Abstract
Background
Coronary artery bypass graft (CABG) is a standard surgical option for patients with diffuse and significant arterial plaque. This procedure, however, is not free of postoperative complications, especially pulmonary and cognitive disorders.
Objective
This study aimed at comparing the impact of two different physiotherapy treatment approaches on pulmonary and cognitive function of patients undergoing CABG.
Methods
Neuropsychological and pulmonary function tests were applied, prior to and following CABG, to 39 patients randomized into two groups as follows: Group 1 (control) – 20 patients underwent one physiotherapy session daily; and Group 2 (intensive physiotherapy) – 19 patients underwent three physiotherapy sessions daily during the recovery phase at the hospital. Non-paired and paired Student t tests were used to compare continuous variables. Variables without normal distribution were compared between groups by using Mann-Whitney test, and, within the same group at different times, by using Wilcoxon test. The chi-square test assessed differences of categorical variables. Statistical tests with a p value ≤ 0.05 were considered significant.
Results
Changes in pulmonary function were not significantly different between the groups. However, while Group 2 patients showed no decline in their neurocognitive function, Group 1 patients showed a decline in their cognitive functions (P ≤ 0.01).
Conclusion
Those results highlight the importance of physiotherapy after CABG and support the implementation of multiple sessions per day, providing patients with better psychosocial conditions and less morbidity.
Keywords: Myocardial Revascularization / rehabilitation, Postoperative Care, Physical Therapy Speciality
Introduction
Coronary artery bypass grafting (CABG) is effective to treat advanced coronary artery disease (CAD), improving quality of life and prognosis of patients with that condition1-3.
Although CABG is the standard surgical option for CAD, the potential for postoperative complications may interfere with patient recovery. The most frequently complications are: pulmonary and/or cognitive function decline; infections; cardiac arrhythmias; acute myocardial infarction; and acute renal failure4 . Undoubtedly, pulmonary complications are the most frequent findings4,5. The decrease in total lung capacity (TLC) and subdivisions [vital capacity (VC), functional residual capacity (FRC), residual volume (RV) and expiratory reserve volume (ERV] following CABG may trigger complications6,7. This decrease results from the monotonous pattern of shallow breaths without periodic maximal insufflations due to respiratory drive depression caused by both anesthesia and the surgical technique8,9.
Other causes of morbidity in the postoperative period of CABG include neurological complications, which affect up to 75% of the patients5. These complications are divided into three levels: 1) cognitive changes (incidence ranging from 33% to 83%); 2) postoperative delirium (incidence ranging from 10% to 30%); and 3) stroke (incidence ranging from 1% to 6%)1,2. Affective and cognitive changes, described as changes in intellectual and behavioral functions, have been defined as comprising the inability to perform arithmetic functions, large mood swings, and explosive temper. Unfortunately, these cognitive changes have not received considerable attention, but are part of the patients’ complains as follows: “I am not the same after surgery” or “I don’t have the same disposition”2.
The mechanisms of neurocognitive changes are still a matter of debate. Possible hypotheses include cerebral hypoperfusion, cerebral macro- and microembolism, and secondary encephalic damage due to systemic inflammatory response1,5. Investigations exploring potential interventions to maintain normal cognitive function are important, mainly when considering the negative impact of its moderate or minor loss on the patient’s quality of life10.
Although physiotherapy is considered to improve post-CABG functional mobility, its ability to prevent pulmonary and/or neurocognitive complications has not been sufficiently investigated. In addition, the frequency of the physiotherapy treatment approaches can differ, and there is no consensus on its ideal protocol. This study assessed the impact of two different physiotherapy protocols on pulmonary and neurocognitive functions of patients recently submitted to CABG11.
Methods
This is a prospective study with patients randomized into two subgroups of different physiotherapy treatment approaches, by use of a list made from a table of random numbers. Control patients (Group 1) underwent physiotherapy only once a day in the morning. The intensive physiotherapy group (Group 2) underwent the same treatment three times a day: morning, afternoon and early evening. This study was performed at São Paulo Hospital, in the city of São Paulo, and at Santa Casa de Misericórdia of the city of Santos, both in the state of São Paulo, Brazil. Approval of the local ethics committee was obtained prior to study initiation, and all patients signed a written informed consent.
