Abstract
Background:
Despite known benefits, only a small proportion of HIV-infected children in sub-Saharan Africa know their status and limited disclosure interventions exist. Namibia's Ministry of Health and Social Services developed and implemented a multipronged intervention to support health care workers (HCWs) and caregivers in the disclosure process.
Methods:
The intervention included a staged disclosure cartoon book, child and caregiver readiness assessment tools, a monitoring form to track progress over visits, and HCW training curriculum. We conducted qualitative interviews with 35 HCWs and 46 caregivers of HIV-positive children at 4 high volume HIV clinics. Interviews elicited detailed information about intervention uptake and impact. HCWs also participated in a self-efficacy survey.
Results:
The intervention improved HCW and caregiver confidence and communication skills in pediatric disclosure. The most valuable intervention component was the disclosure cartoon book, which provided structure, language, and guidance for a gradual disclosure process. HCWs reported it greatly reduced caregiver resistance to disclosure. Both caregivers and HCWs reported improved knowledge and ability to support the pediatric patient, improved child understanding of how HIV medications work, increased child hopefulness for their future, and improved child adherence to care and treatment. HCW self-efficacy surveys found that HCWs who received training felt more confident in their ability to engage in the disclosure process.
Conclusions:
HCWs and caregivers highly endorsed the intervention. Given the urgency to address pediatric HIV disclosure in Africa, and the utility and low cost of the locally-produced disclosure tool, this approach may be useful in other similar settings.
Key Words: disclosure, pediatric HIV, HIV education, adherence, program evaluation
INTRODUCTION
Availability of antiretroviral therapy (ART) has significantly improved the length and quality of life for children living with HIV in sub-Saharan Africa.1,2 The World Health Organization recommends that school-aged children be fully informed and younger children told partial information about their diagnosis.3 Children who learn their HIV status in structured, age appropriate, and supportive ways may be more likely to adhere to treatment and less likely to become depressed.4–13 Yet, child disclosure remains a challenge in sub-Saharan Africa.4,8,9,14,15 Caregivers often feel unprepared to disclose to children, fearing blame, negative judgment, resentment, stigma resulting from the child telling others, or that disclosure will psychologically harm the child.4,7,8,11,14,16–25 Caregivers often desire health care worker (HCW) support for the disclosure process.7,8,18,26–28 However, HCWs often do not feel prepared to fulfill this role,4,17,18,27 and there are few structured interventions to help caregivers and HCWs with the disclosure process.4,5,9,18,24,27,29
Namibia has an antenatal HIV prevalence of nearly 18%30 and over 10,000 children have initiated ART.31 With scale-up of access to ART, HCWs reported experiencing high levels of stress due to their own unpreparedness for talking with pediatric patients about adherence, their HIV status, and caregiver resistance to pediatric disclosure. In response, the Namibian Ministry of Health and Social Services (MOHSS), in collaboration with the International Training and Education Center for Health (I-TECH), developed and implemented an empirically grounded and theoretically informed32–37 child disclosure intervention to reduce barriers to and provide support for HCWs and caregivers in the disclosure process (Fig. 1).
FIGURE 1.
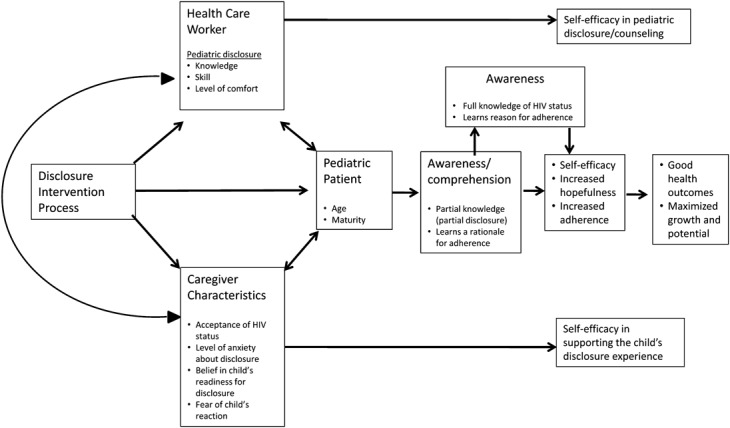
Child disclosure intervention conceptual model.
