Abstract
The concurrent use of traditional African medicine (TAM) and allopathic medicine is not well understood for people living with HIV (PLHIV) in the era of antiretroviral therapy (ART). This cross-sectional, qualitative study examines perceptions of the concurrent use of TAM and ART among: i) patients receiving ART at the Sinikithemba HIV Clinic of McCord Hospital, in Durban, South Africa; ii) allopathic medical providers (doctors, nurses, HIV counsellors) from Sinikithemba; and iii) local traditional healers. Data were collected through in-depth interviews and focus group discussions with 26 participants between July and October, 2011. Patients in this study did not view TAM as an alternative to ART; rather, results show that patients employ TAM and ART for distinctly different needs. More research is needed to further understand the relationship between traditional and allopathic approaches to health care in South Africa, to improve cultural relevance in the provision and delivery of care for PLHIV, and to pragmatically address the concerns of healthcare providers and public health officials managing this intersection in South Africa and elsewhere.
Keywords: HIV/AIDS, traditional African medicine, antiretroviral therapy (ART), South Africa, qualitative research
Introduction
In May, 2013, the government of South Africa’s ‘Mid-Year Population Estimates’ reported an overall HIV prevalence of approximately 15.9 percent for adults aged 15–49 years (Statistics South Africa, 2013). The HIV prevalence in KwaZulu-Natal is the highest of all nine provinces, with a 37.4 percent HIV prevalence among antenatal women reported in 2011 (National Department of Health, 2012) and an overall prevalence of 25.5 percent among 15–24 year olds for the same year (UNAIDS, 2013).
In spite of notable progress in the delivery of antiretroviral therapy (ART), HIV continues to exact a toll on South Africans—socially and economically. While programmes attempt to increase ART uptake for hard-to-reach populations and more individuals are surviving because of treatment, healthcare providers remain challenged by the sheer volume of patients and caring for the underserved (Floyd et al., 2010). As poor retention in care, ART failure and drug resistance become more prevalent, the priorities for combating the epidemic are also shifting (Hosseinipour, Gupta, Van Zy, Eron, & Nachega, 2013). Public health officials, clinicians and researchers are examining contextual considerations including cultural norms and practices in the hope that they will yield insights into innovative ways to control the far-reaching effects of HIV/AIDS (Padian et al., 2011). Traditional medicine has been a particular area of focus for these investigations.
For the purposes of this report, we use the WHO definition of traditional medicine as ‘…the sum total of the knowledge, skills, and practices based on the theories, beliefs, and experiences indigenous to different cultures, whether explicable or not, used in the maintenance of health as well as in the prevention, diagnosis, improvement or treatment of physical and mental illness’ (WHO, 2013, p.15). Our definition also aligns with the WHO’s definition of ‘Complementary Medicine,’ in that the practices ‘are not fully integrated into the dominant health-care system’ of a particular country (WHO, 2013, p.15). Further, our conception of traditional African medicine (TAM) aligns with Karen Flint’s definition, as ‘…African or local medicine [that] has maintained certain core beliefs over time…’ (2008, p. 6). By using the word ‘traditional’ in the context of African medicine, we are referring to the core beliefs maintained over time that connect African medicine with indigenous people’s identity. The term ‘umuthiwesintu’ was used in data collection when discussing with patients or TAM practitioners any medical treatments prescribed by TAM practitioners, as this was the commonly used term in the community and was the term suggested as most appropriate by Zulu study team members (see below).
Much of the research concerning traditional medicine in the context of the HIV epidemic has centered in Africa, a continent arguably more affected by HIV/AIDS than anywhere else in the world and where the use of traditional medicine is common, including among PLHIV (Babb et al., 2007; Littlewood & Vanable, 2011; Peltzer, Friend-du Preez, Ramlagan, Fomumdam, & Anderson, 2010; Scorgie, 2007). A recent publication reported 72 percent usage of TAM among Black Africans, accounting for some 26.6 million people (Mander, Ntuli, Diederichs, & Mavundla, 2008). In South Africa alone, UNAIDS has estimated the prevalence of TAM use among black South Africans to be 80–85 percent (2006).
The incorporation of traditional and allopathic concepts of medicine in South Africa has long been a topic of interest and academic inquiry in the region (Hammond-Tooke, 1989, pp. 14–15). In the context of HIV care and treatment, the role of TAM has been complicated and controversial (Digby, 2006; Karim, Churchyard, Karim,& Lawn, 2009).
In action on the part of the apartheid South African government during the first decade of the HIV epidemic (1980s-early 1990s) and the inaccessibility of HIV treatment for South African PLHIV throughout the next decade (1990s-early 2000s), left a gap in health care options for South African PLHIV in the region (Karim et al., 2009; UNAIDS, 2006). The landscape for South African PLHIV seeking care was further complicated by the South African government’s pervasive denial of HIV and the outward political endorsement of Virodene (an industrial solvent) as a cure for AIDS (Karim et al., 2009; Scorgie, 2007; Simon, Altice, Moll, Shange & Friedland, 2010). Ethnographic and historical literature indicate the continuous relevance of TAM and healers in the context of health seeking behaviours among Zulu people living in KwaZulu-Natal (they often constitute the first contact patients have with healthcare) (Bryant, 1909; Carton, Laband, & Sithole, 2008; Hammond-Tooke, 1989; Jolles & Jolles, 1998;), while scholarly work from the health sciences confirms the dual use of TAM and allopathic medicine by HIV patients in South Africa (Cook, 2009; Dahab et al., 2008; Digby, 2006; Graham, Gwyther, Tiso, & Harding, 2012; Karim et al., 2009; Malangu, 2007; Peltzer et. al, 2010; Peltzer, Friend-du-Preez, Ramlagan, & Fomumdam, 2008; Peltzer & Mngqundaniso, 2008; Peltzer, Mngqundaniso, & Petros, 2006; Shuster, Sterck, Frew, & del Rio, 2009). Thomas et al. explain, ‘[m]ixing strategies while on ART is a controversial, even dangerous matter. But it is more often than not the norm […] it has its own logic’ (Thomas, Schmid, Gwele, Nub, & Cochrane, 2006, p. 6). Scorgie (2007) suggests that ‘it is common for people to ‘try out’ a variety of healing approaches in a fairly eclectic, non-committal way… it is clear that the clinic is often the last – not the first – resort for sick people and their family members’ (p. 58).
