91*** | 0.049 | 0.019 | 2.52* | ||||||
| Random effect | ||||||||||||
| Class† | 0.005 | 0.004 | 1.14 | 0.004 | 0.004 | 1.11 | 0.005 | 0.003 | 1.68* | 0.005 | 0.003 | 1.68* |
| Student (nested within class)† | 0.844 | 0.030 | 28.33*** | 0.842 | 0.030 | 28.31*** | 0.334 | 0.012 | 26.89*** | 0.335 | 0.012 | 26.88*** |
Note: BFOOY= Bahamian Focus on Older Youth; CImPACT= Caribbean Informed Parents and Children Together; GFI=Goal for It; HFLE=Bahamian Health and Family Life Education. BFOOY+CImPACT represents youth assigned to the adolescent sexual risk reduction intervention whose parents were assigned to the communication/sexual risk reduction intervention; BFOOY+GFI represents youth assigned to the adolescent sexual risk reduction intervention whose parents were assigned to the goal-setting intervention; BFOOY (only) represents youth assigned to the adolescent sexual risk reduction intervention whose parents did not receive an intervention; HFLE represents youth who received the school's standard of care and their parents received no intervention.
P<0.05
P<0.01
P<0.001.
z test.
ref=reference.
Significant interaction coefficients between BFOOY+CImPACT (or BFOOY+GFI) and time indicate that the rate of change over time was not the same for the three groups. Specifically, BFOOY+CImPACT youth demonstrated greater improvement in condom use skills, self-efficacy and perceived parent-youth sexual risk communication compared to BFOOY (Only) youth over the 18 month follow-up period; parental monitoring sustained at relatively high levels for both BFOOY+CImPACT and BFOOY+GFI groups while it deceased significantly for BFOOY (Only) youth during the observation period.
Advanced age was negatively associated with condom use skills and parental monitoring. Male youth displayed higher levels of condom use skills and self-efficacy but lower levels of parental monitoring and parent-youth communication compared to female youth. Mean scores for condom use skills at baseline and condom use self-efficacy at baseline and six months were significantly lower compared to mean scores at the 18 months follow up, indicating improvements in scores over time for each group. Mean scores for parental monitoring at baseline and six months were significantly higher compared to mean scores at the 18-month follow up, indicating decreases in scores over time for each group.
It is possible that effects from repeated “test taking” could influence the apparent intervention effect (e.g., the fact that the parents were exposed to a series of specific questions identifying risk and protective behaviors and strategies at six month intervals might increase their awareness of these issues). Therefore, we reconstructed the mixed effects models to allow for direct comparisons between each of the four intervention groups [BFOOY+CImPACT, BFOOY+GFI, HFLE (Only) and BFOOY (Only)] based on the number of questionnaires completed by parents (e.g., one comparison between youth from each of the four intervention groups whose parents did not complete any assessment, a second comparison among those whose parents completed one or two assessments and a final group whose parents had completed all three assessments). The results indicate that BFOOY+CImPACT youth whose parents attended all three CImPACT sessions and completed all three assessments exhibited higher levels of condom use skills (β=0.86, t=4.02, p<0.001), condom use self-efficacy (β=0.19, t=2.17, p<0.05), perceived parent-adolescent sexual risk communication (β=0.40, t=3.39, p<0.001) and parental monitoring (β=0.15, t=1.95, p=0.05), compared to BFOOY (Only) youth whose parents completed all three assessments (and did not receive any intervention). Thus, while there may have been some benefit to either or both groups of parents through repeat test-taking, the intervention (CImPACT) conferred substantial benefit. In addition, BFOOY+CImPACT youth whose parents attended one or two CImPACT sessions and completed one or two assessments also reported higher levels of condom use skills (β=0.16, t=2.13, p<0.05) compared to BFOOY (Only) youth whose parents completed all three assessments; thus even if repeated test-taking by the parent did impact parental-adolescent communication and youth outcomes, CImPACT (alone or with a booster session) had additional positive effects on youth's condom use skills.
5) Overall intervention effect on adolescent risk behavior
The proportion of youth reporting having engaged in sexual intercourse in the last six months increased steadily throughout the follow-up period (22% at baseline to 37% at 18 months). The rates did not differ significantly by intervention assignment.
