Abstract
Objectives
Little is known about the moderators and mediators of change in online pain interventions based on cognitive behavioral therapy (CBT). We hypothesized that the effects of painACTION.com, an online pain self- management program, on pain-related outcomes would be mediated by changes in depression, anxiety, and stress, as well as the use of coping strategies. We also examined potential moderators of change.
Methods
First, the efficacy of painACTION.com and moderators of the intervention effects were evaluated using a pooled sample from previous back, neuropathic, and arthritis pain studies. Next, we explored whether the intervention effect on the primary outcomes - pain severity and patient global impression of change (PGIC) was mediated by coping strategies or emotional functioning.
Results
Compared to controls, experimental participants evidenced significant improvement in pain, emotional functioning, and coping strategies from baseline to follow-up. There were no clear moderators of intervention effects. Changes in emotional factors, particularly stress levels, mediated the relationship between the intervention and outcome (pain severity) over time.
Discussion
This study supports the effectiveness of online interventions when CBT and self-management targets pain levels, emotional factors and wellness-focused coping. The importance of stress as a mediator of pain severity is discussed. The absence of moderators may indicate that the intervention is effective for a wide variety of patients with chronic pain.
Keywords: cognitive behavior therapy, Internet, self-management, moderator, mediator
Introduction
Psychological factors, including stress1, depression,2 pain-related fear,3 pain coping strategies,4 catastrophizing,5 and self-efficacy,2 are associated with the experience of pain and may be related to chronic pain conditions.6 Numerous studies show Cognitive Behavioral Therapy (CBT) is effective in increasing patient functioning and coping.7–9 For chronic low back pain, a meta-analysis showed CBT and self-regulatory interventions were particularly helpful in reducing pain intensity, pain-related interference, and depression, as well as improving health-related quality of life.10
Recently, several studies have provided support for online self-management programs for pain and other health conditions.11–13 These programs typically focus on the development of coping skills, emotional management, interpersonal functioning, and improving communications with peers, family members, and medical professionals.14 Studies indicate that online self-management programs for pain are effective in reducing pain severity, pain-related interference and emotional burden, perceived disability, catastrophizing, pain-induced fear, depression, anxiety and stress.15–18 A systemic review of eleven web-based CBT interventions for chronic pain showed small pain reductions compared to wait-list controls, but better attitudes toward pain, an increase in social and work activities and better clinical outcomes related to depression and anxiety. 19
An understanding of the process of therapeutic change is facilitated by analytical tests, mediation and moderation.20, 21 For example, Turner et al.8 investigated the mediators and moderators of a face-to-face CBT intervention for temperomandibular pain and found that pre- to post-treatment changes in pain-related beliefs mediated the effects of CBT on pain and disability one year following the intervention. Holroyd et al. 22 found that self-efficacy moderated treatment outcomes with chronic tension-type headache. Although online CBT interventions are promising, little is known about what type of patient benefits most.23
Over the past few years, we conducted separate RCTs of three online modules of painACTION.com, a CBT-oriented, self-management website for patients with chronic pain: back pain [BP],24 neuropathic pain [NP],25 and arthritis pain [AP].26 All three studies found positive outcomes for the experimental group participants compared with controls, but the significant outcomes varied by pain patient population. Specifically, improvements were found in worst pain (BP, NP), pain severity (NP), pain interference (NP), percent overall work impairment (NP), self-efficacy (NP, AP), stress (BP), global impression of change (BP, NP, AP), pain catastrophizing (AP), and depression (NP). In addition, there were significant findings for coping strategies, including coping self-statements (BP, AP), relaxation (AP), social support (BP), and resting and guarding (NP).
To date, there have been no studies examining mediators or moderators of pain outcomes using online interventions based on CBT or self-management. In particular, little is known about: (1) therapeutic mechanisms that lead to improvement (mediator effects), and (2) the relationship between patient characteristics and treatment response (moderator effects). As with Turner et al.,8 we expected important mediational effects, but with different mediators. We hypothesized that the effects of painACTION.com on pain-related outcomes would be mediated by changes in: (1) levels of depression, anxiety, and stress, and (2) the use of coping strategies. The moderation analysis was exploratory, so no hypotheses were formed. To conduct these analyses, we first assessed the efficacy of the intervention for the combined sample and then examined the moderators and mediators of treatment effects.
Methods
The current study includes a combined sample of participants from three randomized control trials (RCTs) performed to test the efficacy of painACTION.com, an online self-management intervention program for patients with chronic pain. This secondary data analysis was performed in two stages: First, the efficacy of the painACTION.com intervention program and moderators of the intervention effects (Study 1) were evaluated using the pooled sample of all participants (N=668). Next, we explored the mediators of intervention outcomes (Study 2) by evaluating whether the intervention effects on the primary outcomes, pain severity and global impression of change, were mediated by coping strategies or emotional functioning.
Study 1 -- Efficacy of painACTION.com Intervention Program
Participants and Procedures
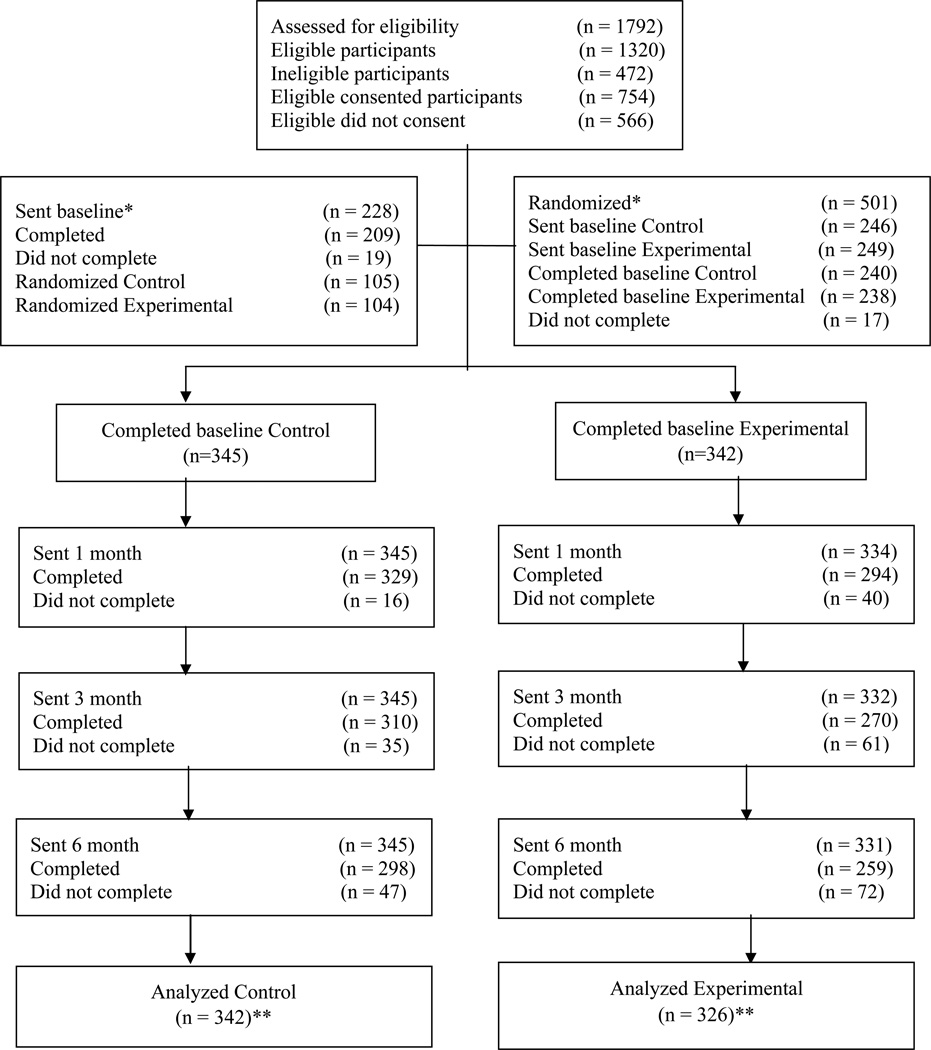
The inclusion criteria across studies were: (1) age 18 years or older; (2) self-reported physician diagnosis of chronic pain due to the type of pain per study: back pain, neuropathic pain or arthritis pain; (3) English-speaking; and (4) reliable access to the Internet and e-mail. Participants who had a history of psychiatric hospitalization in the past year or were registered in a previous painACTION.com randomized controlled trial were excluded from the study. The samples for these studies were mostly recruited online. The back pain study also recruited participants from a pain clinic using flyer postings and referrals. The arthritis pain study also recruited participants via flyers at community locations (e.g., senior citizen centers). All participants signed informed consent forms. Participants were allocated to either the experimental condition (painACTION.com) or a control condition by stratified randomization to ensure group equivalence on preselected variables (e.g., gender, race and age in the back pain study). The participant flow through the studies can be found in the CONSORT chart (Figure 1).
