Abstract
Background
Hospice use has increased substantially during the past decade by an increasingly diverse patient population; however, little is known about patterns of hospice use and how these patterns have changed during the past decade.
Objective
To characterize Medicare hospice users in 2000 and 2010 and estimate the prevalence of 1) very short (one week or less) hospice enrollment, 2) very long (more than 6 months) hospice enrollment, and 3) hospice disenrollment and how these utilization patterns have varied over time and by patient and hospice characteristics.
Research Design
Cross-sectional analysis of Medicare hospice claims data from 2000 and 2010.
Subjects
All U.S. Medicare Hospice Benefit enrollees in 2000 (N=529,573) and 2010 (N=1,150,194).
Results
As of 2010, more than half (53.4%) of all Medicare decedents who used hospice had either very short (one week or less, 32.4%) or very long (more than 6 months, 13.9%) hospice enrollment or disenrolled from hospice prior to death (10.6%). This represents an increase of 4.9 percentage points from 2000. In multivariable analysis, patients with non-cancer diagnoses, the fastest growing group of hospice users, were approximately twice as likely as those with cancer to have very short or long enrollment periods and to disenroll from hospice.
Conclusion
The substantial proportion of hospice users with very short or long enrollment, or enrollments that end prior to death, underscores the potential for interventions to improve the timing and appropriateness of hospice referral so that the full benefits of hospice are received by patients and families.
Keywords: Hospice, Medicare Hospice Benefit, health services research
Introduction
The diversity of the patient population using hospice has increased dramatically during the past decade in terms of patient diagnosis, age, race, and geographic region.1 Although increased use of hospice for individuals with a range of diagnoses and demographic characteristics is generally perceived to be positive for patients and families, recent studies have also documented concerning patterns of hospice use including late referral to hospice, exceedingly long hospice enrollment, and hospice disenrollment.1-5 There have been no national studies, however, to comprehensively examine the prevalence of these hospice utilization patterns in one dataset and to compare contemporary national data with historical data to understand how these patterns may have shifted over time.
One concerning pattern of hospice use is having particularly short or long enrollment periods. Short hospice enrollment (i.e., receiving hospice care for one week or less) may not allow enough time for the patient and family to experience the full benefit of the hospice care team and is associated with poor outcomes for patients and families.6-9 Exceedingly long hospice enrollment (i.e., receiving hospice care for more than 6 months) may indicate inappropriate referral to hospice although the impact on patients and families is unknown. The Centers for Medicare & Medicaid Innovation Center's recent announcement10 of a pilot program to evaluate the timing of hospice initiation demonstrates the urgent need to address potential barriers to timely and appropriate hospice use.
A second pattern of hospice use associated with poor outcomes for patients and families is hospice disenrollment. An estimated 8-18% of patients each year disenroll from hospice3,11-15 and the disenrollment rate at hospice agencies has been found to range from 0% at some hospices to 38% at others,3 with for-profit hospices having higher disenrollment rates than nonprofit hospices.11,15 Although hospice disenrollment may be initiated by either the patient (for example, if the patient wishes to pursue curative care or is dissatisfied with hospice) or the hospice (for example, if the patient no longer meets eligibility criteria or to avoid costly hospitalizations), some have suggested that increasing use of hospice has resulted from enrollment of patients who are not expected to die within 6 months.2 It is also generally believed that hospice disenrollment is primarily driven by patients with diagnoses other than cancer, for whom accurate prognostication is more difficult. We lack data, however, on the extent to which hospice disenrollment rates have changed over the last decade as the proportion of hospice users with non-cancer diagnoses has increased.
To address these gaps, we analyzed data from all fee-for-service Medicare beneficiaries who used hospice in 2000 and 2010, which comprises 84% of all hospice users in the U.S.1 We estimated hospice use by region and describe the characteristics of hospice users and how they have changed during the past decade. We determined the prevalence of hospice utilization patterns including very short and very long hospice enrollment, and hospice disenrollment and identified the patient-level and hospice-level factors associated with these patterns. To the extent that increasing use of hospice reflects increases in very short or very long enrollment periods, or increases in the proportion of patients who disenroll, interventions to improve the timing and appropriateness of hospice referral may be warranted.
Methods
Study Design and Sample
We conducted a cross-sectional analysis using Medicare hospice claims data for all fee-for-service Medicare beneficiaries who used hospice in 2000 (N=529,573) and all who used hospice in 2010 (N=1,150,194). We calculated hospice use in total and by region using the Medicare hospice claims for decedents in 2000 and 2010 combined with data from the Centers for Disease Control and Prevention (CDC) regarding U.S. deaths for individuals age 65 and older in 2000 and 2010.16 For analyses of hospice utilization patterns (i.e., length of hospice enrollment and hospice disenrollment), we used the subsample of all fee-for-service Medicare beneficiaries who first enrolled with hospice in the first quarter of 2000 (N=119,564) and the first quarter of 2010 (N=245,777) to ensure that we had a long enough follow-up period to measure length of enrollment and disenrollment in that calendar year. We obtained hospice ownership information by linking by hospice provider number in the Medicare hospice claims data to the Medicare Provider of Services data for 2000 and 2010.