The three BFOOY groups [BFOOY+CIMPACT, BFOOY+GFI, and BFOOY (Only)] had similar rates of consistent condom use at baseline (71.8% vs. 70.5% vs. 71.2%, χ2=0.05, P=0.973). At six months follow-up, rates of consistent condom use were not significantly different although the two BFOOY groups with parent intervention were slightly higher (75% vs. 74.5% vs. 70.7%). Compared to the BFOOY (Only) group, the two BFOOY groups with parent interventions (BFOOY+GFI and BFOOY+CIMPACT) showed significantly higher rates of consistent condom use at the 12 months follow-up (71.5% vs. 63.6%, χ2=3.94, P<0.05) but this difference did not persist through 18 months (data available upon request).
Discussion
The present study examined whether a brief parent-adolescent sexual risk communication intervention (CImPACT) conferred additional benefit to mid- to late adolescents who had received an effective youth risk reduction intervention. CImPACT is effective in improving the youth's perception of the amount of information communicated on sex-related matters and perceived parental monitoring as well as the youth's condom use skills and perceptions of his/her ability to use condoms. Further, there is an apparent dose effect of the brief parental intervention on parent-adolescent communication and adolescent outcomes; youth whose parents participated in the parent-adolescent communication intervention at baseline and in the booster sessions at six months and 12 months post-intervention demonstrate the greatest benefits. There is a marginal effect on consistent condom use from both parent interventions (CImPACT and GFI). These findings are consistent with recent evidence emphasizing the importance of the inclusion of parents in adolescent risk-reduction prevention and intervention programs (Burrus et al., 2012; Guilamo-Ramos et al., 2007; Murry et al., 2011).
Previous studies have illustrated the difficulty of engaging parents (Spoth, Clair, Greenberg, Redmond, & Shin, 2007); therefore we were uncertain as to whether parents would be receptive to the sexual health educational video or engage in sexual risk discussions with their adolescents. Over two-thirds of enrolled parents voluntarily attended the intervention assessments and sessions (CImPACT and GFI) or, for the parents whose child was in a HFLE (Only) or BFOOY (Only) class, to the assessment (no intervention), an indication that parents are eager to be involved in helping their youth navigate adolescence and young adulthood. All parents received information including a brief overview of the materials that would be presented about the three parent intervention conditions (i.e., no intervention, Goal for IT or CImPACT) prior to giving their consent. Parents did not know which condition they would receive prior to their arrival at the first assessment. Only after completing the questionnaire were they told to which condition they had been assigned. About one-half of parents attended all three evening assessments which for the CImPACT parents also included an intervention and two boosters and for the GFI parents an intervention and one booster. These participation rates among parents are comparable to some previously reported parent interventions (O'Donnell et al., 2005) and are more than twice of those of other parent/family programs (Connell, Dishion, Yasui, & Kavanagh, 2007; Spoth et al., 2007). Our observations of the CImPACT sessions indicated that many parents were actively involved in open discussions with their adolescents about sensitive sex-related issues after viewing the educational video together and openly discussed their questions with the facilitators.
A major challenge in sustained implementation of many effective parent-adolescent interventions has been the significant time commitment required by parents to participate in multi-session, face-to-face facilitated formats (Akers et al., 2011). CImPACT, requiring only about 20 minutes of video-viewing and 20 minutes of discussion (the latter being repeated among interested parents at the six and 12 months follow-ups), represents a promising parental intervention component that can be implemented across a wide population in conjunction with school or community-based delivery of effective adolescent risk-reduction intervention.
Our findings of improved perceived parent-adolescent sexual risk communication and sustained high levels of parental monitoring after receipt of CImPACT among these high school students are encouraging as studies have shown that parental monitoring and communication wane and peer interaction and risk involvement increase throughout the adolescent's high school year (Romer et al., 1999; Wang et al., 2013). We found that the number of communication sessions completed by parents was positively associated with increases in the frequency of sexual communication between parents and adolescents, youth-reported condom use skills and self-efficacy. This dose effect suggests the importance of repetition of the brief parental communication intervention over time. The goal-setting parental intervention (GFI) appears to have resulted in little additional positive impact on youth with respect to sexual risk except for their perceptions of increased parental monitoring. These findings suggest that while including parents in an intervention addressing adolescent children through the general topic of planning for success may be a positive addition, the specific content of a brief parental intervention is important; to reduce sexual risk behavior, the parent intervention should focus on providing parents and their adolescent(s) specific information about parental oversight and communication and specific components of safer sex practices including condom use.
