Summary
The acronym SCIWORA (Spinal Cord Injury Without Radiographic Abnormality) was first developed and introduced by Pang and Wilberger who used it to define “clinical symptoms of traumatic myelopathy with no radiographic or computed tomographic features of spinal fracture or instability”. SCIWORA is a clinical-radiological condition that mostly affects children. SCIWORA lesions are found mainly in the cervical spine but can also be seen, although much less frequently, in the thoracic or lumbar spine. Based on reports from different authors, SCIWORA is responsible for 6 to 19% and 9% to 14% of spinal injuries in children and adults, respectively. Underlying degenerative changes, including spondylosis or spinal canal stenosis, are typically present in adult patients. The level of spinal cord injury corresponds to the location of these changes. With recent advances in neuroimaging techniques, especially in magnetic resonance imaging, and with increasing availability of MRI as a diagnostic tool, the overall detection rate of SCIWORA has significantly improved.
MeSH Keywords: Central Cord Syndrome, Magnetic Resonance Imaging, Spinal Cord Injuries
Background
The acronym SCIWORA (Spinal Cord Injury Without Radiographic Abnormality) was first developed and introduced by Pang and Wilberger who used it to define “clinical symptoms of traumatic myelopathy with no radiographic or computed tomographic features of spinal fracture or instability”. The first case of SCIWORA was reported by Burke in 1974 [1]. The definition does not include spinal cord injury from electric current, obstetric complications, congenital spinal anomalies or penetrating injury to the spinal canal [2]. Differential diagnosis of non-traumatic degenerative changes versus acute traumatic injuries in adults is difficult, and sometimes even impossible. Therefore, some authors use the term SCIWORET (Spinal Cord Injury Without Radiographic Evidence of Trauma) as more appropriate [3].
Recent advances in neuroimaging techniques, especially in magnetic resonance imaging, made it possible to detect damages typical of SCIWORA. The aim of the paper was to discuss physiopathology of SCIWORA and current diagnostic options that can be used to investigate this clinical-radiological condition.
Physiopathology
Based on reports from different authors, SCIWORA is responsible for 6 to 19% and 9% to 14% of spinal injuries in children and adults, respectively. The prevalence of this condition is highest among children below 8 years of age who also have the most unfavorable prognosis, which is probably associated with relatively heavy head, weaker neck muscles and greater elasticity of vertebral ligaments in this patient population [4–6]. More horizontal orientation of facet joints further increases susceptibility to these injuries. Specific biomechanics of the vertebral column in children allows the musculoskeletal system to move beyond the normal physiological range of motion without the risk of fracture. The injury to the spinal cord is caused by a contusion or ischemia due to temporary occlusion of vertebral arteries followed by a spontaneous return of vertebrae to their original position [7].
High-energy injuries are often associated with vertebral fractures or instability due to decreased flexibility of the spine in adults. In most cases, SCIWORA occurs as a result of hyperextension forces (e.g., during a rear-end car accident) or from a direct frontal impact to the face. Launay et al. suggested that these injuries are likely to occur during sports such as diving, rugby, wrestling, and baseball. However, they are most often associated with low-energy falls in the elderly. Underlying degenerative changes, including spondylosis or spinal canal stenosis, are typically present in adult patients. The level of spinal cord injury corresponds to the location of these changes which may suggest that degenerative spine conditions predispose to SCIWORA injuries [8]. Even mild hyperextension injury can cause a central cord syndrome in patients with spinal stenosis. Both bone spur growth at the posterior margins of vertebral bodies, and bulging of the yellow ligament from the back side into the spinal canal (due to a decreased height of vertebral bodies), can cause spinal cord compression and impingement (Figure 1). Venous congestion within the compressed spinal cord is an additional pathogenic factor. Neurological deficit, that is usually more severe in the upper extremities than in the lower extremities, is the most typical clinical presentation in patients with SCIWORA [9,10]. The onset of clinical symptoms is delayed from a few minutes to 48 hours after injury in about 50% of patients. This latency is associated with repeated micro-insults to the spinal cord from striking against the unstable vertebrae.
Figure 1.

A sagittal T2-weighted spin-echo MR image of the cervical spine in a 65-year-old male patient. Arrows indicate the location of spinal cord compression: anterior impingement from bone spurs at the margin of the vertebral body and posterior impingement from bulging yellow ligament.