The intervention, intended for use with children aged six and above, consists of 4 components, including (1) a 5-chapter child-friendly book with colorful cartoon drawings designed to guide HCWs and caregivers in a gradual disclosure process, (2) a tool that assists HCWs to assess caregiver and child readiness for full HIV disclosure and systematically work through barriers, (3) a disclosure form which helps HCWs monitor children's understanding of their disease status over time, and (4) HCW training curriculum on using the disclosure book and tools. The cartoon book, entitled “Why I take my medicine,” was inspired by a book at Baylor Pediatric Clinic in Botswana, and adapted to the Namibian context. Chapter 1 orients the child to thinking about their future, whereas chapters 2–4 describe how taking medicine can keep “body soldiers” strong and help fight the “bad guys,” so the child stays healthy. The story emphasizes the importance of taking medication consistently to keep the “bad guys” asleep. HIV-identifying terminology is not used until chapter 5 when the “body soldiers” are labeled as CD4 cells and the “bad guys” as HIV. The pace of book completion depends on several factors, including the child's understanding of each chapter, the child's developmental stage, and the caregiver's and child's readiness for full HIV disclosure. Since the intervention was implemented in 2010, 317 health care workers from 82 Namibian health facilities have been trained on the disclosure intervention. The book is available in 6 Namibian languages, including English. This article describes evaluation findings on HCW and caregiver perspectives on the effectiveness of the intervention in increasing their capacity to engage in the disclosure process and improving pediatric patient adherence behavior.
METHODS
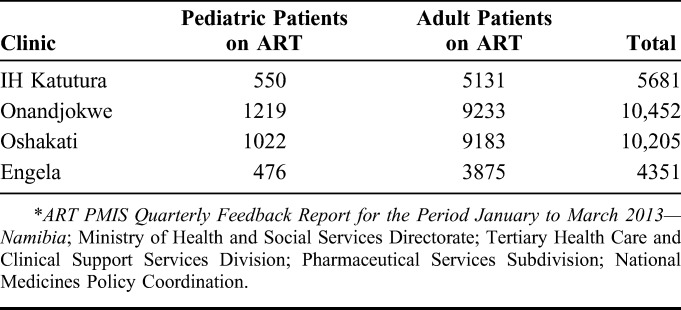
We performed a cross-sectional evaluation of the disclosure intervention at 4 high volume pediatric HIV clinics in the country whose staff were trained in the intervention in 2010 (Table 1).
TABLE 1.
Evaluation Sites and ART Patient Volumes*
Data Collection
Researchers used semistructured questionnaires to lead in-depth interviews at each evaluation site from May to June 2013. Interviews explored the disclosure process in general and elicited descriptive information about intervention uptake and perceived impact. All HCWs (doctors, nurses, and community counselors) who interacted with pediatric HIV patients at the selected sites were interviewed (N = 35). In addition, after the interviews, 34/35 HCWs completed a 6-question written quantitative survey focused on self-efficacy to assist in the disclosure process. Caregivers who were aged 18 years or older and accompanying a child aged 7–15 years already on ART were sampled in the order of their arrival at the clinic on pediatric outpatient days. Interviews from 46 caregivers (enough to reach informational redundancy38) across the 4 facilities reporting that either they or their children were exposed to the disclosure intervention were included in this evaluation.
Interviews were conducted in English or Oshiwambo, digitally recorded, and subsequently transcribed. Interviews conducted in Oshiwambo were translated into English by bilingual members of the interview team.
Data Analysis
Transcripts were independently coded, reviewed by a second investigator, and coding disagreements resolved through discussion. Interview transcripts were analyzed using an inductive approach combining grounded theory and framework analysis.39–41 The goal of analysis was to understand whether the intervention was successful in breaking down barriers to disclosure and effective in influencing children's behavior, and to clarify the intervention's most important “active ingredients.”42
Atlas.ti v.7 (Scientific Software Development GmbH, Berlin, Germany) was used to support coding, analysis, and data management. HCW self-efficacy surveys were analyzed using STATA Intercooled version 12 (StataCorp LP; College Station, TX) T-tests were used to compare HCW self-identified levels of confidence performing disclosure-related procedures between HCWs who had and had not received the formal Namibian training in the disclosure intervention.