The explanatory model of ‘medical systems as cultural systems’ posited by Kleinman in 1978 and its development in medical anthropology as medical pluralism (Baer, 2002) provide the theoretical foundation for the collection and analysis of data in this study. Central to the framework are the notions that ‘health, illness and health-care related aspects of societies are articulated as cultural systems’ (p. 86) and that health, illness and health care must be researched and understood in relation to one another (Kleinman, 1978). By examining the perspectives of patients and health providers, our research explored aspects of Kleinman’s popular and professional social arenas within which sickness is experienced, and their interface (Barnes, 2007). Kleinman’s framework was particularly fitting because of its utility for investigating both individual and social dimensions of health care beliefs and actions (Kleinman, 1978, p. 89)—in this research, the seemingly paradoxical existence of TAM use among HIV patients on ART.
This cross-sectional exploratory research was conducted as part of a larger study at McCord Hospital (McCord), a semi-private, Christian hospital in Durban. That study, entitled Risk Factors for Virologic Failure (RFVF), compared patients experiencing virologic failure of their first ART regimen (viral load [VL] > 1000 copies/mL) to patients with virologic suppression on their first ART regimen (VL ≤ 1000 copies/mL) while receiving care at McCord (Marconi et al., 2013). One of the risk factors for virologic failure explored included the potential use of TAM. Using qualitative research methods, the present study explored the concurrent or consecutive use of TAM and ART from three different perspectives: 1) HIV positive patients receiving ART at an urban clinic in Durban, 2) their doctors, nurses, and HIV counsellors at the clinic, and 3) TAM practitioners in the Durban area. Understanding the perspectives of these stakeholder groups could inform subsequent ways to safely and sensitively enhance the delivery of care for HIV patients who may be attempting different approaches for their treatment and bring to light complexities of HIV treatment and care in the study population.
Methods
This study was conducted in Durban between July and October, 2011. Investigators from Emory University in the United States and from McCord Hospital and the University of KZN in Durban collaborated on the study design and data collection.
Study participants
Study participants comprised three groups which parallel the popular and professional arenas in Kleinman’s 1978 framework: 1) HIV+ patients on ART for at least five months and over 18 years of age. Twelve patients were purposively selected from among 20 recruited, screened and consented RFVF participants to provide diversity by gender and virologic status. Two selected patients did not show up at their scheduled focus group. All participating patients were of self-reported Zulu ethnicity. We use the term ‘Zulu ethnicity’ because: a) participating patients self-reported their identification as ‘Zulu’--the socio-cultural group to which they belong; b) in the context of being patients at McCord Hospital, Zulu was an ethnic category not contested, but widely agreed upon among patients themselves, and c) it is an appropriate descriptive category in the context of a multidisciplinary research study with a very specific aim: understanding the connection between ‘traditional’ African medicine and health seeking behaviours among patients on ART. 2) Allopathic medical providers who had been employed for over six months at McCord and who worked specifically in programmes for HIV+ adults. Six of 13 health providers meeting these criteria were then recruited in-person at McCord to provide variation in position (2 HIV doctors, 2 nurses, 2 counsellors), and based on their willingness and availability to participate in an in-depth interview. One selected doctor was unable to participate due to illness. 3) TAM practitioners from the Durban area. Eleven TAM practitioners from the Durban metropolitan area were recruited by a gatekeeper to the TAM practitioner community. The gatekeeper was a community member and traditional healer who knew several of the participant traditional healers personally. She was also part of the research team. The traditional healers recruited by the gatekeeper recruited other traditional healers, known and trusted as reputable by the original group. TAM practitioners were eligible to participate if they had an active TAM practice at the time of recruitment and self-identified as a practicing ‘Isangoma’ (diviner), ‘Inyanga’ (herbalist), ‘Umthandazi’ (prophet or faith healer).
TAM practitioners were recruited purposively to provide variation in gender and type of TAM practiced (i.e., Isangoma, Inyanga and Umthandazi). We employed these three descriptive categories as defined by anthropologist Hammond-Tooke in his book ‘Rituals and Medicines’ (1989). Most of the traditional healers interviewed, however, identified with more than one of these classifications. All participating TAM practitioners were of Zulu ethnicity.
We recognise that people can display different, context-dependent cultural and social identities, but feel justified in our use of ‘Zulu culture’ or ‘Zulu ethnicity’ in this paper as categories to describe study participants’ sense of identity, given the willingness of isiZulu-speaking African people in KwaZulu-Natal to ‘embrace…a sense of being Zulu, a cultural identity that apparently spoke for itself in defining legitimate African actions’ (Freund, 2008, p. 606).
Data collection
Eleven in-depth interviews and four focus group discussions were conducted between July and October 2011. Semi-structured interview and discussion guides were used, with different interview formats (individual interviews and focus groups) for each type of participant (patients, allopathic medical providers, TAM practitioners).
Interviews and focus group discussions with patients
Six interviews and one focus group discussion were conducted with patients in the isiZulu language. All data collection with patients was conducted in locations away from McCord to provide a confidential setting for patients. Patients were asked about their experience receiving ART at McCord, their views of and experiences with ‘umuthiwesintu’ (how the interviewer referred to TAM), the context in which ‘umuthiwesintu’ was used (if applicable), and if this had changed since they started receiving ART.
Interviews with allopathic medical providers
Individual interviews with allopathic medical providers allowed for a greater depth of information and experiences to be collected from each provider and to avoid potential power dynamics of conducting a group discussion with providers from different professional ranks (doctors, nurses, and counsellors). Providers were asked their views about TAM in the treatment of HIV, and their experiences with patients on ART using TAM. Interviews were conducted in English since all providers were fluent in English. Interviews were conducted at a private space at McCord, after business hours.
Focus groups with TAM practitioners
Three focus groups were held with TAM practitioners to enable interaction and discussion of issues important to them. Focus groups also provided a setting in which the TAM practitioner community would feel it had a strong, collective voice where their perspectives were valued and respected. To capture a variety of perspectives on the use of TAM, both male and female TAM practitioners and those identifying as an Isangoma, Inyanga, or Umthandazi were included in the focus groups. TAM practitioners were asked about the services they provided to PLHIV, their views on ART, and the future of TAM and allopathic medicine in HIV treatment and care.
Ethical considerations
To ensure objectivity and cultural sensitivity, the researchers who conducted interviews and focus groups with McCord patients and TAM practitioners were of Zulu background and not affiliated with McCord. To ensure that participating patients did not conflate this study with endorsement of concurrent TAM/ART use, following each interview and focus group, patients were given an informational sheet (in isiZulu and English) provided by McCord explaining the potential risks associated with concurrent TAM/ART use, and were encouraged to speak to their medical provider(s) if they were using TAM while on ART or considering it. All research instruments were translated into isiZulu by a local translator and back-translated into English by local research assistants to check the accuracy in the meaning of the translations. All interview and focus group research instruments were approved by the McCord Research Ethics Committee (MREC) and the Emory University IRB prior to data collection.