Diagnostic Tests
Specific assessments to determine spine injury should include clinical examination, with a special focus on neurological examination. Patients diagnosed with SCIWORA have a broad spectrum of neurological deficits, from mild and transient symptoms such as paresthesia in fingers to quadriplegia. Some patients experience symptoms only at the moment of injury. When performing physical examination it is important to bear in mind that neurological deficits may only become apparent after several days of injury. Since physical examination is limited, clinicians mainly rely on diagnostic imaging when planning treatment for these patients. Conventional x-rays are usually performed as the first-line imaging test. A lateral spine x-ray can identify 75% of fractures with sensitivity of 85%. The sensitivity increases to over 90% when anteroposterior (AP), lateral, oblique and open mouth or odontoid radiographs are taken [11]. The stability of the cervical spine can also be assessed by flexion and extension dynamic radiographs. However, it should be noted that plain x-rays provide inconclusive evidence in patients with post-traumatic cervical dystonia, so they should be postponed until complete resolution of muscle spasm [12].
Computed tomography is most accurate in detecting bony pathology. A CT scan can be used to visualize subtle injuries to the posterior arch or lateral mass of the vertebra, and injuries to the atlas and odontoid process that are poorly visible on standard x-rays. When a diagnosis of spinal fracture can be excluded by x-rays and CT scan, SCIWORA should be suspected and magnetic resonance tomography (MRT) performed in patients with blunt trauma injuries and neurologic deficits.
Magnetic resonance imaging is the best modality for direct evaluation of the spinal cord. Spin-echo T1 (T1 SE), gradient-echo T2* (T2-weighted GRE*) and STIR-weighted MRI pulse sequences are preferred in patients with spinal injuries. Due to longitudinal anatomy of the spinal cord, its integrity and possible location of changes can be easily determined in sagittal plane. The main symptoms of an acute spinal injury (SCI) include edema, hematoma, anatomic transection (loss of continuity) of the spinal cord and prolapsed nucleus pulposus. T1-weighted spin-echo MR images provide information about morphology and anatomy of the spinal cord and should be performed as first diagnostic step. The bleeding can be best identified on T2-weigted GRE sequences*. An increase in the concentration of deoxyhemoglobin in fresh hematoma causes a decrease in signal intensity on T2-weigted images (Figure 2A, 2B) and, in particular, on T2-weigted GRE images*. One week or more later, with the organization of the hematoma, resulting from the conversion of deoxyhemoglobin into methemoglobin, such lesions are seen as hyperintense on T1- and T2-weighted images. However, hemorrhages will again appear hypointense on T2WI due to the presence of hemosiderin-laden macrophages in the chronic phase. A spinal cord edema is seen as hyperintense signal on T2-weighted images against a background of normal nervous tissue, and is best visible on STIR images (Figure 3). Radiological features of post-traumatic disc herniation are similar to those of non-traumatic. Therefore, it is often virtually impossible to identify the difference between the two forms of disc prolapse. Only the presence of other post-traumatic lesions at the same level may suggest possible diagnosis [13,14]. Magnetic resonance imaging is useful not only for investigating soft tissue abnormalities, it also allows identification of bone marrow edema in injured vertebrae that cannot be seen on CT scans. Short tau inversion recovery (STIR) technique, which is used to suppress the signal from fat, is most valuable in these cases [15]. Differential diagnosis should include embolism from vertebral artery occlusion associated with cardiovascular diseases such as endocarditis, cardiac arrhythmia, persistent foramen ovale, arteritis or bleeding disorder. Acute or chronic myelitis should also be excluded [16,17].
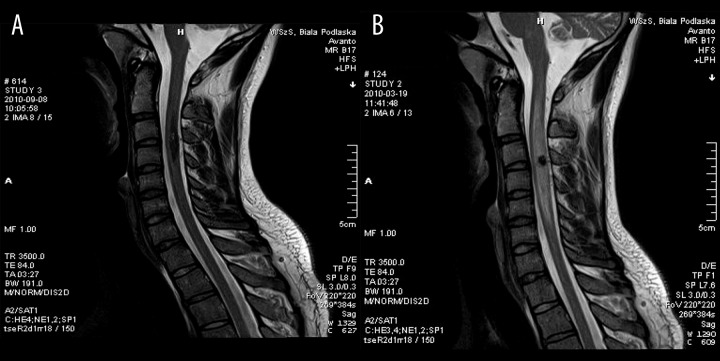
Figure 2.