Several limitations of the present study should be noted. First, the outcome measures used in this study were based on youth self-report. Although studies suggest that youth reports of parental monitoring and parent-adolescent communication tend to be more reliable than parents’ reports (Stattin & Kerr, 2000), these still reflect youth perceptions rather than an objective assessment. Youth may have over-reported or under-reported their sexual behavior and condom use (Palen et al., 2008). Second, this study relied on voluntary participation of parents. Approximately 28% of parents did not participate in this study including completion of the baseline parent questionnaire. We do not know the characteristics of these parents and thus cannot determine whether parents who participated in either CImPACT or GFI and/or completed the parent assessments differed in any significant fashion from parents who did not participate in the study. It is possible that parents who did actively participate in this intervention study might differ in some meaningful way from those who did not. Further, while the study did include two control conditions for the parent intervention (CImPACT), neither were a full “dose” control. The primary GFI and CImPACT interventions for the parents were equivalent in length (about 45 minutes divided between a video and a follow-up discussion); as well CImPACT offered two brief booster sessions delivered after the six months and 12 months assessments were completed by the parent while GFI offered only one booster after the six months assessment. In addition, although youth could attend either the CImPACT or GFI parent sessions with their parent, only CImPACT actually included the youth in the discussion and activities after the video. Finally, approximately 22% of youth were lost to follow-up at 18 months post-intervention. We compared baseline characteristics of youth who were followed versus those who were lost to follow-up at 18 months and found no significant differences in parent-adolescent communication, youth's condom use skills and self-efficacy and condom use between the two groups. However, a higher proportion of youth who were lost to follow-up had reported being sexual experienced at baseline (41.4% vs. 21.9%, χ2= 85.48, p<0.001) and perceived lower levels of parental monitoring (4.0 vs. 4.3, t= 5.12, p<0.001) at baseline. Further, those lost to follow-up were older (14.7 vs. 14.4, t=8.11, p<0.001) and a greater proportion were male (51.5% vs. 41.3%, t=18.82, p<0.001). We compared attrition rates at six months, 12 months and 18 months post-intervention and found attrition was comparable among the four intervention conditions at all three follow-ups.
The strengths of this study include its randomized design, the use of long-term longitudinal data, inclusion of both a control group [HFLE (Only)] and a youth-focused risk reduction intervention group only [BFOOY (Only)] as well as three parent intervention conditions (two receiving an intervention, the third not), and the application of mixed-effects modeling. This study design enables us to determine the impact of a brief parent-adolescent sexual risk communication intervention by controlling for the effect of an adolescent risk- reduction intervention and to assess the impact of adolescent risk-reduction intervention by comparing BFOOY (only) to the control, HFLE (Only).
Findings from this study have important implications for the prevention of HIV-related sexual risk behaviors among mid-late adolescents. First, adolescent sexual risk reduction interventions should include a parent-adolescent component as such a combination appears to produce improved outcomes compared with a program that targets adolescents only. Second, the brief parental intervention component should include specific tools addressing parent-adolescent communication regarding sensitive topics and sexual risk-reduction including condom use skills, involve the adolescent, and offer additional “booster” sessions. Third, while we did not assess the effect of CImPACT when delivered only to parents, the parent-youth dyad appears to be an effective means through which to engage, in a supervised setting, both the youth and their parent in constructive conversation regarding difficult/sensitive topics.