Ethical Considerations
The ethical review board of the University of Washington determined that the disclosure evaluation was not human subjects research as the intervention had been implemented nationally under the auspices of the Namibian MOHSS as part of routine pediatric patient care. The Namibian MOHSS ethics review committee reviewed and approved the study. All interview participants provided written informed consent.
RESULTS
Study Population
HCWs interviewed included community counselors (9), doctors (9), and nurses (17). The majority reported having between 2 and 9 years of experience working at their respective facilities. The 46 caregivers interviewed were mostly female (91%), and the majority (59%) were the biological mother of the child (Table 2). No caregivers exposed to the book refused to begin the disclosure process. Approximately, half of the caregivers (56%) reported that children knew their HIV status (full disclosure) at the time of the interview. The median age of disclosure for these children was 9.5 years.
TABLE 2.
Caregiver Demographics

Disclosure Beliefs and Practices
HCWs believed that developmentally appropriate disclosure was important for the child's long-term outcomes because it would improve adherence, reduce risky sexual behavior, improve the child's capacity to recognize side effects, and improve communication between the HCW and patient. Caregivers reported that disclosure was important for adherence reasons, so children could manage their sexual behavior and alcohol consumption as they got older, and to avoid the child's learning about their status from neighbors or schoolmates. However, both caregivers and HCWs described a range of barriers that could prevent disclosure from occurring that included caregiver fears of blame, stigma, and negative psychological impact on the child and lack of confidence or knowledge of how to broach the topic in an age-appropriate fashion.
Intervention Implementation
Almost all (N = 31) of the 35 HCWs regularly used some component of the disclosure intervention with children and/or caregivers. Factors that seemed to influence use of the intervention components among HCWs at each site were the number of individuals trained in disclosure and whether or not a specific HCW profession was assigned to complete all or only certain aspects of the intervention. The assessment tool and disclosure form are designed to be completed by doctors and nurses, whereas the disclosure book is to be used by doctors, nurses, and counselors. In practice, assigned responsibilities varied by site.
The assessment tool was used by approximately half (N = 17) of interviewed HCWs. Challenges with using the tool included the time it took to complete the questionnaire and questions about family support that were not applicable in situations where family structure was fluid. HCWs who used the tool reported it facilitated gathering information about the child/caregiver relationship that helped them focus and individually tailor disclosure conversations.
[I]t [disclosure assessment tool] allows us to see what is the social circumstances of the child, because at times when you are assessing a child for disclosure that tool also helps us to understand the circumstances the child is staying in, because then obviously after disclosure the child needs a lot of social support—that family readiness tool allows us to do so (P47: KAT_HCW).
The disclosure tracking form was frequently used by 21 of the 35 HCWs interviewed. HCWs reported the biggest challenge to routinely using the form was lack of time. Those who used it reported the form helped them keep track of child progress, ensured continuity of care, and were frustrated that other HCWs in the clinic were not completing the form.
[Y]ou are not the only one who works with the child; [F]illing in the form will inform the next person as to where you stopped, like which chapters you have covered or if full disclosure is needed or the child might have said she knows nothing. So, the next person will know whether to start all over again or where to continue (P25: ENG_HCW).
Overall, the disclosure book was the intervention component most frequently and enthusiastically used by HCWs (N = 31). Of the 4 HCWs who did not use the disclosure book, none had been formally trained in using it. Those who routinely used the book reported not using it when they had inadequate time, or when caregivers were not available to consent to the process. HCWs who used the disclosure book reported that it had increased their communication skills and confidence in performing disclosure.
I think that tool [booklet] has made it easier for us to be able to discuss these HIV issues with children because I think it reduces the whole explanation to something that a child can relate to (P47: KAT_HCW).