Data analysis
All interviews and group discussions were digitally recorded with participants’ consent. Interviews conducted in English were transcribed verbatim by a research assistant; interviews conducted in isiZulu were simultaneously translated and transcribed verbatim into English by professional interpreters/transcribers who were native isiZulu speakers. All transcripts were checked for accuracy and completeness by a different native isiZulu speaker. Textual data were de-identified and entered into MAXQDA software for analysis.
Thematic analysis integrated a data-driven, inductive code development with deductive, predetermined codes to allow for codes based on a conceptual (i.e. literature-based) understanding of TAM use in this context. Reading, re-reading and summarising data were used to identify initial themes. Initial themes were validated by having an external researcher read transcripts, note themes raised, and compare these to those of the study team. Refined inductive codes were then consolidated with pre-determined deductive codes in a codebook. Transcripts from different stakeholder groups (allopathic medical providers, TAM practitioners) were first reviewed separately to identify issues unique to each group, and then compared to identify similarities and differences across groups. Comparing and then sketching a visual representation of individually reported TAM use among patients led to the matrix for TAM use presented in the Results.
Results
The perspectives of the three stakeholder groups frame a narrative regarding the use of TAM in the context of HIV care and treatment. Table 1 presents characteristics of the study participants.
Table 1.
Characteristics of study participants
| Patients (n=10) | Traditional Healers (n=11) | Allopathic Medical Providers (n=5) | ||||
|---|---|---|---|---|---|---|
|
Female Male |
7 3 |
6 5 |
4 1 |
|||
| Other Characteristics | Patients with Virological failure† | 5 | Type of Traditional healing practiced* | Profession | ||
| Isangoma | 4 | HIV Counselor | 2 | |||
| Patients without virological failure† | 5 | Inyanga | 4 | Nurse | 2 | |
| Umthandazi | 8 | Doctor | 1 | |||
Virological failure = viral load>1000 copies/mL after 5+ months treatment
Most healers identified with more than one healing practice. These categorizations were not mutually exclusive, thus total n>11
Knowledge of TAM
Participant groups (patients, allopathic medical providers, TAM practitioners) had similar knowledge of traditional medicines and the various contexts in which they are used. When patients referred to traditional medicines, they typically cited ‘traditional herbs, “herbs,’ and ‘the roots of plants,’ which were commonly boiled and ingested or steamed and inhaled. Few patients mentioned non-herbal healing, such as pricking the skin, communicating with ancestors to determine the cause of illness, or, similarly, providing a ‘spiritual examination.’ Though many patients in this study believed that allopathic medical providers dismiss TAM without understanding how it is used, when asked to describe TAM, allopathic medical providers stated specific medicines their patients had discussed including, simply, ‘traditional herbs’ and varied plants or roots that come in ‘those bottles.’ They described that they are typically boiled, ingested, or applied topically to alleviate illness or ailments. They also described CD4 boosters and ‘uBhejane’ (a well-known mixture of herbs in South Africa said to cure HIV).
Attitudes towards TAM for treating HIV
All allopathic medical providers and some patients expressed negative attitudes about using TAM for treating HIV. Allopathic medical providers discussed negative clinical consequences (e.g. organ damage) associated with TAM use among patients they consult at the clinic. Others implicated TAM as a barrier to open and honest discussion about HIV treatment and care between patients and providers, reporting that ‘we only find out clients are using TAM when there is a problem.’ One allopathic medical practitioner faulted TAM for giving the ‘illusion’ of improved immune function (high CD4 counts), barring patients from ART treatment because their CD4 counts were too high to qualify.
Motivations for TAM use
All participant groups expressed different motivations for TAM use among patients receiving ART, many unrelated to treating HIV. For example, TAM was reportedly used for success in business, sexual virility, ridding oneself of poverty or food insecurity, or as an appetite stimulant. Allopathic medical providers felt that patients who used TAM to treat or ‘cure’ HIV did so out of ‘desperation,’ or due to lack of knowledge about the efficacy of ART. Many allopathic medical providers felt that patients would not consult TAM to treat HIV if they understood the disease and how ART works. This view was not supported by patients. No patients reported using TAM out of ‘desperation,’ and some remarked that continuing to use TAM after beginning treatment is irresponsible, indicating knowledge among the patients in this study of the efficacy of ART for treating HIV. The following passages illustrate some patients’ negative feelings about using TAM concurrently with ART:
If you mix the two, you have jeopardised the [ART] the doctor has given you. It will reverse the positive effects of that treatment. – Female patient
I think the negative effect of mixing traditional herbs with [ART] is that traditional herbs are strong and that [ART is] strong, and they clash. That clash has a negative effect on the kidneys. That is why you find cases where patients taking [ART] end up dying of kidney failure all of a sudden. – Female patient
Mixing the two means you are not taking responsibility for your own life. – Male patient
TAM as part of Zulu and African culture
All participant groups described TAM as a vital part of Zulu and African identity. Many patients had used TAM during their lifetime and connected this use with manifestations of their ‘Zulu’ or ‘African’ identity. Similarly, traditional healers posited TAM as a central part of life as a Zulu person--one that does not recede simply because a person becomes HIV positive. Patients who did not use TAM themselves acknowledged that its use was integral to one’s identity as an African, as did allopathic medical providers who opposed the use of TAM for managing HIV. Importantly, among patients and allopathic medical providers who believed ART should be used to treat HIV, TAM was perceived as appropriate for some reasons, as shown in the following statements:
If the person is being [bewitched] by the other person, the herbal medication it does help…. Really, there are things that need to be treated by [traditional healers]. –Allopathic medical provider
It is through our belief as Africans that we believe in the spiritual realm. So the traditional healers act as mediators between us and the ancestors. Most people visit traditional healers seeking a spiritual examination, and some believe that their problems can only be solved by traditional healers. Faith in the healers plays a vital role in the African community. – Male patient
As Zulu people we use [traditional medicine] in the home….Sometimes it does help. Yes, that’s how I would define it, that back in our religion and in rural areas people are still using it for particular things. These are old beliefs, but they do work. – Female patient
Intersection of TAM and ART among members of the study population
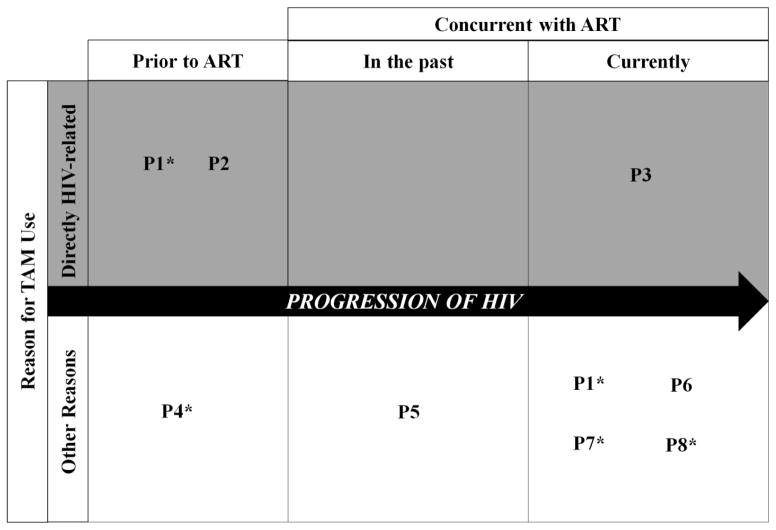
Figure 1 shows the context of TAM use and its intersection with ART among patients in this study. Only three patients reported using TAM for reasons directly related to HIV. Two patients used TAM prior to ART. One patient (P1) used TAM at the early stages of the disease, as she believed it would boost her CD4 count. Another patient (P2) used ‘uBhejane’ at the beginning stages of his illness, as he believed it would ‘heal’ HIV. Although both patients reported that they stopped TAM upon initiating ART, P1 reported using TAM while on ART at a later stage, but not to treat HIV. The same participant said she uses TAM despite being on ART for reasons unrelated to HIV, because ‘as a Zulu person [my] home needs to be protected.’ This participant gave no further description of the TAM used for such protection. A different participant (P7) also described using TAM while on ART because ‘besides HIV/AIDS there are still other diseases which affect us.’ The remaining patient who used TAM while receiving ART (P8 in Figure1) stated that it was never used to treat HIV.