Figure 1.
Consolidated Standards of Reporting Trials flow diagram
* Participants in the back pain study were given baseline and then randomized. Participants in the arthritis and neuropathic pain studies were randomized and then given the baseline assessment. In the neuropathic pain study 25 eligible consented participants did not complete the background assessment and therefore were not randomized.
** For analysis, ten participants (1 control, 9 experimental) in the back pain study were removed from the study for various reasons (illness, illiterate, in multiple studies, no data, used for usability and used multiple names). Further, due to technical reasons data from 9 participants in the back pain study were missing, hence excluded from analysis (2 control, 7 experimental).
Experimental and Control Conditions
painACTION.com is based on the principles of CBT and teaches pain self-management by reducing counterproductive beliefs and self-statements; enhancing management of depression, anxiety, and stress; increasing social support for pain management; and collaborating with pain treatment providers. painACTION.com includes: (1) self-assessments with tailored, real-time feedback; (2) an online pain tracker; (3) interactive skill-based lessons; and (3) media-rich content (videos, interactive tools). Participants randomized to the intervention condition were directed to use the program at least twice a week for four weeks then at least one a month for five months for a total of six months. The median time spent on the website was 215 minutes (interquartile range: 57–387 minutes).
Control participants were not given an interactive, online intervention. In the back and neuropathic pain studies, participants were mailed or emailed a pain-specific guide that was representative of typical print materials given to patients with their conditions. In the arthritis study, control participants were put on a waitlist and given the online intervention after the study was completed. All participants in the study were told to maintain their regular treatment regimens, and were free to change or try new treatments as they saw fit. These treatments were not controlled for as treatment regimens for pain are participant specific and based on need and level of adherence.
Measures
The three pain studies included various measures to assess for outcomes of interest. Measures created for specific types of pain were used in the original studies to allow for the most accurate measure of outcome variables. For this analysis, we included only the variables that were consistently measured in all three studies.
Brief Pain Inventory – Short Form (BPI-SF).27
This self-report measure uses a 0 to 10 numeric rating scale to obtain information on two subscales; the intensity of pain and the degree to which pain interferes with daily function. The Pain Severity Score uses four items (worst, least, average and current pain) to measure the average level of pain intensity for the patient. The Pain Interference Score uses seven items to measure how much pain interferes with daily life, such as general activities, mood, walking, work, relationships, sleep and enjoyment of life. The BPI’s reliability and validity were first established in patients with cancer pain, but have now been demonstrated in multiple types of chronic non-cancer pain.28–30
Patient Global Impression of Change Scale (PGIC). 31
This scale is a measure of participant’s perception of improvement due to an intervention. The measure contains a single, self-rated item on a 7-point scale, from “very much improved” to “very much worse”. The PGIC has been widely used in chronic pain research32 and improvement on this scale has been linked to reduced chronic pain intensity.
Depression Anxiety Stress Scales (DASS-21).33
The DASS is a 21-item questionnaire which measures negative emotional states, and is comprised of three subscales: depression, anxiety and stress. The DASS has continually been shown to have high reliability and validity across multiple studies.34–37 This measure has been shown to produce meaningful discriminations in a variety of settings, and demonstrates changes in states over time during treatment.
Chronic Pain Coping Inventory (CPCI-42).38
The CPCI is an empirically validated scale designed to rate the use of behavioral and cognitive coping strategies. This measurement consists of subscales representing eight types of strategies which are typically targeted for change in multidisciplinary pain treatment programs: guarding, resting, asking for assistance, relaxation, task persistence, exercise/stretching, seeking social support, and coping self-statements. This 42-item self-report instrument asks the individual to indicate the frequency with which they use coping strategies to mitigate their pain. The CPCI-42 shows strong reliability and validity demonstrated by high correlations between the original and abbreviated CPCI scales (Cronbach α all.70 or above), high internal consistency, and test-retest reliability.
Statistical Analysis
Descriptive statistics were computed for demographic variables from the pooled sample as well as stratified by the study (back pain, neuropathic pain, and arthritis pain). Pooled analyses of the mean differences between conditions (experimental vs. control) over time on the study outcomes were performed using a generalized linear mixed model approach. Mixed models were used because of the ability to incorporate clustering of individuals within studies as well as covariance among repeated measures. Moreover, this approach automatically handles missing data by maximum likelihood.39 Each model included the fixed effects condition (experimental vs. control), time (baseline, one month follow-up, three month follow-up and six month follow-up), and condition-by-time. The models treated time as a repeated measures variable to allow for covariation across time points and study as a random intercept to account for within-study clustering. Statistical focus of these analyses was the interaction effect, condition-by-time, as this effect tests differences between conditions over time. Global impression of change was compared at each follow-up assessment between the experimental and control condition using t-tests.
Moderators of the intervention effects
Moderation analyses tested whether the association between the intervention and the outcome was differential across levels of certain key covariates including gender, age (≤50 years vs. >50 years), race (white vs. non-white), baseline pain intensity (average baseline pain ≤6 vs. >6), and pain condition (back pain vs. neuropathic pain vs. arthritis pain). These exploratory models were conducted using generalized linear mixed model procedures (described in the section above), with the exception of adding the variable of interest (e.g., gender) and higher order interaction effects (e.g. gender*time, gender*condition, gender*condition*time). Statistical focus of these analyses were the higher order interaction effects (gender*condition*time).
If the higher order interaction effect was statistically significant, post-hoc tests were performed with multiplicity adjustments using the simulation technique in LSMESTIMATE statement in SAS 9.340; p-values reported for post-hoc comparisons were corrected for Type I error. The level of significance for hypothesis testing was set at α = 0.05 for each analysis. Data analyses were performed in SAS 9.3. The GLIMMIX procedure was used wherever generalized linear mixed model approach was applied.41
Results
Participant characteristics
The total study sample comprised of 668 eligible participants from the three RCTs: back pain (n = 190), neuropathic pain (n = 250), and arthritis pain (n = 228). The majority of the study sample was female (72.6%), and white (88.8%), with a mean age of 48.7 years (SD = 11.7). Approximately half of the participants were college graduates (50.9%) and half were married (55.5%). At baseline, the mean self-reported level of current pain of the study sample was 5.3 (SD = 2.2).