Participants
Participants were recruited by the cardiac surgery team. The inclusion criterion was to undergo CABG with cardiopulmonary bypass (CPB). The exclusion criteria were as follows: emergency surgical indication for CABG; age > 74 years; left ventricular ejection fraction < 30%; and cognitive deficits preventing the performance of neurocognitive tests.
Postoperative Clinical Evaluation
Postoperative complications were assessed via search in the patients’ medical records by the same medical team and meeting standardized diagnostic criteria.
Pulmonary Function Evaluation
Pulmonary expiratory volumes and respiratory muscle strength were assessed during the preoperative period, and on the third and sixth postoperative days. The last evaluation was on the day of hospital discharge. Forced vital capacity (FVC) and forced expiratory volume in the first second (FEV1) were determined with a spirometer (Microquark, Cosmed, Rome, Italy). Maximal inspiratory and expiratory pressures (MaxIP and MaxEP, respectively), which are indicators of respiratory muscle strength, were assessed with a manovacuometer (Gerar®, São Paulo, SP, Brazil). All procedures abided by the American Thoracic Society/European Respiratory Society Statement on respiratory muscle testing12. The pulmonary function results were interpreted by the first author (ESC), who was blind to group assignment.
Cognitive Function Evaluation
The cognitive assessment, carried out in all patients, consisted of a battery of four tests applied by a certified psychologist (RM) in the pre- (one day before surgery) and postoperative (on the day of hospital discharge) periods. The tests included: the Digit Span Subtest of the Wechsler Adult Intelligence Scale-Revised12,13; the Benton Revised Visual Retention Test14; the Trail Making Test15; and the Digit Symbol Subtest of the Wechsler Adult Intelligence Scale-Revised12.
Those tests focused on different cognitive aptitudes. Selective attention, ability for alternating sequence, mental flexibility, and visual skill to search were assessed by using the Trail Making Test. Short-term memory, visual skill and attention were assessed by using the Digit Span Test. Recent memory and verbal immediate recall were assessed by using the Digit Symbol Test, and visual motor coordination speed, by using the Coding Test. Finally, visual memory, visual discernment and visual motor skill were assessed by using the Benton Visual Test. All these tests are acknowledged by the American Society of Neuropsychiatry13.
Patients were instructed about the tests before taking them to ensure their understanding12,15. The psychologist interpreted the cognitive tests blindly to group assignment13.
Physiotherapy Protocol
On the first and second postoperative days, the patients remained at the Postoperative Intensive Care Unit under the care of the cardiovascular surgery physiotherapy team and following a specific postoperative protocol. The physiotherapy protocol of this study was applied by co-authors ESC and CAC during length of stay in cardiac ward on the third postoperative day. This day was chosen to avoid interference with the medical staff of the intensive care unit.
The breathing exercises consisted of the following trainings with four sets of ten repetitions: diaphragmatic breathing pattern; and ventilatory pattern inspiration in 2 times associated with elevation of the arms. This protocol is based on respiratory kinesiotherapy.
Data Analysis
Variables were expressed as means, proportions, standard deviation and frequency, according to their nature. Continuous variables with normal distribution were compared intragroup (same group at different times) and intergroup (Group 1 versus Group 2) by using paired and non-paired Student t tests, respectively. Chi-square test was applied for categorical variables. For variables without normal distribution, the Mann-Whitney test was used for comparison between different groups, and Wilcoxon test for intragroup analysis at different times.
Assuming a 5% alpha error and a 20% beta error, a sample of at least 18 patients in each group was estimated to be necessary to detect a 30% difference between the physiotherapy protocols evaluated. Statistical tests with p value ≤ 0.05 were considered significant. The SPSS for Windows, version 11, was used for statistical analyses.
Results
The sample consisted of 39 patients with mean age of 61.95 ± 8.5 years, and 17 (43.6%) males and 22 (56.4%) females. Regarding their educational level, 24 patients (61.5%) had only elementary education, 12 (30.8%) had high-school education, and three (7.7%), higher education. Table 1 shows the demographic characteristics and surgical variables.
Table 1.
Demographic and surgical data of the patients
| Group 1 | Group 2 | |
|---|---|---|
| N | 20 | 19 |
| Age | 60.75 (± 7.43) | 63.21 (± 9.57) |
| Gender Male | 10 | 7 |
| Female | 10 | 12 |
| Total coronary grafts | 43 | 52 |
| One coronary graft | 2 | 0 |
| Two coronary grafts | 13 | 5* |
| Three coronary grafts | 5 | 14* |
| Total surgical time (minutes) | 321.25 (± 45.66) | 361.00 (± 72.64) |
| Anoxia time (minutes) | 53.30 (± 19.61) | 50 (± 14.17) |
| Perfusion time (minutes) | 89.90 (± 28.12) | 98.21 (± 21.51) |
Intergroup analysis by using Student t test.
