Abstract
Composition of the bacterial microbiome in the vagina and vestibule from 30 women with vulvar vestibulitis syndrome (VVS) and 15 healthy controls were compared by pyrosequencing 16S rRNA amplicons. Vaginal concentrations of interleukin (IL)-1β were determined by ELISA. Questionnaires elicited clinical and symptom data. Eighteen genera were detected in vaginal samples, and 23 genera were identified in vestibule samples, from women with VVS. The genera at both sites and the mean number of genera in subjects with VVS were largely similar to those in control subjects. However, differences were noted including higher proportions of Streptococcus and Enterococcus in women with VVS. Furthermore, Lactobacillus iners was more frequently identified in women with VVS while L. crispatus was more frequent in the control women. The dominant bacterial genera in the vagina closely paralleled the dominant genera present in the corresponding vestibular sample in both groups, leading us to postulate that vaginal secretions are an important source of bacteria present on the vestibule. Vaginal IL-1β levels were similar and varied depending on the dominant bacteria. We conclude in this pilot study that no major differences are apparent in the vagina and vestibule between women with or without VVS, except for an increased prevalence of Streptococcus and L. iners in some women with VVS.
Keywords: interleukin-1β, Lactobacilli, vaginal microbiome, vestibular microbiota, vulvar vestibulitis syndrome
Introduction
Vulvar vestibulitis syndrome (VVS), otherwise known as vestibulodynia, is a clinical diagnosis given to women whose symptoms include intense pain upon attempted vaginal penetration, provoked pain when discrete regions of the vaginal vestibule are touched with a cotton swab, variable degrees of vestibular inflammation ranging from non-detectable to extreme, symptom persistence for at least 3-6 months and with no detectable neurological, microbiological or immunological explanation (Bachmann et al., 2006). The frequency of VVS remains unsubstantiated but a prevalence as high as 15-20% in one United States city has been reported (Harlow and Stewart, 2003). A prevailing hypothesis is that exposure of susceptible women to a variety of environmental or endogenous triggers results in induction of a chronic localized stimulation and/or proliferation of peripheral nerve fibers that result in long lasting allodynia (pain due to application of a normally non-painful stimulus) and hyperalgesia (an exaggerated response to a painful stimulus). The factors that trigger and/or perpetuate this disorder remain speculative. While causality has not been demonstrated, approximately half of the women with VVS can associate a specific event with symptom onset, commonly either sexual intercourse with a specific partner, a vaginal microbial infection, or a vaginal trauma (Harlow and Stewart, 2003; Witkin et al., 2002). Polymorphisms in genes involved in inflammation, anti-microbial immunity or oxidative stress have also been associated with VVS (Jeremias et al., 2000; Gerber et al., 2003; Foster et al., 2004; Babula et al., 2004; Lev-Sagie et al., 2009; Lev-Sagie et al., 2010).
We wished to test the hypothesis that infection or an altered microbial ecology of the vagina and/or vestibule is a factor in the promotion of persistent clinical symptoms characteristic of this disorder. The microbiome of the vagina and vestibule in women with VVS has not previously been evaluated. In this communication we provide an initial characterization of the Lactobacillus species and other bacterial genera present in paired vaginal and vestibular samples from women with VVS and compare the findings to the contemporary analysis of vaginal and vestibular samples from control women.
Material and methods
Subjects
The study population consisted of 30 reproductive age women with strictly defined VVS: pain confined to the vaginal vestibule, pain upon attempted vaginal penetration and symptom duration of at least 6 months. All were diagnosed by the same physician (WJL) and filled out a detailed questionnaire with his assistance. Fifteen healthy reproductive age women from the same practice with no history of vulvodynia, no history or current complaints of a genital tract problem, including a herpesvirus infection or bacterial vaginosis and who were being seen for a routine gynecological examination, served as controls. All of the subjects in both groups were White and none were using oral contraceptives. The procedures followed were in accordance with the ethical standards of the Institutional Review Board of Weill Cornell Medical College and with the Helsinki Declaration. All subjects gave written informed consent. The subjects comprised a convenience sample of women seen between January and December 2011.