References
- Akers AY, Holland CL, Bost J. Interventions to improve parental communication about sex: a systematic review. Pediatrics. 2011;127:494–510. doi: 10.1542/peds.2010-2194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atienzo EE, Walker DM, Campero L, Lamadrid-Figueroa H, Gutiérrez JP. Parent-adolescent communication about sex in Morelos, Mexico: does it impact sexual behaviour? The European Journal of Contraception & Reproductive Health Care. 2009;14:111–119. doi: 10.1080/13625180802691848. [DOI] [PubMed] [Google Scholar]
- Bahamian Ministry of Health . HIV/AIDS. The commonwealth of the Bahamas: Ministry of Health HIV/AIDS Center; Nassau: 2006. [Google Scholar]
- Brody GH, Chen YF, Kogan SM, Yu T, Molgaard VK, DiClemente RJ, et al. Family-centered program deters substance use, conduct problems, and depressive symptoms in black adolescents. Pediatrics. 2012;129:108–115. doi: 10.1542/peds.2011-0623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U. The ecology of human development: Experiments by nature and design. Harvard University Press; Cambridge, MA: 1979. [Google Scholar]
- Burrus B, Leeks KD, Sipe TA, Dolina S, Soler R, Elder R, et al. Person-to-person interventions targeted to parents and other caregivers to improve adolescent health: a community guide systematic review. American Journal of Preventive Medicine. 2012;42:316–326. doi: 10.1016/j.amepre.2011.12.001. [DOI] [PubMed] [Google Scholar]
- Buzi RS, Smith PB, Weinman ML. Parental communication as a protective factor in increasing condom use among minority adolescents. International Journal of Adolescent Medicine and Health. 2009;21:51–59. doi: 10.1515/ijamh.2009.21.1.51. [DOI] [PubMed] [Google Scholar]
- Chen X, Lunn S, Deveaux L, Li X, Brathwaite N, Cottrell L, et al. A cluster randomized controlled trial of an adolescent HIV prevention program among Bahamian youth: effect at 12 months post-intervention. AIDS and Behavior. 2009;13:499–508. doi: 10.1007/s10461-008-9511-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connell AM, Dishion TJ, Yasui M, Kavanagh K. An adaptive approach to family intervention: linking engagement in family-centered intervention to reductions in adolescent problem behavior. Journal of Consulting and Clinical Psychology. 2007;75:568–579. doi: 10.1037/0022-006X.75.4.568. [DOI] [PubMed] [Google Scholar]
- Cupp PK, Atwood KA, Byrnes HF, Miller BA, Fongkaew W, Chamratrithirong A, et al. The impact of Thai family matters on parent-adolescent sexual risk communication attitudes and behaviors. Journal of Health Communication. 2013;18:1384–1396. doi: 10.1080/10810730.2013.778371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deptula DP, Henry DB, Schoeny ME. How can parents make a difference? Longitudinal associations with adolescent sexual behavior. Journal of Family Psychology. 2010;24:731–739. doi: 10.1037/a0021760. [DOI] [PubMed] [Google Scholar]
- Deveaux L, Stanton B, Lunn S, Cottrell L, Yu S, Brathwaite N, et al. Reduction in human immunodeficiency virus risk among youth in developing countries. Archives of Pediatrics & Adolescent Medicine. 2007;161:1130–1139. doi: 10.1001/archpedi.161.12.1130. [DOI] [PubMed] [Google Scholar]
- DiClemente RJ, Wingood GM, Crosby R, Cobb BK, Harrington K, Davies SL. Parent-adolescent communication and sexual risk behaviors among African American adolescent females. The Journal of Pediatrics. 2001;139:407–412. doi: 10.1067/mpd.2001.117075. [DOI] [PubMed] [Google Scholar]
- Dinaj-Koci V, Lunn S, Deveaux L, Wang B, Chen X, Li X, et al. Adolescent age at time of receipt of one or more sexual risk reduction interventions. The Journal of Adolescent Health. 2014 doi: 10.1016/j.jadohealth.2014.01.016. doi: 10.1016/j.jadohealth.2014.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong J, Stanton B, Lunn S, Deveaux L, Li X, Marshall S, et al. Effects through 24 months of an HIV/AIDS prevention intervention program based on protection motivation theory among preadolescents in the Bahamas. Pediatrics. 2009;123:e917–928. doi: 10.1542/peds.2008-2363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guilamo-Ramos V, Jaccard J, Dittus P, Bouris A, Holloway I, Casillas E. Adolescent expectancies, parent-adolescent communication and intentions to have sexual intercourse among inner-city, middle school youth. Annals of Behavioral Medicine. 2007;34:56–66. doi: 10.1007/BF02879921. [DOI] [PubMed] [Google Scholar]
- Hutchinson MK, Jemmott JB, 3rd, Jemmott LS, Braverman P, Fong GT. The role of mother-daughter sexual risk communication in reducing sexual risk behaviors among urban adolescent females: a prospective study. The Journal of Adolescent Health. 2003;33:98–107. doi: 10.1016/s1054-139x(03)00183-6. [DOI] [PubMed] [Google Scholar]
- Jackson CA, Henderson M, Frank JW, Haw SJ. An overview of prevention of multiple risk behaviour in adolescence and young adulthood. Journal of Public Health (Oxford, England) 2012;34:i31–40. doi: 10.1093/pubmed/fdr113. [DOI] [PubMed] [Google Scholar]
- Kopko K, Dunifon R. What's new: parenting and adolescent development. 2010 Retrieved from: www.human.cornell.edu/pam/outreach/parenting/research/loader.cfm.