Statistically significant when p < 0.05.
Postoperative Clinical Assessment
Postoperative complications were found in 59% of the patients, and consisted of atelectasis, pleural effusion, pneumonia, pericardial effusion, and acute atrial fibrillation. Atelectasis was the major postoperative complication, present in 25% of Group 1 patients and 42% of Group 2 patients, followed by pleural effusion in 10% and 15%, respectively, but without statistical significance.
Pulmonary Function
Both groups showed a respiratory rate (RR) increase from the preoperative period to the third postoperative day. Similar behavior was observed between the third postoperative day and hospital discharge, with a decrease in RR, which returned to baseline values. Both FVC and FEV1 decreased in Groups 1 and 2 from the preoperative to the postoperative periods. As expected, until discharge, there was a gradual return of those variables to baseline values (Table 2).
Table 2.
Respiratory variables (mean ± SD) in the preoperative period (Pre) and on the 3rd and 6th postoperative (PO) days
| Respiratory variables | Group 1 | Group 2 | ||||
|---|---|---|---|---|---|---|
| Pre | 3rd PO | 6th PO | Pre | 3rd PO | 6th PO | |
| RR | 15.5 (2.28) | 17.25 (1.97)* | 14.75 (2.07)* | 14.21 (20) | 17.84 (3.0)* | 14.89 (2.26)* |
| FVC | 319.80 (119.68) | 161.20 (83.26)* | 216.65 (109.20) | 299.47 (96.87) | 163.74 (74.17)* | 226.32 (67.06) |
| FEV1 | 2.45 (0.82) | 1.25 (0.58) | 1.71 (0.79) | 2.44 (0.88) | 1.31 (0.57)* | 1.79 (0.51) |
| MaxIP | -100.50 (25.13) | -55.75 (19.62)* | -84 (25.68)* | -98.42 (±26.51) | -53.16 (17.97)* | -81.05 (21.45)* |
| MaxEP | 108.75 (4.05) | 78.75 (26.30)* | 85.60 (48.79) | 108.95 (22.89) | 76.58 (18.19)* | 99.11 (18.11)* |
RR: respiratory rate per minute; FVC: forced vital capacity; FEV1: forced expiratory volume in the 1st second; MaxIP: maximal inspiratory pressure; MaxEP: maximal expiratory pressure.
Statistically significant when p < 0.05.
Regarding respiratory muscle strength, from the preoperative period to the third postoperative day, MaxIP and MaxEP decreased in both groups. An increase in MaxIP and MaxEP was observed before hospital discharge in both groups and with statistical significance in all periods (p < 0.05). However, MaxEP showed statistical difference only between the preoperative period and the third postoperative day (Table 2).
Comparing Group 1 and Group 2, no respiratory variable showed statistical difference.
Cognitive Function
Several tests expressing different neurocognitive functions were performed to detect postoperative changes as already reported in the literature.
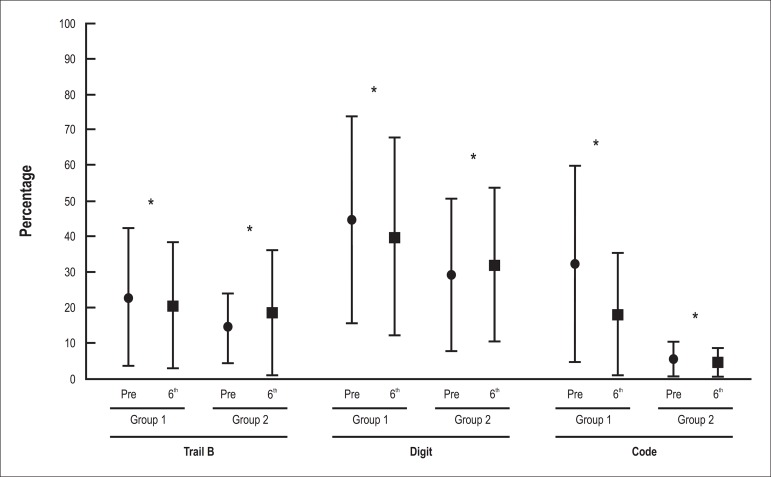
Regarding the neurocognitive function analysis focusing on selective attention and ability for alternating sequence, assessed by using part A of the Trail Making Test, both groups showed increasing scores between the preoperative period and hospital discharge, but without statistical significance (Table 3). However, part B of the same test showed a different behavior: Group 1 had a decrease in its initial score, while Group 2 had an increase during that same period. Comparing Group 1 and Group 2, the difference was statistically significant (p < 0.01) (Figure 1).