Bacterial characterization
All paired vaginal and vestibular samples were obtained by a single investigator who rubbed swabs against the vaginal vestibule or posterior vaginal wall. Samples were placed in Copan Diagnostics ESwab sample collection tubes (Fisher Healthcare, Houston,Tx), stored at −80°C and shipped by overnight express mail on dry ice to the University of Idaho for analysis. The bacterial community composition of samples was determined as previously described (Ravel et al., 2011) by pyrosequencing the V1-V3 region of the 16S rRNA genes amplified from total genomic DNA isolated from the samples. On average there was 3243 sequences for each sample and these were classified using tools of the Ribosomal Database Project (Wang et al., 2007).
Interleukin (IL)-1β determination
During a speculum examination, a cotton swab was placed against the posterior vaginal wall for 5 seconds and then removed into a tube containing 1.0 ml sterile phosphate-buffered saline. The supernatant fraction was collected by centrifugation and stored in aliquots at −80°C. Thawed samples were assayed in duplicate for concentrations of IL-1β by a commercial ELISA kit (R&D Systems, Minneapolis, MN). The lower level of sensitivity was 3.9 pg/ml.
Statistics
An Exact Test was used to test for differences between VVS patients and controls in the number of specific bacterial genera or species of Lactobacillus. IL-1β levels in the various samples were not normally distributed and so differences in concentration were analyzed by the non-parametric Mann-Whitney test. The VVS group was over-sampled to increase the chances for identifying unique bacterial genera and/or Lactobacillus species. A p value < 0.05 was considered significant. The statistics package used for the analysis was SAS (Cary, NC).
Results
Women in the VVS and control groups were of similar mean age (standard deviation), 30.8 (5.7) years and 32.6 (8.1) years, respectively. None of the subjects were overweight (body mass index <25). Six of the experimental subjects had primary VVS, defined as symptom initiation with first attempt at vaginal penetration. The remaining 24 subjects had secondary VVS where their consistent pain upon vaginal penetration was preceded by a period of pain-free penetration. The median duration of symptoms in the VVS group was 28 (range 6-264) months.
The bacterial genera detected in paired vaginal and vestibular samples from women with VVS are shown in Table 1. A total of 18 genera were detected in the vaginal samples and 23 were identified in the vestibule. In all but one woman, the genera present in the vaginal sample were also identified in the vestibule sample. There were 6 genera present in either 1 or 2 vestibular samples that were not present in the corresponding vaginal sample. Additionally, the predominant genus in the vagina was almost always the predominant genus in the vestibule. In one woman with VVS the predominant genus was Anaerococcus in the vestibule and Gardnerella in the vaginal sample. This individual had one of the greatest number of genera from both sites (13 in vagina and 11 in vestibule). Lactobacillus was most often detected in samples from both sites, and when present it was usually the predominant taxon. Other dominant genera at both sites in a minority of subjects were Streptococcus, Gardnerella and Enterococcus. Hence, there were only a few differences in the number of dominant genera between the vaginal and vestibular samples and this difference was not significant (X2 = 2.43, p = 0.85).
Table 1.
Bacterial genera in the vagina and vestibule of women with vulvar vestibulitis syndrome (VVS).