There were 326 participants in the experimental group and 342 in the control group. There was no significant difference in age, gender, race, education level, marital status, income or pain at baseline between these two groups. Participants in the back pain study were younger (M = 45.6 years; SD = 11.8) than the participants in the arthritis pain (M = 49.9 years; SD = 11.6) and neuropathic pain studies (M = 50.2 years; SD = 11.4); while the percentages of females were greater in the neuropathic pain study (80.0%) in comparison to arthritis (68.4%) and back pain (67.9%) studies. Of the 668 participants, 492 (experimental, n = 231; control, n = 261) completed all the study assessments. A combination of loss to follow-up and partial assessments resulted in a 26.5% attrition rate (n = 176). A comparison of these groups on demographic variables and baseline study measures revealed only one significant difference: frequency of use of social support as a coping strategy (Completers: M = 2.9; SD =1.9; vs. Noncompleters: M = 2.6; SD = 1.8).
Efficacy of painACTION.com Intervention Program
Participants in the painACTION.com experimental condition, as compared to the control group, evidenced a significantly greater mean change over time on reported pain severity, emotional functioning (depression, stress, anxiety), use of chronic pain coping strategies, and global impression of change. In comparison to the control group, the experimental group evidenced significantly greater improvement over time which was more pronounced at the six-month follow-up.
Pain Severity
Change over time was noted for pain severity as measured by the BPI but not for pain interference. Specifically, significant overall effect of condition-by-time was noted for pain severity (F-test = 4.04, p = 0.007) and its subscales: current pain (F-test = 3.67, p = 0.0117) and average pain (F-test = 2.84, p = 0.0367). Post hoc comparisons revealed that the participants in the experimental condition reported a greater decrease in (1) pain severity score from baseline to six-month follow-up (t = −3.14, p = 0.0049); (2) current pain from baseline to one-month follow-up (t = −3.09, p = 0.0058) and six-month follow-up (t = −2.60, p = 0.0259); and (3) average pain from baseline to six-month follow-up (t = −2.78, p = 0.0157), as compared to the control participants.
Emotional Functioning
Significant overall effect of condition-by-time was noted for all three subscales of the DASS (Depression: F-test = 6.32, p = 0.0003; Anxiety: F-test = 2.75, p = 0.0416; Stress: F-test = 6.32, p = 0.0003). The experimental group showed significant reduction in (1) depression from baseline to three-month follow-up (t = −2.58, p = 0.0262) and six-month follow-up (t = −4.30, p < 0.0001); (2) anxiety from baseline to three-month follow-up (t = −2.27, p = 0.0489) and six-month follow-up (t = −2.80, p = 0.0141); and (3) stress from baseline to one-month follow-up (t = −2.50, p = 0.0328), three-month follow-up (t = −3.56, p = 0.0010) and six-month follow-up (t = −4.10, p < 0.0001).
Coping Strategies
Experimental participants reported a significantly greater frequency of using three coping strategies [coping self-statements (F-test = 4.72, p = 0.0028), relaxation (F-test = 6.93, p = 0.0001) and social support (F-test = 3.63, p = 0.0125)]. Post hoc comparisons revealed that the experimental group showed a significant increase in using (1) coping self-statements from baseline to one-month follow-up (t = 2.46, p = 0.0366), three-month follow-up (t = 3.70, p = 0.0006) and six-month follow-up (t = 2.57, p = 0.0274); (2) relaxation from baseline to three-month follow-up (t = 4.29, p < 0.0001) and six-month follow-up (t = 3.62, p = 0.0008); and (3) social support from baseline to three-month follow-up (t = 3.16, p = 0.0048) and six-month follow-up (t = 2.37, p = 0.0475).
Global Impression of Change
As expected, the experimental group reported a significantly greater global impression of change as compared to the control group at one-month follow-up (t = 5.08, p < 0.0001), three-month follow-up (t = 4.05, p < 0.0001) and six-month follow-up (t = 5.70, p < 0.0001) (see Table 2).
Table 2.
Least square means and standard errors for all outcome measures
| Control (N=342) | Experimental (N=326) | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Post | 3-month | 6-month | Baseline | Post | 3-month | 6-month | |
| BPI | ||||||||
| Worst | 6.89 (0.11) | 6.70 (0.12) | 6.40 (0.14) | 6.47 (0.14) | 6.86 (0.11) | 6.37 (0.12) | 6.20 (0.14) | 6.08 (0.14) |
| Least | 3.75 (0.12) | 3.63 (0.12) | 3.51 (0.13) | 3.67 (0.13) | 3.63 (0.12) | 3.49 (0.13) | 3.40 (0.14) | 3.19 (0.13) |
| Current | 5.48 (0.12) | 5.31 (0.12) Δa | 5.07 (0.13) | 5.03 (0.13) Δc | 5.46 (0.12) | 4.95 (0.13) Δa | 4.82 (0.13) | 4.64 (0.14) Δc |
| Average | 5.39 (0.12) | 5.09 (0.12) | 4.86 (0.14) | 5.04 (0.14) Δc | 5.24 (0.12) | 4.73 (0.13) | 4.61 (0.15) | 4.41 (0.14) Δc |
| Pain Severity | 5.38 (0.09) | 5.18 (0.10) | 4.96 (0.11) | 5.06 (0.11) Δc | 5.29 (0.10) | 4.89 (0.10) | 4.76 (0.12) | 4.58 (0.12) Δc |
| Interference | 5.71 (0.13) | 5.17 (0.14) | 4.94 (0.15) | 4.83 (0.15) | 5.48 (0.13) | 4.69 (0.14) | 4.59 (0.15) | 4.49 (0.15) |
| DASS | ||||||||
| Anxiety | 8.81 (0.43) | 8.55 (0.46) | 7.98 (0.41) Δb | 8.46 (0.45) Δc | 9.46 (0.44) | 8.31 (0.48) | 7.42 (0.43) Δb | 7.54 (0.47) Δc |
| Depression | 11.79 (0.64) | 11.13 (0.64) | 10.80 (0.65) Δb | 11.30 (0.65) Δc | 12.85 (0.65) | 11.10 (0.66) | 10.20 (0.67) Δb | 9.39 (0.67) Δc |
| Stress | 14.43 (0.47) | 14.26 (0.49) Δa | 13.74 (0.50) Δb | 14.38 (0.52) Δc | 15.02 (0.48) | 13.46 (0.51) Δa | 12.17 (0.52) Δb | 12.31 (0.54) Δc |
| CPCI | ||||||||
| Assistance | 2.82 (0.14) | 2.85 (0.13) | 2.80 (0.14) | 2.92 (0.14) | 2.96 (0.14) | 2.94 (0.14) | 3.02 (0.14) | 3.11 (0.15) |
| Coping | 4.00 (0.11) | 4.10 (0.11) Δa | 3.98 (0.11) Δb | 4.06 (0.12) Δc | 3.92 (0.11) | 4.33 (0.11) Δa | 4.41 (0.12) Δb | 4.36 (0.12) Δc |
| Exercise | 2.62 (0.35) | 2.93 (0.35) | 2.94 (0.35) | 2.99 (0.36) | 2.49 (0.35) | 2.94 (0.36) | 3.04 (0.36) | 3.11 (0.36) |
| Persistence | 3.80 (0.11) | 3.95 (0.11) | 3.93 (0.11) | 4.03 (0.12) | 3.85 (0.11) | 4.01 (0.12) | 4.13 (0.12) | 4.11 (0.12) |
| Resting | 3.87 (0.11) | 3.86 (0.11) | 3.70 (0.12) | 3.75 (0.12) | 4.02 (0.11) | 3.84 (0.11) | 3.97 (0.12) | 3.99 (0.12) |
| Relaxation | 2.37 (0.10) | 2.65 (0.10) | 2.54 (0.10) Δb | 2.59 (0.11) Δc | 2.31 (0.10) | 2.82 (0.11) | 2.99 (0.11) Δb | 2.98 (0.11) Δc |
| Social | 2.83 (0.11) | 2.97 (0.11) | 2.74 (0.11) Δb | 2.91 (0.12) Δc | 2.83 (0.11) | 3.25 (0.11) | 3.18 (0.12) Δb | 3.27 (0.12) Δc |
| Guarding | 3.57 (0.10) | 3.38 (0.09) | 3.41 (0.10) | 3.41 (0.11) | 3.67 (0.10) | 3.36 (0.10) | 3.36 (0.11) | 3.35 (0.11) |
| PGIC | 3.57 (0.98) a | 3.37 (1.06)b | 3.33 (1.15)c | 3.19 (0.89)a | 3.01 (1.07)b | 2.79 (1.00)c | ||
BPI = Brief Pain Inventory; CPCI = Chronic Pain Coping Inventory; DASS = Depression Anxiety Stress Scale; PGIC = Patients Global Impression of Change.
