Abstract
Purpose
The purpose of this study was to examine the prevalence and correlates of suicidal ideation (SI) in patients with stable moderate to very severe chronic obstructive pulmonary disease (COPD).
Patients and methods
We conducted an exploratory mixed methods analysis of data from participants in a longitudinal observational study of depression in COPD. We measured depression with the Patient Health Questionnaire-9 (PHQ-9), which includes an item on SI. We compared participants with and without SI in relation to sociodemographics, symptoms, anxiety, and healthcare resource use with independent t-tests and chi-square tests. Content analysis was performed on qualitative data gathered during a structured SI safety assessment.
Results
Of 202 participants, 121 (60%) had depressive symptoms (PHQ ≥6); 51 (25%) had a PHQ-9 ≥10, indicating a high likelihood of current major depression; and 22 (11%) reported SI. Compared to the 99 depressed participants without SI, those with SI were more likely to be female (59% vs 27%, P=0.004); had worse dyspnea (P=0.009), depression (P<0.001), and anxiety (P=0.003); and were also more likely to have received treatment for depression and/or anxiety (82% vs 40%, P<0.001) and more hospitalizations for COPD exacerbations (P=0.03) but had similar levels of airflow obstruction and functioning than participants without SI. Themes from the qualitative analysis among those with SI included current or prior adverse life situations, untreated or partially treated complex depression, loss of a key relationship, experience of illness and disability, and poor communication with providers.
Conclusion
Our findings suggest that current SI is common in COPD, may occur disproportionately in women, can persist despite mental health treatment, and has complex relationships with both health and life events. Adequate management of SI in COPD may therefore require tailored, comprehensive treatment approaches that integrate medical and mental health objectives.
Keywords: depression, qualitative, PHQ-9, suicide, pulmonary disease, chronic obstructive
Introduction
The prevalence of depression among patients with chronic obstructive pulmonary disease (COPD) is high, ranging between 25% and 50%,1–3 and patients with COPD are 2.5 times more likely to have depressive symptoms that those without COPD.4
Depression in COPD is associated with poor outcomes including worse quality of life,1,5 higher respiratory symptom burden,6 increased rates of hospitalization,1,7–9 and increased mortality.1,6,10,11 Depression is one of the strongest risk factors for suicidal thoughts and attempts (suicidal ideation [SI]), and there is epidemiologic evidence that COPD is independently associated with increased risk for suicide.12,13
Many studies of depression in COPD have used depressive symptom scales such as the Hospital Anxiety and Depression scale14 or the Geriatric Depression Scale,15 and although these scales assess the severity of depressive symptoms, they do not measure whether a patient is experiencing SI. As a result, little published data exist on the prevalence of suicidal thoughts in COPD. In a recent study of a nationally representative sample in the United States, Goodwin16 found that 27% of respondents with COPD had experienced SI at some time in their lives, compared to 20% of those without COPD, and that 15% of participants with COPD had attempted suicide, compared to 7% of those without COPD. A limitation of this study was that COPD was self-reported, the diagnosis and severity were not confirmed by spirometry, and the social, emotional, and medical contexts of SI in COPD were not investigated.
The Patient Health Questionnaire (PHQ)-917 is widely used in clinical practice to measure the severity of depressive symptoms and includes a question (item 9) identifying feelings of despair. A positive score on this item predicted risk of suicide attempt or suicide death in a large health care system population,18 supporting its value for studies of SI.
Given that few studies have explored either the prevalence or context of SI in persons with a serious chronic disease such as COPD, the aim of this study was to assess the point prevalence of SI with the PHQ-9 in a cohort of patients with moderate to very severe COPD enrolled in the CASCADE study (COPD Activity: Serotonin transporter, Cytokines, and Depression). In addition, we also sought to explore the narrative context of SI using qualitative data collected as part of the study protocol.
Methods
Study design
CASCADE is a prospective multisite observational study of individuals with COPD that examines the biological correlates and functional consequences of depression in persons with COPD. Here we report a cross-sectional descriptive analysis of data from the first 202 subjects. The study was approved by the respective institutional review boards at three clinical sites (University of Washington, Puget Sound Veterans Health Care System, and University of Texas Health Science Center at San Antonio/South Texas Veterans Health Care System), and was registered with ClinicalTrials.gov (NCT01074515).
Participants
English speakers aged 40+ years, recruited from multiple sources,19 were included if they had a diagnosis of COPD (postbronchodilator forced expiratory volume in 1 second/forced vital capacity (FEV1/FVC) <70%), moderate to very severe disease by the Global initiative for chronic Obstructive Lung Disease (GOLD) criteria (FEV1 <80%), at least a 10 pack-year history of cigarette smoking and stable disease with no acute exacerbations in the prior 4 weeks. We excluded patients with any of the following conditions: other chronic obstructive lung diseases such as asthma, bronchiectasis, or cystic fibrosis; idiopathic pulmonary fibrosis; uncompensated congestive heart failure (left ventricular dysfunction); primary pulmonary vascular disease; non-COPD-related chronic inflammatory diseases; infectious or autoimmune disease; lung cancer or metastatic cancer; chronic renal failure that requires dialysis; chronic uncompensated liver disease; human immunodeficiency virus/acquired immune deficiency syndrome; chronic antibiotic use or ongoing infection; chronic oral prednisone use; bipolar disease; psychotic disorders; or dementia.