| Taxona | Vagina |
Vestibule |
||
|---|---|---|---|---|
| % positive | % dominant | % positive | % dominant | |
| Lactobacillus | 90.0 | 73.3 | 96.7 | 76.7 |
| Streptococcus | 20.0 | 13.3 | 16.7 | 10.0 |
| Gardnerella | 13.3 | 10.0 | 26.7 | 6.7 |
| Dialister | 13.3 | 0.0 | 3.3 | 0.0 |
| Finegoldia | 13.3 | 0.0 | 20.0 | 0.0 |
| Peptoniphilus | 13.3 | 0.0 | 20.0 | 0.0 |
| Prevotella | 13.3 | 0.0 | 20.0 | 0.0 |
| E. coli/Shigella | 10.0 | 0.0 | 6.7 | 0.0 |
| Anaerococcus | 6.7 | 0.0 | 20.0 | 3.3 |
| Corynebacterium | 6.7 | 0.0 | 13.3 | 0.0 |
| Ureaplasma | 6.7 | 0.0 | 6.7 | 0.0 |
| Staphylococcus | 3.3 | 0.0 | 3.3 | 0.0 |
| Enterococcus | 3.3 | 3.3 | 6.7 | 3.3 |
| Peptostreptococcus | 3.3 | 0.0 | 6.7 | 0.0 |
| Acidovorax | 3.3 | 0.0 | 6.7 | 0.0 |
| Acinetobacter | 3.3 | 0.0 | 0.0 | 0.0 |
| Cloacibacterium | 3.3 | 0.0 | 3.3 | 0.0 |
| Diaphonobacter | 3.3 | 0.0 | 3.3 | 0.0 |
| Bifidobacterium | 0.0 | 0.0 | 3.3 | 0.0 |
| Coriobacter | 0.0 | 0.0 | 3.3 | 0.0 |
| Alloscardovia | 0.0 | 0.0 | 3.3 | 0.0 |
| Clostridiaceae | 0.0 | 0.0 | 6.7 | 0.0 |
| Atopobium | 0.0 | 0.0 | 3.3 | 0.0 |
| Alloscandivia | 0.0 | 0.0 | 3.3 | 0.0 |
Bacterial communities of the vagina and vestibule were characterized by gene amplification and classification of the 16S rRNA amplicon sequences obtained. “Dominant” was defined as any bacterial taxon that constituted > 25% of a community.
The bacterial genera in paired vaginal and vestibular samples from the control women were also similar to each other (Table 2). A total of 13 genera were detected in vaginal samples and 20 were identified in vestibule samples while 12 genera were common to samples from both sites. In only 1 of 15 control cases was there a bacterial genus found in the vagina that was absent from the corresponding vestibule; and 8 woman had one genus that was present in her vestibule but absent from her vagina. The number of bacterial populations in common between vaginal and vestibule samples led us to postulate that vaginal secretions are an important source of bacteria present on the vestibule. As expected from these observations, there were no statistically significant differences between the dominant genera of the vagina and vestibule (X2 = 1.55, p = 0.685).
Table 2.
Bacterial genera in the vagina and vestibule of women without vulvar vestibulitis syndrome (VVS).
| Taxona | Vagina |
Vestibule |
||
|---|---|---|---|---|
| % positive | % dominant | % positive | % dominant | |
| Lactobacillus | 86.7 | 66.7 | 100.0 | 80.0 |
| Gardnerella | 46.7 | 33.3 | 60.0 | 20.0 |
| Atopobium | 33.3 | 0.0 | 20.0 | 0.0 |
| Prevotella | 26.7 | 0.0 | 33.3 | 0.0 |
| Sneathia | 20.0 | 0.0 | 13.3 | 0.0 |
| Megasphaera | 20.0 | 0.0 | 13.3 | 0.0 |
| Veillonella | 20.0 | 0.0 | 6.7 | 0.0 |
| Streptococcus | 13.3 | 0.0 | 13.3 | 0.0 |
| Coriobacter | 13.3 | 0.0 | 6.7 | 0.0 |
| Dialister | 13.3 | 0.0 | 6.7 | 0.0 |
| TM7 | 6.7 | 0.0 | 0.0 | 0.0 |
| E. coli/Shigella | 6.7 | 0.0 | 6.7 | 0.0 |
| Anaerococcus | 6.7 | 0.0 | 13.3 | 0.0 |
| Peptoniphilus | 0.0 | 0.0 | 6.7 | 0.0 |
| Corynebacterium | 0.0 | 0.0 | 6.7 | 0.0 |
| Propionimicrobium | 0.0 | 0.0 | 6.7 | 0.0 |
| Segniliparus | 0.0 | 0.0 | 6.7 | 0.0 |
| Alloscardovia | 0.0 | 0.0 | 6.7 | 0.0 |
| Anaerospaera | 0.0 | 0.0 | 6.7 | 0.0 |
| Campylobacter | 0.0 | 0.0 | 6.7 | 0.0 |
| Clostridiaceae | 0.0 | 0.0 | 6.7 | 0.0 |
Bacterial communities of the vagina and vestibule were characterized by gene amplification and classification of the 16S rRNA amplicon sequences obtained. “Dominant” was defined as any bacterial taxon that constituted > 25% of a community.