Pairwise post hoc contrasts between experimental and control groups at each time point for PGIC and for the mean change in differences for all other outcomes.
Unique superscripts indicate significant pairwise post hoc tests (p < 0.05);
change for condition-BY-time compared to baseline.
Moderators of Intervention Effects
Gender and race moderated the relationship between the intervention and outcomes although no clear patterns emerged. Pain condition, baseline pain intensity and age did not moderate the intervention effects on outcomes. Post-hoc comparisons revealed a significant reduction in current pain among males at three-month (t = −3.16, p = 0.0096) but no such change was noted among females. White participants evidenced reduction in worst pain at six-month follow-up (t = −2.95, p = 0.0191) but no such change was seen in nonwhites.
Study 2: Mediation of Intervention Effects
Statistical Analyses
Various methodologies have been applied to examine mediation in longitudinal repeated measures studies including recent advancement in: (1) generalized estimating equations42 and (2) structural equation model43, 44 procedures. We based our approach on the methods described by MacKinnon44 and Cappelleri et. al.43 but we applied generalized linear mixed models which also accounts for within-subject covariance longitudinally. We tested the hypothesis that changes in specific process variables would mediate the effects of intervention on each outcome over time. The putative mediators were coping (CPCI) and emotional functioning (DASS) and the outcomes were pain severity and PGIC. Mediation models were constructed using the following steps.
First, the intervention effect on each outcome over time (total effect) was examined by modeling condition, time and condition-by-time as the independent variables. Second, the intervention effect on each mediating variable over time was examined by modeling condition, time, and condition-by-time as the independent variables. Finally, the full mediation model was constructed which included condition, mediator, time, condition-by-time and mediator-by-time as the independent variables. If the F-tests for condition-by-time in the first two models were significant, mediation was examined by the interaction effect, mediator-by-time (indirect effect) in the third model, as this tests the effect of the putative mediator on the outcome over time beyond the direct intervention effects over time. To infer mediation, the above three F-tests must be significant. Partial mediation is present if the F-test for condition-by-time in the full mediation model is significant (i.e., the direct effect of intervention over time is significant). There is full mediation if the F-test for condition-by-time in the full mediation model is non-significant (i.e., the direct effect of intervention over time is non-significant). All models treated time as a repeated measures variable to allow for covariation within-subjects across time points and used study as a random intercept to account for within-study clustering. It should be noted that mediation models for outcome PGIC excludes baseline assessment as this outcome was not measured at baseline. The level of significance for hypothesis testing was set at α = 0.05 for each analysis. Data analyses were performed in SAS 9.3 using the GLIMMIX procedure.
Results
Mediation Effects
The total intervention effects on outcomes pain severity and global impression of change were significant, i.e., participants in the experimental group showed significantly greater change on pain severity (F-test = 4.04, p = 0.007) and global impression of change (F-test = 4.39, p = 0.0125) over time as compared to the control group. Results from the full mediation model with the overall F-test and β coefficients of the direct effect of painACTION.com intervention on each outcome and the indirect effects through each mediator variables are presented in Tables 3 and 4.
Table 3.
Mediators of painACTION.com intervention effects on outcome pain severity (BPI) over time
| Full mediation model (condition, mediator, time and interaction effects) † | Intervention over time model (condition, time and interaction effects; without the mediator) ‡ |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mediating (indirect) effects over time | Intervention (direct) effects over time with mediator in the model |
Intervention (total) effects over time without mediator in the model |
||||||||||
| Putative Mediator | β coefficient |
p value | F-test | p value | β coefficient |
p value | F-test | p value | β coefficient |
p value | F-test | p value |
| DASS | ||||||||||||
| Depression | 2.40 | 0.0659 | 2.04 | 0.1067 | 4.04 | 0.0070 | ||||||
| Baseline | reference | reference | reference | |||||||||
| Post | 0.0050 | 0.3384 | 0.1610 | 0.1051 | 0.2043 | 0.0402 | ||||||
| 3-month | 0.0121 | 0.0437 | 0.0421 | 0.719 | 0.1209 | 0.3147 | ||||||
| 6-month | 0.0159 | 0.0145 | 0.2495 | 0.0421 | 0.4102 | 0.0013 | ||||||
| Anxiety | 1.66 | 0.1730 | 2.78 | 0.0395 | 4.04 | 0.0070 | ||||||
| Baseline | reference | reference | reference | |||||||||
| Post | 0.0099 | 0.1264 | 0.1645 | 0.0979 | 0.2043 | 0.0402 | ||||||
| 3-month | 0.0140 | 0.0787 | 0.0614 | 0.6038 | 0.1209 | 0.3147 | ||||||
| 6-month | 0.0159 | 0.0533 | 0.3232 | 0.0098 | 0.4102 | 0.0013 | ||||||
| Stress € | 3.73 | 0.0108 | 2.17 | 0.0900 | 4.04 | 0.0070 | ||||||
| Baseline | reference | reference | reference | |||||||||
| Post | 0.0075 | 0.2099 | 0.1468 | 0.1399 | 0.2043 | 0.0402 | ||||||
| 3-month | 0.0152 | 0.0253 | 0.0120 | 0.9185 | 0.1209 | 0.3147 | ||||||
| 6-month | 0.0228 | 0.0013 | 0.2524 | 0.0393 | 0.4102 | 0.0013 | ||||||
| CPCI | ||||||||||||
| Coping | 1.01 | 0.3884 | 4.35 | 0.0046 | 4.04 | 0.0070 | ||||||
| Baseline | reference | reference | reference | |||||||||
| Post | 0.0003 | 0.9919 | 0.2100 | 0.0359 | 0.2043 | 0.0402 | ||||||
| 3-month | 0.0225 | 0.4683 | 0.1419 | 0.2407 | 0.1209 | 0.3147 | ||||||
| 6-month | 0.0509 | 0.1170 | 0.4330 | 0.0007 | 0.4102 | 0.0013 | ||||||
| Relaxation | 0.93 | 0.4275 | 4.62 | 0.0032 | 4.04 | 0.0070 | ||||||
| Baseline | reference | reference | reference | |||||||||
| Post | −0.0379 | 0.1864 | 0.2180 | 0.0292 | 0.2043 | 0.0402 | ||||||
| 3-month | −0.0103 | 0.7549 | 0.1648 | 0.177 | 0.1209 | 0.3147 | ||||||
| 6-month | 0.0116 | 0.7366 | 0.4552 | 0.0004 | 0.4102 | 0.0013 | ||||||
| Social | 0.91 | 0.4374 | 4.48 | 0.0038 | 4.04 | 0.0070 | ||||||
| Baseline | reference | reference | reference | |||||||||
| Post | −0.0231 | 0.3935 | 0.2218 | 0.0272 | 0.2043 | 0.0402 | ||||||
| 3-month | 0.0225 | 0.4669 | 0.1722 | 0.155 | 0.1209 | 0.3147 | ||||||
| 6-month | −0.0129 | 0.6913 | 0.4424 | 0.0005 | 0.4102 | 0.0013 | ||||||
BPI = Brief Pain Inventory; CPCI = Chronic Pain Coping Inventory; DASS = Depression Anxiety Stress Scale.