Measures
We calculated hospice use for decedents aged 65 and older in total and by region in 2000 and 2010 by dividing the number of Medicare decedents who died while enrolled with hospice (obtained from the Medicare hospice claims) by the total number of decedents in the U.S. aged 65 and older (obtained from the CDC) . We measured the length of hospice enrollment as the number of days from the individual's hospice start date on their first hospice claim to their death or hospice disenrollment. For the subset of individuals with multiple hospice enrollment periods, we measured the length of hospice enrollment as the sum of all enrollment periods. We identified individuals as having disenrolled from hospice if: 1) they had only one hospice enrollment period and the patient status indicator code on the final hospice claim indicated that the patient was discharged (rather than died) and there was no date of death on the final hospice claim; or 2) if they had more than one hospice enrollment period.
Patient demographic characteristics were gender, age (categorized as <65, 65-69, 70-74, 75-79, 80-84, and >=85), and race/ethnicity (white, black, Hispanic, Asian, other). The individual's primary diagnosis was based on International Classification of Diseases, Ninth Revision (ICD-9) codes and categorized as follows: (neoplasms; mental disorders; diseases of the nervous system and sense organs; diseases of the circulatory system; diseases of the respiratory system; symptoms, signs, and ill-defined conditions; and other). We also included the year the individual received hospice care (2000 or 2010) and the census region in which the patient lived. Hospice agency characteristics were: ownership (for-profit, nonprofit, and government/other obtained from the Medicare Provider of Services file), and size (calculated from the Medicare claims data as the annual number of individuals cared for by the hospice categorized at the quartiles of the distribution as <250, 250-599, 600-1,299, and >=1,300).
Statistical Analyses
We summarized the characteristics of hospice users and the hospice agencies that cared for them in 2000 and 2010. We compared the prevalence of hospice utilization patterns (i.e., very short hospice enrollment, very long hospice enrollment, hospice disenrollment) by patient characteristics, hospice characteristics, and year using t-tests and chi-square tests, as appropriate. We used multivariable logistic generalized estimating equations (GEE)17 to estimate the associations between our outcomes and patient and hospice characteristics. All tests were performed using techniques to account for the clustering of patient observations within hospices. We performed all analyses using the statistical software SAS, version 9.2 (Cary, N.C.).
Results
Hospice Use
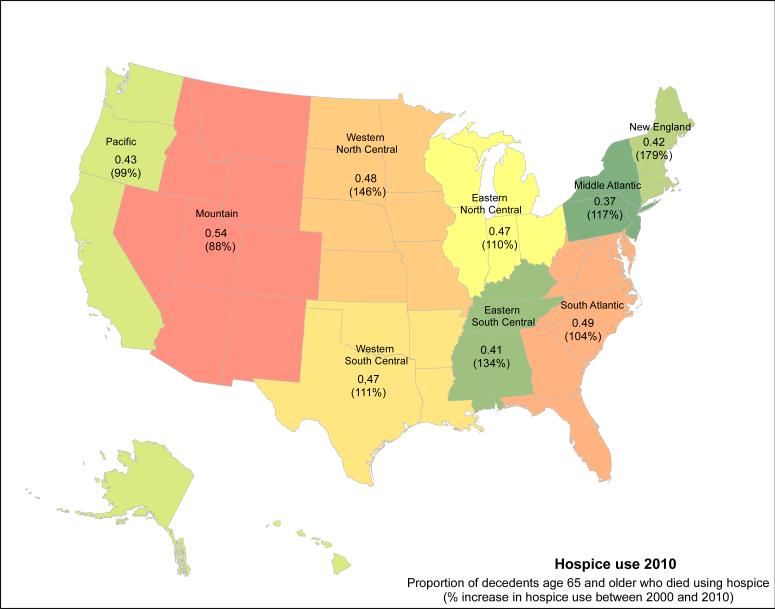
The percentage of Medicare decedents older than 65 years who received care from a Medicare-certified hospice increased from 15.9% in 2000 to 32.3% in 2010 and varied by region (Figure 1). The number of Medicare hospice users more than doubled during the decade (620,621 additional hospice users, a 117% increase) (Table 1). The proportion of hospice users age 85 and older increased more than any other age category. In 2010, hospice users age 85 and older comprised 46% of all hospice users and increased by 356,870 (or 203%) from 2000 to 2010. The proportion of hospice users by race remained fairly stable from 2000 to 2010 with approximately 88-89% of hospice users white, 7-8% black, 1-2% Hispanic, and 1-2% other races. The greatest increase in hospice use by primary diagnosis category was for individuals with “symptoms, signs and ill-defined conditions” (164,644 additional hospice users, a 501% increase). The second highest percentage increase in primary diagnosis category during the past decade was for individuals with a primary diagnosis of a mental disorder, which includes dementia (91,733 additional hospice users, a 327% increase).
Figure 1.