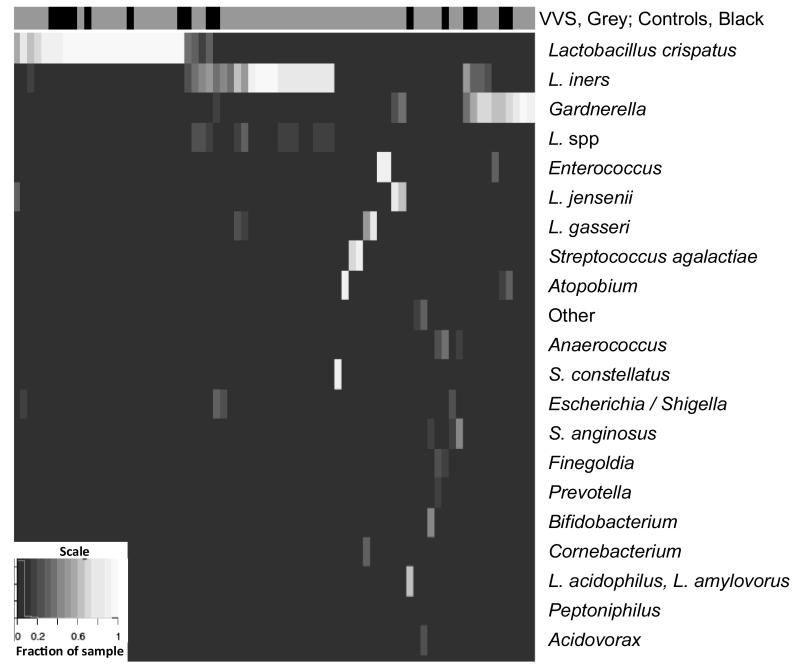
The bacterial populations of vaginal and vestibular samples of women with VVS and control subjects were largely similar at the genus level. Gardnerella and Atopobium were more prevalent in women of the control group, while Streptococcus and Enterococcus were found more often in samples from women with VVS. Accordingly, the dominant genera found on the vestibule or in the vaginas of women with symptoms were not significantly different from those without symptoms (X2 = 3.6, p = 0.38 and X2 = 5.63, p = 0.12, respectively). A heat map showing the frequencies of 21 bacterial taxa found in the vestibular samples of women with VVS and control subjects illustrates an important finding: symptoms of VVS occur in women regardless of whether or not lactobacilli are prominent members of vaginal and vestibular communities (Fig. 1).
Figure 1.
Heat map showing the proportions of 21 bacterial taxa in vestibule samples from cases of VVS and control subjects. Each column is the sample from one woman and whether they exhibited VVS symptoms or not is shown in the top horizontal bar (VVS, grey; Controls, black). The proportions of bacterial populations found in vestibule samples of each woman are shown in columns with high (white) to low (black) proportions of each taxon in the sample.
Although the frequency of Lactobacillus dominance in the vagina and vestibule was similar in both groups, intriguing differences were noted in the prevalence of various Lactobacillus species (Table 3). The vaginas of 53.3% of the controls as opposed to 30.0% of the VVS subjects were dominated by L. crispatus, while L. iners was the dominant Lactobacillus in 13.3% of the controls and 33.3% of VVS subjects. L. gasseri and L. jensenii were each dominant in the vagina only from 2 women in the VVS group. L. gasseri was not detected in the control group and was identified in 26.7% of women in the VVS group; L. jensenii was identified in 26.7% of women in both groups. L. coleohominis was identified only in the vestibule from a minority of women with VVS as well as in control women. None of the differences between women with VVS and controls reached the level of significance.
Table 3.