Figure 1.
Patients’ reasons for TAM use at different stages of ART
Note: *indicates patient failing ART regimen (vL>1000 copies/mL) after 5+ months of treatment. P1, P2, etc. each represent a distinct patient who reported ever using TAM in his or her lifetime. P1 indicates that she used TAM for HIV and non-HIV related reasons at different stages.
One patient believed it was acceptable to use TAM concurrently with ART and others expressed the desire to use both TAM and ART, but only one patient (P3) reported actually using TAM concurrently with ART specifically to treat HIV. This patient was using TAM long before she was diagnosed with HIV and continued to drink and steam the roots of plants after she began ART. She described that using TAM was part of her Zulu heritage that she is proud of and she believed that it ‘brings [her] health’ to use both TAM and ART concurrently.
Other patients reported using TAM while on ART for reasons they perceived to be unrelated to treating HIV. P4 said he used TAM before learning he was HIV positive because he felt his health ‘was not in good shape.’ P5 described using TAM briefly and in secret when she first initiated ART to treat high blood pressure, but not to treat HIV specifically. Other patients (P1, P6, P7, and P8) also described using TAM for varied reasons they did not associate with HIV, like treating headaches or swollen feet. While the symptoms might in fact be related to HIV infection or side effects of ART use, the patients did not explicitly discuss these symptoms or subsequent TAM use in the context of HIV (or ART).
Perceptions of traditional healers’ role in HIV care
Traditional healers expressed a central role for themselves in the provision of care for PLHIV--to give and restore patients’ hope for life. No traditional healers believed they could ‘cure’ HIV; rather, the predominant feeling among traditional healers was that ‘you will help [a patient with symptoms of HIV], but you are not going to cure him completely.’ Many traditional healers described the efficacy of ‘traditional liquid medicine[s] that we will concoct with some ingredients’ in treating what they defined as symptoms of opportunistic infections that are characteristic of HIV infection, including sores, swollen lymph nodes, or loss of appetite. In this role, traditional healers supported concurrent use of TAM and ART. ‘…By and large,’ said a male traditional healer, ‘we feel that [ART is] complementary to traditional medicine.’ The notion that TAM and ART are complementary is supported by the ways in which TAM use was reported among patients illustrated in Figure 1.
Allopathic medical providers did not generally support the notion of engaging traditional healers in HIV care, but many believed it would be beneficial to have a dialogue between the two traditions to foster understanding and mutual respect. Several TAM practitioners remarked that they could teach each other ‘a few tricks,’ acknowledging that ‘as traditional healers we don’t have the means or expertise to detect [HIV].’ Nurses and counsellors felt that many TAM practitioners are ‘illiterate’ and so lack medical knowledge and ‘don’t understand what’s going on in the body.’ This fueled strong feelings of mistrust for TAM practitioners among many allopathic medical providers. One nurse felt that traditional healers ‘rob’ patients by making them pay exorbitant prices for traditional treatments. Traditional Healers, on the other hand, described trust as a reason why so many patients seek out traditional treatment. A common sentiment among traditional healers was that ‘patients want us to solve their problems because they trust us.’ Many traditional healers described their allopathic medical counterparts, on the other hand, as lacking confidentiality and outwardly critical of patients who are HIV positive. Nevertheless, there was an overarching sentiment among all traditional healers that allopathic medical providers and traditional healers are working toward a common end—the welfare of patients, many of whom are living with HIV. As a male traditional healer stated, ‘…the only thing is the culture that separates us; otherwise we are the same.’ Support for collaboration between different approaches to HIV care is further evidenced in the following statement:
Ah, according to my opinion, that would be a very good thing if traditional healers and Western doctors could work together, because they both share the desire to heal people. The problem is that we were divided from the start… We have to unite because Western doctors are healers just as I am a healer. We both direct our prayers to God in order to help our patients; we both ask for divine powers from the same God. –Female traditional healer
Discussion
Previous studies that have explored the intersection of TAM and allopathic medicine in the context of HIV have often viewed TAM either as a barrier to or a mediator of safe and effective HIV treatment and adherence to ART, without taking into consideration the overall context and motivators of TAM and its relation to HIV treatment and care (Peltzer et al., 2010; Dahab et al., 2008; Dahab et al., 2010; Dahab, et al., 2011). Findings here could provide important insights for addressing the concerns of healthcare providers and public health officials managing this intersection in South Africa and elsewhere, who remain at odds and in need of clarity around the feasibility of a plural health system (Cook, 2009).
We see this study as one ‘voice’ amidst many, aiming to understand the connection between ‘traditional’ African medicine and health seeking behaviours among South Africans dealing with ART (particularly, black South Africans who self-identify as Zulu). In order to advance a much needed interdisciplinary dialogue in the field of HIV healthcare, we believe in the importance of recognising the polyphonic character of interpretations about the subject and the different and valid contributions of these interpretations.
Study findings here show that all participant groups have a general knowledge of ‘traditional herbs,” the roots of plants,” holy water,’ nondescript ‘CD4 boosters,’ and ‘uBhejane’ (advertised in the Durban area as a ‘cure’ for HIV). This contrasts with another study in Durban which found that participating healthcare workers did not possess a basic knowledge of TAM, based on self-reported answers to a voluntary survey (Mbutho, Gqaleni & Korporaal, 2012). Patients and traditional healers also note the role of TAM and traditional healers in consulting with ancestors to predict or understand the cause of illness, ‘protecting the house,’ performing a ‘spiritual assessment,’ and counseling patients. Although findings from this study show general knowledge of TAM, feelings about the utility and efficacy of TAM appear to be context-driven and dependent on the reasons for TAM use.