Hospice use 2010
Proportion of decedents age 65 and older who used hospice (% increase in hospice use between 2000 and 2010)
Table 1.
Characteristics of Medicare Beneficiaries who used Hospice, 2000 and 2010
| 2000 | % | 2010 | % | Change | % Change | |
|---|---|---|---|---|---|---|
| Number of Hospice Users | 529,573 | 1,150,194 | 620,621 | 117% | ||
| Gender | ||||||
| Female | 300,928 | 57% | 686,189 | 60% | 385,261 | 128% |
| Male | 228,645 | 43% | 464,002 | 40% | 235,357 | 103% |
| Age | ||||||
| <65 | 24,901 | 5% | 61,419 | 5% | 36,518 | 147% |
| 65-69 | 50,203 | 9% | 80,985 | 7% | 30,782 | 61% |
| 70-74 | 76,194 | 14% | 108,199 | 9% | 32,005 | 42% |
| 75-79 | 98,730 | 19% | 151,198 | 13% | 52,468 | 53% |
| 80-84 | 104,162 | 20% | 216,140 | 19% | 111,978 | 108% |
| 85+ | 175,383 | 33% | 532,253 | 46% | 356,870 | 203% |
| Race | ||||||
| White | 472,869 | 89% | 1,015,019 | 88% | 542,150 | 115% |
| Black | 39,151 | 7% | 91,921 | 8% | 52,770 | 135% |
| Hispanic | 6,401 | 1% | 18,664 | 2% | 12,263 | 192% |
| Asian | 2,604 | 0% | 9,751 | 1% | 7,147 | 274% |
| Other | 8,548 | 2% | 14,839 | 1% | 6,291 | 74% |
| Primary Diagnosis | ||||||
| Neoplasms | 264,735 | 50% | 346,703 | 30% | 81,968 | 31% |
| Mental disorders | 28,028 | 5% | 119,761 | 10% | 91,733 | 327% |
| Diseases of the nervous system and sense organs | 35,555 | 7% | 103,881 | 9% | 68,326 | 192% |
| Diseases of the circulatory system | 94,870 | 18% | 213,241 | 19% | 118,371 | 125% |
| Diseases of the respiratory system | 37,272 | 7% | 102,745 | 9% | 65,473 | 176% |
| Symptoms, signs, and ill-defined conditions | 32,849 | 6% | 197,493 | 17% | 164,644 | 501% |
| Other | 36,196 | 7% | 66,348 | 6% | 30,152 | 83% |
| Hospice Ownership | ||||||
| For-profit | 150,092 | 28% | 490,643 | 43% | 340,551 | 227% |
| Nonprofit | 361,253 | 68% | 539,146 | 47% | 177,893 | 49% |
| Government/other | 16,259 | 3% | 117,838 | 10% | 101,579 | 625% |
| Hospice Size: (annual number of patients) | ||||||
| <250 | 149,023 | 28% | 222,042 | 19% | 73,019 | 49% |
| 250-599 | 164,165 | 31% | 290,650 | 25% | 126,485 | 77% |
| 600-1299 | 110,975 | 21% | 308,120 | 27% | 197,145 | 178% |
| 1300+ | 105,410 | 20% | 329,382 | 29% | 223,972 | 212% |
| Region | ||||||
| New England | 20,659 | 4% | 52,128 | 5% | 31,469 | 152% |
| Middle Atlantic | 63,118 | 12% | 132,704 | 12% | 69,586 | 110% |
| Eastern North Central | 93,020 | 18% | 189,700 | 16% | 96,680 | 104% |
| Western North Central | 36,716 | 7% | 85,228 | 7% | 48,512 | 132% |
| South Atlantic | 112,273 | 21% | 252,964 | 22% | 140,691 | 125% |
| Eastern South Central | 32,965 | 6% | 77,308 | 7% | 44,343 | 135% |
| Western South Central | 61,953 | 12% | 134,915 | 12% | 72,962 | 118% |
| Mountain | 38,439 | 7% | 84,637 | 7% | 46,198 | 120% |
| Pacific | 70,430 | 13% | 140,610 | 12% | 70,180 | 100% |
Consistent with reports regarding the increase in the number of for-profit hospices in the U.S. in the past decade,1,18 the number of individuals cared for by for-profit hospices more than tripled while the increase in the number of individuals cared for by nonprofit hospices increased 49% during the past decade. The proportion of individuals served by very small hospices declined to 19%, and the proportion served by the largest hospices increased to 29%. The region with the greatest increase in number of hospice users was the South Atlantic (Delaware, Florida, Georgia, Maryland, North Carolina, South Carolina, Virginia, West Virginia, and Washington, D.C.) with 140,691 additional hospice users in 2010 and in percentage terms the greatest increase (152% increase) in hospice users during the past decade was in the New England region (Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, Vermont).