Lactobacillus species in the vagina and vestibule from women with vulvar vestibulitis syndrome and control women.
| VVS |
Controls |
|||
|---|---|---|---|---|
| Species | % positive | % dominant | % positive | % dominant |
| Vagina | ||||
| L. crispatus | 40.0 | 30.0 | 60.0 | 53.3 |
| L. iners | 43.3 | 33.3 | 33.3 | 13.3 |
| L. gasseri | 26.7 | 6.7 | 0.0 | 0.0 |
| L. jensenii | 26.7 | 6.7 | 26.7 | 0.0 |
| Vestibule | ||||
| L. crispatus | 43.3 | 30.0 | 73.3 | 53.3 |
| L. iners | 50.0 | 33.3 | 33.3 | 6.7 |
| L. gasseri | 36.7 | 3.3 | 0.0 | 0.0 |
| L. jensenii | 26.7 | 6.7 | 46.7 | 0.0 |
| L. coleohominis | 10.0 | 0.0 | 13.3 | 0.0 |
Samples obtained from the vagina and vestibule from 30 women with vulvar vestibulitis syndrome and 15 control women were analyzed for Lactobacillus species by amplification and analysis of the 16S ribosomal RNA gene. “Dominant” was defined as any bacterial genus that constituted > 25% of a community.
In addition, two women in the VVS group were positive for Candida albicans and two were positive for C. glabrata by routine culture. All controls were Candida culture negative. Although the number of Candida-positive subjects was very small there was no difference in the bacterial microbiota between women who were positive or negative for either Candida species (data not shown).
To begin to assess whether controls and VVS patients differed in their pro-inflammatory immune responses to the most prevalent bacterial genera, the vaginal concentrations of the primary pro-inflammatory cytokine, IL-1β, were determined and found to vary widely (Table 4). No significant differences between VVS patients and controls in IL-1β levels in association with Gardnerella, L. crispatus or L. iners predominance were detected. Although the total number of samples tested was small, median IL-1β levels in both VVS patients and controls were reduced in samples dominated by L. crispatus (p = 0.0026) or L. iners (p = 0.0425) as compared to Gardnerella-dominated samples. The differences in IL-1β levels between women with L. crispatus or L. iners-dominated vaginal biotypes did not reach statistical significance.
Table 4.
Vaginal interleukin-1β levels in vaginal secretions of women with VVS symptoms and control subjects in relation to the dominant bacterial genus or species present.
| Bacteria | Median IL-1β in pg/ml (range) a |
||
|---|---|---|---|
| Controls | VVS | Combined | |
| L. crispatus | <3.9 (<3.9-211) | 4.5 (<3.9-91) | <3.9 (<3.9-211) |
| L .iners | 18.2 (7.5-258) | 53.5 (<3.9-107) | 18.2 (<3.9-258) |
| Gardnerella | 100 (<3.9-200) | 134 (29-534) | 118 (<3.9-534)b |
Vaginal secretions were analyzed for concentrations of IL-1β by a commercial ELISA kit. The number of women in the control and VVS groups dominant for L. crispatus was 8 and 8, for L. iners 2 and 10 and for Gardnerella 5 and 3, respectively.
p = 0.0026 Gardnerella vs. L. crispatus and 0.0425 Gardnerella vs. L. iners.
We did not identify any association between bacterial genera in the vagina or vestibule in women with VVS and knowledge of any event associated with symptom initiation, the self-reported history of vaginal yeast infections, primary or secondary VVS, and history of allergy or pregnancy (data not shown).