Full mediation model includes the condition, mediator, time, condition*time and mediator*time as the independent variables.
Model includes only the condition over time effects i.e., condition, time and condition*time as the independent variables.
Statistically significant at p < 0.05.
To infer mediation, the following type III tests of effects (F-test) must be statistically significant: (1) Intervention (total) effect over time on outcome pain severity; (2) Intervention effect over time on mediator (not shown in table); (3) Mediating (indirect) effect over time on outcome pain severity in the mediation model. For example, in this table stress mediates the intervention effects on pain severity as the following tests are significant: (1) Intervention (total) effect over time on outcome pain severity (F-test = 4.04, p = 0.0070); (2) Intervention effect over time on stress (F-test = 6.32, p = 0.0003; not shown in table); (3) Mediating (indirect) effect over time on outcome pain severity in the mediation model (F-test = 3.73, p = 0.0108).
Table 4.
Mediators of painACTION.com intervention effects on outcome PGIC over time (excluding baseline) £
| Full mediation model (condition, mediator, time and interaction effects) † | Intervention over time model (condition, time and interaction effects; without the mediator) ‡ |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mediating (indirect) effects over time | Intervention (direct) effects over time with mediator in the model | Intervention (total) effects over time without mediator in the model |
||||||||||
| Putative Mediator |
β coefficient |
p value | F-test | p value | β coefficient |
p value | F-test | p value | β coefficient |
p value | F-test | p value |
| DASS | ||||||||||||
| Depression | 1.62 | 0.1974 | 2.73 | 0.0654 | 4.39 | 0.0125 | ||||||
| Post | reference | reference | reference | |||||||||
| 3-month | 0.0025 | 0.5728 | −0.0438 | 0.6011 | −0.0306 | 0.7178 | ||||||
| 6-month | 0.0088 | 0.0770 | 0.1584 | 0.0912 | 0.2202 | 0.0203 | ||||||
| Anxiety ¥ | 4.23 | 0.0147 | 3.73 | 0.0241 | 4.39 | 0.0125 | ||||||
| Post | reference | reference | reference | |||||||||
| 3-month | 0.0138 | 0.0144 | −0.0419 | 0.6155 | −0.0306 | 0.7178 | ||||||
| 6-month | 0.0154 | 0.0117 | 0.1927 | 0.0391 | 0.2202 | 0.0203 | ||||||
| Stress | 2.99 | 0.0508 | 3.04 | 0.0482 | 4.39 | 0.0125 | ||||||
| Post | reference | reference | reference | |||||||||
| 3-month | 0.0008 | 0.8643 | −0.0447 | 0.5962 | −0.0306 | 0.7178 | ||||||
| 6-month | 0.0117 | 0.0287 | 0.1682 | 0.0737 | 0.2202 | 0.0203 | ||||||
| CPCI | ||||||||||||
| Coping | 0.36 | 0.6983 | 4.46 | 0.0118 | 4.39 | 0.0125 | ||||||
| Post | reference | reference | reference | |||||||||
| 3-month | −0.0185 | 0.4039 | −0.0416 | 0.6262 | −0.0306 | 0.7178 | ||||||
| 6-month | −0.0133 | 0.5841 | 0.2156 | 0.0239 | 0.2202 | 0.0203 | ||||||
| Relaxation | 0.18 | 0.8385 | 4.17 | 0.0156 | 4.39 | 0.0125 | ||||||
| Post | reference | reference | reference | |||||||||
| 3-month | −0.0062 | 0.7917 | −0.0491 | 0.5654 | −0.0306 | 0.7178 | ||||||
| 6-month | −0.0151 | 0.5543 | 0.2024 | 0.0337 | 0.2202 | 0.0203 | ||||||
| Social | 0.60 | 0.5484 | 4.62 | 0.0100 | 4.39 | 0.0125 | ||||||
| Post | reference | reference | reference | |||||||||
| 3-month | 0.0068 | 0.7577 | −0.0315 | 0.7119 | −0.0306 | 0.7178 | ||||||
| 6-month | 0.0258 | 0.2895 | 0.2263 | 0.0174 | 0.2202 | 0.0203 | ||||||
PGIC = Patient Global Impression of Change; CPCI = Chronic Pain Coping Inventory; DASS = Depression Anxiety Stress Scale.
Baseline data excluded from analysis as PGIC was not measured.
Full mediation model includes the condition, mediator, time, condition*time and mediator*time as the independent variables.
Reduced model includes only the condition over time effects i.e., condition, time and condition*time as the independent variables.
To infer mediation, the following type III tests of effects (F-test) must be statistically significant: (1) Intervention (total) effect over time on outcome PGIC; (2) Intervention effect over time on mediator (not shown in table); (3) Mediating (indirect) effect over time on outcome PGIC in the mediation model.
Anxiety did NOT mediate the intervention effects on PGIC as the second criteria was not met.
Pain Severity
Table 3 shows that stress fully mediated the intervention effect on pain severity over time as all three tests of mediation were significant: (1) intervention (total) effect over time on outcome pain severity (F-test = 4.04, p = 0.0070); (2) intervention effect over time on stress (F-test = 6.32, p = 0.0003; not shown in table); (3) mediating (indirect) effect over time on outcome pain severity in the mediation model (F-test = 3.73, p = 0.0108). It is worth noting that although not statistically significant, the indirect effect of depression over time (indirect effect: F-test = 2.40, p = 0.0659) in the full mediation model attributed to a reduction in the condition-by-time effect (direct effect: F-test = 2.04, p = 0.1067). Anxiety and the coping strategies (i.e., coping self-statements, relaxation and social support) did not mediate the relationship between the intervention and pain severity over time.
Global Impression of Change
Depression, anxiety, stress and coping strategies (i.e., coping self-statements, relaxation and social support) did not mediate the relationship between intervention and PGIC over time. The indirect effect of stress on PGIC over time in the full mediation model was close to statistical significance α = 0.05 (F-test = 2.99, p = 0.0508). Of note, although the indirect effect of anxiety on PGIC is statistically significant, anxiety did not mediate the intervention effects on PGIC as the second mediation criteria (intervention effect over time on anxiety; F-test = 0.54, p = 0.5835) was not met. Although it is debatable whether this criterion is an absolute requisite to determine mediation, we chose to be conservative in our tests of inference.