Hospice Utilization Patterns
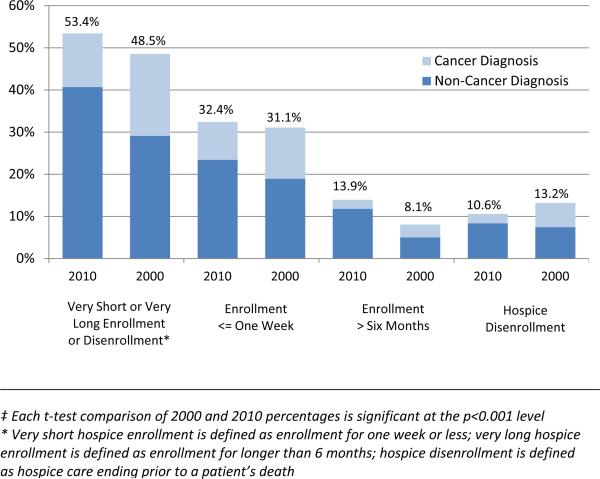
In 2010, more than half (53.4%) of hospice users were either enrolled for a very short or very long period of time or disenrolled prior to death, an increase from 48.5% in 2000 (Figure 2). Of hospice users with very short or very long enrollment periods or disenrollment, a consistently higher proportion had a non-cancer diagnosis than a cancer diagnosis and this differential increased from 2000 to 2010 for each hospice utilization pattern measured (Figure 2). In 2010, approximately (32.4%) of hospice users had a very short (less than or equal to one week) enrollment period, 13.9% had a very long enrollment period (more than 6 months) and 10.6% disenrolled (Figure 2). The proportion of hospice users who disenrolled from hospice prior to death has declined slightly (2.6 percentage points) over the past decade, primarily due to a decline in disenrollment for patients with cancer (4.3 percentage point decline). For hospice users with a non-cancer diagnosis, the proportion with either very short or very long enrollment or disenrollment is significantly higher than for patients with a diagnosis of cancer (59.0% versus 41.1% in 2010, p<0.001) (results not shown).
Figure 2.
Hospice Utilization Patterns By Primary Diagnosis, 2000 and 2010‡
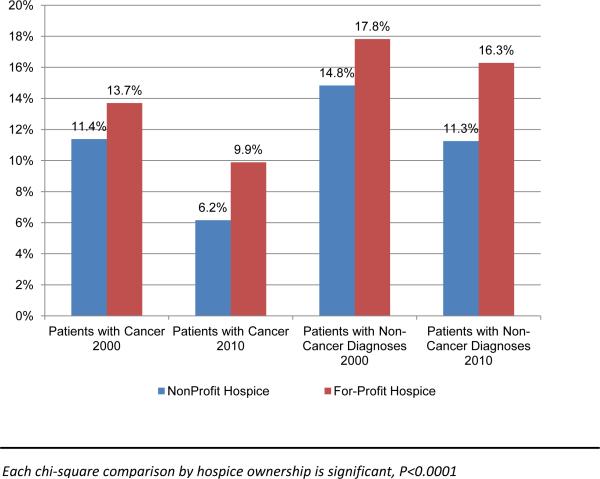
Almost all individuals (95.4% in 2000 and 93.2% in 2010) had a single stay with hospice. The proportion of patients who disenrolled from hospice and re-enrolled with hospice at a later date was 4.1% in 2000 and 6.0% in 2010. Fewer than 1% of patients in each year exhibited a pattern of more than two hospice enrollment and dis-enrollment episodes. Hospice disenrollment was significantly higher at for-profit compared with nonprofit hospices for both the subgroup of patients with cancer and the subgroup of patients with diagnoses other than cancer (Figure 3).
Figure 3.
Hospice Disenrollment Rates for Patients with Cancer versus Non-Cancer Diagnoses By Hospice Ownership, 2000 and 2010
Factors Associated with Patterns of Hospice Use
In multivariable analysis (Table 2), the strongest factor associated with having a very short or long enrollment period or hospice disenrollment prior to death was having a primary diagnosis other than cancer. Individuals with non-cancer diagnoses had approximately twice the odds of experiencing the hospice utilization patterns evaluated.
Table 2.