Table 3.
Neurocognitive variables (mean ± SD) in the preoperative period (Pre) and on the 6th postoperative (PO) day
| Cognitive variables | Group 1 | Group 2 | ||||
|---|---|---|---|---|---|---|
| Pre | 6th PO | Pre | 6th PO | |||
| Trail A | 39.5 (27.81) | 41.25 (29.77) | 19,47 (21.91) | 21.58 (17.08) | ||
| Trail B** | 24.5 (19.05) | 20.5 (17.84) | 15 (12.8) | 19.47 (19) | ||
| Digit Test** | 45.5 (30.8) | 40.8 (28.23) | 30.89 (22.73) | 32.05 (23.64) | ||
| Coding Test** | 31.2 (32.16) | 17.95 (23.85) | 5.95 (8.13) | 4.63 (4.96) | ||
| Benton Start | 21.6 (20.89) | 18.40 (19.24) | 23.47 (20.78) | 18.84 (21.50) | ||
| Benton End | 13.65 (17.23) | 11.25 (13.76) | 33.63 (27.85) | 30.16 (30.24) |
Statistically significant for comparison between Group 1 and Group 2 (p < 0.05).
Figure 1.
Evolution of the neurocognitive functions - Trail B Test, Digit Test and Coding Test - during the preoperative period (Pre) and on the 6th postoperative (PO) day. The results are expressed as mean ± SD. The comparison between groups was performed by using Mann-Whitney Test (* p < 0.01).
The Digit Symbol Test detected a decrease in score of Group 1 between the preoperative period and hospital discharge. Differently, Group 2 showed an increase in score, but without statistical significance. By the same token, when we compared Group 1 and Group 2, the difference was statistically significant. Regarding the Coding Test, both Group 1 and Group 2 showed a decreasing score, which was lower in Group 2. The statistical analysis between the groups was significant in both Digit Symbol and Coding tests (Table 3 and Figure 1, p < 0.01).
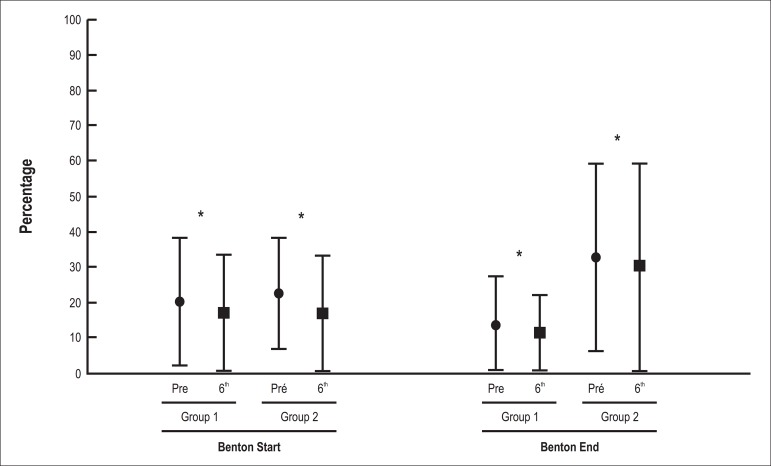
Similar findings were observed with Benton Visual Test, with groups showing a decrease in score between the preoperative period and hospital discharge. The results of Benton End Test were also statistically significant when comparing Group 1 and Group 2 (p < 0.01). From the viewpoint of the cognitive tests applied, Group 2 performed better (Table 3, Figure 2).
Figure 2.
Evolution of the neurocognitive functions - Benton Test Start and Benton Test End - during the preoperative period (Pre) and on hospital discharge (6th day). The results are expressed as mean ± SD. The comparison between groups was performed by using Mann-Whitney Test (* p < 0.01).