Discussion
We are unaware of other studies that have examined mediators and moderators of online CBT- and self-management-based interventions. Through the examination of important mediators such as emotional factors (anxiety, depression, stress) and coping behaviors, this study extends the work of Turner et al.,8 who found that cognitive factors such as pain beliefs (control over pain, disability, and pain signals harm), catastrophizing, and pain management self-efficacy mediated the effects of CBT. As hypothesized, an emotional factor (i.e., stress) mediated pain severity. As in Turner et al., 8 this study did not reveal any notable results with regard to moderators.
First, we conducted pooled analyses of all three study samples to test our hypotheses that, in comparison to the control group, the use of painACTION.com leads to significant reductions in pain, increased use of adaptive coping strategies, and enhanced emotional functioning over time. These hypotheses were supported. The finding that the impact of painACTION.com appears to increase more at longer follow-up duration was unexpected. There were more significant changes in outcomes for pain, emotional functioning, and coping skill usage at longer follow-ups. There were significant differences in current pain between experimental and control participants at one-month follow-up. The impact was even greater at the six-month follow-up, with significant differences between experimental and control groups in least pain, current pain, average pain, and pain severity scores. This pattern was repeated with emotional functioning, as there were significant between-group differences in stress at the one-month follow-up but that all three DASS subscales (depression, anxiety, and stress) improved significantly at three-month and six-month follow-ups. Experimental participants reported a significantly greater frequency of using coping strategies (coping self-statements, relaxation and social support) at three-month and six-month follow-up in comparison to the controls. Experimental participants cited significantly higher ratings of perceived global impression of change than controls at six-month follow-up. It is interesting to note that the median time spent on the website was 215 minutes so these results were obtained with a minimal time compared to face-to-face CBT interventions that typically require 12 weeks. We do not know what differences might have been found if similar content was delivered in a face-to-face manner.
The reasons for the pattern of these results, showing early initial differences between the groups in ratings of current pain and stress, with greater improvement over time for the experimental group in other measures, is unclear. It may be that exposure to the intervention increased hope and perceived control over pain, which had an early effect on ratings of current pain and stress. Although we did not measure daily use of skills, the larger effects over time may have resulted from increased use of newly acquired skills. These results are different from those of an online wellness program that found a decrease in pain intensity over six months, but found no decrease in ratings of stress over the same period.45 Future qualitative studies might assist in a greater understanding of participants’ attributions of increased effect of the intervention over time.
The moderation analyses conducted in Study 1 revealed no clear patterns except for some indications of greater pain reductions in male and white participants. The lack of moderation findings is consistent with previous pain studies.7, 8, 46 These findings may be interpreted in positive terms, suggesting that painACTION.com may be helpful to pain sufferers regardless of personal characteristics. In addition, the type of pain experienced by participants was not found to be a moderator of intervention effects. This result is not surprising as CBT and self-management has been shown to be effective with a variety of medical illnesses and types of pain.47 Alternatively, the lack of findings from the moderation analyses could be because of inadequate sample size for the three way interaction conducted and the composition of the sample (e.g., predominantly white women).
The pattern of results from the mediation analyses partially supported our hypotheses that emotional factors may exert an important effect. In this analysis, stress mediated the relationship between painACTION.com intervention and pain severity. The link between pain and stress has long been supported in the literature,48,49 to the extent that cognitive-behavioral stress-management has been used as a treatment for chronic tension-type headaches.22 Although not statistically significant, a similar trend was noted for depression. Global impression of change was not mediated by any emotional functioning or coping, although stress showed a nonsignificant trend. This finding was unexpected. As discussed earlier, the change in global impression of change in the experimental group may have been related to a variable we did not study, such as hope or perceived control over pain. Unlike some of the other constructs measured in this study, PGIC is highly subjective and may be affected by treatment effects and expectations.50 Overall, results from our study extend the importance of addressing stress in online interventions.
Coping was not a significant mediator of treatment outcome, and this finding conforms to previous studies of CBT delivered in a traditional format.8 Several possible explanations for our results exist. It appears that one’s perceptions of personal coping (such as control beliefs, self-efficacy) exert a more influential meditational role than does the self-reported performance of coping behaviors.51 Alternatively, the effectiveness of pain coping behaviors, even well-practiced and wellness-focused ones, may be more dependent on pain levels than behavioral competence (e.g., very high pain levels may render coping behaviors ineffective). Future research is needed to more fully understand potential mediating roles of emotional factors and coping in the context of chronic pain.
This study possesses some distinct advantages over previous meditational studies of CBT treatments and pain. First, this is the first study that has examined mediators and moderators of an online CBT pain intervention. It appears that online interventions based on CBT principles may affect some of the same dimensions targeted by face-to-face CBT treatment. Second, this study examines pooled data from three types of pain (back pain, neuropathic pain, and arthritis pain), which addressed the lack of power that has been a limitation in previous work in mediator and moderator analyses with pain. Third, the emphasis of painACTION.com on self-management, which is consistent with current psychosocial approaches52, may provide some understanding of how stress can exert a meditational effect.
The present study also has several limitations. First, although we measured self-efficacy in all three studies, the measures were specific to pain types. In addition, catastrophizing was not measured in the neuropathic pain study. As a result, these data could not be combined. Previous researchers have found that these two cognitive factors are critical in explaining the effects of CBT on pain.8 However, we were able to evaluate other important mediators – emotional status and coping skills – that are commonly addressed within CBT and self-management programs. Second, there was a 26% attrition rate due to a combination of loss to follow- up and partial missing data. Our analysis indicated no meaningful significant differences between completers and noncompleters, and our rate of persistence is toward the upper range of studies of online psychological interventions.53 Third, participants in the three studies continued their normal pain treatment regimens, but their use of pain medication and other treatments were not tracked. It is possible that positive treatment outcomes may be at least partially due to the effects of other concurrent treatments, but it may also be possible that patients whose concurrent treatments were working may not have been motivated to be study participants. Unfortunately, we are not able to assess these possibilities given the available data.
Clinically, the present study adds to the literature showing the importance of stress in mediating changes in outcome of an online self-management intervention for several chronic pain conditions. Clinicians have long been aware of the importance of attending to emotional factors and in the treatment of chronic pain.47,54 This study provides support for online CBT and self-management websites that may be helpful in supporting the clinical goals pain clinicians have for their patients. Additionally, in the absence of interdisciplinary health professionals with training in CBT and self-management, health providers should consider recommending a site that supports outcomes consistent with ideal interdisciplinary clinical care. Finally, due to the lack of moderator findings, this study suggests that patient characteristics may be less important in pain management than the cognitive, emotional, and behavioral factors that change in response to treatment.
Table 1.