Overview of study procedures
Baseline study assessments were conducted both in person (spirometry, 6-minute walk distance, and questionnaires as detailed below), and 2–5 days later, by telephone. Telephone assessments included the PHQ-9,20 the Hospital Anxiety and Depression Scale (HADS),21 and a brief past history of depressive episodes using the Structured Clinical Interview for Depression (SCID).22
The PHQ-9 is a depression questionnaire that includes this final question: “Over the last two weeks, how often have you been bothered by thoughts that you would be better off dead, or of hurting yourself in some way?” with response options of “not at all,” “several days,” “more than half the days,” or “nearly every day.” If participants replied “yes” to any of the positive response options to this SI questions, a structured suicide risk assessment was conducted and the participant’s primary care provider or pulmonologist and, if applicable, mental health specialty providers were notified to ensure patient safety and continuity of care.
The interviewer had a background as a clinical therapist and received initial training on how to conduct the interviews from the study psychiatrist (SB). The interviewer used a written protocol when a participant endorsed suicidal thoughts in the last 2 weeks, including telephone consultation with the study psychiatrist. To assess quality control for the telephone depression assessments, the initial training included mock interviews with SB followed by cointerviews with at least five patients or until SB was confident in the fidelity of the interviews. In addition, ongoing quality checks of 5% of the phone calls throughout the study were performed by the study psychiatrist. In addition to the depression assessments, participants were also followed with phone calls every 3–6 months regarding health care utilization and exacerbations. Participants are followed for a total of 2 years and have an annual in-person study visit followed by an annual telephone depression assessment.
Measures
Demographic data included age, sex, education, income, living situation, and marital status.
Severity of chronic disease included spirometry, performed to American Thoracic Society standards;23 use of supplemental oxygen; 6-minute walk distance; number of COPD hospitalizations in the previous year; self-reported chronic conditions (Charlson comorbidity index);24 physical functioning (Medical Outcomes Study-Short Form 36);25 and dyspnea and fatigue measured with the Chronic Respiratory Questionnaire (CRQ).26
Psychiatric history/status
The final question on the PHQ-9,20 “How often in the last two weeks have you been bothered by thoughts that you would be better off dead or of hurting yourself in some way?”, was used to classify participants as having or not having suicidal ideation (SI). Any response other than “not at all” was scored as positive. Though responses may reflect feelings of demoralization and futility about participants’ lives (not always intent to inflict self-harm), this question has been found to have a sensitivity of 0.84 and a specificity of 0.69 when compared to endorsement of explicit SI in a structured clinical interview,27 and positive scores are associated with risk for future suicide.18,27
The PHQ-9 was used as the primary measure of current depression.20 Scores of 6 or more denote at least mild depression; scores ≥10 suggest a high likelihood of major depression.28 In this study, subjects scoring at least 6 points or more were classified as depressed. The SI score (question #9) was excluded from comparisons of participants with and without SI; PHQ-8 was used as the total. We also examined the psychological (Questions 1, 2, 6) and physiological (Questions 3, 4, 5, 7, 8) items separately to determine whether patients with SI had greater psychological distress.29
Lifetime history of depression was measured using the SCID.22 Any score other than 0 on the SCID (indicating at least one episode of depression during a participant’s lifetime, excluding the current episode of depression, if any) was considered to be positive.
History of post-traumatic stress disorder and drug abuse were obtained via self-report as part of the medical history. Use of antidepressants, anxiolytics, and psychotherapy or counseling as well as response to these treatments were obtained via self-report. Psychological well-being was measured with the HADS scale,21 the Medical Outcome Study Short-Form-36 mental component summary,25 the CRQ-emotional functioning scales,26 and total score of the Medical Outcomes Study Social Support Scale.30 Engagement in self care was measured with the CRQ-mastery scale26 and the Patient Activation Measure.31
Data analysis
We used chi-square and independent t-tests to compare participants endorsing SI to patients with depression but no SI. All analyses were conducted using SPSS 15.0 (SPSS Inc., Chicago, IL, USA). A P-value <0.05 was considered statistically significant.
As part of the study protocol, the mental health research staff (SF) used an interview guide to elicit background factors, circumstances temporally related to the SI, and level of risk on all subjects who endorsed SI during the mental health assessment. Detailed notes were taken using an electronic data collection tool. These qualitative data were categorized into themes by two raters (SF and SB).