Discussion
In this pilot study the vaginal and vestibular microbiome in the majority of women with VVS contained the same bacterial genera and there were a similar mean number of genera per subject as in control women. The genera present in our control women paralleled that found in previous investigations (Ravel et al., 2011; Gajer et al., 2012). Differences were noted in the relative frequency of a few dominant genera between the two groups. Gardnerella and Atopobium were identified at a higher frequency in the vagina and vestibule from controls than in women with VVS while Streptococcus was more frequently present and was sometimes dominant in the vagina and vestibule from women with VVS. Gardnerella and Atopobium are components of the vaginal microbiome in a variable proportion of healthy women (Ravel et al., 2011; Gajer et al., 2012). Their presence at high levels has been associated with the occurrence of bacterial vaginosis (Verhelst et al., 2004), a frequently diagnosed vaginal disorder that may or may not be accompanied by clinical symptoms. We stress that all subjects in the present study had no vaginal symptoms. We think that it is highly unlikely that the absence of Gardnerella or Atopobium alters the vaginal microbial milieu to such an extent as to increase the likelihood of development of VVS symptoms. Low concentrations of Streptococcus are typically considered as normal flora while high levels have been associated with a condition known as aerobic vaginitis (Donders et al., 2011). There is a report, however, linking group B Streptococcus with vulvar pain (Mirowski et al., 2012). In addition, lactic acid has been shown to be the major metabolic acid produced by group B Streptococcus and may be involved in induction of tissue toxicity (Kling et al., 2009). Vaginal secretions from women in which Streptococcus was the dominant bacterial phylotype had the highest concentrations of L-lactic acid (unpublished observation). Thus, it is possible that a vaginal flora dominated by Streptococci may contribute to development of VVS in a subset of women. Further studies on larger numbers of women with VVS are obviously necessary to validate or refute this suggestion.
Differences were noted in the presence and frequency of Lactobacillus species between the two groups. While L. crispatus was more frequently present and more often dominant in both the vagina and vestibule from the control women, L. iners was present and dominant at both sites at a higher frequency from women with VVS. L. gasseri was also present only in women with VVS. L. iners and l. gasseri are components of the vaginal microbiota of healthy women (Ravel et al., 2011; Gajer et al., 2012). However, their presence has also been associated with an increased likelihood to develop bacterial vaginosis (Verstraelen et al., 2009). Whether these differences contribute to VVS remain to be determined.
The observation that vaginal concentrations of IL-1β were higher in women whose vaginal microbiota was dominated by Gardnerella as opposed to Lactobacillus parallels previous studies of an association between vaginal IL-1β levels and bacterial vaginosis (Cauci et al., 2003), a condition often characterized by a marked increase in Gardnerella and a diminution or lack of lactobacilli. It is apparent, therefore, that pro-inflammatory immunity is induced in the vagina when this genus predominates. The finding that vaginal IL-1β levels were similar in VVS patient and controls in samples when the vaginal communities were dominated by the same species argues against differences in host immune reactions to a similar bacterial distribution as a factor contributing to altered pain responses. Analysis of additional women and expansion of the immune mediators evaluated is necessary to further evaluate this initial observation.
The observation that communities of the vagina and vestibule were similar parallels previous studies in which the bacterial microbiota of the vagina was found to be similar to that of the labia majora (Shiraishi et al., 2011) and labia minora (Shiraishi et al., 2011; Brown et al., 2007). Thus, it appears that vaginal secretions with accompanying bacteria leak from the vagina, then coat and become the dominant bacterial genera that reside on the vestibular surface.
A limitation of our study is that the number of bacterial genera that were identified represents only the most abundant types present in each woman. Rare genera could not practically be detected by the procedure employed. Thus, it remains possible that one or more undetected bacterial genera may still contribute to symptoms of VVS. Two species of Candida were also detected in four women with VVS and in none of the controls. None of these women had signs or symptoms of candidiasis and, thus, these organisms were most likely commensal. Candida species, chiefly C. albicans is present in the vagina of about 20% of healthy, asymptomatic reproductive age women (Sobel, 2007). In addition, women with frequent episodes of vaginal candidiasis have been shown to have a vaginal microbiota similar to women with no history of candidiasis (Zhou et al., 2009). Thus, the presence of this fungus as a commensal microbe most likely does not alter the vaginal microbiota.
Another limitation of our investigation is the relatively small number of women evaluated. The present study, therefore, must be labeled as hypothesis testing and hopefully will serve as a starting point for more expansive investigations to evaluate whether vaginal flora differences influence VVS symptoms. In addition, VVS is a clinical diagnosis of exclusion and, therefore, women with this diagnosis are a heterogeneous group with most likely varying underlying causes. Further characterization of VVS subgroups with well defined etiologies will lead to an improved appreciation of a possible influence of the vaginal and vestibular microbiota on this syndrome. Vaginal and vestibular sample collection in the women with VVS occurred long after the initiation of clinical symptoms. Therefore, we cannot rule out the possibility that a unique bacterial genus or a unique combination of bacteria provided the initial but transient trigger for symptom onset. Once initiated the pain cycle may have become persistent due to secondary mechanisms.