Consistent with studies that have noted an ideological acceptance of ART among traditional healers (Shuster et al., 2009), traditional healers in this study were accepting of ART as an effective treatment for HIV, but more readily than any other stakeholder group they support a complementary role for TAM in HIV care. This finding reinforces literature that encourages the integration of traditional healers into HIV care, identifying them as talented and culturally relevant HIV-support or ART-adherence counsellors (UNAIDS, 2006; Cook, 2009; Homsy, King, Balaba, & Kabatesi, 2004; Giarelli, & Jacobs, 2003; Peltzer, 2009).
Patients in this study underscored the important finding that individuals on ART who receive TAM for cultural uses like protecting their home do not embrace TAM as an HIV-related health-seeking behaviour. This suggests that there was no ‘clash’ in popular or professional understandings of illness or disease in this context; rather, that the use of TAM as a cultural phenomenon was perceived as entirely independent of behaviours related to treating HIV among patients. Even patients who described TAM use for symptoms that are consistent with known side effects of ART (e.g., headaches, swollen feet) did not perceive their use of TAM to treat these symptoms as directly related to HIV.
Previous studies have linked cultural beliefs directly to health seeking behaviours (including TAM use) in the context of HIV (Golooba-Mutebi &Tollman, 2007; Dahab et al., 2011), but for the patients receiving ART in this study (many of whom noted the importance of Zulu culture in their lives), a strong connection to Zulu culture and use of TAM in daily life did not necessarily undermine their exclusive use of ART for treating HIV. Across the study population, results indicated widespread support for directly managing HIV with ART, even among patients who believed in the need for TAM for other reasons. This finding differs from studies that have examined TAM as a culturally mediated behaviour that negatively impacts adherence to ART (Peltzer et al., 2010; Simon et al., 2010; Dahab et al., 2010), and recent studies about the prevalence of false beliefs about the effectiveness of ART (Nozaki, Kuriyama, Manyepa, Zyambo, Kakimoto, & Bärnighausen, 2013).
Allopathic medical providers, by far the strongest proponents of ART in this study population, implicitly understood the notion of TAM and ART as distinct but parallel phenomena. They strongly encouraged exclusive use of ART for treating HIV, yet understood the cultural reasons that would necessitate TAM use, specifically, someone wishing you ill will, or ‘bewitching’ you. The findings here underscore the important distinction between ascribing to TAM treatments for HIV that could potentially undermine adherence to ART (not found in this study) and ascribing to TAM for reasons perceived by patients as unrelated to HIV (which was found in this study.) This second type of TAM use did not affect patients’ positive feelings or commitment to ART.
The duality of TAM and ART use in this context was further suggested by patients who used TAM and ART concurrently, but felt strongly that they should not be ‘mixed.’ These patients expressed a clear understanding of potentially harmful interactions between the TAM and ART and did not believe that they were mixing the two by using ART to manage HIV and TAM for other reasons apart from HIV. This discontinuity—that ART should be used independent of TAM, and the simultaneous understanding that TAM is necessary in certain situations—raises an important practical question for patients who both believe TAM is necessary (culturally) and use ART. Presumably, a person living with HIV should use only ART for treatment. However, if the same individual seeks protection from spirits or wishes to observe a cultural practice that necessitates TAM use, he or she must use TAM. In this way, TAM and ART lead a parallel, often paradoxical existence. Patients themselves do not perceive this duality as ‘mixing’ treatments for HIV.
It is important to note that although TAM and allopathic medicine are fluid, constantly changing concepts and practices that have mutual influence, we consider it appropriate to use them here as separate, comparable and differentiable systems to reflect the source of treatment obtained by patients. Treatments prescribed by traditional healers are derived and developed through the lens of a cosmology that is clearly distinct from the one in which the biomedical approach (used to develop medications prescribed by allopathic practitioners) originates (e.g., ancestral divination vs. scientific method). In the context of our research, all participants demonstrated a clear, a priori understanding of the concepts of traditional African medicine, ‘umuthiwesintu’ and traditional healers. Patients also clearly expressed that they perceived distinct differences between traditional African healthcare and healthcare received from ‘western’ allopathic providers. Further, while these distinctions and the very notion of a defined duality between TAM and allopathic medicine are perhaps not a philosophical consideration for ART patients in their daily lives, they clearly correspond to the conceptualisation by allopathic medicine providers in our study of how TAM and allopathic medicine exist in this context.
The reality of TAM use among patients with HIV as opposed to TAM use for treating HIV is an important finding with implications for treatment. It hints that TAM use can be a conscious and informed choice made for different purposes than HIV treatment—one that does not necessarily compromise a patient’s adherence to ART. This finding is consistent with the shift in academic literature that recognises TAM and ART (or allopathic medicine in general) not as competing paradigms that must be balanced, but as parallel traditions that are not by definition at odds with one another (Shuster et al., 2009; Liddell, Barrett, & Bydawell, 2006). In considering the clinical possibility of a dual approach to HIV treatment and care, safety during concurrent ART and TAM practices, rather than changes in ART adherence patterns, becomes the primary issue to address. There is already a growing body of pharmacological research concerning herb-drug interactions as well as the use of plants like Hypoxishemerocallidea and Sutherlandiafrutescens to treat HIV primarily by enhancing the immune system or some with actual antiviral properties (Awortwe, Bouic, Masimirembwa, & Rosenkranz, B., 2014; Chinsembu & Hedimbi, 2009; Mills, Cooper, Seely, & Kanfer, 2005; Rosenberg et al., 2013); findings here affirm the importance of continuing to advance this important area of study.
Discussions among traditional healers and allopathic medical providers supported coming together—physically and intellectually—to learn about each other’s healing practices for different afflictions. However, traditional healers were skeptical of allopathic medical providers’ ability to accept their healing practices without judging healers’ training or education. This reticence is consistent with the few findings in the literature that have addressed tension between traditional and allopathic medicine practitioners and have found, for example, that traditional healers felt ‘nurses undermined their work, did not accept TAM’s efficacy in treatment and consequently did not refer patients’ (Mngqundaniso & Peltzer, 2008, p. 380).