Results
Of 202 total participants, 51 (25%) had a PHQ-9 score ≥10, indicating high likelihood of current major depression, and 121 (60%) had a score ≥6, indicating at least mild depressive symptoms. A total of 18 participants (9%) reported SI at baseline; four others without SI at baseline reported new onset SI at their second study evaluation a year later and were included in the SI cohort (n=22) for descriptive purposes (Table 1). Participants with SI were significantly more likely to be female (P=0.004) and had more severe dyspnea (P=0.009) and COPD hospitalizations in the previous year (P=0.03) but similar levels of airflow obstruction, functional capacity, and physical functioning compared to depressed participants without SI.
Table 1.
Baseline characteristics of patients with COPD according to suicide and depression status (n=121)
| Variables | Depressed with SI (n=22)* | Depressed – no SI (n=99) | P-value |
|---|---|---|---|
| Sociodemographics | |||
| Age, years | 64.1±8.7 | 65.5±8.4 | 0.47 |
| Sex, women | 13 (59%) | 27 (27%) | 0.004 |
| Education | |||
| High school or less | 16 (73%) | 78 (78%) | 0.54 |
| Some college or more | 6 (27%) | 21 (21%) | |
| Income | |||
| <$20K/year | 14 (64%) | 46 (46%) | 0.15 |
| ≥$20K/year | 8 (36%) | 53 (53%) | |
| Marital status | |||
| Partnered | 8 (36%) | 45 (45%) | 0.44 |
| Unpartnered | 14 (64%) | 54 (54%) | |
| Live with others | 14 (64%) | 67 (68%) | 0.72 |
| Current smoker | 5 (23%) | 32 (32%) | 0.38 |
| Pulmonary disease | |||
| FEV1/FVC | 0.45±0.12 | 0.46±0.13 | 0.80 |
| FEV1% predicted | 46.3±16.6 | 42.5±14.2 | 0.28 |
| Any daily O2 supplementation | 10 (46%) | 40 (40%) | 0.66 |
| % hospitalized for COPD in past year† | 4 (18%) | 19 (19%) | – |
| Number of hospitalizations for COPD in previous year | 0.68±1.7 | 0.24±0.55 | 0.03 |
| Number of comorbidities | 0.8±0.9 | 0.8±1.1 | 0.86 |
| Six-minute walk distance (feet) | 1,022.9±408 | 1,066.3±403 | 0.66 |
| SF-36 Physical Component (0–100↑) | 31.4±8.6 | 31.8±8.5 | 0.83 |
| CRQ-Dyspnea (5–35↑) | 17.7±6.4 | 21.6±6.3 | 0.009 |
| CRQ-Fatigue (4–28↑) | 12.3±4.4 | 13.2±4.0 | 0.34 |
| Psychiatric history/status | |||
| Lifetime history of depression | 18 (82%) | 76 (77%) | 0.61 |
| History of drug abuse† | 2 (9%) | 7 (7%) | – |
| History of PTSD | 8 (36%) | 20 (20%) | 0.10 |
| PHQ-8 (↓0–24) | 12.2±3.6 | 8.9±3.3 | <0.001 |
| PHQ-8 (Physiological Domain)‡ | 6.8±3.0 | 6.0±2.6 | 0.24 |
| PHQ-8 (Psychological Domain)‡ | 6.9±2.1 | 2.9±1.9 | <0.001 |
| Receiving medications or counseling for depression or anxiety, %§ | 18 (82%) | 40 (40%) | <0.001 |
| Symptoms improved with medications or counseling, % | 17 (94%) | 33 (83%) | 0.22 |
| Psychological well-being | |||
| HADS-depression (↓0–21) | 11.0±3.4 | 6.4±3.5 | <0.001 |
| HADS-anxiety (↓0–21) | 9.4±3.0 | 6.7±3.9 | 0.003 |
| SF-36 mental component (0–100↑) | 37.8±6.3 | 43.4±8.9 | 0.005 |
| CRQ-emotional functioning (7–49↑) | 24.1±5.6 | 28.4±7.1 | 0.009 |
| MOS Social Support Scale (0–100↑) | 58.8±29.0 | 61.0±28.0 | 0.73 |
| Engagement in self-care | |||
| CRQ-Mastery (4–28↑) | 15.5±4.5 | 18.4±5.7 | 0.03 |
| Patient Activation Measure (0–40↑) | 21.5±5.3 | 23.6±5.0 | 0.08 |
Notes:
SI assessed by PHQ-9 item: “Being bothered by thoughts that you would be better off dead or of hurting yourself in some way”. Four of the 22 SI patients reported SI at follow-up study visit 1 year after baseline
chi square not done for cells <5 counts
PHQ-9 Physiological Domain includes items #3, 4, 5, 7, and 8 and Psychological Domain includes items #1, 2, and 6
11% of the total sample was on both antidepressants and anxiolytics. Arrows next to instrument score range indicate direction of better scores. The upward arrow shows that “higher scores indicate better health status on the measure”. The downward arrow shows that “lower scores indicate better health status on the measure”.