In conclusion, while the majority of women with VVS appear to have a bacterial distribution that is similar to control women, small differences in a minority of subjects were detected. There were varying rates of colonization with Candida, Lactobacillus species and Streptococcus. Further studies on larger numbers of women with enhanced ability to evaluate down to the species level are needed to resolve whether differences in bacterial and/or fungal colonization or alterations in the vaginal microbiome contribute to symptoms in a subset of VVS subjects. It will also be of major interest to determine whether a specific vaginal microbiota elicits production of compounds that stimulate pathological peripheral nerve activation in the vestibule.
Acknowledgements
This study was supported by a grant from the National Vulvodynia Association to SSW and LJF and grant P20RR16448 from the National Institutes of Health (USA) to LJF.
The technical assistance of Hannah Mossop from Weill Cornell and Sanqing Yuan from the University of Idaho are gratefully acknowledged. Matt Settles from the University of Idaho provided bioinformatic support for analysis of pyrosequencing data and classification of partial 16S rRNA gene sequences. We thank Drs. Georgios Doulaveris, Theofani Orfanelli, Tomi Kanninen and Giovanni Sisti for helpful discussions and a critical review of the manuscript.
References
- Babula O, Danielsson I, Sjoberg I, Ledger WJ, Witkin SS. Altered distribution of mannose-binding lectin alleles at exon I codon 54 in women with vulvar vestibulitis syndrome. Am J Obstet Gynecol. 2004;191:762–766. doi: 10.1016/j.ajog.2004.03.073. [DOI] [PubMed] [Google Scholar]
- Bachmann GA, Rosen R, Pinn VW, et al. Vulvodynia. A state-of-the-art consensus on definitions, diagnosis and management. J Reprod Med. 2006;51:447–456. [PubMed] [Google Scholar]
- Brown CJ, Wong M, Davis CC, Kanti A, Zhou X, Forney LJ. Preliminary characterization of the normal microbiota of the human vulva using cultivation-independent methods. J Med Microbiol. 2007;56:271–276. doi: 10.1099/jmm.0.46607-0. [DOI] [PubMed] [Google Scholar]
- Cauci S, Guaschino S, de Aloysio D, Driussi S, De Santo D, Penacchioni P, Quadrifoglio F. Interrelationships of interleukin-8 with interleukin-1β and neutrophils in vaginal fluid of healthy and bacterial vaginosis positive women. Mol Hum Reprod. 2003;9:53–58. doi: 10.1093/molehr/gag003. [DOI] [PubMed] [Google Scholar]
- Donders G, Bellen G, Rezeberga D. Aerobic vaginitis in pregnancy. BJOG. 2011;118:1163–1170. doi: 10.1111/j.1471-0528.2011.03020.x. [DOI] [PubMed] [Google Scholar]
- Foster DC, Sazenski TM, Stodgell CJ. Impact of genetic variation in interleukin-1 receptor antagonist and melanocortin-1 receptor genes on vulvar vestibulitis syndrome. J Reprod Med. 2004;49:503–509. [PubMed] [Google Scholar]
- Gajer P, Brotman RM, Bai G, et al. Temporal dynamics of the human vaginal microbiota. Sci Transl Med. 2012;4:ra52. doi: 10.1126/scitranslmed.3003605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerber S, Bongiovanni AM, Ledger WJ, Witkin SS. Interleukin-1β gene polymorphism in women with vulvar vestibulitis syndrome. Eur J Obstet Gynecol Reprod Med. 2003;107:74–77. doi: 10.1016/s0301-2115(02)00276-2. [DOI] [PubMed] [Google Scholar]
- Harlow BL, Stewart EG. A population-based assessment of chronic unexplained vulvar pain: Have we underestimated the prevalence of vulvodynia? J Am Med Womens Assoc. 2003;58:82–88. [PubMed] [Google Scholar]