Multivariable Logistic Regression¥: Factors Associated with Hospice Utilization Patterns
| Very Short or Very Long Enrollment or Disenrollment* AOR (95%CI) | Enrollment <= One Week AOR (95%CI) | Enrollment > Six Months AOR (95%CI) | Hospice Disenrollment AOR (95%CI) | |
|---|---|---|---|---|
| Gender | ||||
| Female | 1.00 | 1.00 | 1.00 | 1.00 |
| Male | 1.04 (1.03, 1.06) * | 1.22 (1.20, 1.24) ‡ | 0.76 (0.74, 0.77) ‡ | 0.98 (0.96, 1.00) ‡ |
| Age | ||||
| <75 | 1.00 | 1.00 | 1.00 | 1.00 |
| 75-79 | 0.96 (0.94, 0.98) ‡ | 0.98 (0.96, 1.01) | 1.04 (1.00, 1.09) ‡ | 0.85 (0.82, 0.88) ‡ |
| 80-84 | 0.95 (0.93, 0.97) ‡ | 0.96 (0.93, 0.98) ‡ | 1.11 (1.07, 1.15) ‡ | 0.83 (0.80, 0.85) ‡ |
| 84+ | 0.95 (0.93, 0.96) ‡ | 0.93 (0.91, 0.95) ‡ | 1.24 (1.19, 1.28) ‡ | 0.74 (0.71, 0.76) ‡ |
| Race | ||||
| White | 1.00 | 1.00 | 1.00 | 1.00 |
| Black | 1.01 (0.98, 1.04) | 0.85 (0.82, 0.88) ‡ | 1.09 (1.04, 1.14) ‡ | 1.34 (1.29, 1.40) ‡ |
| Hispanic | 1.05 (0.99, 1.12) | 0.97 (0.90, 1.04) | 1.03 (0.96, 1.12) | 1.23 (1.13, 1.34) ‡ |
| Asian | 1.04 (0.96, 1.13) | 1.02 (0.94, 1.12) | 0.90 (0.78, 1.04) | 1.21 (1.08, 1.34) * |
| Other | 1.02 (0.96, 1.08) | 0.97 (0.91, 1.04) | 1.04 (0.94, 1.14) | 1.11 (1.01, 1.20) * |
| Primary Diagnosis | ||||
| Neoplasms | 1.00 | 1.00 | 1.00 | 1.00 |
| Mental disorders | 1.95 (1.89, 2.01) ‡ | 1.08 (1.04, 1.12) ‡ | 2.80 (2.67, 2.93) ‡ | 1.88 (1.79, 1.98) ‡ |
| Diseases of the nervous system and sense organs | 1.96 (1.90, 2.02) ‡ | 1.05 (1.00, 1.10) * | 3.07 (2.94, 3.20) ‡ | 1.80 (1.71, 1.89) ‡ |
| Diseases of the circulatory system | 2.15 (2.10, 2.20) ‡ | 1.74 (1.69, 1.79) ‡ | 1.68 (1.62, 1.75) ‡ | 1.91 (1.83, 1.99) ‡ |
| Diseases of the respiratory system | 2.46 (2.37, 2.54) ‡ | 1.94 (1.87, 2.02) ‡ | 1.86 (1.79, 1.95) ‡ | 1.77 (1.69, 1.85) ‡ |
| Symptoms, signs, and ill-defined conditions | 1.78 (1.73, 1.83) ‡ | 1.12 (1.07, 1.16) ‡ | 2.01 (1.92, 2.10) ‡ | 2.26 (2.15, 2.36) ‡ |
| Other | 2.45 (2.37, 2.54) ‡ | 2.82 (2.72, 2.91) ‡ | 0.70 (0.66, 0.75) ‡ | 1.64 (1.56, 1.72) ‡ |
| Hospice Ownership | ||||
| Nonprofit | 1.00 | 1.00 | 1.00 | 1.00 |
| For-profit | 1.07 (1.04, 1.11) ‡ | 0.82 (0.78, 0.85) ‡ | 1.54 (1.46, 1.62) ‡ | 1.13 (1.01, 1.26) ‡ |
| Hospice Size: (annual number of patients) | ||||
| <250 | 1.00 | 1.00 | 1.00 | 1.00 |
| 250 to <600 | 0.94 (0.90, 0.98) * | 1.24 (1.20, 1.29) ‡ | 0.85 (0.81, 0.89) ‡ | 0.66 (0.57, 0.76) ‡ |
| 600 to <1300 | 0.96 (0.91, 1.00) | 1.47 (1.40, 1.55) ‡ | 0.79 (0.75, 0.84) ‡ | 0.52 (0.44, 0.62) ‡ |
| 1300 or more | 1.00 (0.95, 1.05) | 1.58 (1.47, 1.69) ‡ | 0.79 (0.73, 0.86) ‡ | 0.62 (0.53, 0.72) ‡ |
| Year | ||||
| 2000 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2010 | 1.02 (0.99, 1.06) | 1.09 (1.05, 1.13) ‡ | 1.42 (1.36, 1.49) ‡ | 0.69 (0.62, 0.70) ‡ |
Multivariable model controls for all variables shown in the table in addition to region; multivariable model for hospice disenrollment also controls for the log of length of hospice stay
£ Very short hospice enrollment is defined as enrollment for one week or less; very long hospice enrollment is defined as enrollment for longer than 6 months; hospice disenrollment is defined as hospice care ending prior to a patient's death
AOR=Adjusted Odds Ratio; CI=Confidence Interval
p<0.0001
p<0.05
In terms of demographic factors, men were more likely to have very short hospice enrollment periods and less likely to have very long enrollment periods. Older individuals were less likely to have very short enrollment periods and to disenroll but were more likely to have very long enrollment periods. Individuals who were black were less likely to have very short hospice enrollment periods and more likely to have very long enrollment periods. Individuals who were non-white were significantly more likely to disenroll from hospice than those who were white.
For-profit hospice ownership and hospice size were both significantly associated with hospice utilization patterns. Individuals cared for by for-profit hospices were more likely to be enrolled for more than 6 months, were more likely to disenroll from hospice, but were less likely to enroll with hospice for one week or less compared with those cared for by nonprofit hospices. Individuals cared for by larger hospices were more likely to receive hospice for a week or less. Larger hospice size was inversely related to very long hospice stays (longer than 6 months) and hospice disenrollment.