Abbreviations: $20K, $20,000; COPD, chronic obstructive pulmonary disease; CRQ, Chronic Respiratory Questionnaire; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; HADS, Hospital Anxiety and Depression Scale; MOS, Medical Outcomes Study; O2, oxygen; PHQ, Patient Health Questionnaire; SF-36, Medical Ouctome Study Short-Form-36; SI, suicide ideation; PTSD, post-traumatic stress disorder.
There were no significant differences between groups in lifetime history of depression, drug abuse or post-traumatic stress disorder (PTSD), or the PHQ-8 physiological domain score. Participants with SI had significantly more emotional distress on all scales that measured depression, anxiety, and psychological well-being compared to participants without SI (P<0.05) and were more likely to be receiving treatment for anxiety and/or depression (P=0.001) but equally likely (P=0.22) to report that treatment helped, despite ongoing high levels of symptoms. Levels of mastery and activation for self-care were lower for participants reporting SI compared to those without SI.
Qualitative themes
Qualitative information about patient experiences with SI (n=22), gleaned from the depression interviews and triangulated with the quantitative data were related to: 1) recent hospitalization for COPD exacerbation or other medical problem and 2) untreated depression or persistence of depression despite treatment. Four additional themes not already captured in the standardized instruments emerged during the SI safety interviews: 3) adverse life situations, including chronic psychosocial difficulties such as history of abuse, PTSD, and other mental health issues; 4) loss of a key relationship; 5) experience of disability; and 6) poor communication with providers (Figure 1). These themes are described in further detail below.
Figure 1.
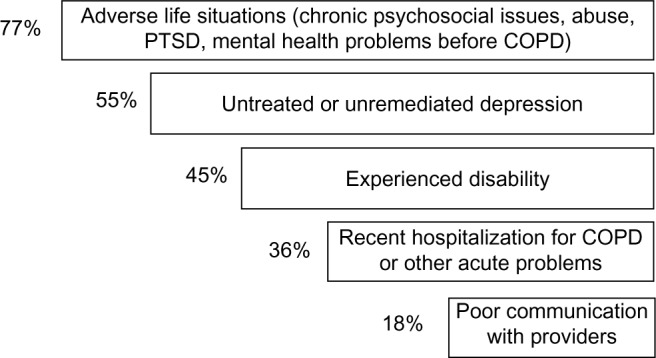
Percentage of subjects who endorsed any of the five major themes as a primary or secondary reason for reporting suicide ideation (n=22).
Abbreviations: COPD, chronic obstructive pulmonary disease; PTSD, post-traumatic stress disorder.
Recent hospitalization for COPD exacerbation or other medical problems
Serious, unexpected health events related to COPD or other major illness were often cited as one of the precipitating events for suicidal thoughts. One participant reported, “I was hospi-talized for blood clots in my lungs two months ago. I wasn’t all that concerned about my health before that, but now I am pretty worried. After that I started thinking that maybe I didn’t want to be here anymore.” Another participant stated, “I hate the hospital. When I had to go in last month with pneumonia, I hit the wall and felt like I snapped a bit. I never want to go back to the hospital. I wish the good Lord would just take me now so I don’t have to put up with this anymore.”
The four participants reporting SI during their year one study visit all articulated that worsening of their COPD that resulted in a recent hospitalization was a major causal factor. One said,
I’ve been sick five times in the last seven months. I’ve been in the hospital twice. I watched my mother die of COPD – literally. My health is declining. I know what’s happening. I know I’m near the end. My mind is getting worse, too. My husband tells me I have Alzheimer’s. I just want things to end – I just want it to all be over sometimes.
This participant had struggled with depression off and on since age 10 and had suicidal thoughts before, but not for a long time – until her recent decline in health.
Persistent or untreated depression
While it would be reasonable to think that participants who were currently in treatment for depression would be experiencing less severe emotional symptoms, this was not necessarily the case. Many participants reporting SI were already in treatment with antidepressant (and sometimes anxiolytic) medication and/or psychotherapy or counseling. One participant stated, “I have struggled with depression on and off for many years, so I often think that it would be better if I just wasn’t here. I have been in way worse shape than I am right now, so it doesn’t seem so bad at the moment in comparison to where I have been.” While this statement seems to suggest that the participant’s depression is not as severe as it has been in the past, he/she is still experiencing SI.
A second participant also reported lifelong difficulties with depression and related, “I don’t have anyone to talk to about these thoughts. My husband and my daughter just dismiss them whenever I bring anything like this up.” Another participant reported never having depression before reported suicidal thoughts, stating, “I’ve been sick a lot lately with my COPD. I hate the hospital and I had to go a few times because I had pneumonia and what not. It got me thinking that maybe I would be better off just kicking the bucket now and saving me all this worry.” Despite ongoing treatment for 82% of those reporting SI, SI was still current and many continued to have high levels of depression.