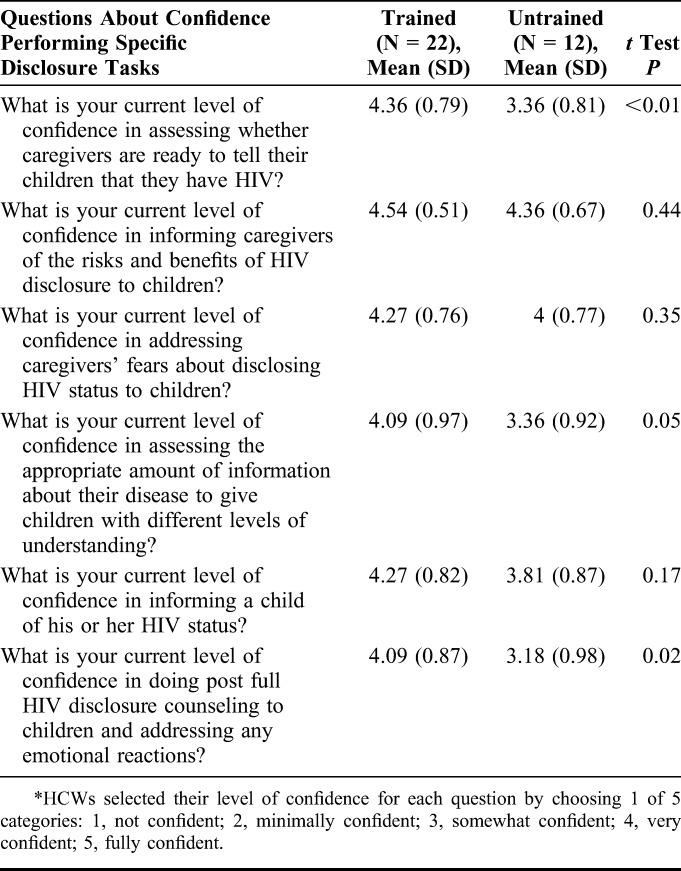
Of the 34 HCWs who completed the self-efficacy survey, 22 had received formal training on the disclosure intervention, 2 reported having other forms of training in disclosure, and 10 reported not receiving any training. When compared with HCWs who reported receiving no official training in disclosure, HCWs who received training reported increased confidence in assessing readiness, sharing information with children, and providing postdisclosure counseling (Table 3).
TABLE 3.
HCW Self-Efficacy Survey Results (N = 34)*
Benefits of Using the Disclosure Book
HCWs appreciated the book's content because it supported them through a standardized disclosure process and provided simple language for discussing complicated concepts.
[The book] simplifies the disclosure process … because …. it is arranged stage-wise…. you are building a story and you reach full disclosure, it's not haphazard. And if maybe we were to do it from our own heads, we can jumble things and mix things and actually create problems with the kids that we are disclosing to. [I]t builds the story as you go for the kids to understand and it uses very simple pictures…and a simplified….language …. (P90: OSH_HCW).
HCWs found that the staged process of disclosure facilitated children's understandings about taking medication before reaching full disclosure and helped children be better prepared for full disclosure.
This book was very helpful in the sense that the book has pictures and kids can also see for themselves how the good and bad guys look, at the end of the session with a child, you can see that it is very fruitful, the book helps to create [a] conducive environment. So when we get to chapter 5, the final chapter, the child is already mentally prepared for that chapter. When it comes to full disclosure it makes it very easy because of that preparedness of the child (P96: OSH_HCW).
HCWs also found the book improved HIV comprehension for children who already knew their status.
[M]ost of them…, they are just told at home, “you are HIV positive, your mother died with HIV.” So for them to know what is all this HIV thing about, they really don't understand, and why someone who is HIV positive should be taking that medicine on a daily basis. So with that tool, I've actually seen it is quite helpful for them to understand that whole process, so if they are talking about HIV and these are the bad guys in me, it means I have to take my medication throughout, to keep those bad guys asleep (P17: ENG_HCW).
HCWs reported that talking about the book not only assisted caregivers with language to discuss the virus with children, but also helped caregivers better understand the disease.
They [caregivers] generally like the book. It also makes the caregiver understand the virus. You would assume that they already know, but once you use that book you will see the interest of the parent go higher. They will say that I did not understand this myself, so it also works both ways (P93: OSH_HCW).
Overall, HCWs felt that using the disclosure book reduced caregiver resistance to disclosure.
If you didn't use that book most of them [caregivers] they will not accept. The book is making a good job, because if you just tell them the child needs to be told why he is taking the medication, they will always tell you that he/she is too young but when you go through this book, they will just be nodding their heads like this is good (P92: OSH_HCW).