(A, B) A 23-year-old patient who suffers from a cervical spine injury due to a fall from a platform. The patient exhibited muscle weakness in the upper extremities and severe neck pain on physical examination. There were no bony abnormalities on x-rays or CT scans. MR images revealed a large hyperintense lesion in the cervical spine corresponding to edema of the cervical spinal cord. A focal signal drop out can be seen in the center of the lesion (a region of hyperacute hematoma). Chronic hematoma would give a similar appearance, except for the presence of spinal edema.
Figure 3.
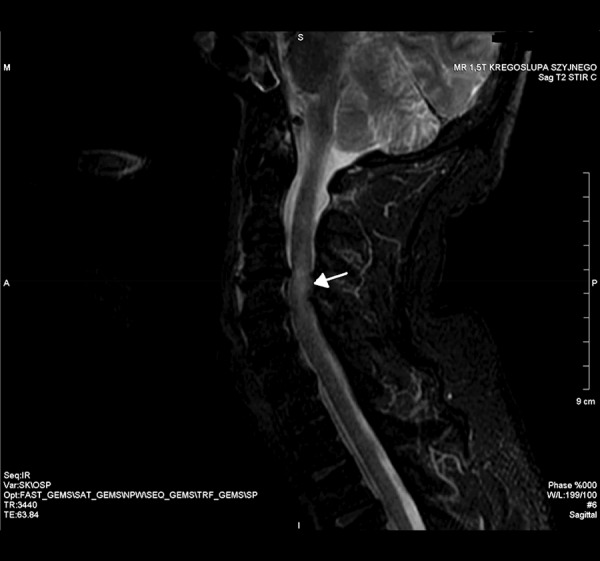
A sagittal STIR-weighted MR image of the spine. A hyperintense area pointed by an arrow represents edema of the spinal cord.
Spinal cord lesions revealed by MRI are important prognostic factors in patients with SCIWORA. Small hematomas (measuring up to 1/3 of the spinal cord diameter) or edema have favorable prognosis and resolve over time in most cases. Anatomic transection of the spinal cord or large hematomas (greater than 1/2 of the spinal cord diameter) have poor prognosis and are manifested clinically as paresis or paralysis [18].
The increasing use of MRI as the primary imaging study for spinal trauma resulted in increased number of patients diagnosed with SCIWORA who had normal MRI findings. These cases should be classified as SCIWNA or spinal cord injury without neuroimaging abnormality [14]. Shen et al. have demonstrated clinical utility of diffusion weighted imaging (DWI) in evaluation of patients with SCIWNA. Patients with normal MRI findings had hyperintense lesions on DWI [19]. Diffusion tensor magnetic resonance imaging (DTI) also becomes an important diagnostic tool in patients with SCIWORA due to its ability to assess white matter integrity. Due to a small transverse diameter of the spinal cord, DTI requires high spatial resolution and relatively small voxel volume. Moreover, the images may have artifacts introduced by breathing, swallowing or pulsatile flow of the cerebrospinal fluid. The most modern parallel imaging methods, as well as ECG-triggering or ECG-gating scan techniques can improve the image quality [20,21]. Myelography or angiography would have no application as diagnostic tools for SCIWORA.
Treatment
External immobilization of the spine for up to 12 weeks is the main therapeutic option for patients with spinal injury. Patients are also advised to avoid increased-risk activities for 6 months after diagnosis to prevent acute exacerbations of symptoms and reduce the risk of another injury. In asymptomatic patients who obtained stable spine fixation as assessed by flexion and extension dynamic radiographs, external immobilization devices can be removed earlier. Drug treatment includes the use of antihypertensive agents to maintain blood pressure within normal limits [18].