Adverse life situations, including chronic psychosocial issues, abuse, PTSD, and other mental health issues
Participants often reported having experienced family abuse by a parent, partner, or both, and/or had at least one alcoholic parent. One patient stated, “I was raped when I was eight years old and then was molested a bunch of other times by my dad. That, you know, would make someone depressed.” Another participant stated that it was the family dynamics generated by her father’s alcoholism that led her to attempt suicide five or six times during her youth, including checking herself into a hospital when she felt like she wanted to kill herself. She stated, “It would have been enough if it stopped there. I also had a husband who stalked me after abusing me during our marriage.” Yet another participant reported that her abusive father and alcoholic mother fought all the time. “I used to see my mother get beaten up by my father regularly,” she stated. Clearly, for these participants, long-term effects of family violence and alcoholism were familiar and lingering dynamic contextual factors linked to their current SI.
While many study participants had at least one episode of clinical depression in the past, including some without current depression, those reporting current SI often described their experience of depression as a lifelong struggle. One patient stated, “I’ve been married six times, so yeah, I have struggled with depression most of my lifetime.” Many participants reported that they had had trouble with depression since their teenage years or even earlier. “I never intended to live this long,” stated one patient, thus depicting the depth of lifelong suffering related to depression. She went on to say:
I tried to kill myself multiple times; once I almost succeeded but basically by accident. I was standing on a chair to take a crystal off the chandelier at home because they were sharp and I was going to slit my wrist with it. I slipped off the chair, causing the entire chandelier to come crashing down and it shattered on the floor and all around me. I was so badly cut up that when they found me they had to rush me to the hospital because I had lost so much blood.
Still other participants reported that they had been diagnosed with PTSD prior to developing COPD. “Then I got diagnosed with PTSD, which I have struggled with ever since,” articulated one participant after depicting an experience of rape and molestation. Yet another participant discussed the impact of serving in Vietnam, stating,
I came back and they didn’t have a word for why I was having a hard time. I guess they called it “Post-Vietnam Syndrome.” It wasn’t until years later that they assessed me for PTSD and diagnosed me with it. It’s what I had all along, but they didn’t call it that at first. But I’ve had trouble with depression since then.
Still another participant said, “My mother was kind of crazy. She had a lot of undiagnosed mental problems. She would hit me and my other siblings, and she did a lot of, you know, what’s that called … mental abuse stuff. I think it was because of that that I have PTSD.”
Relationship loss
Two participants related “wanting to join a (deceased) spouse on the other side.” Neither reported a plan or intent to harm themselves, but losing their partner took away a reason to live. One said, “Once my wife passed, I was so sad and lonely, and I really just wanted to be with her again. That was eight years ago, but I still go to sleep every night hoping that I won’t wake up the next morning. I’m not going to try to end my life, but I am ready.”
Experience of disability
Many participants with SI described difficulty coping with the challenges of disease-related disability, often framed in terms of being tired of the daily struggle with their limitations, expressing thoughts of wanting to “move on,” or “enter the next phase,” or simply to “not have to do this anymore.” While these statements do not convey overt intent to commit suicide, it is nevertheless clear that these participants were ready to be done with suffering, worry, exertion, and pain. They expressed a desire to move beyond their current daily experience to something else, “something beyond.” One participant reported, “I’m actually chicken. I attempted suicide twice a long time ago, but I could never actually go through with it. Even though my depression has gotten worse as I have gotten older, I have not tried to kill myself in a long time. And I won’t try it again. I hate pain.” Another participant mentioned that, “It might be time to move on to the next life, past being here on earth. I don’t plan to hurt myself, but maybe it’s time to move on.”
Poor communication with providers
Some participants reported that their health care providers were unreceptive to attempts to discuss their experience of illness and suicidal thoughts. When one participant was asked what her doctor said about her disease and her feelings about her life, she responded, “My pulmonologist doesn’t care. She just dismisses what I’m saying and changes the topic. She doesn’t want to talk about how I feel about it. She is not supportive. So I just don’t bring it up anymore.” Another participant articulated, “He doesn’t give a shit. I don’t think anyone would give a shit if I was gone tomorrow, least of all him. He just starts squirming when I talk about feeling like I want to give up and feel hopeless. It’s gonna make him go over his (allotted appointment) time with me to talk about it, you know.”
Yet another participant described that she left her provider in favor of a new one due to a lack of attention to her thoughts and feelings. “He just wasn’t listening to what I was saying. He kept asking questions that weren’t related to what I was talking about. He kept skirting the issue of me feeling like I wanted this to all be over. I guess he just didn’t want to hear it. That was enough for me. I had to see someone else.” A final participant stated, “I just stopped bringing it up-feeling down and hopeless and not wanting to do anything. I think she thought it was just about the COPD. But it’s (about more than that).”