Caregivers consistently corroborated HCW reports of positive reactions to the disclosure book. They described how the book improved both their own and their child's understanding of how important medication was to staying healthy.
That book really helps us. …. it has also taught to me personally (P87: mother of 13 year old male).
The book makes children understand, we should not stop with it [medication] at all because it has one small person when you don't take your medication and a bigger person when you do take your medication…the small person is like when you don't take your medication you will abandon yourself, but then if you are drinking [taking your medicine] you are moving forward. So that book, don't leave it, we should use the book to teach the children and it should be reviewed with them when they come to the hospital (P32: mother of 12 year old female).
Caregivers reported that the book was helpful in increasing their skills in supporting the child in medication adherence.
They [the HCWs] gave me a book which I assisted the child to go through, I told her about how she should take her medication and explained the pictures of healthy children from the book. And I told her that if she does not take her medication her CD4 counts will go down (will be low) and the bad guys will wake up and then you will be weak. P35: mother of 10 year-old female).
It has helped because this book, even if you are travelling now, you will remember to put the medication in the bag. So, the book has helped me a lot, because [I] remember that page in the book (P2: mother of 8 year-old male).
Both caregivers and HCWs reported that the structure of the book helped to motivate children to take their medicine because of its focus on the future.
It makes them happy actually if you explain to them that …. if you are having this ARV, …even if you have HIV you can still grow up to become a nurse or a doctor from there they will be having hope that they can still achieve their goals (P92: OSH_HCW).
I like it because it's nice, there is nothing that can scare the child, where the child might think that if I continue to take the medication I might die like my uncle…the book encourages the kids that if they continue to take their medication and go to school they can become whatever I want to be (P78: mother of 11 year-old boy).
Both HCWs and caregivers believed that using the disclosure book facilitated adherence, regardless of whether the child had reached full disclosure or not.
But if you ask such parent/caregiver about the child's reactions at home after partial disclosure was given, the parent/caregiver will tell you that “S/he is now fine, because you will find him/her (referring to the child) saying: bring the medicines, it was said that the thing will wake up.” That's why a parent/caregiver will find the information to be enough to the child for the time being, we should not add words like HIV and others until the time is right (P98: OSH_HCW).
The child always talks about bad guys. Sometimes, when he almost forgets his medication he says, “no, I am going to take my medication because these bad guys are trying to fight me” (P1: mother of 7 year-old boy).
Caregivers also reported that reading through the disclosure book helped the child in keeping track of their clinic days.
She knows that she should come [to the clinic] and she also tells me “tomorrow is the day for the doctor” (P26: mother of 9 year old girl).
DISCUSSION
There has been widespread reporting on the barriers to pediatric disclosure and various disclosure guidelines and frameworks exist.3,33,36,43 However, information on specific tools and resources for low-resource settings is sparse.9 The Namibian disclosure intervention responds to recommendations to develop resources that support disclosure as an ongoing process that is integrated into routine clinical care,4,7,21,25,29,33–35,44 and does not rely on availability of professionals such as social workers or psychologists. Our evaluation used qualitative methods to explore how a novel child disclosure intervention breaks down barriers to the disclosure process. Qualitative methods are useful for describing contextual factors and latent influences (eg, motivation) and for understanding which aspects of an intervention work well and why.37,42
Similar to the evaluation of a multipronged intervention implemented in Puerto Rico,27 we found having a structured intervention improved HCW confidence to engage in disclosure. Social cognitive theory suggests that self-efficacy is an important precursor to implementing challenging behaviors, for example, disclosure.32,45,46 The enthusiastic uptake of the disclosure book by HCWs in busy Namibian clinic settings and adaptation of its language by caregivers is related to their belief in its efficacy as they witnessed children's positive response. The disclosure book was designed for gradual disclosure that is matched to child readiness and where “HIV” is not mentioned until the end. An unexpected benefit of this approach is that the delayed mention of HIV reduced caregiver resistance to beginning the disclosure process. Although not directly tackling issues of stigma, child resentment and blame, the description of keeping “bad guys” asleep so “body soldiers” stay strong and protect the child provides a hopeful, nonthreatening narrative that reduces caregiver fear and increases confidence to begin the process.