Discussion
The postoperative period immediately following CABG is a critical time when a number of complications may influence patient recovery. However, patient care during early recovery does not only focus on complication and morbidity prevention, but is also aimed at improving the patient’s functional recovery.
In this study, CABG with CPB showed morbidity related to abnormalities of the respiratory and neurocognitive functions. The oxygenation and artificial circulation employed in that type of surgery, in addition to the procedure itself (sternotomy), are likely culprits for those changes11. In this sample of patients, the motor and sensory stimulation delivered by physiotherapy sessions three times a day improved the cognitive functions despite lack of additional effect on the pulmonary functions.
Of the risk factors involved in neurocognitive dysfunction in the perioperative period, three specifically stand out: age, educational level, and previous diseases. Particularly important risk factors in the intraoperative period are as follows: embolus formation; CPB time; air bubbles originating from the oxygenator; blood pressure level; and the temperature elevation that may occur in the postoperative period16,17.
The mean CPB time of 95.05 minutes found in this study was not a risk factor for complication per se. In medical literature, there is concern about time longer than 100 minutes18,19. In accordance with other studies, we found a significant decrease in lung volume, lung capacities and respiratory muscle strength (FVC, FEV1, MaxIP and MaxEP) during the postoperative period (third postoperative day)6. In both groups, all respiratory variables (FVC, FEV1, MaxIP and MaxEP) decreased, but without statistical significance. These changes are due to an increase in the peak pressure of airways and a decrease in lung compliance, indicating an elevation in respiratory system resistance, which can be influenced by CPB, surgical incision, diaphragmatic dysfunction, pain and immobilization in bed9,11,20. Most factors described emphasize the importance of physiotherapy in this population. Less pain, better chest mobility and alveolar ventilation are known to minimize the likelihood of postoperative complications, thus leading to less morbidity21. It is also well-known that breathing exercises may attenuate the decline of respiratory variables in the postoperative period of thoracic surgeries. Our findings indicate that one daily physiotherapy session was sufficient to produce the desired pulmonary improvements during the acute postoperative phase. Surprisingly, the group performing more physiotherapy exercises had a significantly better restoration of neurocognitive functions. Therefore, the increase in the frequency of physiotherapy sessions may reduce postoperative morbidity related to neurocognitive dysfunction, which usually lasts days and even months after heart surgery, impairing memory, concentration, language, understanding, learning, speed of response and visual motor integration. It is worth noting that such negative effects have been linked to the quality of life of patients undergoing CABG16. We hypothesized that the increase in physiotherapy frequency may result in a greater stimulation of the sensory/motor system, providing a greater activation of afferent nerves to the neurocognitive system and influencing a better patient outcome.
The major exclusion criterion for this study was age older than 74 years. Neurocognitive function decline in the postoperative period (reported as up to 9%) is much more common and expected above that age. The cohort assessed in this study had a mean age of 60 years, which has been related to a smaller effect on neurocognitive functions in the postoperative period. When age was related to cognitive function, only the Digit Span test, which assesses visual motor coordination speed, found different scores, represented by a smaller one in Group 222.
In this study, some results of cognitive impairment in patients undergoing CABG with CPB differed from those reported in the medical literature. Most of the neurocognitive tests performed showed increased or slightly decreased scores between the preoperative period and hospital discharge in Group 2, which underwent much more intense and frequent physiotherapy sessions.
Evaluation of selective attention and ability for alternating sequence, assessed by using Trail Making Test, part A, in both groups showed a slight score increase between the preoperative period and hospital discharge. However, in part B of the same test, Group 2, unlike Group 1, increased its score between the preoperative period and hospital discharge, suggesting that greater stimuli improved cognitive function. Similar behavior occurred when the short-term memory and verbal immediate recall were evaluated by using Digit Symbol Test: Group 1 showed a score decrease, while Group 2 showed a score increase. When the speed of visual motor coordination and visual memory (Coding and Benton Visual Tests) were analyzed, a decline in both groups was observed, being bigger in Group 1 (p < 0.01).
The medical literature has reported that mild neurocognitive abnormalities may occur following cardiac surgery16. Surprisingly, some tests showed an increase in the scores of the group treated with physiotherapy three times a day. To our knowledge, this is the first study to assess the influence of physiotherapy on cognitive function. In our clinical practice, we have observed that patients undergoing cardiac surgery evolve better in relation to both pulmonary physiology and neurocognitive function when treated with more frequent physiotherapy sessions, highlighting the dynamic interaction between body and mind. This led us to plan this project in an attempt to verify whether this effect would actually occur.