Discussion
More than half of all patients used hospice either for very short or very long time periods or disenrolled prior to death. This proportion has increased almost 5 percentage points over the decade in conjunction with a two-fold increase in hospice use. Although we found that more traditional use of hospice (i.e., enrollment between one week and 6 months and ending in death) is more likely for patients with cancer compared with other diagnoses, the prevalence of more problematic patterns of hospice use for patients with cancer is also fairly high at 41%. The change in hospice utilization patterns in 2000 and 2010 may be due to a number of potentially counteracting effects. First, the growth of non-hospice palliative care options during the past decade19 may have acted as a substitute for hospice enrollment early in a patient's course of illness, leading to hospice referral only in the last week of life. Simultaneously, however, greater awareness and understanding during the past decade of the benefits and appropriate timing of hospice referral may have led to more timely hospice enrollment and reduced disenrollment. Additional research regarding these potential influences on the timing of hospice referral and disenrollment are needed.
Hospice use has increased substantially by individuals across almost all demographic and clinical categories. In absolute terms, the greatest increases were among individuals age 85 and older, individuals who are white, female, and for individuals with a primary diagnosis of “symptoms, signs, and ill-defined conditions”. The significant increase (164,644 individuals or 501% increase from 2000 to 2010) in the number of individuals enrolled with hospice with a primary diagnosis of “symptoms, signs, and ill-defined conditions” is likely one of the reasons the Center for Medicare & Medicaid Services (CMS) plans to restrict the use of non-specific, symptom-classified diagnoses such as “debility” and “adult failure to thrive” (the main sub-categories of “symptoms, signs and ill-defined conditions”) as the principal terminal diagnosis on hospice claims beginning in October 2014.20 Although the reason for this change is not clear, it may be that CMS does not consider these to be terminal diagnoses and is concerned that hospices are increasingly enrolling individuals who are chronically ill rather than terminally ill. It may also be that individualized, patient-centered plans of care are more difficult to develop for patients with these conditions and, consequently, the patient may not receive the full benefit of hospice services.
In terms of hospice agency characteristics, for-profit hospices, large hospices and hospices in the South Atlantic experienced the greatest increase in patients served. The increasing proportion of hospice users 85 years of age and older has important implications for hospice teams. Individuals 85 and older are more likely to have multiple chronic conditions relative to those younger than 8521 and may be more likely to have a caregiver who is also 85 or older and potentially less able to perform caregiver duties. The complexity and intensity of care required by a hospice may therefore be greater.
Our finding regarding the high prevalence of short hospice enrollment periods underscores the importance of the recently announced CCMI Medicare Care Choices pilot project.10 The pilot seeks to determine the impact of concurrent hospice and life-prolonging care on patient quality of care and Medicare expenditures. Although there may be numerous factors causing short hospice enrollment periods, including physician reluctance or delay in having conversations about hospice and patient and family difficulty in accepting a terminal diagnosis,4,22,23 the refusal of patients and families to stop life-prolonging treatment is likely a major barrier to earlier hospice enrollment.24 Our finding that almost one-third of patients with cancer, for whom prognostication is considered more accurate than for patients with non-cancer diagnoses,25-27 have short enrollment periods suggests that the prohibition against concurrent life-prolonging and palliative care is an important barrier to earlier enrollment. In fact, our earlier work has shown that a substantial proportion of hospices will not enroll patients who desire such concurrent care.28
Our study provides new results regarding how patient disenrollment varies by patient diagnosis and hospice ownership and how this has changed over the past decade. We find that although the patient disenrollment rate has declined during the past decade, it is consistently higher for patients with non-cancer diagnoses than for those with cancer and is higher for patients (both those with cancer and those with non-cancer diagnoses) cared for by for-profit hospices compared with non-profit hospices. Given evidence of poor outcomes for patients who disenroll from hospice including higher rates of emergency department admission and hospital death,12 hospice disenrollment rates and the reason for disenrollment should be a reportable hospice quality measure.
We found that an increasing proportion of hospice enrollment periods are longer than 6 months. The structure of Medicare's hospice payment system makes longer hospice enrollment more profitable for hospices than shorter enrollment periods,22 which may provide an incentive for hospices to pursue business models that maximize profit by enrolling patients more likely to have long stays,22,23 particularly for-profit hospices. From a patient quality perspective, the impact of very long hospice enrollment periods is unknown, however it may be that alternatives to hospice care, for example, outpatient palliative care, may be more appropriate than hospice enrollment for some individuals. The increase in long hospice stays, however, may have a negative effect on Medicare expenditures given that the greatest costs savings from hospice use occur with enrollment periods of 15-30 days.29 Regulatory measures, in addition to the existing aggregate annual cap,5 may be necessary to reverse the trend in long hospice enrollment periods.