In addition to providing a description and evaluation of a specific intervention, our findings have implications for future research. Although disclosure is often referred to as a process, much of the literature on child disclosure focuses on describing prevalence, when and why it occurred, and whether it positively impacts adherence,9 thus forcing its operationalization as a dichotomous variable. Our findings suggest the underlying mechanism for improving adherence may not be knowledge of HIV status, but whether children understand why taking medicine is important. The simplified concept of regularly taking medicine to keep “body soldiers” strong and “bad guys asleep” resonated with both children and caregivers and reportedly helped motivate adherence to care and treatment. In addition, categorizing “disclosure status” often relies on children reporting they “have HIV.”9 We found that children may report they “have HIV” without understanding what it means. Future research should take into consideration the complexity of disclosure classification and attempt to clarify the underlying causal mechanisms of disclosure interventions. Finally, how a child is told he/she is HIV positive may be as important as whether a child is told. The future-oriented nature of the Namibian disclosure book, focusing on what children want to grow up to be, sets the tone advocated by scholars and practitioners for approaches that promote future orientation, and resilience rather than focusing on pathologies.34
This evaluation has a variety of strengths and limitations. It was conducted after HCWs at the HIV clinics had been trained and does not build on efficacy research of this particular disclosure intervention. However, the evaluation did enable us to look at intervention uptake, experience, and perceived benefits in routine settings. There could have been some social desirability bias in responses by HCWs and caregivers. However, the detail with which informants described children's responses using language from the disclosure book, the corroborating reports from both caregivers and HCWs, and the observed use of the disclosure intervention on the day interviews were conducted strengthen the validity of our findings. Caregiver reports of improved adherence by children exposed to the intervention are not accompanied by supporting viral load data. However, our qualitative data describes a strong reduction in well-established barriers to disclosure in high-volume routine clinic settings, an important first step in the causal pathway leading from partial or full disclosure to increased adherence.
To the best of our knowledge, this is the first formal evaluation of a disclosure intervention in sub-Saharan Africa. Given the well-established urgency to address pediatric disclosure, this intervention and evaluation provide a timely and significant contribution to the evidence base of successful disclosure interventions to improve health outcomes of children living with HIV.
Footnotes
Funding for this evaluation was provided by the US National Institute of Health 1R21HD074071—01.
The authors have no conflicts of interest to disclose.
G.O.: protocol development, data collection, coding of caregiver and health care worker articles, data analysis, and article development; L.B. and M.S-P.: protocol development, data interpretation, and article development; K.B-S.: data collection, coding of HCW transcripts, analysis, and article development; L.F.: data collection, coding of caregiver transcripts, and article development; F.K-T., N.H., and G.J-S.: protocol development, data interpretation, critical review, and input of article.
REFERENCES
- 1.GLOBAL HIV/AIDS RESPONSE: Epidemic Update and Health Sector Progress Towards Universal Access Progress Report: United Nations Program on HIV/AIDS; World Health Organization; Geneva, Switzerland; 2011. [Google Scholar]
- 2.UNAIDS. Know your epidemic. Available at: http://www.unaids.org/en/dataanalysis/knowyourepidemic/. Accessed October 4, 2012.