Previous studies on the use of TAM in the context of HIV treatment have posited TAM and allopathic medicine as parallel, sometimes polarised approaches whose use depends on multiple factors like availability and access to treatment (Littlewood & Vanable, 2011), and have called for further examination into the motivations for TAM use (Puoane, Hughes, Uwimana, Johnson, & Folk, 2012). The findings here suggested implicit cultural motivators for TAM use that were independent of a patient’s HIV-related health-seeking behaviour(s). TAM for patients on ART was not ‘either-or’, as was evident from the concurrent but complementary role of TAM for patients using both. For these patients, TAM was not a mediator of or a barrier to safe and effective HIV related health-seeking behaviours; it worked in tandem and for a different purpose. To conflate the independent identities of TAM use for cultural reasons with TAM use for HIV management is to lose the nuanced distinctions that characterised TAM use for patients like those in this study population.
This study was an exploratory study that employed qualitative methods to allow for rich data that captured perspectives of diverse stakeholder groups regarding the use of TAM for and in the context of HIV. The study design addressed a noted gap in literature by directly involving traditional healers. Other studies (Graham et al., 2012; Mngqundaniso & Peltzer, 2008) have engaged traditional healers and allopathic medical practitioners, but to date and to the best of our knowledge, few in South Africa have engaged doctors, allopathic medical health care providers, and traditional healers in the same study (Puoane et al., 2012). The perspectives of traditional healers contributed immensely to the findings and themes revealed here.
This study worked to address the sensitive nature of the discourse around TAM in clinical settings and by clinical practitioners, many of whom oppose TAM use (Peltzer et al., 2010; Peltzer et al., 2008) by engaging local, isiZulu-speaking researchers with no affiliation to McCord to conduct interviews and group discussions in locations outside of McCord. Investigators believe this strategy added credibility to the interviews, put patients at ease, and allowed them to speak openly and candidly about a topic that often goes undisclosed among patients in clinical settings (Puoane, et al., 2012; Thomas, Aggleton, & Anderson, 2010).
It is important to note that the opinions expressed here represent only those of the members of this study population. TAM use (frequency, amount, duration) at McCord likely differs from TAM use elsewhere due to the education and discouragement given during ART training and follow-up. Patients by definition were engaged and retained in allopathic HIV care which does not necessarily represent the voice of those who have been lost to follow-up. Out of necessity, traditional healers were recruited through a single gatekeeper, which may have limited the range of experiences or opinions among traditional healers selected for participation. Allopathic medical practitioners were interviewed at McCord to accommodate their schedules, which may have affected their willingness to disclose sensitive opinions regarding TAM use. Lastly, the translation of interview transcripts from isiZulu into English opened the possibility of inconsistencies in translation. Two Zulu translators/transcribers were hired to translate recordings of patient interviews and traditional healer focus groups from isiZulu into English. Each recording was only translated and transcribed by one of the translator/transcribers. Transcripts were spot-checked for accuracy by a native isiZulu-speaking study team member, however, inner and inter-translator reliability were not assessed.
Conclusion
Findings revealed tacit and learned knowledge of TAM and ART, respectively, among all study participants. Among patients, there was a nuanced understanding of TAM’s utility in the context of their management of HIV. Specifically, patients and providers in this study illustrated that TAM does not necessarily undermine adherence to ART and further, that TAM is not limited to herbal treatments that are ingested. The latter is important in recognising the role of TAM moving forward, despite not yet having ample evidence that TAM does or does not result in adverse effects and drug interactions that could cause harm or limit the effectiveness of ART.
We feel it is important to note that these findings are of great clinical and public health interest. This investigation was born out of a widespread concern about medical pluralism in HIV care and treatment voiced by policy leaders, traditional healers and allopathic clinicians, social scientists, patients and community members. This concern often involved accusations and conflict stemming from groups seeing themselves on opposing sides of a debate over the appropriate model of care for individuals living with HIV. Likewise, there have been calls to action, conferences and policies proposed to specifically mediate this process. Members of this study team have been involved with clinical care, research and policy decisions affecting individuals living with HIV in this region for decades, thereby observing over time the unfavorable effects of this debate.
That traditional healers and patients noted the critical role of TAM and traditional healers for psychosocial and spiritual counseling or communicating with ancestors (practices that do not have the potential for drug interactions or adverse physiological effects in the body) gives hope to the possibility that distinct modalities of healing could each have a place in the delivery of care for PLHIV in South Africa someday. This study provides a methodological approach for future research and for the design of a larger, longitudinal qualitative and quantitative project to further understand the diversity of health seeking behaviours among HIV patients in the KwaZulu-Natal province. This broader framework could also provide a substantial benefit and augment the standard of care in the setting of critical allopathic medical personnel shortages, with traditional healers serving as integrated providers of HIV testing in the field, linkage to treatment (i.e. ART), patient navigation and adherence counseling.
Acknowledgments
We gratefully thank the Sinikithemba Clinic at McCord Hospital in Durban, South Africa and traditional healers in Durban and the surrounding communities for their commitment to improve patient care and support research. We thank all the patients of this clinic for their participation and the staff (counsellors, medical records staff, nurses, and medical officers) for providing vital assistance in the data collection. We also thank Krista Dong, MD and Deli Mthimkhulu of the iTEACH programme at Edendale Hospital, and Carlos del Rio, MD of Emory University Rollins School of Public Health for their generous support of our work.
Funding
Grant support came from Emory University Center for AIDS Research (CFAR) [P30 AI050409] and the Emory School of Medicine Division of Infectious Diseases, NIH [R01 – AI098558], CDC Cooperative Agreement [U62/CCU123541-01], and the Elizabeth Glaser Pediatric AIDS Foundation as part of Project HEART.