- Mayberry M. Adolescent risk behaviors: considering the influences and interactions of multiple contexts. Proquest, Umi Dissertation Publishing; 2011. [Google Scholar]
- Murry VM, Berkel C, Chen YF, Brody GH, Gibbons FX, Gerrard M. Intervention induced changes on parenting practices, youth self-pride and sexual norms to reduce HIV-related behaviors among rural African American youths. Journal of Youth and Adolescence. 2011;40:1147–1163. doi: 10.1007/s10964-011-9642-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Donnell L, Stueve A, Agronick G, Wilson-Simmons R, Duran R, Jeanbaptiste V. Saving Sex for Later: an evaluation of a parent education intervention. Perspectives on Sexual and Reproductive Health. 2005;37:166–173. doi: 10.1363/psrh.37.166.05. [DOI] [PubMed] [Google Scholar]
- Palen LA, Smith EA, Caldwell LL, Flisher AJ, Wegner L, Vergnani T. Inconsistent reports of sexual intercourse among South African high school students. The Journal of Adolescent Health. 2008;42:221–227. doi: 10.1016/j.jadohealth.2007.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrino T, González-Soldevilla A, Pantin H, Szapocznik J. The role of families in adolescent HIV prevention: a review. Clinical Child and Family Psychology Review. 2000;3:81–96. doi: 10.1023/a:1009571518900. [DOI] [PubMed] [Google Scholar]
- Prado G, Pantin H, Huang S, Cordova D, Tapia MI, Velazquez MR, et al. Effects of a family intervention in reducing HIV risk behaviors among high-risk Hispanic adolescents: a randomized controlled trial. Archives of Pediatrics & Adolescent Medicine. 2012;166:127–133. doi: 10.1001/archpediatrics.2011.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers R. Cognitive and physiological processes in fear appeals and attitude change: A revised theory of protection motivation. In: Caaioppi T, Petty R, editors. Social Psychology. Guilford Press; New York, NY: 1983. pp. 153–176. [Google Scholar]
- Romer D, Stanton B, Galbraith J, Feigelman S, Black MM, Li X. Parental influence on adolescent sexual behavior in high-poverty settings. Archives of Pediatrics & Adolescent Medicine. 1999;153:1055–1062. doi: 10.1001/archpedi.153.10.1055. [DOI] [PubMed] [Google Scholar]
- Schwartz SJ, Unger JB, Des Rosiers SE, Huang S, Baezconde-Garbanati L, Lorenzo-Blanco EI, et al. Substance use and sexual behavior among recent Hispanic immigrant adolescents: effects of parent-adolescent differential acculturation and communication. Drug and Alcohol Dependence. 2012;125:S26–34. doi: 10.1016/j.drugalcdep.2012.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sieverding JA, Adler N, Witt S, Ellen J. The influence of parental monitoring on adolescent sexual initiation. Archives of Pediatrics & Adolescent Medicine. 2005;159:724–729. doi: 10.1001/archpedi.159.8.724. [DOI] [PubMed] [Google Scholar]
- Small SA, Kerns D. Unwanted sexual activity among peers during early and middle adolescence: Incidence and risk factors. Journal of Marriage and Family. 1993;55:941–952. [Google Scholar]
- Spoth R, Clair S, Greenberg M, Redmond C, Shin C. Toward dissemination of evidence-based family interventions: maintenance of community-based partnership recruitment results and associated factors. Journal of Family Psychology. 2007;21:137–146. doi: 10.1037/0893-3200.21.2.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanton B, Cole M, Galbraith J, Li X, Pendleton S, Cottrell L, et al. Randomized trial of a parent intervention: parents can make a difference in long-term adolescent risk behaviors, perceptions, and knowledge. Archives of Pediatrics & Adolescent Medicine. 2004;158:947–955. doi: 10.1001/archpedi.158.10.947. [DOI] [PubMed] [Google Scholar]