- 3.World Health Organization. Guidelines on HIV Disclosure Counselling for Children up to 12 Years of Age. Geneva, Switzerland: WHO; 2011. [PubMed] [Google Scholar]
- 4.Kouyoumdjian F, Meyers T, Mtshizana S. Barriers to disclosure to children with HIV. J Trop Pediatr. 2005;51:285–287. [DOI] [PubMed] [Google Scholar]
- 5.Vreeman RC, Nyandiko VM, Ayaya SO, et al. The perceived impact of disclosure of pediatric HIV status on pediatric antiretroviral therapy adherence, child well-being, and social relationships in a resource-limited setting. AIDS Patient Care STDs. 2010;24:639–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vaz LME, Eng E, Maman S, et al. Telling children they have HIV: lessons learned from findings of a qualitative study in sub-Saharan Africa AIDS Patient Care STDs. 2010;24:247–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vaz L, Corneli A, Dulyx J, et al. The process of HIV status disclosure to HIV-positive youth in Kinshasa, Democratic Republic of the Congo. AIDS Care. 2008;20:8420852. [DOI] [PubMed] [Google Scholar]
- 8.Moodley K, Myer L, Michaels D, et al. Paediatric HIV disclosure in South Africa—caregivers' perspectives on discussing HIV with infected children. S Afr Med J. 2006;96:201–204. [PubMed] [Google Scholar]
- 9.Vreeman RC, Gramelspacher AM, Gisore PO, et al. Disclosure of HIV status to children in resource-limited settings: a systematic review. J Int AIDS Soc. 2013;16:18466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wiener LS, Kohrt BA, Battles HB, et al. The HIV experience: youth identified barriers for transitioning from pediatric to adult care. J Pediatr Psychol. 2011;36:141–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vaz LM, Maman S, Eng E, et al. Patterns of disclosure of HIV status to infected children in a Sub-Saharan African setting. J Dev Behav Pediatr. 2011;32:307–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bikaako-Kajura W, Luyirika E, Purcell DW, et al. Disclosure of HIV status and adherence to daily drug regimens among HIV-infected children in Uganda. AIDS Behav. 2006;10(4 suppl):S85–S93. [DOI] [PubMed] [Google Scholar]
- 13.Butler AM, Williams PL, Howland LC, et al. Impact of disclosure of HIV infection on health-related quality of life among children and adolescents with HIV infection. Pediatrics. 2009;123:935–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hejoaka F. Care, and secrecy: being a mother of children living with HIV in Burkina Faso. Soc Sci Med. 2009;69:869–876. [DOI] [PubMed] [Google Scholar]
- 15.Menon A, Glazebrook C, Campain N, et al. Mental health and disclosure of HIV status in Zambian adolescents with HIV infection: implications for peer-support programs. J Acquir Immune Defic Syndr. 2007;46:349–354. [DOI] [PubMed] [Google Scholar]
- 16.Brown BJ, Oladokun RE, Osinusi K, et al. Disclosure of HIV status to infected children in a Nigerian HIV Care Programme. AIDS Care. 2011;23:1053–1058. [DOI] [PubMed] [Google Scholar]
- 17.Kallem S, Renner L, Ghebremichael M, et al. Prevalence and pattern of disclosure of HIV status in HIV-infected children in Ghana. AIDS Behav. 2011;15:1121–1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Myer L, Moodley K, Hendricks F, et al. Healthcare providers' perspectives on discussing HIV status with infected children. J Trop Pediatr. 2006;52:293–295. [DOI] [PubMed] [Google Scholar]
- 19.Biadgilign S, Deribew A, Amberbir A, et al. Factors associated with HIV/AIDS diagnostic disclosure to HIV infected children receiving HAART: a Multi-Center study in Addis Ababa, Ethiopia. PLoS One. 2011;6:e17572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fetzer BC, Mupenda B, Lusiama J, et al. Barriers to and facilitators of adherence to pediatric antiretroviral therapy in a sub-Saharan setting: insights from a qualitative study. AIDS Patient Care STDs. 2011;25:611–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vreeman RC, Nyandiko WM, Ayaya SO, et al. The perceived impact of disclosure of pediatric HIV status on pediatric antiretroviral therapy adherence, child well-being, and social relationships in a resource-limited setting. AIDS Patient Care STDs. 2010;24:639–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Demmer C. Experiences of families caring for an HIV-infected child in KwaZulu-Natal, South Africa: an exploratory study. AIDS Care. 2011;23:873–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vaz LM, Eng E, Maman S, et al. Telling children they have HIV: lessons learned from findings of a qualitative study in sub-Saharan Africa. AIDS Patient Care STDs. 2010;24:247–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wiener L, Mellins CA, Marhefka S, et al. Disclosure of an HIV diagnosis to children: history, current research, and future directions. J Dev Behav Pediatr. 2007;28:155–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lesch A, Swartz L, Kagee A, et al. Paediatric HIV/AIDS disclosure: towards a developmental and process-oriented approach. AIDS Care. 2007;19:811–816. [DOI] [PubMed] [Google Scholar]