- Jeremias J, Ledger WJ, Witkin SS. Interleukin 1 receptor antagonist gene polymorphism in women with vulvar vestibulitis. Am J Obstet Gynecol. 2000;182:283–5. doi: 10.1016/s0002-9378(00)70212-2. [DOI] [PubMed] [Google Scholar]
- Kling DE, Cavicchio AJ, Sollinger CA, Madoff LC, Schnitzer JJ, Kinane TB. Lactic acid is a potential virulence factor for group B Streptococcus. Microb Pathog. 2009;46:43–52. doi: 10.1016/j.micpath.2008.10.009. [DOI] [PubMed] [Google Scholar]
- Lev-Sagie A, Linhares IM, Ledger WJ, Witkin SS. A manganese superoxide dismutase gene polymorphism and development of vulvar vestibulitis syndrome following physical vaginal trauma. It J Gynaecol Obstet. 2010;22:59–64. [Google Scholar]
- Lev-Sagie A, Prus D, Linhares IM, Lavy Y, Ledger WJ, Witkin SS. Polymorphism in a gene coding for the inflammasome component NALP3 and recurrent vulvovaginal candidiasis in women with vulvar vestibulitis syndrome. Am J Obstet Gynecol. 2009;200:303.e1–303.e6. doi: 10.1016/j.ajog.2008.10.039. [DOI] [PubMed] [Google Scholar]
- Mirowski GW, Schlosser BJ, Stika CS. Cutaneous vulvar streptococcal infection. J Low Genit Tract Dis. 2012;16:281–284. doi: 10.1097/LGT.0b013e3182431753. [DOI] [PubMed] [Google Scholar]
- Ravel J, Gajer P, Abdo Z, et al. Vaginal microbiome of reproductive-age women. Proc Natl Acad Sci USA. 2011;108(suppl 1):4680–3687. doi: 10.1073/pnas.1002611107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiraishi T, Fukuda K, Morotomi N, Imamura Y, Mishima J, Imai S, Miyazawa K, Taniguchi H. Influence of menstruation on the microbiota of healthy women’s labia minora as analyzed using a 16S rRNA gene-based clone library method. Jpn J Infect Dis. 2011;64:76–80. [PubMed] [Google Scholar]
- Sobel JD. Vulvovaginal candidosis. Lancet. 2007;369:1961–71. doi: 10.1016/S0140-6736(07)60917-9. [DOI] [PubMed] [Google Scholar]
- Verhelst R, Verstraelen H, Claeys G, Verschraegen G, Delanghe J, Van Simaey L, De Ganick C, Temmerman M, Vaneechoutte M. Cloning of 16S rRNA genes amplified from normal and disruoted vaginal microflora suggests a strong association between Atopobium vaginae, Gardnerella vaginalis and bacterial vaginosis. BMC Microbiol. 2004;4:16–26. doi: 10.1186/1471-2180-4-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verstraelen H, Verheist R, Claeys G, De Backer E, Temmerman M, Vaneechoutte M. Longitudinal analysis of the vaginal microflora in pregnancy suggests that L. crispatus promotes the stability of the normal vaginal microflora and that L. gasseri and.or L. iners are more conducive to the occurrence of abnormal vaginal microflora. BMC Microbiol. 2009;9:116. doi: 10.1186/1471-2180-9-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q, Garrity GM, Tiedje JM, Cole JR. Naïve Bayesian Classifier for rapid assignment of rRNA sequences into the new bacterial taxonomy. Appl Environ Microbiol. 2007;73:5361–5267. doi: 10.1128/AEM.00062-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkin SS, Gerber S, Ledger WJ. Differential characterization of women with vulvar vestibulitis syndrome. Am J Obstet Gynecol. 2002;87:589–594. doi: 10.1067/mob.2002.125889. [DOI] [PubMed] [Google Scholar]
- Zhou X, Westman R, Hickey R, Hansmann MA, Kennedy C, Osborn TW, Forney LJ. Vaginal microbiota of women with frequent vulvovaginal candidiasis. Infect Immun. 2009;77:4130–4135. doi: 10.1128/IAI.00436-09. [DOI] [PMC free article] [PubMed] [Google Scholar]