Although the study has a number of strengths, including the two periods of data, the large sample size, and comprehensive approach of evaluating hospice utilization patterns, there are also limitations. For one, we are unable with our data to identify the reasons for differing hospice enrollment periods and hospice disenrollment. Future studies, which include patient and caregiver interviews, are needed to more thoroughly understand the hospice enrollment and disenrollment process. Second, our sample does not include individuals covered by managed care, private insurance, Medicaid, or charity care and thus our findings may not be generalizable to these groups. Our sample, however, reflects the 84% of patients and 88% of patient care days that are covered by the Medicare Hospice Benefit.1 Third, because this is a cross-sectional study of hospice users in 2000 and 2010, hospice stays that occur in the years prior to or after the years of our study will not be captured. For example, an individual who enrolls and disenrolls from hospice in 2009 and then re-enrolls in the first quarter of 2010 will have a hospice enrollment period that is calculated only for use in 2010. Given our finding that only 5-7% of hospice users have multiple hospice stays and our prior work finding that the median time from hospice disenrollment to re-enrollment is 28 days,12 this is not likely to materially impact our results. Similarly, because a small percentage (4% in 2000 and 8% in 2010) of our sample enrolled with hospice in the first quarter of the year, had very long hospice enrollment, and were still patients at the end of the calendar year, we do not know if they ultimately disenrolled from hospice and thus our estimates of hospice disenrollment may be understated. Finally, we estimated the associations between hospice utilization patterns and patient and hospice characteristics using odds ratios, which are higher than risk ratios given that study outcomes are common.
Increased use of hospice has the potential to provide high quality of care at the end of life to a growing number of patients and families. As the traditional hospice model of patients with cancer receiving hospice care from enrollment to death by local non-profit providers has transitioned into a much more diverse patient population served by a more diverse hospice provider population, there are persisting patterns of hospice use that are concerning. Currently, more than half of individuals who enroll with a hospice program receive care for either one week or less, more than 6 months, or stop hospice care prior to death. Recognition of these patterns and the impact that they have on hospices’ ability to provide high quality pain and symptom management and caregiver support through the end of life are largely unknown. Current demonstration projects are critical in understanding and potentially addressing the barriers to these utilization patterns through public education, provider education, and financial incentives to curb these less than ideal patterns of end-of-life care.
Acknowledgments
Funding/Support:
This study was supported by the National Institute of Nursing Research 5R01NR013499 (Aldridge); and the John D. Thompson Foundation (Bradley).
Contributor Information
Melissa D. Aldridge, Department of Geriatrics and Palliative Medicine, Icahn School of Medicine at Mount Sinai, One Gustave L. Levy Place, Box 1070, New York, NY 10029 and James J. Peters VA, Bronx, NY..
Maureen Canavan, Department of Health Policy and Management, Yale School of Public Health, 2 Church Street South, Suite 409, New Haven, CT 06520..
Emily Cherlin, Department of Health Policy and Management, Yale School of Public Health, 2 Church Street South, Suite 409, New Haven, CT 06520..
Elizabeth H. Bradley, Department of Health Policy and Management, Yale School of Public Health, 60 College Street 300A, New Haven, CT 06520-8034..
References
- 1. [November 2013];NHPCO Facts and Figures: Hospice Care in America. Available at: http://www.nhpco.org/sites/default/files/public/Statistics_Research/2013_Facts_Figures.pdf 2013.
- 2.Teno JM, Gozalo PL, Bynum JP, et al. Change in end-of-life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA. 2013;309:470–7. doi: 10.1001/jama.2012.207624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carlson MD, Herrin J, Du Q, et al. Hospice characteristics and the disenrollment of patients with cancer. Health Serv Res. 2009;44:2004–21. doi: 10.1111/j.1475-6773.2009.01002.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miller SC, Weitzen S, Kinzbrunner B. Factors associated with the high prevalence of short hospice stays. J Palliat Med. 2003;6:725–36. doi: 10.1089/109662103322515239. [DOI] [PubMed] [Google Scholar]
- 5.MedPac . Report to the Congress: Medicare Payment Policy: Chapter 12. Hospice Services; 2013. [Google Scholar]
- 6.Bradley EH, Prigerson H, Carlson MD, Cherlin E, Johnson-Hurzeler R, Kasl SV. Depression among surviving caregivers: does length of hospice enrollment matter? Am J Psychiatry. 2004;161:2257–62. doi: 10.1176/appi.ajp.161.12.2257. [DOI] [PubMed] [Google Scholar]
- 7.Kris AE, Cherlin EJ, Prigerson H, et al. Length of hospice enrollment and subsequent depression in family caregivers: 13-month follow-up study. Am J Geriatr Psychiatry. 2006;14:264–9. doi: 10.1097/01.JGP.0000194642.86116.ce. [DOI] [PubMed] [Google Scholar]
- 8.Rickerson E, Harrold J, Kapo J, Carroll JT, Casarett D. Timing of hospice referral and families' perceptions of services: are earlier hospice referrals better? J Am Geriatr Soc. 2005;53:819–23. doi: 10.1111/j.1532-5415.2005.53259.x. [DOI] [PubMed] [Google Scholar]
- 9.Miller SC, Mor V, Teno J. Hospice enrollment and pain assessment and management in nursing homes. J Pain Symptom Manage. 2003;26:791–9. doi: 10.1016/s0885-3924(03)00284-7. [DOI] [PubMed] [Google Scholar]
- 10. [April, 2014];Medicare Care Choices Model. 2014 (at http://innovation.cms.gov/initiatives/Medicare-Care-Choices/.)