References
- Awortwe C, Bouic PJ, Masimirembwa CM, Rosenkranz B. Inhibition of major drug metabolizing CYPs by common herbal medicines used by HIV/AIDS patients in Africa: Implications for herb-drug Interactions. Drug Metabolism Letters. 2014;7(2):83–95. doi: 10.2174/1872312808666140129123210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babb DA, Pemba L, Seatlanyane P, Charalambous S, Churchyard GJ, Grant AD. Use of traditional medicine by HIV-infected individuals in South Africa in the era of antiretroviral therapy. Psychology, Health & Medicine. 2007;12:314–320. doi: 10.1080/13548500600621511. [DOI] [PubMed] [Google Scholar]
- Baer HA. Contributions to a critical analysis of medical pluralism: An examination of the work of Libbet Crandon-Malamud. In: Koss-Chioino JD, Leatherman T, Greenway C, editors. Medical pluralism in the Andes. Abingdon: Routledge; 2002. pp. 42–60. [Google Scholar]
- Barnes L. Plural health systems: Meanings and analytical issues. Paper presented at ARHAP International Colloquium 2007, Collection of Concept Papers; March 13–16, 2007.Cape Town, South Africa: Monkey Valley Resort; 2007. [Google Scholar]
- Bryant AT. Zulu medicine and medicine men. In: Chidester D, Kwenda C, Petty R, editors. African traditional religion in South Africa: An annotated bibliography. Westport: Greenwood Publishing Group; 1909. [Google Scholar]
- Carton B, Laband J, Sithole J, editors. Zulu identities, being Zulu past and present. New York: Columbia University Press; 2008. [Google Scholar]
- Cook C. Sangomas: Problem or solution for South Africa’s health care system. Journal of the National Medical Association. 2009;101:261–265. doi: 10.1016/s0027-9684(15)30855-5. [DOI] [PubMed] [Google Scholar]
- Chinsembu KC, Hedimbi M. A survey of plants with anti-HIV active compounds and their modes of action. Medical Journal of Zambia. 2009;36:178–186. [Google Scholar]
- Dahab M, Charalambous S, Hamilton R, Fielding K, Kielmann K, Churchyard G, Grant A. ‘That is why I stopped ART’: Patients’ & providers’ perspectives on barriers to an enabler of HIV treatment adherence in a South African workplace programme. BMC Public Health. 2008;8:63. doi: 10.1186/1471-2458-8-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahab M, Charalambous S, Karstaedt A, Fielding K, Hamilton R, La Grange L, Grant A. Contrasting predictors of poor antiretroviral therapy outcomes in two South African HIV programmes: Acohort study. BMC Public Health. 2010;10:430. doi: 10.1186/1471-2458-10-430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahab M, Kielmann K, Charalambous S, Karstaedt A, Hamilton R, La Grange L, Grant AD. Contrasting reasons for discontinuation of antiretroviral therapy in workplace and public-sector HIV programs in South Africa. AIDS Patient Care and STDs. 2011;25:53–59. doi: 10.1089/apc.2010.0140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health, South Africa. The National Antenatal Sentinel HIV and Syphilis Prevalence Survey in South Africa, 2011. 2012 Retrieved from http://www.avert.org/south-africa-hiv-aids-statistics.htm.
- Digby A. Studies in the History of Medicine. Vol. 5. Oxford: Peter Lang; 2006. Diversity and division in medicine: Health care in South Africa from the 1800s. [Google Scholar]
- Floyd S, Molesworth A, Dube A, Banda E, Jahn A, Mwafulirwa C, French N. Population-level reduction in adult mortality after extension of free anti-retroviral therapy provision into rural areas in northern Malawi. PLoS One. 2010;5:e13499. doi: 10.1371/journal.pone.0013499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flint K. Healing Traditions: African Medicine, Cultural Exchange, and Competition in South Africa, 1820–1948. Athens: Ohio University Press; 2008. [Google Scholar]
- Freund B. Zulu identity in the international context. In: Carton B, Laband J, Sithole J, editors. Zulu identities, being Zulu past and present. New York: Columbia University Press; 2008. pp. xii–xx. [Google Scholar]
- Giarelli E, Jacobs L. Traditional Healing and HIV–AIDS in KwaZulu-Natal, South Africa: To curb the epidemic, South African nurses, physicians, and traditional healers are learning to collaborate. American Journal of Nursing. 2003;103:36–46. doi: 10.1097/00000446-200310000-00018. [DOI] [PubMed] [Google Scholar]
- Golooba-Mutebi F, Tollman S. Confronting HIV/AIDS in a South African village: The impact of health-seeking behaviour. Scandinavian Journal of Public Health Supplement. 2007;69:175–180. doi: 10.1080/14034950701355437. doi:10.1080%2F14034950701355437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham N, Gwyther L, Tiso T, Harding R. Traditional healer’s views of the required processes for a ‘good death’among Xhosa patients pre- and post-death. Journal of Pain and Symptom Management. 2012;46(3):386–94. doi: 10.1016/j.jpainsymman.2012.08.005. [DOI] [PubMed] [Google Scholar]
- Hammond-Tooke WD. Rituals and medicines: Indigenous healing in South Africa. Africa: Ad. Donker Publisher; 1989. [Google Scholar]
- Homsy J, King R, Balaba D, Kabatesi D. Traditional health practitioners are key to scaling up comprehensive care for HIV/AIDS in sub-Saharan Africa. AIDS. 2004;18:1723–1725. doi: 10.1097/01.aids.0000131380.30479.16. [DOI] [PubMed] [Google Scholar]
- Hosseinipour MC, Gupta RK, Van Zy G, Eron JJ, Nachega JB. Emergence of HIV drug resistance during first- and second-line antiretroviral therapy in resource-limited settings. Journal of Infectious Disease. 2013;207(suppl 2):S49–S56. doi: 10.1093/infdis/jit107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jolles S, Jolles F. African traditional medicine—potential route for viral transmission? The Lancet. 1998;352:71. doi: 10.1016/S0140-6736(05)79558-1. [DOI] [PubMed] [Google Scholar]
- Karim S, Churchyard G, Karim Q, Lawn S. HIV Infection and tuberculosis in South Africa: an urgent need to escalate the public health response. The Lancet. 2009;374:921–933. doi: 10.1016/S0140-6736(09)60916-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinman A. Concepts and a model for the comparison of medical systems as cultural systems. Social Science and Medicine. 1978;12:85–93. doi: 10.1016/0160-7987(78)90014-5. [DOI] [PubMed] [Google Scholar]
- Liddell C, Barrett L, Bydawell M. Indigenous beliefs and attitudes to AIDS precautions in a rural South African community: An empirical study. Annals of Behavioral Medicine. 2006;32:218–225. doi: 10.1207/s15324796abm3203_7. [DOI] [PubMed] [Google Scholar]
- Littlewood R, Vanable P. A global perspective on complementary and alternative medicine use among people living with HIV/AIDS in the era of antiretroviral treatment. Current HIV/AIDS Report. 2011;8:257–268. doi: 10.1007/s11904-011-0090-8. [DOI] [PubMed] [Google Scholar]
- Malangu N. Self-reported use of traditional, complementary and over-the-counter medicines by HIV-infected patients on antiretroviral therapy in Pretoria, South Africa. African Journal of Traditional Complementary and Alternative Medicine. 2007;4:273–278. doi: 10.4314/ajtcam.v4i3.31219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mander M, Ntuli L, Diederichs N, Mavundla K. Economics of the traditional medicine trade in South Africa: health care delivery. South African Health Review. 2007:189–196. [Google Scholar]