Discussion
In this study, we found in the quantitative analyses that suicidal thoughts were common among patients with COPD and that suicidal ideation was associated with more severe depression, comorbid mental illness such as anxiety, more frequent COPD hospitalizations, more severe dyspnea, and less engagement in self-care despite similar disease severity as measured by lung function and need for supplemental oxygen. The qualitative analyses supported the quantitative results in that patients with SI reported that recent hospitalizations, disability, and persistent severe depression were important contributors to SI. In addition, the qualitative analysis also found that adverse life situations, loss of a key relationship such as a spouse, and difficulty communicating with their provider about these issues were important themes for patients with SI.
Our study builds on the findings of two large epidemiologic studies which found that COPD is associated with an increased risk of suicide. A longitudinal observational cohort study from Sweden found that a diagnosis of COPD was independently associated with a more than twofold increased risk of suicide among both men and women even after adjusting for psychiatric and somatic disorders.12 A nested case-control study in family practices in England also found that COPD was associated with nearly twofold increased odds of suicide, and that the risk may be higher in women and likely mediated by depression.13 Another population-based study in the United States found that COPD was associated with both suicidal ideation and suicide attempts16 at some point in patients’ lifetime. After adjustment, the association between COPD and suicide attempts had an odds ratio of 2.43 (95% confidence interval, 1.02–5.77). Although this US study used self-reported COPD and focused on a past history of suicidal ideation, it supports our findings that more than 10% of patients had current thoughts of suicide within the last 2 weeks.
As expected, people with SI are depressed and many meet criteria for major depression based on their PHQ-9 scores. Most participants reporting SI were already in treatment for depression and/or other mental health problems, either with antidepressant (with or without anxiolytic) medication, psychotherapy/counseling, or both. In spite of treatment, however, these patients with SI continued to have high levels of depressive symptomatology, indicating inadequate therapeutic response. In addition, although most patients (n=19) with SI had a PHQ-9 ≥10 consistent with major depression, three had “minor” depression (PHQ-9 <10).
The qualitative analyses suggested that COPD patients with SI may have difficulty engaging their health care providers in discussion of their illness experience and outlook, leaving them without the comprehensive clinical assistance they consider vital. Providers may contribute to this by assuming, incorrectly, that depression is an understandable reaction to COPD.32 While dealing with COPD does pose powerful adaptive challenges for patients, depression and SI are not inevitable and require an effective clinical response that starts with increased provider awareness of depression, suicide ideation, and suicide risk in COPD, and understanding that these problems are not the direct result of having COPD but of a separate but interacting comorbid condition.
We also found that many individuals with COPD and SI have complex emotional histories and psychosocial difficulties not limited to depression, including PTSD, a history of abuse and/or neglect, unstable or strained relationships, and other psychosocial difficulties. They also had more frequent hospitalizations for COPD in the past year, and several reported that being in the hospital was a particularly stressful event, even reporting PTSD-like responses to hospitalization. In addition, COPD exacerbations may lead to increased disability which we found was also associated with SI. The period following hospitalization appears to heighten vulnerability to depression and suicidal thoughts for patients with COPD.
Importantly, we assessed for suicidal thoughts with an interviewer-administered questionnaire, the PHQ-9. Although not specifically designed to be a screen for potential suicide, a large study of 84,418 outpatients who were administered the PHQ-9 found that any positive response to PHQ-9 questions about SI was prospectively associated with an increased risk of suicide attempt or suicide death.18 Even after adjusting for treatment history and severity of depressive symptoms, patients who reported “several days” of thoughts of SI in the last 2 weeks had a more than twofold increased risk of suicide attempt or death. This supports our use of the PHQ-9 question on SI as a marker of increased risk of suicide in these patients, and argues against the impression that SI is an expected finding among those with a severe chronic illness.
There are several potential limitations to our study. This analysis was not the primary aim of our study, and we therefore did not power it on understanding the factors associated with SI in patients with COPD. It is therefore possible that we were underpowered to detect some differences between patients with and without SI. Because of the main study exclusion criteria (eg, patients were able to ambulate, no chronic oral steroid use), our findings may not be generalizable to all COPD patients. In addition, although we did not a priori design this portion of the study using specific qualitative analyses methods, we report these findings because we unexpectedly found a high prevalence of suicidal ideation during the course of this study. The in-depth notes collected as part of the research protocol to further assess SI in these patients allowed us to better understand the associated factors.
Given the very limited existing data on factors associated with suicide in COPD, we believe that our results raise important issues regarding the treatment of depression in COPD. These quantitative and qualitative findings reinforce the need to identify depression in all clinical settings where patients with COPD receive their care, but argue for a much more nuanced approach to assessment and treatment than is possible with simple screening tools like the PHQ-9. Such an approach would share a common framework with palliative care,33,34 including elicitation of individuals’ experience of their illness, disability, and health care providers; history of traumatic experiences, both related to and separate from COPD; psychosocial as well as psychological and psychiatric management; and facilitation of patient-provider communication to allow productive exchange about topics that are awkward or painful.