References
- 1.Burke DC. Traumatic spinal paralysis in children. Paraplegia. 1974;11:268–76. doi: 10.1038/sc.1973.39. [DOI] [PubMed] [Google Scholar]
- 2.Bruce DA. Efficacy of barbiturates in the treatment of resistant intracranial hypertension in severely head-injured children. Pediatr Neurosci. 1989;15(4):216. doi: 10.1159/000120471. [DOI] [PubMed] [Google Scholar]
- 3.Como JJ, Samia H, Nemunaitis GA, et al. The misapplication of the term spinal cord injury without radiographic abnormality (SCIWORA) in adults. J Trauma Acute Care Surg. 2012;73:1261–66. doi: 10.1097/TA.0b013e318265cd8c. [DOI] [PubMed] [Google Scholar]
- 4.Eleraky MA, Theodore N, Adams M, et al. Pediatric cervical spine injuries: report of 102 cases and review of the literature. J Neurosurg. 2000;92(Suppl 1):12–17. doi: 10.3171/spi.2000.92.1.0012. [DOI] [PubMed] [Google Scholar]
- 5.Kothari P, Freeman B, Grevitt M, Kerslake R. Injury to the spinal cord without radiological abnormality (SCIWORA) in adults. J Bone Joint Surg Br. 2000;82(7):1034–37. doi: 10.1302/0301-620x.82b7.10641. [DOI] [PubMed] [Google Scholar]
- 6.Parent S, Mac-Thiong JM, Roy-Beaudry M, et al. Spinal cord injury in the pediatric population: a systematic review of the literature. J Neurotrauma. 2011;28(8):1515–24. doi: 10.1089/neu.2009.1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmann PA, Smith SA, Schwartz JF, et al. Spinal cord infarction due to minor trauma in children. Neurology. 1975;25:301–7. doi: 10.1212/wnl.25.4.301. [DOI] [PubMed] [Google Scholar]
- 8.Launay F, Leet AI, Sponseller PD. Pediatric spinal cord injury without radiographic abnormality: a meta-analysis. Clin Orthop Relat Res. 2005;(433):166–70. doi: 10.1097/01.blo.0000151876.90256.bf. [DOI] [PubMed] [Google Scholar]
- 9.Kasimatis GB, Panagiotopoulos E, Megas P, et al. The adult spinal cord injury without radiographic abnormalities syndrome: magnetic resonance imaging and clinical findings in adults with spinal cord injuries having normal radiographs and computed tomography studies. J Trauma. 2008;65(1):86–93. doi: 10.1097/TA.0b013e318157495a. [DOI] [PubMed] [Google Scholar]
- 10.El Masri WS, Kumar N. Traumatic spinal cord injuries. Lancet. 2011;377:972–74. doi: 10.1016/S0140-6736(11)60248-1. [DOI] [PubMed] [Google Scholar]
- 11.West OC, Anbari MM, Pilgram K, Wilson AJ. Acute cervical spine trauma: diagnostic performance of single view versus three-view radiographic screening. Radiology. 1997;204:819–23. doi: 10.1148/radiology.204.3.9280266. [DOI] [PubMed] [Google Scholar]
- 12.Pollack CV, Jr, Hendey GW, Martin DR, et al. Use of flexion-extension radiographs of the cervical spine in blunt trauma. Ann Emerg Med. 2001;38(1):8–11. doi: 10.1067/mem.2001.116810. [DOI] [PubMed] [Google Scholar]
- 13.Scarabino T, Salvolini U, Jinkins JR. Emergency Neuroradiology. 2006;5:321–34. [Google Scholar]
- 14.Yucesoy K, Yuksel KZ. SCIWORA in MRI era. Clin Neurol Neurosurg. 2008;110:429–33. doi: 10.1016/j.clineuro.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 15.Parizel PM, van der Zijden T, Gaudino S, et al. Trauma of the spine and spinal cord: imaging strategies. Eur Spine J. 2010;19(Suppl 1):S8–17. doi: 10.1007/s00586-009-1123-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ergun A, Oder W. Pediatric care report of spinal cord injury without radiographic abnormality (SCIWORA): case report and literature review. Spinal Cord. 2003;41(4):249–53. doi: 10.1038/sj.sc.3101442. [DOI] [PubMed] [Google Scholar]
- 17.Ramrattan NN, Oner FC, Boszczyk BM, et al. Cervical spine injury in the young child. Eur Spine J. 2012;21(11):2205–11. doi: 10.1007/s00586-012-2292-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rozzelle, Curtis J, Aarabi, et al. Spinal Cord Injury Without Radiographic Abnormality (SCIWORA) Neurosurgery. 2013;72:227–33. doi: 10.1227/NEU.0b013e3182770ebc. [DOI] [PubMed] [Google Scholar]
- 19.Shen H, Tang Y, Huang L, et al. Applications of diffusion-weighted MRI in thoracic spinal cord injury without radiographic abnormality. Int Orthop. 2007;31(3):375–83. doi: 10.1007/s00264-006-0175-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thurnher MM, Law M. Diffusion-weighted imaging, diffusion-tensor imaging, and fiber tractography of the spinal cord. Magn Reson Imaging Clin N Am. 2009;17(2):225–44. doi: 10.1016/j.mric.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 21.Bozzo A, Marcoux J, Radhakrishna M, et al. The role of magnetic resonance imaging in the management of acute spinal cord injury. J Neurotrauma. 2011;28(8):1401–11. doi: 10.1089/neu.2009.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]