- Stanton B, Deveaux L, Lunn S, Yu S, Brathwaite N, Li X, et al. The condom use skills checklist (CUSC): a proxy for assessing condom use knowledge and skills when direct observation is not possible. Journal of Health, Population, and Nutrition. 2009;27:406–413. doi: 10.3329/jhpn.v27i3.3383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanton B, Li X, Ricardo I, Galbraith J, Feigelman S, Kaljee L. A randomized controlled effectiveness trial of an AIDS prevention program for low-income African-American youth. Archives of Pediatrics and Adolescent Medicine. 1996;150:363–372. doi: 10.1001/archpedi.1996.02170290029004. [DOI] [PubMed] [Google Scholar]
- Stanton B, Wang B, Deveaux L, Lunn S, Rolle G, Li X, et al. Analysis of a multifaceted, integrated HIV-risk reduction intervention targeting mid-adolescents: assessing the impacts of a complimentary parent intervention and of prior exposure to a preadolescent program. American Journal of Public Health (submitted) doi: 10.2105/AJPH.2014.302345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stattin H, Kerr M. Parental monitoring: A reinterpretation. Child Development. 2000;71:1072–1085. doi: 10.1111/1467-8624.00210. [DOI] [PubMed] [Google Scholar]
- UNAIDS Report on the Global AIDS Epidemic. 2012 Retrieved from http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2012/gr2012/20121120_UNAIDS_Global_Report_2012_with_annexes_en.pdf.
- Van Ryzin MJ, Fosco GM, Dishion TJ. Family and peer predictors of substance use from early adolescence to early adulthood: an 11-year prospective analysis. Addictive Behaviors. 2012;37:1314–1324. doi: 10.1016/j.addbeh.2012.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Véronneau MH, Dishion TJ. Predicting change in early adolescent problem behavior in the middle school years: a mesosystemic perspective on parenting and peer experiences. Journal of Abnormal Child Psychology. 2010;38:1125–1137. doi: 10.1007/s10802-010-9431-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villarruel AM, Cherry CL, Cabriales EG, Ronis DL, Zhou Y. A parent-adolescent intervention to increase sexual risk communication: results of a randomized controlled trial. AIDS Education and Prevention. 2008;20:371–383. doi: 10.1521/aeap.2008.20.5.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang B, Stanton B, Li X, Cottrell L, Deveaux L, Kaljee L. The influence of parental monitoring and parent-adolescent communication on Bahamian adolescent risk involvement: a three-year longitudinal examination. Social Science & Medicine. 2013;97:161–169. doi: 10.1016/j.socscimed.2013.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willoughby T, Hamza CA. A longitudinal examination of the bidirectional associations among perceived parenting behaviors, adolescent disclosure and problem behavior across the high school years. Journal of Youth and Adolescence. 2011;40:463–478. doi: 10.1007/s10964-010-9567-9. [DOI] [PubMed] [Google Scholar]
- Wu Y, Stanton B, Galbraith J, Kaljee L, Cottrell L, Li X, et al. Sustaining and broadening intervention impact: a longitudinal randomized trial of 3 adolescent risk reduction approaches. Pediatrics. 2003;111:e32–38. doi: 10.1542/peds.111.1.e32. [DOI] [PubMed] [Google Scholar]