Conclusion
In summary, we found that suicidal ideation was common and associated with more severe depressive symptoms and coexisting other mental illness, more frequent COPD hospitalizations, increased dyspnea and disability, as well as adverse life situations, loss of a key relationship such as with a spouse, and difficulty communicating with their provider. These findings emphasize the importance of awareness of SI in COPD patients among all providers and consideration of a comprehensive team-based treatment approach for patients with depression to include specialists, primary care, and mental health providers.
Acknowledgments
We would like to express our heartfelt gratitude to all the study participants. This work was supported in part by: 5R01HL093146 and UL1RR025014. Dr Fan has funding through the Department of Veterans Affairs.
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.
Author contributions
Dr Fan and Dr Borson contributed substantially to the study design, data analysis and interpretation, and the preparation of this manuscript. Dr Fan had full access to the data and will vouch the integrity of the work as a whole, from inception to published article. Ms Fleehart and Dr Nguyen contributed substantially to the study design, data analysis and interpretation, and the preparation of this manuscript. Dr Herting, Dr Kohen, Dr Matute-Bello, Dr Pagalilauan, and Dr Adams contributed to the interpretation and preparation of this manuscript. Ms Lee contributed to the data acquisition and preparation of this manuscript.
Disclosure
Sandra G Adams, MD, MS, FCCP, discloses the following affiliations and funding sources: Investigator/Grant Research: National Institute of Health, Veterans Affairs Cooperative Studies Program, Bayer Pharmaceuticals Corp; Boehringer Ingelheim Pharmaceuticals, Inc.; Centocor Inc., GlaxoSmithKline; Novartis Pharmaceuticals AG; Pfizer Inc.; Schering-Plough Corp; Honoraria for Speaking at Continuing Education Programs (Unrestricted Grants for Continuing Education): AstraZeneca Pharmaceuticals LP; Bayer Pharmaceuticals Corp; Boehringer Ingelheim Pharmaceuticals, Inc.; GlaxoSmithKline; Novartis Pharmaceuticals AG; Pfizer Inc.; Schering-Plough Corp. The other authors report no conflicts of interest in this work.
References
- 1.Ng TP, Niti M, Tan WC, Cao Z, Ong KC, Eng P. Depressive symptoms and chronic obstructive pulmonary disease: effect on mortality, hospital readmission, symptom burden, functional status, and quality of life. Arch Intern Med. 2007;167(1):60–67. doi: 10.1001/archinte.167.1.60. [DOI] [PubMed] [Google Scholar]
- 2.Norwood R. Prevalence and impact of depression in chronic obstructive pulmonary disease patients. Curr Opin Pulm Med. 2006;12(2):113–117. doi: 10.1097/01.mcp.0000208450.50231.c6. [DOI] [PubMed] [Google Scholar]
- 3.van Ede L, Yzermans CJ, Brouwer HJ. Prevalence of depression in patients with chronic obstructive pulmonary disease: a systematic review. Thorax. 1999;54(8):688–692. doi: 10.1136/thx.54.8.688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Manen JG, Bindels PJ, Dekker FW, IJzermans CJ, van der Zee JS, Schade E. Risk of depression in patients with chronic obstructive pulmonary disease and its determinants. Thorax. 2002;57(5):412–416. doi: 10.1136/thorax.57.5.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Di Marco F, Verga M, Reggente M, et al. Anxiety and depression in COPD patients: The roles of gender and disease severity. Respir Med. 2006;100(10):1767–1774. doi: 10.1016/j.rmed.2006.01.026. [DOI] [PubMed] [Google Scholar]
- 6.de Voogd JN, Wempe JB, Koeter GH, et al. Depressive symptoms as predictors of mortality in patients with COPD. Chest. 2009;135(3):619–625. doi: 10.1378/chest.08-0078. [DOI] [PubMed] [Google Scholar]
- 7.Coventry PA, Gemmell I, Todd CJ. Psychosocial risk factors for hospital readmission in COPD patients on early discharge services: a cohort study. BMC Pulm Med. 2011;11:49. doi: 10.1186/1471-2466-11-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dahlen I, Janson C. Anxiety and depression are related to the outcome of emergency treatment in patients with obstructive pulmonary disease. Chest. 2002;122(5):1633–1637. doi: 10.1378/chest.122.5.1633. [DOI] [PubMed] [Google Scholar]
- 9.Xu W, Collet JP, Shapiro S, et al. Independent effect of depression and anxiety on chronic obstructive pulmonary disease exacerbations and hospitalizations. Am J Respir Crit Care Med. 2008;178(9):913–920. doi: 10.1164/rccm.200804-619OC. [DOI] [PubMed] [Google Scholar]