- 11.Aldridge MD, Schlesinger M, Barry CL, et al. National Hospice Survey Results: For-Profit Status, Community Engagement, and Service. JAMA Internal Medicine, R&R. 2013 doi: 10.1001/jamainternmed.2014.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carlson MD, Herrin J, Du Q, et al. Impact of hospice disenrollment on health care use and medicare expenditures for patients with cancer. J Clin Oncol. 2010;28:4371–5. doi: 10.1200/JCO.2009.26.1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Casarett DJ, Marenberg ME, Karlawish JH. Predictors of withdrawal from hospice. J Palliat Med. 2001;4:491–7. doi: 10.1089/109662101753381638. [DOI] [PubMed] [Google Scholar]
- 14.Taylor DH, Steinhauser K, Tulsky JA, Rattliff J, Van Houtven CH. Characterizing Hospice Discharge Patterns in a Nationally Representative Sample of the Elderly, 1993-2000. Am J Hosp Palliat Care. 2008 doi: 10.1177/1049909107310136. [DOI] [PubMed] [Google Scholar]
- 15.Teno JM, Plotzke M, Gozalo P, Mor V. A National Study of Live Discharges from Hospice. J Palliat Med. 2014 doi: 10.1089/jpm.2013.0595. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention . CDC Wonder: About underlying cause of death, 1999-2010. US Department of Health and Human Services; Atlanta, GA: 2013. [Google Scholar]
- 17.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–-22. [Google Scholar]
- 18.Thompson JW, Carlson MD, Bradley EH. US Hospice Industry Experienced Considerable Turbulence From Changes In Ownership, Growth, And Shift To For-Profit Status. Health Aff (Millwood) 2012;31:1286–93. doi: 10.1377/hlthaff.2011.1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Center to Advance Palliative Care and the National Palliative Care Research Center . AMERICA'S CARE OF SERIOUS ILLNESS:A State-by-State Report Card on Access to Palliative Care in Our Nation's Hospitals. New York: 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Center for Medicare & Medicaid Services [July 2014];42 CFR Part 418 FY 2014 Hospice Wage Index and Payment Rate. 2013 Available at www.gpo.gov/fdsys/pkg/FR-2013-08-07/pdf/2013-18838.pdf.
- 21.Centers for Medicare and Medicaid Services . Chronic Conditions among Medicare Beneficiaries, Chartbook, 2010 Edition. Baltimore, MD: 2012. [Google Scholar]
- 22.Medicare Payment Advisory Commission . Report to the Congress: Reforming the Delivery System, Chapter 8: Evaluating Medicare's Hospice Benefit. Washington, D.C.: 2008. [Google Scholar]
- 23.Medicare Payment Advisory Commission . Report to the Congress: Medicare's Payment Policy: Reforming Medicare's Hospice Benefit. Washington, D.C.: 2009. [Google Scholar]
- 24.Casarett D, Van Ness PH, O'Leary JR, Fried TR. Are patient preferences for life-sustaining treatment really a barrier to hospice enrollment for older adults with serious illness? J Am Geriatr Soc. 2006;54:472–8. doi: 10.1111/j.1532-5415.2005.00628.x. [DOI] [PubMed] [Google Scholar]
- 25.Fried TR, Bradley EH, O'Leary J. Changes in prognostic awareness among seriously ill older persons and their caregivers. J Palliat Med. 2006;9:61–9. doi: 10.1089/jpm.2006.9.61. [DOI] [PubMed] [Google Scholar]
- 26.Murtagh FE, Preston M, Higginson I. Patterns of dying: palliative care for non-malignant disease. Clinical medicine. 2004;4:39–44. doi: 10.7861/clinmedicine.4-1-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bradley EH, Fried TR, Kasl SV, Idler E. Quality-of-Life Trajectories in the End of Life. In: Lawton MP, editor. Annual Review of Gerontology and Geriatrics. Springer Publishing Company, Inc.; New York, NY: 2001. [Google Scholar]
- 28.Aldridge Carlson MD, Barry CL, Cherlin EJ, McCorkle R, Bradley EH. Hospices' enrollment policies may contribute to underuse of hospice care in the United States. Health Aff (Millwood) 2012;31:2690–8. doi: 10.1377/hlthaff.2012.0286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kelley AS, Deb P, Du Q, Aldridge Carlson MD, Morrison RS. Hospice enrollment saves money for Medicare and improves care quality across a number of different lengths-of-stay. Health Aff (Millwood) 2013;32:552–61. doi: 10.1377/hlthaff.2012.0851. [DOI] [PMC free article] [PubMed] [Google Scholar]