- 26.Petersen I, Bhana A, Myeza N, et al. Psychosocial challenges and protective influences for socio-emotional coping of HIV+ adolescents in South Africa: a qualitative investigation. AIDS Care. 2010;22:970–978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blasini I, Chantry C, Cruz C, et al. Disclosure model for pediatric patients living with HIV in Puerto Rico: design, implementation, and evaluation. Dev Behav Pediatr. 2004;25:181–189. [DOI] [PubMed] [Google Scholar]
- 28.De Baets AJ, Sifovo S, Parsons R, et al. HIV disclosure and discussions about grief with Shona children: a comparison between health care workers and community members in Eastern Zimbabwe. Soc Sci Med. 2008;66:479–491. [DOI] [PubMed] [Google Scholar]
- 29.Domek GJ. Debunking common barriers to pediatric HIV disclosure. J Trop Pediatr. 2010;56:440–442. [DOI] [PubMed] [Google Scholar]
- 30.Report of the 2010 National HIV Sentinel Survey. Windhoek, Namibia: Ministry of Health and Social Services (MOHSS); 2010. [Google Scholar]
- 31.Ugburo EO, Sumbi VM, Ongeri B. Quarterly ART PMIS Feedback Report for the Period January to March 2013. Windhoek, Namibia: Ministry of Health and Social Services—Pharmaceutical Services Division; 2013. [Google Scholar]
- 32.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. [DOI] [PubMed] [Google Scholar]
- 33.Gerson AC, Joyner M, Fosarelli P, et al. Disclosure of HIV diagnosis to children: when, where, why, and how. J Pediatr Health Care. 2001;15:161–167. [DOI] [PubMed] [Google Scholar]
- 34.Amzel A, Toska E, Lovich R, et al. Promoting a combination approach to paediatric HIV psychosocial support. AIDS. 2013;27:S147–S157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Boon-Yasidhi V, Chokephaibulkit K, McConnell MS, et al. Development of a diagnosis disclosure model for perinatally HIV-infected children in Thailand. AIDS Care. 2013;25:756–762. [DOI] [PubMed] [Google Scholar]
- 36.Cantrell K, Patel N, Mandrell B, et al. Pediatric HIV disclosure: a process-oriented framework. AIDS Educ Prev. 2013;25:302–314. [DOI] [PubMed] [Google Scholar]
- 37.Rowe AK, de Savigny D, Lanata CF, et al. How can we achieve and maintain high-quality performance of health workers in low-resource settings? Lancet. 2005;366:1026–1035. [DOI] [PubMed] [Google Scholar]
- 38.Sandelowski M. Focus on qualitative methods: sample size in qualitative research. Res Nurs Health. 1995;18:179–183. [DOI] [PubMed] [Google Scholar]
- 39.Strauss A, Corbin J. Basics of Qualitative Research. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- 40.Pope C, Ziebland S, Mays N. Qualitative research in health care: analysing qualitative data. Br Med J. 2000;320:114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Miles M, Huberman A. Qualitative Data Analysis: An Expanded Sourcebook. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- 42.Sandelowski M, Leeman J. Writing usable qualitative health research findings. Qual Health Res. 2012;22:1404–1413. [DOI] [PubMed] [Google Scholar]
- 43.National Guidelines for Antiretroviral Therapy. Windhoek, Namibia: Ministry of Health and Social Services, Directorate of Special Programmes; 2010. [Google Scholar]
- 44.Wachira J, Middlestadt SE, Vreeman R, et al. Factors underlying taking a child to HIV care: implications for reducing loss to follow-up among HIV-infected and -exposed children. SAHARA J. 2012;9:20–29. [DOI] [PubMed] [Google Scholar]
- 45.Ozer E, Adams S, Rieder Gardner L, et al. Provider self-efficacy and the screening of adolescents for risky health behaviors. J Adolesc Health. 2004;35:101–107. [DOI] [PubMed] [Google Scholar]
- 46.Snow RC, Asabir K, Mutumba M, et al. Key factors leading to reduced recruitment and retention of health professionals in remote areas of Ghana: a qualitative study and proposed policy solutions. Hum Resour Health. 2011;9:13. [DOI] [PMC free article] [PubMed] [Google Scholar]