- 10.Fan VS, Ramsey SD, Giardino ND, et al. Sex, depression, and risk of hospitalization and mortality in chronic obstructive pulmonary disease. Arch Intern Med. 2007;167(21):2345–2353. doi: 10.1001/archinte.167.21.2345. [DOI] [PubMed] [Google Scholar]
- 11.Abrams TE, Vaughan-Sarrazin M, Van der Weg MW. Acute exacerbations of chronic obstructive pulmonary disease and the effect of existing psychiatric comorbidity on subsequent mortality. Psychosomatics. 2011;52(5):441–449. doi: 10.1016/j.psym.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 12.Crump C, Sundquist K, Sundquist J, Winkleby MA. Sociodemographic, psychiatric and somatic risk factors for suicide: a Swedish national cohort study. Psychol Med. 2014;44(2):279–289. doi: 10.1017/S0033291713000810. [DOI] [PubMed] [Google Scholar]
- 13.Webb RT, Kontopantelis E, Doran T, Qin P, Creed F, Kapur N. Suicide risk in primary care patients with major physical diseases: a case-control study. Arch Gen Psychiatry. 2012;69(3):256–264. doi: 10.1001/archgenpsychiatry.2011.1561. [DOI] [PubMed] [Google Scholar]
- 14.Mykletun A, Stordal E, Dahl AA. Hospital Anxiety and Depression (HAD) scale: factor structure, item analyses and internal consistency in a large population. Br J Psychiatry. 2001;179:540–544. doi: 10.1192/bjp.179.6.540. [DOI] [PubMed] [Google Scholar]
- 15.Sheikh JI, Yesavage JA. Clinical Gerontology: A Guide to Assessment and Intervention. New York: The Haworth Press; 1986. Geriatric Depression Scale (GDS): Recent evidence and development of a shoter version; pp. 165–173. [Google Scholar]
- 16.Goodwin RD. Is COPD associated with suicide behavior? J Psychiatr Res. 2011;45(9):1269–1271. doi: 10.1016/j.jpsychires.2011.01.014. [DOI] [PubMed] [Google Scholar]
- 17.Spitzer RL, Williams JB, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA. 1994;272(22):1749–1756. [PubMed] [Google Scholar]
- 18.Simon GE, Rutter CM, Peterson D, et al. Does response on the PHQ-9 Depression Questionnaire predict subsequent suicide attempt or suicide death? Psychiatr Serv. 2013;64(12):1195–1202. doi: 10.1176/appi.ps.201200587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nguyen HQ, Fan VS, Herting J, et al. COPD Patients with Higher Levels of Anxiety Are More Physically Active. Chest. 2013;144(1):145–151. doi: 10.1378/chest.12-1873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 22.Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID). I: History, rationale, and description. Arch Gen Psychiatry. 1992;49(8):624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- 23.Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 24.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996;34(1):73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 26.Williams JE, Singh SJ, Sewell L, Guyatt GH, Morgan MD. Development of a self-reported Chronic Respiratory Questionnaire (CRQ-SR) Thorax. 2001;56(12):954–959. doi: 10.1136/thorax.56.12.954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Uebelacker LA, German NM, Gaudiano BA, Miller IW. Patient health questionnaire depression scale as a suicide screening instrument in depressed primary care patients: a cross-sectional study. The primary care companion to CNS disorders. 2011;13(1) doi: 10.4088/PCC.10m01027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kroenke K, Spitzer RL. The PHQ-9: A New Depression Diagnostic and Severity Measure. Psychiatric annals. 2002;32(9) [Google Scholar]
- 29.Giardino ND, Curtis JL, Andrei AC, et al. Anxiety is associated with diminished exercise performance and quality of life in severe emphysema: a cross-sectional study. Respir Res. 2010;11:29. doi: 10.1186/1465-9921-11-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 31.Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40(6 Pt 1):1918–1930. doi: 10.1111/j.1475-6773.2005.00438.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hegerl U, Mergl R. Depression and suicidality in COPD: understandable reaction or independent disorders? Eur Respir J. 2014 doi: 10.1183/09031936.00193213. [DOI] [PubMed] [Google Scholar]
- 33.Lanken PN, Terry PB, Delisser HM, et al. An official American Thoracic Society clinical policy statement: palliative care for patients with respiratory diseases and critical illnesses. Am J Respir Crit Care Med. 2008;177(8):912–927. doi: 10.1164/rccm.200605-587ST. [DOI] [PubMed] [Google Scholar]
- 34.Rocker GM, Sinuff T, Horton R, Hernandez P. Advanced chronic obstructive pulmonary disease: innovative approaches to palliation. Journal of palliative medicine. 2007;10(3):783–797. doi: 10.1089/jpm.2007.9951. [DOI] [PubMed] [Google Scholar]