Baseline demographic characteristics of the study sample (N = 668)
| Total N = 668 |
Control N = 342 |
Experimental N = 326 |
Test Statistic† |
p- value‡ |
|
|---|---|---|---|---|---|
| Age (Mean ± SD) | 48.75 ± 11.72 | 47.93 ± 11.18 | 49.62 ± 12.21 | −1.9 | 0.06 |
| Gender | |||||
| Female | 485 (72.6) | 252 (73.7) | 233 (71.5) | 0.41 | 0.52 |
| Race | |||||
| White | 593 (88.8) | 302 (88.3) | 291 (89.3) | 5.57 | 0.47 |
| Black | 40 (6.0) | 19 (5.6) | 21 (6.4) | ||
| Other | 35 (5.2) | 21 (6.1) | 14 (4.3) | ||
| Education | |||||
| Less than HS | 5 (0.8) | 2 (0.6) | 3 (0.9) | 2.33 | 0.80 |
| HS | 133 (19.9) | 66 (19.3) | 67 (20.6) | ||
| Some college | 190 (28.4) | 101 (29.5) | 89 (27.3) | ||
| Completed college | 340 (50.9) | 173 (50.6) | 167 (51.2) | ||
| Marital Status | |||||
| Never Married | 108 (16.2) | 58 (17.0) | 50 (15.3) | 4.60 | 0.60 |
| Married | 371 (55.5) | 184 (53.8) | 187 (57.5) | ||
| Separated/ Divorced | 102 (15.3) | 50 (14.6) | 52 (15.9) | ||
| Other | 87 (13.0) | 50 (14.6) | 37 (11.3) | ||
| Income | |||||
| $49,999 or less | 226 (33.8) | 113 (33.0) | 113 (34.7) | 3.74 | 0.81 |
| $50,000-$99,999 | 243 (36.4) | 125 (36.5) | 118 (36.2) | ||
| over $100,000 | 136 (20.4) | 72 (21.0) | 64 (19.6) | ||
| Choose not to answer | 63 (9.4) | 32 (9.5) | 31 (9.5) | ||
| Current pain | 5.32 (2.24) | 5.41 (2.19) | 5.23 (2.29) | 1.02 | 0.31 |
Values expressed as N (%), except for age.
Test statistics is t-test for continuous variable age and χ2 for categorical variables, comparing control and experimental groups.
p-values pertain to tests for difference between control and experimental groups.
Footnotes
Conflicts of Interest and Source of Funding: The authors have no conflicts of interest to report. The preparation of this manuscript was funded by SBIR Grant # 5R44AR061191-03, awarded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases.
References
- 1.Baer RA, Carmody J, Hungsinger M. Weekly change in mindfulness and perceived stress in a mindfulness-based stress reduction program. J Clin Psychol. 2012 Jul;68(7):755–65. doi: 10.1002/jclp.21865. [DOI] [PubMed] [Google Scholar]
- 2.Rahman A, Reed E, Underwood M. Factors affecting self-efficacy and pain intensity in patients with chronic musculoskeletal pain seen in a specialist rheumatology pain clinic. Rheumatology. 2008;47(12):1803–1808. doi: 10.1093/rheumatology/ken377. [DOI] [PubMed] [Google Scholar]
- 3.Grotle M, Vollestad NK, Veierod MB, et al. Fear-avoidance beliefs and distress in relation to disability in acute and chronic low back pain. Pain. 2004;112(3):343–352. doi: 10.1016/j.pain.2004.09.020. [DOI] [PubMed] [Google Scholar]
- 4.Esteve R, Ramírez-Maestre C, López-Marínez AE. Adjustment to chronic pain: the role of pain acceptance, coping strategies, and pain-related cognitions. Ann Behav Med. 2007 Apr;33(2):179–88. doi: 10.1007/BF02879899. [DOI] [PubMed] [Google Scholar]
- 5.Edwards RR, Bingham CO3rd, Bathon J, et al. Catastrophizing and pain in arthritis, fibromyalgia, and other rheumatic diseases. Arthritis Rheum. 2006;55:325–332. doi: 10.1002/art.21865. [DOI] [PubMed] [Google Scholar]
- 6.Young CC, Greenberg MA, Nicassio PM. Transition from acute to chronic pain and disability: a model including cognitive, affective, and trauma factors. Pain. 2008;134(1–2):69–79. doi: 10.1016/j.pain.2007.03.032. [DOI] [PubMed] [Google Scholar]
- 7.Ritter PL, Lee J, Lorig K. Moderators of chronic disease self-management programs: who benefits? Chronic Illn. 2011;7(2):162–172. doi: 10.1177/1742395311399127. [DOI] [PubMed] [Google Scholar]
- 8.Turner JA, Holtzman S, Mancl L. Mediators, moderators, and predictors of therapeutic change in cognitive-behavioral therapy for chronic pain. Pain. 2007;127:276–286. doi: 10.1016/j.pain.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 9.Vlaeyen JWS, Morley S. Cognitive-behavioral treatments for chronic pain: what works for whom? Clin J Pain. 2005;21:1–8. doi: 10.1097/00002508-200501000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Hoffman BM, Papas RK, Chatkoff DK, et al. Meta-analysis of psychological interventions for chronic low back pain. Health Psychol. 2007;26(1):1–9. doi: 10.1037/0278-6133.26.1.1. [DOI] [PubMed] [Google Scholar]
- 11.Dirmaier J, Härter M, Weymann N. A tailored, dialogue-based health communication application for patients with chronic low back pain: study protocol of a randomised controlled trial. BMC Med Inform Decis. 2013;13:66–74. doi: 10.1186/1472-6947-13-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Simon D, Kriston L, von Wolff A. Effectiveness of a web-based, individually tailored decision aid for depression or acute low back pain: a randomized controlled trial. Patient Educ Couns. 2012;87(3):360–368. doi: 10.1016/j.pec.2011.10.009. [DOI] [PubMed] [Google Scholar]
- 13.Solomon M, Wagner SL, Goes J. Effects of a Web-based intervention for adults with chronic conditions on patient activation: online randomized controlled trial. J Med Internet Res. 2012;14(1):e32. doi: 10.2196/jmir.1924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holman H, Lorig K. Patient self-management: a key to effectiveness and efficiency in care of chronic disease. Public Health Rep. 2004 May-Jun;119(3):239–43. doi: 10.1016/j.phr.2004.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berman RLH, Iris MA, Bode R, et al. The effectiveness of an online mind-body intervention for older adults with chronic pain. J Pain. 2009;10(1):68–79. doi: 10.1016/j.jpain.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 16.Carpenter KM, Stoner SA, Mundt JM, et al. An online self-help CBT intervention for chronic lower back pain. Clin J Pain. 2012;28(1):14–22. doi: 10.1097/AJP.0b013e31822363db. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lorig KR, Ritter PL, Laurent DD, et al. The internet-based arthritis self-management program: a one-year randomized trial for patients with arthritis or fibromyalgia. Arthritis Rheum. 2008 Jul 15;59(7):1009–1017. doi: 10.1002/art.23817. [DOI] [PubMed] [Google Scholar]
- 18.Ruehlman LS, Karoly P, Enders C. A randomized controlled evaluation of an online chronic pain self-management program. Pain. 2012;153(2):319–330. doi: 10.1016/j.pain.2011.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Macea DkazD, Gajos K, Daglia Calil YA, Fregni F. The efficacy of web-based cognitive behavioral interventions for chronic pain: a systematic review and meta-analysis. J Pain. 2010 Oct;11(10):917–29. doi: 10.1016/j.jpain.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 20.Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annu Rev Clin Psycho. 2007;3:1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- 21.Kraemer HC, Wilson GT, Fairburn CG, et al. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiat. 2002 Oct;59(10):877–83. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- 22.Holroyd KA, Labus J, Carlson B. Moderation and mediation in the psychological and drug treatment of chronic tension-type headache: the role of disorder severity and psychiatric comorbidity. Pain. 2009;143(3):213–222. doi: 10.1016/j.pain.2009.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bender JL, Radhakrishnan A, Diorio C, et al. Can pain be managed through the Internet? a systematic review of randomized controlled trials. Pain. 2011;152(8):1740–1750. doi: 10.1016/j.pain.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 24.Chiauzzi E, Pujol LA, Wood M. painACTION-back pain: a self- management website for people with chronic back pain. Pain Med. 2010;11:1044–1058. doi: 10.1111/j.1526-4637.2010.00879.x. [DOI] [PubMed] [Google Scholar]