- Marconi V, Wu B, Hampton J, Ordonez C, Johnson B, Singh D, Sunpath H. Early warning indicators for first-line virologic failure independent of adherence measures in a South African urban clinic. AIDS Patient Care and STDs. 2013;27:657–668. doi: 10.1089/apc.2013.0263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mbutho N, Gqaleni N, Korporaal C. Traditional complementary and alternative medicine: Knowledge, attitudes and practices of health care workers in HIV and AIDS clinics in Durban hospitals. African Journal of Traditional Complementary and Alternative Medicine. 2012;9:370–379. doi: 10.4314/ajtcam.v9i3s.8. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3746618/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills E, Cooper C, Seely D, Kanfer I. African herbal medicines in the treatment of HIV: Hypoxis and Sutherlandia. An overview of evidence and pharmacology. Nutrition Journal. 2005;4:19. doi: 10.1186/1475-2891-4-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mngqundaniso N, Peltzer K. Traditional healers and nurses: Aqualitative study on their role on sexually transmitted infections including HIV and AIDS in KwaZulu-Natal, South Africa. African Journal of Traditional Complementary and Alternative Medicine. 2008;5:380–386. doi: 10.4314/ajtcam.v5i4.31293. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2816575/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nozaki I, Kuriyama M, Manyepa P, Zyambo MK, Kakimoto K, Bärnighausen T. False beliefs about ART effectiveness, side effects and the consequences of non-retention and non-adherence among ART patients in Livingstone, Zambia. AIDS and Behavior. 2013;17:122–126. doi: 10.1007/s10461-012-0221-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padian NS, McCoy SI, Abdool Karim SS, Hasen N, Kim J, Bartos M, Cohen MS. HIV prevention transformed: The new prevention research agenda. The Lancet. 2011;378:269–278. doi: 10.1016/S0140-6736(11)60877-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peltzer K. Utilization and practice of traditional complementary/alternative medicine (TM/CAM) in South Africa. African Journal of Traditional Complementary and Alternative Medicine. 2009;6:175–185. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2816568/ [PMC free article] [PubMed] [Google Scholar]
- Peltzer K, Friend-du-Preez N, Ramlagan S, Fomumdam H. Use of traditional complementary and alternative medicine for HIV patients in KwaZulu Natal South Africa. BMC Public Health. 2008;8:255. doi: 10.1186/1471-2458-8-255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peltzer K, Friend-du Preez N, Ramlagan S, Fomumdam H, Anderson J. Traditional, complementary and alternative medicine and antiretroviral treatment use among HIV patients in KwaZulu-Natal, South Africa. African Jounal of Traditional Complementary and Alternative Medicine. 2010;7:125–137. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2503977/ [PMC free article] [PubMed] [Google Scholar]
- Peltzer K, Mngqundaniso N. Patients consulting traditional health practitioners in the context of HIV/AIDS in urban areas in KwaZulu-Natal South Africa. African Journal of Traditional Complementary and Alternative Medicine. 2008;5:370–379. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2816585/ [PMC free article] [PubMed] [Google Scholar]
- Peltzer K, Mngqundaniso N, Petros G. HIV/AIDS/STI/TB knowledge, beliefs and practices of traditional healers in KwaZulu-Natal, South Africa. AIDS Care. 2006;18:608–613. doi: 10.1080/09540120500294206. [DOI] [PubMed] [Google Scholar]
- Puoane T, Hughes G, Uwimana J, Johnson Q, Folk W. Why HIV positive patients on antiretroviral treatment and/or cotrimoxazole prophylaxis use traditional medicine: Perceptions of health workers, traditional healers and patients: A study in two provinces of South Africa. African Journal of Traditional Complementary and Alternative Medicine. 2012;9:495–502. doi: 10.4314/ajtcam.v9i4.6. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3746650/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg Y, Sack M, Montefiori D, Forthal D, Mao L, Hernandez-Abanto S, Jiang X. Rapid high-level production of functional HIV broadly neutralizing monoclonal antibodies in transient plant expression systems. PLoS ONE. 2013;8(3):e58724. doi: 10.1371/journal.pone.0058724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scorgie F. Plural health systems. Paper presented at ARHAP International Colloquium, Collection of Concept Papers.2007. [Google Scholar]
- Simon M, Altice F, Moll A, Shange M, Friedland G. Preparing for a highly active antiretroviral therapy rollout in rural South Africa: An assessment using the information, motivation and behavioral skills model. AIDS Care. 2010;22:462–474. doi: 10.1080/09540120903220253. [DOI] [PubMed] [Google Scholar]
- Sithole J. Zuluness in South Africa: From ‘struggle’ debate to democratic transformation. In: Carton B, Laband J, Sithole J, editors. Zulu identities, being Zulu past and present. New York: Columbia University Press; 2008. pp. 606–612. [Google Scholar]
- Shuster J, Sterck C, Frew P, del Rio C. The cultural and community-level acceptance of antiretroviral therapy (ART) among traditional healers in Eastern Cape, South Africa. Journal of Community Health. 2009;34:16–22. doi: 10.1007/s10900-008-9121-9. [DOI] [PubMed] [Google Scholar]
- Statistics South Africa. Mid-year Population Estimates, 2013. 2013 Retrieved from http://www.statssa.gov.za/publications/P0302/P03022013.pdf.
- Thomas F, Aggleton P, Anderson J. ‘Experts’, ‘partners’ and ‘fools’: Exploring agency in HIV treatment seeking among African migrants in London. Social Science and Medicine. 2010;770:736–743. doi: 10.1016/j.socscimed.2009.10.063. [DOI] [PubMed] [Google Scholar]
- Thomas E, Schmid B, Gwele M, Nub R, Cochrane J. Let us embrace: The role and significance of an integrated faith-based initiative for HIV and AIDS. 2006 Retrieved from http://www.arhap.uct.ac.za/downloads/masang_full.pdf.
- UNAIDS. Collaborating with traditional healers for HIV prevention and care in sub-Saharan Africa: Suggestions for programme managers and field workers. 2006 Retrieved from http://data.unaids.org/Publications/IRC-pub07/jc967-tradhealers_en.pdf.
- UNAIDS. Global report: UNAIDS report on the global AIDS epidemic. 2012 Retrieved from http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2012/gr2012/20121120_UNAIDS_Global_Report_2012_en.pdf.
- UNAIDS. Progress on HIV brings hope to the province of KwaZulu Natal. 2013 Retrieved from http://www.unaids.org/en/resources/presscentre/featurestories/2013/june/20130604kznpremier/
- World Health Organization. General Guidelines for Methodologies on Research and Evaluation of Traditional Medicine. Geneva: World Health Organization; 2000. [Google Scholar]
- World Health Organization. Traditional medicine strategy 2014–2023. 2013 Retrieved from http://apps.who.int/iris/bitstream/10665/92455/1/9789241506090_eng.pdf?ua=1.
- Wimmer A. How (not) to think about ethnicity in immigrant societies: A boundary making perspective. University of Oxford; 2007. Retrieved from http://www.compas.ox.ac.uk/fileadmin/files/Publications/working_papers/WP_2007/WP0744-Wimmer.pdf. [Google Scholar]