Sample size is the most important study limitation. But even with a not very large number of patients and relatively simple physiotherapy protocol23, our results confirm the hypothesis that patients undergoing more physiotherapy sessions have a better cognitive restoration until hospital discharge.
We suggest that the greater amount of physiotherapy during hospitalization would increase the number of synapses in the cortical afferent system and improve neuronal communication, resulting in the minimization or mitigation of neurocognitive disorders caused by cardiac surgery.
Conclusion
As shown in this study, CABG with CPB leads to alterations of pulmonary and neurocognitive functions in the postoperative period that may hinder the patient’s clinical outcome. Respiratory therapy is a way to minimize the damage to lung function in this population.
Surprisingly, neurocognitive functions showed increased scores in the group undergoing more respiratory physiotherapy sessions per day, with enhanced perioperative levels, suggesting that when patients are more stimulated, they have greater neurocognitive development.
Studies correlating respiratory physiotherapy with neurocognitive function in the postoperative period of cardiac surgery lack. Our results encourage further studies on this theme. This new approach opens a new avenue of exploration, not only to the possibility of decreasing the potential damage related to the neuropsychological sphere secondary to cardiac surgery with CPB, but perhaps as a simple and practical strategy to prevent or minimize such changes.
Footnotes
Author contributions
Conception and design of the research: Cavalcante ES, Conforti CA, Carvalho ACC, Buffolo E, Luna Filho B; Acquisition of data: Cavalcante ES, Magario R; Analysis and interpretation of the data: Cavalcante ES, Magario R, Luna Filho B; Statistical analysis: Luna Filho B; Writing of the manuscript: Cavalcante ES, Cipriano Júnior G, Arena R, Luna Filho B; Critical revision of the manuscript for intellectual content: Cavalcante ES, Conforti CA, Cipriano Júnior G, Carvalho ACC, Buffolo E, Luna Filho B.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Sources of Funding
There were no external funding sources for this study.
Study Association
This article is part of the thesis of master submitted by Elder dos Santos Cavalcante, from UNIFESP - Escola Paulista de Medicina.
References
- 1.van Harten AE, Scheeren TW, Absalom AR. A review of postoperative cognitive dysfunction and neuroinflammation associated with cardiac surgery and anaesthesia. Anaesthesia. 2012;66(3):280–293. doi: 10.1111/j.1365-2044.2011.07008.x. [DOI] [PubMed] [Google Scholar]
- 2.Selnes OA, Gottesman RF, Grega MA, Baumgartner WA, Zeger SL, Mckhann GM. Cognitive and neurologic outcomes after coronary-artery bypass surgery. N Engl J Med. 2012;366(3):250–257. doi: 10.1056/NEJMra1100109. [DOI] [PubMed] [Google Scholar]
- 3.Keenan TD, Abu-Omar Y, Taggart DP. Bypassing the pump: changing practices in coronary artery surgery. Chest. 2005;128(1):363–369. doi: 10.1378/chest.128.1.363. [DOI] [PubMed] [Google Scholar]
- 4.Wynne R, Botti M. Postoperative pulmonary dysfunction in adults after cardiac surgery with cardiopulmonary bypass: clinical significance and implications for practice. Am J Crit Care. 2004;13(5):384–393. [PubMed] [Google Scholar]
- 5.Selnes OA, Mckhann GM. Cognitive changes after coronary artery bypass surgery. Curr Opin Psychiatry. 2002;15(3):285–290. [Google Scholar]
- 6.Guizilini S, Gomes WJ, Faresin SM, Bolzan DW, Alves FA, Catani R, et al. Avaliação da função pulmonar em pacientes submetidos à cirurgia de revascularização do miocárdio com e sem circulação extracorpórea. Rev Bras Cir Cardiovasc. 2005;20(3):310–316. [Google Scholar]