- 25.Venuti SV, Zacharoff KL, Pant PK, Black RA, DasMahapatra P, Bromberg J, Surette D. Web-based support to self-manage neuropathic Pain; Palm Springs, CA. Poster presented at: American Academy of Pain Medicine Annual Meeting.2012. Feb, [Google Scholar]
- 26.Trudeau KJ, Wall R, Pujol LM, DasMahapatra P, Pavek M, Venuti SW, Zacharoff K. A randomized controlled trial of an online pain self-management program for people with arthritis Pain; New Orleans, LA. Poster presented at: the American Pain Society.2013. May, [Google Scholar]
- 27.Cleeland CS. Pain Research Group Brief pain inventory (short form) 1991 [Google Scholar]
- 28.Keller S, Bann CM, Dodd SL, et al. Validity of the brief pain inventory for use in documenting the outcomes of patients with noncancer pain. Clin J Pain. 2004;20(5):309–318. doi: 10.1097/00002508-200409000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Mendoza T, Mayne T, Rublee D, et al. Reliability and validity of a modified brief pain inventory short form in patients with osteoarthritis. Eur J Pain. 2006;10(4):353–361. doi: 10.1016/j.ejpain.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 30.Tan G, Jensen MP, Thornby JI, et al. Validation of the brief pain inventory for chronic nonmalignant pain. J Pain. 2004;5(2):133–137. doi: 10.1016/j.jpain.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 31.Guy W. ECDEU Assessment Manual for Psychopharmacology. Washington, DC: US Government Printing Office; 1976. [Google Scholar]
- 32.Dworkin RH, Turk DC, Farrar JT, et al. IMMPACT. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005 Jan;(113)(1–2):9–19. doi: 10.1016/j.pain.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 33.Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. 2nd Ed. Sydney: Psychology Foundation; 1995a. [Google Scholar]
- 34.Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy. 1995b;33:335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- 35.Antony M, Bieling PJ, Cox BJ, et al. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and community a sample. Psychol Assessment. 1998;10:176–181. [Google Scholar]
- 36.Brown TA, Chorpita BF, Korotitsch W, et al. Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples. Behaviour Research and Therapy. 1997;35:79–89. doi: 10.1016/s0005-7967(96)00068-x. [DOI] [PubMed] [Google Scholar]
- 37.Crawford JR, Henry JD. The Depression Anxiety Stress Scales (DASS): normative data and latent structure in a large non-clinical sample. Brit J Clin Psychol. 2003;42:11–131. doi: 10.1348/014466503321903544. [DOI] [PubMed] [Google Scholar]
- 38.Jensen MP, Turner JA, Romano JM, et al. The chronic pain coping inventory: development and preliminary validation. Pain. 1995;60(2):203–216. doi: 10.1016/0304-3959(94)00118-X. [DOI] [PubMed] [Google Scholar]
- 39.Allison PD. [Accessed August 1, 2013];Handling missing data by maximum likelihood [Statistical Horizons SAS Global Forum] 2012 Available at: http://www.statisticalhorizons.com/wp-content/uploads/MissingDataByML.pdf.
- 40.Kiernan K, Tobias R, Gibbs P. [Accessed August 1, 2013];CONTRAST and ESTIMATE statements made easy: the LSMESTIMATE [Statistical Horizons SAS Global Forum] 2011 Available at: http://support.sas.com/resources/papers/proceedings11/351-2011.pdf.
- 41.Schabenberger O. Introducing the GLIMMIX procedure for generalized linear mixed models. [SAS Institute, Data Analysis Papers] [Accessed August 1, 2013];2005 Available at: http://www2.sas.com/proceedings/sugi30/196-30.pdf.
- 42.Schluchter MD. Flexible approaches to computing mediated effects in generalized linear models: Generalized estimating equations and bootstrapping. Multivariate Behav Res. 2008;43(2):268–288. doi: 10.1080/00273170802034877. [DOI] [PubMed] [Google Scholar]
- 43.Cappelleri JC, Zou KH, Bushmakin AG, Alvir JMJ, Alemayehu D, Symonds T. Patient-Reported Outcomes: Measurement, Implementation and Interpretation. Boca Raton, FL: CRC Press; 2014. [Google Scholar]
- 44.MacKinnon DP. Introduction to Statistical Mediation. New York, NY: Lawrence Erlbaum Associates; 2008. [Google Scholar]
- 45.Nevedal DC, Wang C, Oberleitner L, et al. Effects of an individually tailored web-based chronic pain management program on pain severity, psychological health, and functioning. J Med Internet Res. 2013 Sep 25;15(9):e201. doi: 10.2196/jmir.2296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Miles CL, Pincus T, Carnes D. Can we identify how programmes aimed at promoting self-management in musculoskeletal pain work and who benefits? a systematic review of sub-group analysis within RCTs. Eur J Pain. 2011;15(8):775.e1–775.e11. doi: 10.1016/j.ejpain.2011.01.016. [DOI] [PubMed] [Google Scholar]
- 47.Williams AC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Db Syst Rev. 2012;11:CD007407. doi: 10.1002/14651858.CD007407.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vachon-Presseau E, Martel MO, Roy M, et al. Acute stress contributes to individual differences in pain and pain-related brain activity in healthy and chronic pain patients. J Neuro Sci. 2013;33(16):6826–6833. doi: 10.1523/JNEUROSCI.4584-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ellegaard H, Pedersen BD. Stress is dominant in patients with depression and low back pain. A qualitative study of psychotherapeutic interventions for patients with non-specific low back pain of 3–12 months’ duration. BMC Musculoskel Dis. 2012;13:166–174. doi: 10.1186/1471-2474-13-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Farrar JT, Young JP, LaMoreaux L. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94:149–158. doi: 10.1016/S0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- 51.Lledo-Boyer A, Pastor-Mira MA, Pons-Calatayud N, Lopez-Roig S, Rodriguez-Marin J, Bruehl S. Control beliefs, coping and emotions: exploring relationships to explain fibromyalgia health outcomes. Int J Clin Health Psych. 2010;10(3):459–476. [Google Scholar]
- 52.Gatchel RJ, Peng YB, Peters ML, et al. The biopsychosocial approach to chronic pain: scientific advances and future directions. Pol Psychol Bull. 2007;133(4):581–624. doi: 10.1037/0033-2909.133.4.581. [DOI] [PubMed] [Google Scholar]
- 53.Donkin L, Glozier N. Motivators and motivations to persist with online psychological interventions: a qualitative study of treatment completers. J Med Internet Res. 2012;14(3):e91. doi: 10.2196/jmir.2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.McCracken LM, Turk DC. Behavioral and cognitive-behavioral treatment for chronic pain: outcome, predictors of outcome, and treatment process. Spine. 2002;27(22):2564–2573. doi: 10.1097/00007632-200211150-00033. [DOI] [PubMed] [Google Scholar]