- 7.Ng CS, Wan S, Yim AP, Arifi AA. Pulmonary dysfunction after cardiac surgery. Chest. 2002;121(4):1269–1277. doi: 10.1378/chest.121.4.1269. [DOI] [PubMed] [Google Scholar]
- 8.Jackson CV. Preoperative pulmonary evaluation. Arch Intern Med. 1988;148(10):2120–2127. [PubMed] [Google Scholar]
- 9.Hedenstierna G. Mechanism of postoperative pulmonary dysfunction. Acta Chir Scan Suppl. 1988;550:152–158. [PubMed] [Google Scholar]
- 10.Newman MF, Blumenthal JA. Longitudinal assessment of neurocognitive function after coronary-artery bypass surgery. N Engl J Med. 2001;344(6):395–402. doi: 10.1056/NEJM200102083440601. [DOI] [PubMed] [Google Scholar]
- 11.Renaut JA, Costa-Val R, Rossetti MB. Fisioterapia respiratória na disfunção pulmonar pós-cirurgia cardíaca. Rev Bras Cir Cardiovasc. 2008;23(4):562–569. doi: 10.1590/s0102-76382008000400018. [DOI] [PubMed] [Google Scholar]
- 12.American Thoracic Society. European Respiratory Society ATS/ERS Statement on respiratory muscle testing. Am J Respir Crit Care Med. 2002;166(4):518–624. doi: 10.1164/rccm.166.4.518. [DOI] [PubMed] [Google Scholar]
- 13.Spreen O, Strauss E. A compendium of neuropsychological tests. New York: Oxford University Press; 1998. pp. 270-9, 533-47. [Google Scholar]
- 14.Walsh WB, Nancy EB. Tests and assessment. Englewood Cliffs. New Jersey: Prentice Hall; 1990. [Google Scholar]
- 15.Lezak MD, Howieson DB, Loring DW. Neuropsychological assessment. New York: Oxford University Press; 2004. [Google Scholar]
- 16.Gao L, Taha R, Gauvin D, Othmen LB, Wang Y, Blaise G. Postoperative cognitive dysfunction after cardiac surgery. Chest. 2005;128(5):3664–3670. doi: 10.1378/chest.128.5.3664. [DOI] [PubMed] [Google Scholar]
- 17.Martin JF, Melo RO, Sousa LP. Disfunção cognitiva após cirurgia cardíaca. Rev Bras Cir Cardiovasc. 2008;23(2):245–255. doi: 10.1590/s0102-76382008000200015. [DOI] [PubMed] [Google Scholar]
- 18.Al-Ruzzeh S, Nakamura K, Athanasiou T, Modine T, Georg S, Yacoub M, et al. Does off-pump coronary artery bypass (OPCAB) surgery improve the outcome in high-risk patients? A comparative study of 1398 high-risk patients. Eur J Cardiothorac Surg. 2003;23(1):50–55. doi: 10.1016/s1010-7940(02)00654-1. [DOI] [PubMed] [Google Scholar]
- 19.Higgins TL, Estafanous FG, Loop FD, Beck GJ, Blum JM, Paranandi L. Stratification of morbidity and mortality outcome by preoperative risk factors in coronary artery bypass patients: a clinical severity score. JAMA. 1992;267(17):2344–2348. Erratum in JAMA. 1992;268(14):1860. [PubMed] [Google Scholar]
- 20.Cox CM, Ascione R, Cohen AM, Davies IM, Ryder IG, Angelini GD. Effect of cardiopulmonary bypass on pulmonary gas exchange: a prospective randomized study. Ann Thorac Surg. 2000;69(1):140–145. doi: 10.1016/s0003-4975(99)01196-0. [DOI] [PubMed] [Google Scholar]
- 21.Stiler K, Montarello J, Wallace M, Daff M, Grant R, Jenkins S, et al. Efficacy of breathing and coughing exercises in the prevention of pulmonary complications after coronary artery surgery. Chest. 1994;105(3):741–747. doi: 10.1378/chest.105.3.741. [DOI] [PubMed] [Google Scholar]
- 22.Kadoi Y, Goto F. Factors associated with postoperative cognitive dysfunction in patients undergoing cardiac surgery. Surg Today. 2006;36(12):1053–1057. doi: 10.1007/s00595-006-3316-4. [DOI] [PubMed] [Google Scholar]
- 23.Matte P, Jacquet L, Van Dyk M, Goenen M. Effects of conventional physiotherapy, continuous positive airway pressure and non-invasive ventilatory support with bilevel positive airway pressure after coronary artery bypass grafting. Acta Anaesthesiol Scand. 2002;44(1):75–81. doi: 10.1034/j.1399-6576.2000.440114.x. [DOI] [PubMed] [Google Scholar]